Abstract
Background:
Few studies have examined the role of maternal emotions in breastfeeding outcomes.
Research aim:
We aimed to determine the extent to which maternal positive emotions during human milk feeding at two months were associated with time to any and exclusive human milk feeding cessation and overall breastfeeding experience.
Methods:
A sample of 192 women intending to breastfeed at least two months was followed from the third trimester through 12 months postpartum. Positive emotions during infant feeding at two months were measured using the modified Differential Emotions Scale. Cox proportional hazards regression was used to estimate adjusted hazard ratios (aHR) for time to any and exclusive human milk feeding cessation associated with a one-point increase in positive emotions. Linear regression was used to estimate the association between positive emotions and maternal breastfeeding experience reported at 12 months.
Results:
Among those human milk feeding at two months, positive emotions during feeding were not associated with human milk feeding cessation by 12 months (aHR=0.94, 95% CI: 0.64, 1.31). However, among women exclusively human milk feeding at two months, a one-point increase in positive emotions was associated with a 35% lower hazard of introducing formula or solid foods by six months (aHR=0.65, 95% CI: 0.46, 0.92). Positive emotions were associated with a significantly more favorable maternal report of breastfeeding experience at 12 months. Results were similar in sensitivity analyses using maternal feelings about breastfeeding in the first week as the exposure.
Conclusions:
A positive maternal emotional experience of feeding is associated with breastfeeding outcomes.
Keywords: breastfeeding experience, breastfeeding duration, epidemiological methods, exclusive breastfeeding, maternal psychology
Background
Breastfeeding is associated with a number of well-established health benefits for mothers and infants (Feltner et al., 2018; Horta, de Mola, & Victora, 2015; Sankar et al., 2015; Victora et al., 2016). As a result of these benefits, major medical organizations recommend exclusive breastfeeding for six months, with continued breastfeeding through the first year “or longer as mutually desired by the woman and her infant” (AAFP, 2014; AAP Section on Breastfeeding, 2012; ACOG, 2016). In the US, approximately 83.2% of women initiated breastfeeding in 2015, indicating a widespread desire to breastfeed; however, only 24.9% reported exclusive breastfeeding at six months and only 35.9% reported any breastfeeding at one year (Centers for Disease Control and Prevention, 2018).
The maternal experience of breastfeeding has not been rigorously studied; however, preliminary evidence suggests that maternal affect and feelings toward breastfeeding may affect breastfeeding outcomes. A systematic review of psychosocial correlates of exclusive breastfeeding identified three studies showing that positive maternal attitudes toward breastfeeding were associated with a higher likelihood of exclusive breastfeeding compared with ambivalent or negative attitudes (de Jager, Skouteris, Broadbent, Amir, & Mellor, 2013). In an Australian cohort, maternal breastfeeding satisfaction was a stronger predictor of time to weaning than breastfeeding problems (Cooke, Sheehan, & Schmied, 2003). In another study, prenatal negative affect was associated with an increased odds of mixed breastfeeding and bottle-feeding at six months postpartum (Ystrom, Niegel, Klepp, & Vollrath, 2008). A positive emotional experience of breastfeeding may also have implications for outcomes besides duration and exclusivity. Leff et al. found that maternal enjoyment and attainment of one’s desired maternal role were identified by mothers as more important for “successful” breastfeeding than duration (Leff, Gange, & Jefferis, 1994). Qualitative researchers have found that women who described breastfeeding as pleasurable and enjoyable report feeling an intimate connection with the infant, maternal confidence, and adequate support (Burns, Schmied, Sheehan, & Fenwick, 2010). In 1955, breastfeeding researcher Niles Newton wrote: “The number of months of breastfeeding are probably much less important psychologically than the type of breastfeeding and the type of weaning involved. Was the breastfeeding unsuccessful breastfeeding—with all the tension, fear, and pain that that involves? Or was it successful breastfeeding with its peace of mind and physical pleasure?” (Newton, 1955).
Barbara Fredrickson’s broaden-and-build theory of positive emotions states that experiences of positive emotions lead to adaptive benefits by broadening one’s thought-action repertoire, facilitating the accrual of resources to improve health. Interventions that increase experiences of positive emotions have been shown to improve resilience to future stressors through psychosocial resources, including social support and coping skills (Fredrickson & Joiner, 2018; Van Cappellen, Rice, Catalino, & Fredrickson, 2018). The broaden-and-build theory suggests that positive emotions experienced during breastfeeding may broaden the scope of a mother’s thoughts and actions, allowing her to build the resources necessary to cope with challenges.
In this study, we aimed to determine the extent to which positive emotions during human milk feeding at two months were associated with longer duration of any and exclusive human milk feeding. We also aimed to estimate the association between positive emotions at two months and women’s overall experience of breastfeeding at 12 months. We hypothesized that women with higher positive emotions at two months would sustain a longer duration of any and exclusive human milk feeding and report a better overall experience of breastfeeding at 12 months, compared to women with lower positive emotions. We explored modification of these relationships by maternal psychopathology in pregnancy.
Methods
Design
The Mood, Mother and Infant: The Psychobiology of Impaired Dyadic Development (MMI) study was designed as a prospective, longitudinal, one-group observational non-experimental study. The objective of this parent study was to determine the role of oxytocin and stress reactivity in maternal depression and impaired dyadic development. Data collected included detailed prospective information on maternal psychological health and infant feeding intentions and outcomes, from the third trimester until 12 months postpartum. All study procedures were approved by the University of North Carolina at Chapel Hill’s Institutional Review Board.
Setting
This cohort comprised women living near Chapel Hill, North Carolina, in the Southeast United States. The ethnic composition of this setting is predominantly non-Hispanic white (70%), followed by African American (12%) and Hispanic/Latino (9%) (United States Census Bureau, 2018). While breastfeeding rates in the Southeast are lower compared with other regions of the United States, breastfeeding rates in North Carolina are the highest in this region, with approximately 85% of women ever breastfeeding and 27% exclusively breastfeeding at six months (Centers for Disease Control and Prevention, 2018). Women living near Chapel Hill have been found to have greater access to Baby-Friendly Hospitals and IBCLCs compared with women in other areas of the state (Liberty, Wouk, Chetwynd, & Ringel-Kulka, 2019; Wouk, Chetwynd, Vitaglione, & Sullivan, 2016). Women were recruited for this study from study fliers and obstetric or psychiatric visits at clinics affiliated with the University of North Carolina Hospital, a Baby-Friendly hospital, between May 2013 through April 2017.
Sample
A total sample of 222 pregnant women were enrolled in the MMI study. Women with an elevated risk for postpartum depression and anxiety were oversampled to study the role of maternal and infant hormones in postpartum depression and breastfeeding. Risk status was ascertained based on a Structured Clinical Interview for DSM-IV (SCID)-confirmed history of depression/anxiety or active depressive/anxiety disorder in pregnancy; by design, about 1/3 of study participants had a SCID-reported history of depression or anxiety, and 1/3 had an active diagnosis. Eligible study participants were 18-45 years old, enrolled at >34 weeks’ gestation of a singleton pregnancy, able to communicate in English, and intending to breastfeed at least two months. Women were excluded from the study if they met any of the following criteria: history or current diagnosis of psychiatric disorders other than depression/anxiety; substance use; NICU admission >48 hours, major congenital anomaly, or neonatal death; use of tricyclic antidepressants; or contraindication for breastfeeding. For this analysis, we restricted to participants completing their 12-month visit by January 2018 (n=205). We excluded participants missing exposure data (n=12) and one who withdrew before contributing any infant feeding outcome data. The remaining 192 participants comprise our analytic sample, providing an adequate sample size to achieve 80% power with a two-sided alpha of 0.05 to detect a significant difference in the hazard of stopping any and exclusive human milk feeding.
Measurement
Positive Emotions.
We measured positive emotions during infant feeding at two months using the modified Differential Emotions Scale (mDES), which asks about 10 positive and 10 negative emotions experienced during infant feeding over the past week using a 5-point Likert scale (0=not at all, 4=extremely). The mDES was adapted from Izard’s Differential Emotions Scale (Izard, 1977) and has a high internal reliability ranging from 0.82-0.94 and high external validity with peer reports and biological markers (Cohn, Fredrickson, Brown, Mikels, & Conway, 2009; Fredrickson, Cohn, Coffey, Pek, & Finkel, 2008). Our exposure uses the positive emotions subscale of the mDES, which provides a mean score (range: 0-4) across 10 discrete emotions: amusement, awe, contentment, gratitude, hope, joy, interest, love, pride, and inspiration (Cronbach’s α = 0.91 conducted on our study sample) (Supplemental Figure 1).
Because this is the first time the mDES was applied in the context of infant feeding, we conducted a confirmatory factor analysis indicating the 10 positive emotions are unidimensional with roughly equal factor loadings (Supplemental Figure 2). Maternal positive emotions were analyzed as a continuous exposure and compared for consistency with alternate categorizations based on the distributions observed in the data. Using a priori criteria of model fit, a continuous exposure measure was chosen to estimate effects associated with a one-point increase in positive emotions in all analyses. A dichotomous classification of high (>2.5) versus low (<=2.5) positive emotions was chosen to present descriptive characteristics and Kaplan-Meier survival curves using the categorical exposure measure with most optimal model fit.
Participants who had discontinued human milk feeding by two months were censored from the primary analytic sample, leading to possible selection bias as the exposure was first measured at two months (Liang, Seeger, & Dore, 2016). To address this immortal person-time bias, sensitivity analyses were conducted using a measure of maternal feelings about breastfeeding in the first week. This exposure was defined by asking participants how they felt about breastfeeding using a Likert scale (1=Disliked very much, 5=Liked very much). By repeating analyses with a measure of maternal feelings about breastfeeding in week one, the entire sample was retained to determine if results differed due to selection bias. We also repeated analyses using the measure of maternal feelings about breastfeeding in the first week in the immortal person-time-flawed sample of participants doing any human milk feeding at two months to assess whether both exposures showed similar estimates of effect. As with the main exposure, a continuous measure of positive feelings in the first week was chosen based on model fit to estimate effects associated with a one-point increase.
Breastfeeding Outcomes.
Monthly between 1 and 12 months postpartum, participants were asked about how many times on average over the previous week their infant was fed human milk (including at-breast, expressed, or donor human milk), formula, or solid foods. Participants were also asked if their infant had been fed formula in the previous month. Time to cessation of any human milk feeding was defined using the infant age in weeks from birth to the date of the visit when the mother reported no longer feeding any human milk in the previous week. Participants who reported any human milk feeding at the final visit were censored at that date. Time to cessation of exclusive human milk feeding was defined using the infant age in weeks from birth to the date of the visit when the mother reported having fed formula any time in the previous month or any formula or solid foods in the previous week. Participants who reported exclusive human milk feeding at the six month-visit were censored at that date.
The overall experience of breastfeeding was assessed using the Maternal Breastfeeding Evaluation Scale (MBFES) at 12 months postpartum. The MBFES asks participants to consider their overall experience of breastfeeding and/or expressing milk for their most recent baby, comprising 30 items including the following: “It was a burden being my baby’s main source of food” and “My baby and I worked together to make breastfeeding go smoothly” (Leff, Jefferis, & Gagne, 1994) using a 4-point Likert scale (0=strongly disagree, 4=strongly agree). This tool has been shown to have high reliability and validity (Leff, Jefferis, et al., 1994), and we calculated a Cronbach’s alpha of 0.90 using our study sample (Supplemental Figure 3). The total MBFES score was considered the primary outcome, and secondary outcomes included subscores for three dimensions of maternal breastfeeding experience: maternal enjoyment/role attainment, infant satisfaction/growth, and lifestyle/maternal body image (Leff, Jefferis, et al., 1994).
Potential Covariates.
We used a directed acyclic graph (DAG) (Wouk, Bauer, & Gottfredson, 2018) to identify potential confounders (Supplemental Figure 4) and present measures of internal consistency for these variables from the literature where available (values are not calculated from the current study): prenatal depression symptoms via Beck Depression Inventory (Beck, Steer, & Brown, 1996) (Supplemental Figure 5) with a mean reliability α=0.87 and validity of α ≥ 0.60 (Beck, Steer, & Carbin, 1988); anxiety symptoms via State Trait Anxiety Inventory-State scores (Spielberger, Gorsuch, & Lushene, 1970) (Supplemental Figure 6) with a Cronbach’s alpha of 0.91-0.95 (Meades & Ayers, 2011); moderate/severe childhood trauma via the Childhood Trauma Questionnaire (Bernstein & Fink, 1998) (Supplemental Figure 7); attachment via Maternal Antenatal Attachment Scale (Supplemental Figure 8); prenatal breastfeeding intention (Nommsen-Rivers & Dewey, 2009) (Supplemental Figure 9); birth trauma via Modified Perinatal Post-Traumatic Stress Disorder Questionnaire (Callahan, Borja, & Hynan, 2006) (Supplemental Figure 10); early breastfeeding problems in the first two weeks; professional lactation support indexed by having received help from a lactation consultant in the hospital; social support (Sherboume & Stewart, 1991) (Supplemental Figure 11); return to work by two months; and concurrent negative emotions during infant feeding via mDES (Supplemental Figure 1) to highlight the unique contribution of positive emotions.
We explored modification of the association between positive emotions and breastfeeding outcomes by participants’ baseline psychopathology, where “high risk” was indexed by a SCID-confirmed history of depression/anxiety or an active depressive/anxiety disorder in pregnancy. Secondary analyses explored modification by infant feeding status at the time of exposure assessment.
Data Collection
Eligible participants were approached by study staff and invited to compete an online eligibility questionnaire or contact the study coordinator by phone. Written informed consent was obtained for all women who chose to enroll in the study. All data collection was conducted between May 2013 and April 2018. Baseline data were collected through questionnaires and interviews with study staff at the third trimester laboratory visit. Follow-up contacts occurred through monthly phone interviews and laboratory visits at 2, 6, and 12 months postpartum.
Data Analysis
Cox proportional hazards regression was used to estimate hazard ratios for time to any and exclusive human milk feeding cessation associated with a one-point increase in positive emotions. Participants who were exclusively formula feeding at two months (n=18, 9.4%) were excluded from the analysis of time to cessation of any human milk feeding, and participants not exclusively human milk feeding (n=78, 40.6%) were excluded from the time to cessation of exclusive human milk feeding, as they could not contribute time-to-event outcome data. Linear regression was used to estimate crude and multivariable associations between experiences of positive emotions during infant feeding at two months and the total score and subscores of overall breastfeeding experience at 12 months.
Confounders were included in multivariable Cox regression models where they were identified as important to adjust for based on subject-matter knowledge as represented in the DAG (Supplemental Figure 2, Dagitty, version 2.3). Crude Kaplan-Meier curves were computed to illustrate time to cessation of any and exclusive human milk feeding by high (>2.5) versus low (<=2.5) positive emotions. Crude and adjusted estimates and their associated 95% confidence intervals (CI) are presented for all models. Effect measure modification was considered to be present where p-values on interaction terms were <0.05.
Sensitivity analyses were conducted to repeat the above models using the measure of how much a participant liked breastfeeding in the first week postpartum, using both the full sample of those doing any human milk feeding at week one and the restricted sample of those doing any human milk feeding at month two. All analyses were conducted using SAS version 9.4 (“SAS,” 2014).
Results
Study sample characteristics
Descriptive characteristics are presented for the 192 study participants by high versus low positive emotions scores (Tables 1a and 1b). The mean positive emotions score was 2.8 (SD=0.8), with 66% (n=127) of the sample classified as experiencing high positive emotions. Participants with higher positive emotions during infant feeding at two months were significantly more likely to have had a vaginal birth, practiced skin-to-skin in the first hour, returned to work by two months, and report higher levels of antenatal attachment, social support, and positive feelings about breastfeeding in the first week postpartum. Participants with higher positive emotions during feeding were also significantly less likely to experience concurrent negative emotions, a traumatic birth experience, or early breastfeeding problems (Tables 1a and 1b).
Table 1a.
Frequency distribution of low (0-2.5) versus high (>2.5-4) positive emotions during infant feeding at two months (N= 192)
| Positive Emotionsa |
|||||
|---|---|---|---|---|---|
| Overall | Low n=65 |
High n=127 |
|||
| N (%) | n (%) | n (%) | Test statistic | p-valueb | |
| Positive emotions during infant feeding at 2 monthsa | 2.8 (0.8) | 1.9 (0.6) | 3.3 (0.4) | 192.00 | <0.001 |
| Infant feeding status at 2 months | 2.04 | 0.36 | |||
| Exclusive human milk feeding | 114 (59.4) | 34 (52.3) | 80 (63.0) | ||
| Any human milk feeding, not exclusive | 60 (31.3) | 24 (36.9) | 36 (28.4) | ||
| No human milk feeding | 18 (9.4) | 7 (10.8) | 11 (8.7) | ||
| Baseline psychopathologyc | 1.25 | 0.52 | |||
| Low risk | 58 (36.0) | 18 (31.0) | 41 (38.7) | ||
| High risk, history of depression/anxiety | 51 (31.1) | 18 (31.0) | 33 (31.1) | ||
| High risk, active depression/anxiety disorder | 54 (32.9) | 22 (37.9) | 32 (30.2) | ||
| Race/ethnicity | 1.94 | 0.34 | |||
| Non-Hispanic White | 141 (73.4) | 51 (78.5) | 90 (70.9) | ||
| Non-Hispanic Black | 19 (9.9) | 4 (6.2) | 15 (11.8) | ||
| Hispanic, any race | 21 (10.9) | 5 (6.2) | 16 (12.6) | ||
| Other | 11 (5.7) | 5 (7.7) | 6 (4.7) | ||
| Education Level | 0.52 | 0.77 | |||
| Some high school or high school graduate | 12 (6.3) | 5 (7.7) | 7 (5.5) | ||
| Some college or college graduate | 92 (47.9) | 32 (49.2) | 60 (47.2) | ||
| Post-graduate level | 88 (45.8) | 28 (43.1) | 60 (47.2) | ||
| Marital Status | 0.01 | 0.92 | |||
| Married/partnered | 169 (88.0) | 57 (87.7) | 112(88.2) | ||
| Single/divorced | 23 (12.0) | 8 (12.3) | 15(11.8) | ||
| Parity | 0.06 | 0.81 | |||
| Nulliparous | 104 (54.2) | 36 (55.4) | 68(53.5) | ||
| Multiparous | 88 (45.8) | 29 (44.6) | 59(46.5) | ||
| Psychotropic medication between baseline and 2 monthsd | 3.97 | 0.05 | |||
| Yes | 59 (30.7) | 26 (40.0) | 33(26.0) | ||
| No | 133 (69.3) | 39 (60.0) | 94(74.0) | ||
| Met prenatal breastfeeding intention at 2 monthse | 0.55 | 0.46 | |||
| Yes | 125 (65.1) | 40 (61.5) | 85(66.9) | ||
| No | 67 (34.9) | 25 (38.5) | 42(33.1) | ||
| Returned to work by 2 months | 5.82 | 0.02 | |||
| Yes | 57 (29.7) | 12 (18.5) | 45 (35.4) | ||
| No | 133 (69.3) | 52 (80.0) | 81 (63.8) | ||
| Moderate to Severe Childhood Trauma Experiencef | 0.77 | 0.38 | |||
| Yes | 54 (28.1) | 16 (24.6) | 38 (29.9) | ||
| No | 132 (68.8) | 48 (73.8) | 84 (66.1) | ||
| Skin-to-skin practiced in the first hour postpartum | 6.07 | 0.01 | |||
| Yes | 179 (93.7) | 57 (87.7) | 122 (96.8) | ||
| No | 12 (6.3) | 8 (12.3) | 4 (3.2) | ||
| Type of birth | 4.14 | 0.04 | |||
| Vaginal | 162 (84.4) | 50 (76.9) | 112 (88.2) | ||
| Cesarean section | 30 (15.6) | 15 (23.1) | 15 (11.8) | ||
| Received in-hospital BF help from IBCLC in hospital | 0.53 | 0.47 | |||
| Yes | 157 (81.2) | 55 (84.6) | 102 (80.3) | ||
| No | 35 (18.2) | 10 (15.4) | 25 (19.7) | ||
Note: Other race/ethnicity includes Asian, Native Hawaiian or other Pacific Islander, and American Indian/Alaska Native. BF = breastfeeding.
mDES scores range from 0 to 4, with higher scores indicating more emotions; descriptive statistics are presented by high positive emotions (score of >2.5-4) and low positive emotions (0-2.5).
Chi-Square test where cell counts>5 observations or Fisher’s exact test for small cell sizes; p-values bolded if significant a p<0.05.
Based on Structured Clinical Interview for Diagnosis (SCID) criteria for a history of or current depression (including Major Depressive Disorder, Dysthymic Disorder, Depressive Disorder NOS, or Postpartum Depression) or anxiety (including Panic Disorder, Agoraphobia, Social Phobia, Obsessive Compulsive Disorder, Generalized Anxiety Disorder, or Post Traumatic Stress Disorder), administered in the third trimester of pregnancy
Includes self-reported use of any of the following medications: antidepressants, benzodiazepines, antipsychotics, and hypnotics
Defined as meeting prenatal intention for any and exclusive breastfeeding; 2 missing values
Defined as meeting the threshold for moderate/severe emotional abuse, physical abuse, sexual abuse, emotional neglect, or physical neglect on the 28-item Childhood Trauma Questionnaire; 6 missing values
Table 1b.
A comparison of the mean (SD) low (0-2.5) versus high (>2.5-4) positive emotions during infant feeding at two months (N = 192)
| Positve Emotions2 |
|||||
|---|---|---|---|---|---|
| Total | Low n=65 |
High n=127 |
|||
| Variable & Scale Scores | M (SD) | M (SD) | M (SD) | t- Test | p-value |
| Negative emotions during infant feedinga | 0.6 (0.6) | 0.7 (0.6) | 0.5 (0.5) | 2.68 | 0.01 |
| Infant feeding intentionb | 14.6 (2.3) | 14.4 (2.5) | 14.9 (1.9) | −1.62 | 0.11 |
| Modified perinatal trauma scorec | 6.4 (6.8) | 8.2 (7.3) | 5.6 (6.4) | 2.52 | 0.01 |
| Antenatal attachmentd | 76.4 (6.2) | 74.0 (6.9) | 77.7 (5.4) | −3.99 | <0.001 |
| Social support at 2 monthse | 3.4 (0.7) | 3.3 (0.7) | 3.5 (0.6) | −2.55 | 0.01 |
| Breastfeeding problems in first 2 weeksf | 4.1 (2.0) | 4.6 (2.0) | 3.9 (1.9) | 2.38 | 0.02 |
| Breast pain, day one postpartumg | 1.01 (0.9) | 1.15 (0.9) | 0.94 (0.9) | 1.58 | 0.12 |
| Positive feelings about breastfeeding, week one,h median (IQR) | 4 (2-5) | 3 (2-4) | 4 (3-5) | −3.29 | 0.001 |
Note: p-values are bolded if significant a p<0.05.
Modified Differential Emotion Scale scores range from 0 to 4, with higher scores indicating more emotions; descriptive statistics are presented by high positive emotions (score of >2.5-4) and low positive emotions (0-2.5).
Infant Feeding Intentions Scale scores range from 0-16, with higher scores indicating a stronger intent to initiate and sustain exclusive breastfeeding
Modified Perinatal Post-Traumatic Stress Disorder Questionnaire scores range from 0-56, with higher scores indicating more perinatal ptsd
Maternal Antenatal Attachment Scale scores range from 19-95, with higher scores indicated stronger attachment
Medical Outcomes Study Social Support Survey (MOS) scores range from 0-4, with higher scores indicating more support
Early breastfeeding problems scores range from 0 to 18, with higher scores indicating more problems
Likert scale from “0: None” to “3: Severe”
Likert scale measured feelings about breastfeeding in the first week postpartum, ranging from “1: Disliked very much” to “5: Liked very much”
Positive emotions and time to cessation of any human milk feeding
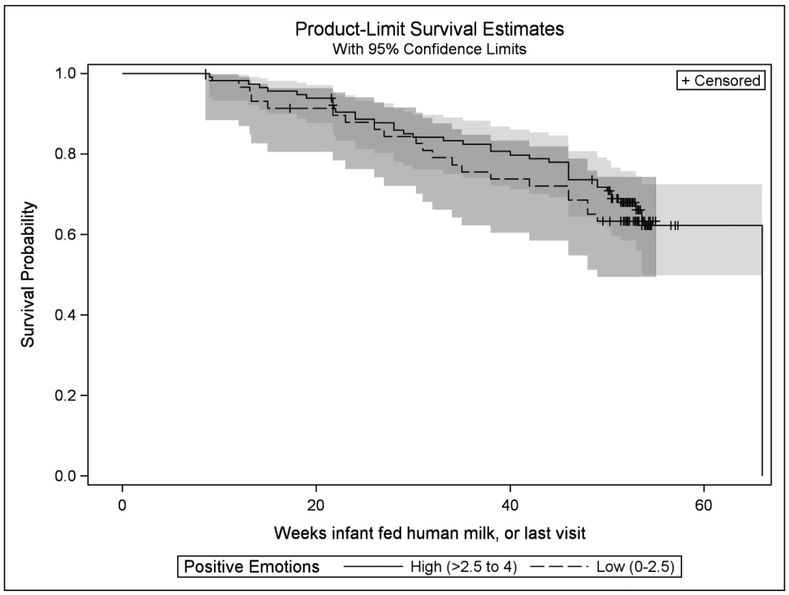
The crude Kaplan-Meier curves for time to cessation of any human milk feeding were not significantly different by high versus low positive emotions (Figure 1). A one-point increase in positive emotions at two months was associated with 0.94 (95% CI: 0.64, 1.31) times the hazard of stopping any human milk feeding after adjustment for confounders (Table 2). This association was not significantly different by a participant’s baseline psychopathology (LRT p=0.82). Results were similar in sensitivity analyses conducted using both the same restricted sample as main analyses and using the entire sample of participants doing any human milk feeding at one week postpartum (Table 2).
Figure 1:
Crude Kaplan-Meier curves and 95% confidence intervals for time to cessation of any human milk feeding stratified by high (>2.5-4) versus low (0-2.5) positive emotions
Table 2:
Estimates of association between a one-unit increase in positive emotions and time to any and exclusive human milk feeding cessation
| Any human milk feeding cessationa | Exclusive human milk feeding cessationa | |||||
|---|---|---|---|---|---|---|
| Exposure | N | Crude HR (95% CI) |
Adjusted HR (95% CI) |
N | Crude HR (95% CI) |
Adjusted HR (95% CI) |
| Positive emotions during human milk feeding at 2 monthsb | 174 | 0.88 (0.64, 1.20) | 0.94 (0.64, 1.31) | 114 | 0.74 (0.53, 1.03) | 0.65 (0.46, 0.92) |
| Week 1 positive feelings about breastfeeding, among those human milk feeding at 2 monthsc | 174 | 0.78 (0.65, 0.93) | 0.89 (0.72, 1.11) | 114 | 0.85 (0.70, 1.02) | 0.75 (0.60, 0.94) |
| Week 1 positive feelings about breastfeeding, among those human milk feeding at week 1c | 192 | 0.77 (0.65, 0.91) | 0.87 (0.72, 1.06) | 185 | 0.74 (0.66, 0.84) | 0.77 (0.66, 0.89) |
Note: Bolded results are significant at p<0.05.
Cox proportional hazards regression models were used to estimate hazard ratios (HR) for time to cessation of human milk feeding and exclusive human milk feeding. Participants who were exclusively formula feeding at two months (n=18, 9.4%) were excluded from the analysis of time to cessation of any human milk feeding, and participants not exclusively human milk feeding (n=78, 40.6%) were excluded from the time to cessation of exclusive human milk feeding, as they could not contribute time-to-event outcome data.
Models using positive emotions at two months as the exposure were adjusted for confounding by prenatal depression score, social support, professional breastfeeding support from an IBCLC in the hospital, modified Perinatal PTSD Questionnaire score, number of breastfeeding problems in the first two weeks, and negative emotions during infant feeding at two months
Models using positive emotions at one week postpartum as the exposure were adjusted for confounding by prenatal infant feeding intention score, social support, modified Perinatal PTSD Questionnaire score, and professional breastfeeding support from an IBCLC in the hospital.
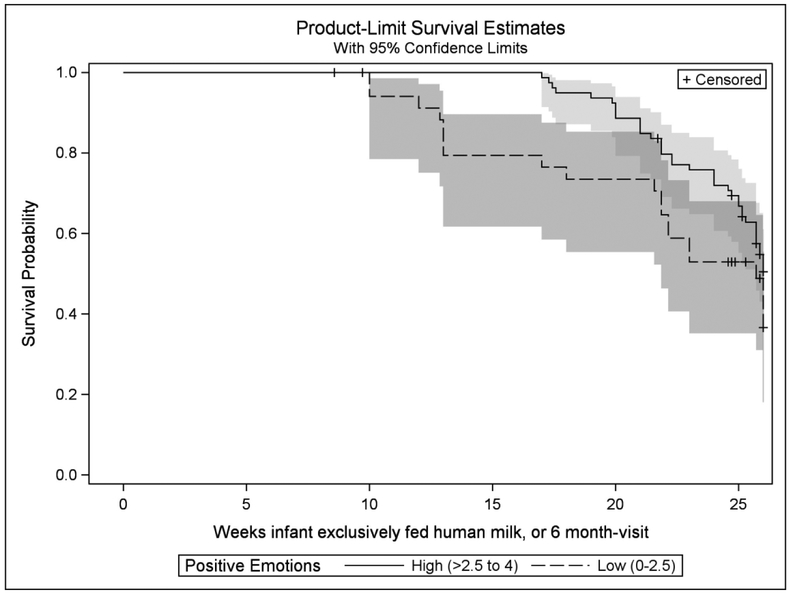
Positive emotions and time to cessation of exclusive human milk feeding
The crude Kaplan-Meier curves for time to cessation of exclusive human milk feeding differed by high versus low positive emotions (Figure 2). A one-point increase in positive emotions at two months was associated with 0.65 (95% CI: 0.46, 0.92) times the hazard of stopping exclusive human milk feeding after adjustment for confounders (Table 2). There was no modification by baseline psychopathology (LRT p=0.75) or infant feeding status (exclusive v. non-exclusive, LRT p=0.22). Results from sensitivity analyses were similar and slightly more precise (Table 2).
Figure 2:
Crude Kaplan-Meier curves and 95% confidence intervals for time to cessation of exclusive human milk feeding stratified by high (>2.5-4) versus low (0-2.5) positive emotions
Positive emotions and overall experience of breastfeeding
In the overall sample, a one-point increase in positive emotions at two months was associated with an adjusted 5.96 (95% CI: 3.16, 8.76) points higher score on the MBFES (Table 3). This association was not significantly different by infant feeding status at two months (p=0.68). In secondary analyses probing the overall experience of breastfeeding by MBFES subscale and adjusted for confounders, positive emotions at two months were associated with the maternal enjoyment/role attainment and lifestyle/maternal body image subscales (Table 3). In adjusted sensitivity analyses using the complete sample, a one-point increase in positive feelings about breastfeeding at one week postpartum was associated with an adjusted 4.74 (95% CI: 3.12, 6.35) point increase on the MBFES. This earlier exposure measure was also associated with higher scores on all MBFES subscales (Table 3).
Table 3:
Estimates of association between a one-unit increase in positive emotions and overall maternal breastfeeding experience at 12 months
| Exposure | N | Crude Beta (95% CI) |
Adjusted Beta (95% CI) |
|---|---|---|---|
| Overall breastfeeding experience: MBFES (range 0-120)a | |||
| Positive emotions during infant feeding at 2 months | 186 | 7.11 (4.29, 9.92) | 5.96 (3.16, 8.76) |
| Positive feelings about breastfeeding at week 1 | 186 | 5.58 (4.01, 7.16) | 4.74 (3.12, 6.35) |
| Maternal Enjoyment and Role Attainment Subscale (range 0-56) | |||
| Positive emotions during infant feeding at 2 months | 186 | 4.30 (2.68, 5.93) | 3.88 (2.25, 5.51) |
| Positive feelings about breastfeeding at week 1 | 186 | 3.24 (2.33, 4.16) | 2.85 (1.91, 3.79) |
| Infant Satisfaction and Growth Subscale (range 0-32) | |||
| Positive emotions during infant feeding at 2 months | 186 | 1.60 (0.40, 2.80) | 1.01 (−0.14, 2.17) |
| Positive feelings about breastfeeding at week 1 | 186 | 1.79 (1.11, 2.46) | 1.49 (0.79, 2.19) |
| Lifestyle and Maternal Body Image Subscale (range 0-32) | |||
| Positive emotions during infant feeding at 2 months | 186 | 2.15 (0.91, 3.39) | 1.49 (0.28, 2.69) |
| Positive feelings about breastfeeding at week 1 | 186 | 2.22 (1.54, 2.91) | 1.83 (1.12, 2.53) |
Note: Linear regression models were used for continuous Maternal Breastfeeding Evaluation Scale total and subscore outcomes. Models using positive emotions at two months as the exposure were adjusted for confounding by prenatal depression score, social support, professional breastfeeding support from an IBCLC in the hospital, birth trauma, number of breastfeeding problems in the first two weeks, and negative emotions during infant feeding at two months. Models using positive emotions at one week postpartum as the exposure were adjusted for confounding by prenatal infant feeding intention score, social support, birth trauma, and professional breastfeeding support from an IBCLC in the hospital. Bolded results are significant at p<0.05.
Discussion
Consistent with our hypothesis, positive emotions during feeding at two months were associated with a longer time to cessation of exclusive human milk feeding and with a better overall maternal breastfeeding experience. Contrary to our hypothesis, positive emotions at two months were not associated with any human milk feeding cessation across the first year postpartum. Maternal feelings about breastfeeding in the first week yielded similar and more precise associations with all outcomes.
Higher positive emotions during exclusive human milk feeding at two months were predictive of a longer exclusive human milk feeding duration. By two months, when mothers are able to exclusively human milk feed, maternal enjoyment of feeding may provide sufficient motivation to meet public health targets. However, higher positive emotions during any human milk feeding at two months were not predictive of a longer duration of human milk feeding. We did not observe differences by human milk feeding status at two months, exclusive vs. non-exclusive. However, the group of mothers who are feeding any human milk at two months comprises both women who have met their prenatal intention and those who have faced early physiological and/or structural barriers that prevented them from meeting their exclusivity goals. This heterogeneity may attenuate the effect of positive emotions seen among those exclusively human milk feeding. We speculate that when a mother is feeding any human milk feeding at two months but faced many early challenges to exclusive feeding, maternal enjoyment of feeding may reflect satisfaction with the experiential aspects of feeding and less concern about providing human milk as a product.
In our sample, participants with low positive emotions during feeding at two months were more likely to have also had a cesarean birth, a more traumatic birth experience, and no skin-to-skin with the infant in the first hour after birth. The early maternal breastfeeding experience may be a modifiable factor for improving long-term breastfeeding outcomes, underscoring the importance of supporting mothers to process difficult birth experiences and cope with early breastfeeding challenges. Maternity practices like those implemented through the Baby-Friendly Hospital Initiative have been found to increase breastfeeding duration and exclusivity in several studies (Munn, Newman, Mueller, Phillips, & Taylor, 2016; Pérez-Escamilla, Martinez, & Segura-Pérez, 2016). Specific Baby-Friendly Hospital practices like skin-to-skin contact in the first hour after birth also correlate with later maternal breastfeeding satisfaction even among mothers not intending to breastfeed exclusively (Hongo, Nanishi, Shibanuma, & Jimba, 2015). Mother-centered maternity practices that support the relational and experiential aspects of breastfeeding may improve both breastfeeding rates and maternal breastfeeding satisfaction. The association between positive feelings about breastfeeding in the first week and breastfeeding outcomes across the first year postpartum underscores the importance of providing timely mother-centered support in the hospital and community to help women enjoy the early breastfeeding experience. Healthcare providers who interface with mothers in the early postpartum should use collaborative decision-making tools, asking open-ended questions and offering resources tailored to each woman’s experiences and constraints, to support the experiential aspects of infant feeding (Schmied, Beake, Sheehan, McCourt, & Dykes, 2011; Tully, Stuebe, & Verbiest, 2017).
Maternal emotions during infant feeding appear to be predictive of breastfeeding outcomes, and not just reflective of an easy breastfeeding experience. After controlling for numerous covariates known to predict early breastfeeding cessation, including early breastfeeding problems, professional lactation support, and social support, we found an association between positive maternal emotions and both exclusive human milk feeding and a better maternal experience of breastfeeding. The lack of modification of our findings by prenatal psychopathology or infant feeding status at two months suggests that the experiential and relational aspects of infant feeding may yield benefits regardless of early postpartum challenges. Therefore, healthcare providers and peer supporters should address the maternal emotional experience of infant feeding regardless of infant feeding method, given the potential benefits for both postpartum mental health (Wouk, Gottfredson, et al., 2018) and overall maternal satisfaction with breastfeeding.
Our study has several strengths. To our knowledge, we are the first investigators to apply the broaden-and-build theory of positive emotions as a framework for research about the maternal infant feeding experience. While the mDES has not been previously used in the context of infant feeding, it has been validated across numerous contexts (Fredrickson & Joiner, 2018), and we used a factor analysis to confirm the positive emotions subscale best represented one construct in relation to maternal emotions during feeding. Future researchers would benefit from applying this tool at various timepoints across the breastfeeding experience to clarify temporal dynamics of positive emotions. We also collected extensive longitudinal data about infant feeding and maternal and infant characteristics across the postpartum, addressing some limitations of previous correlational and cross-sectional research about positive emotions.
Limitations
Our findings should be interpreted in the context of study limitations. Participants must have intended to breastfeed at least two months to enroll in the parent study; their high motivation to breastfeed may have limited our ability to detect differences in any human milk feeding cessation. We oversampled women at risk for postpartum psychopathology and comprised predominantly Non-Hispanic White, partnered, and highly educated women. Future research about positive emotions during infant feeding should be conducted in diverse populations, especially among underrepresented minority women and groups with lower breastfeeding intentions. Self-report measures used in analyses may have led to measurement bias, especially to the extent that affective responses were influenced by concurrent depression or anxiety; however, we did not observe modification of our results by baseline psychopathology. While sensitivity analyses used a measure of positive feelings that has not been well validated, results were similar to the mDES exposure, suggesting that both tools were capturing similar constructs. We used a DAG to identify causal and non-causal paths between our exposure and outcomes of interest, and used online software to identify the minimally sufficient adjustment set of confounders to adjust for in models. Researchers should build upon or alter our theoretical model using new evidence to ensure its appropriateness and to justify using an appropriate set of confounders. Unmeasured confounding is reduced in these analyses due to breadth of data collected over time on participants and the minor amount of missingness.
Conclusions
The maternal emotional experience of infant feeding and associated maternal and infant outcomes have not yet been rigorously researched. According to the broaden-and-build theory of positive emotions, experiences of positive emotions trigger upward spirals that improve well-being (Fredrickson & Joiner, 2018). In this study, we provide preliminary evidence for an association between maternal positive emotions during breastfeeding and improved duration of exclusive human milk feeding and overall maternal breastfeeding experience. These results can inform future mother-centered interventions and policies to support the quality of the breastfeeding experience and to improve maternal and infant health.
Supplementary Material
Key Messages:
Maternal emotions have been studied in relation to breastfeeding mostly through the lens of psychopathology; few studies have explored the role of positive maternal emotions.
In our cohort, positive emotions were not associated with any human milk feeding duration across the first year; however, positive emotions were associated with longer exclusive human milk feeding duration across the first six months.
Positive emotions during feeding were associated with a better overall maternal experience of breastfeeding.
Research testing strategies to increase positive emotions can inform mother-centered interventions and policies to better support the emotional experience of infant feeding.
Acknowledgments:
Thank you to Brenda Pearson, the entire Mood, Mother and Infant study team, and to all the families who participated in this research.
Funding Acknowledgment: This work was supported by the National Institute of Child Health and Human Development (R01HD073220 and 4T32HD052468-09) and the National Institute on Drug Abuse (K01 DA035153).
Footnotes
Conflict of Interest Statement: The authors have no conflicts of interest to disclose.
References
- American Academy of Family Physicians. (2014). Breastfeeding, Family Physicians Supporting (Position Paper) -- AAFP Policies. [Google Scholar]
- American Academy of Pediatrics Section on Breastfeeding. (2012). Breastfeeding and the use of human milk. Pediatrics, 129(3), e827–e841. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio. [Google Scholar]
- Beck AT, Steer RA, & Carbin MG (1988). Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 5(1), 77–100. 10.1016/0272-7358(88)90050-5 [DOI] [Google Scholar]
- Bernstein DP, & Fink L (1998). Childhood Trauma Questionnaire: A Retrospective Self-Report Manual. San Antonio. [Google Scholar]
- Burns E, Schmied V, Sheehan A, & Fenwick J (2010). A meta-ethnographic synthesis of women’s experience of breastfeeding. Maternal and Child Nutrition, 6(3), 201–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callahan JL, Borja SE, & Hynan MT (2006). Modification of the Perinatal PTSD Questionnaire to enhance clinical utility. Journal of Perinatology, 26(9), 533–539. 10.1038/sj.jp.7211562 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018). Breastfeeding Report Card - United States, 2018.
- Cohn MA, Fredrickson BL, Brown SL, Mikels JA, & Conway AM (2009). Happiness unpacked: Positive emotions increase life satisfaction by building resilience. Emotion, 9(3), 361–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke M, Sheehan A, & Schmied V (2003). A Description of the Relationship Between Breastfeeding Experiences, Breastfeeding Satisfaction, and Weaning in the First 3 Months After Birth. J Hum Lact, 19(2), 145–156. [DOI] [PubMed] [Google Scholar]
- de Jager E, Skouteris H, Broadbent J, Amir L, & Mellor K (2013). Psychosocial correlates of exclusive breastfeeding: A systematic review. Midwifery, 29(5), 506–518. [DOI] [PubMed] [Google Scholar]
- Feltner C, Palmieri Weber R, Stuebe AM, Grodensky CA, Orr C, & Viswanatha M (2018). Breastfeeding Programs and Policies, Breastfeeding Uptake, and Maternal Health Outcomes in Developed Countries. Comparative Effectiveness Review, (210). 10.23970/AHRQEPCCER210 [DOI] [PubMed] [Google Scholar]
- Fredrickson BL, Cohn MA, Coffey KA, Pek J, & Finkel SM (2008). Open hearts build lives: positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology, 95(5), 1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, & Joiner T (2018). Reflections on Positive Emotions and Upward Spirals. Perspectives on Psychological Science, 13(2), 194–199. 10.1177/1745691617692106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hongo H, Nanishi K, Shibanuma A, & Jimba M (2015). Is Baby-Friendly Breastfeeding Support in Maternity Hospitals Associated with Breastfeeding Satisfaction Among Japanese Mothers? Maternal and Child Health Journal, 19(6), 1252–1262. 10.1007/s10995-014-1631-8 [DOI] [PubMed] [Google Scholar]
- Horta BL, de Mola CL, & Victora CG (2015). Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure, and type-2 diabetes: systematic review and meta-analysis. Acta Paediatrica, 104, 30–37. [DOI] [PubMed] [Google Scholar]
- Izard C (1977). Human emotions. New York: Plenum Press. [Google Scholar]
- Leff E, Gange M, & Jefferis S (1994). Maternal perceptions of successful breastfeeding. Journal of Human Lactation, 10, 99–104. [DOI] [PubMed] [Google Scholar]
- Leff E, Jefferis S, & Gagne M (1994). The development of the Maternal Breastfeeding Evaluation Scale. J Hum Lact, 10(2), 105–111. [DOI] [PubMed] [Google Scholar]
- Liang C, Seeger JD, & Dore DD (2016). Implications of immortal person-time when outcomes are nonfatal. Annals of Epidemiology, 26(3), 212–217. [DOI] [PubMed] [Google Scholar]
- Liberty AL, Wouk K, Chetwynd E, & Ringel-Kulka T (2019). A Geospatial Analysis of the Impact of the Baby-Friendly Hospital Initiative on Breastfeeding Initiation in North Carolina. Journal of Human Lactation, 35(1), 114–126. 10.1177/0890334418776645 [DOI] [PubMed] [Google Scholar]
- Meades R, & Ayers S (2011). Anxiety measures validated in perinatal populations: A systematic review. Journal of Affective Disorders, 133(1–2), 1–15. 10.1016/j.jad.2010.10.009 [DOI] [PubMed] [Google Scholar]
- Munn A, Newman S, Mueller M, Phillips S, & Taylor S (2016). The impact in the United States of the Baby-Friendly Hospital Initiative on early infant health and breastfeeding outcomes. Breastfeed Med, 11(5), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton N (1955). Maternal emotions; a study of women’s feelings toward menstruation, pregnancy, childbirth, breast feeding, infant care, and other aspects of their femininity. New York: P.B. Hoeber. [Google Scholar]
- Nommsen-Rivers LA, & Dewey KG (2009). Development and validation of the infant feeding intentions scale. Matern Child Health J, 13(3), 334–342. [DOI] [PubMed] [Google Scholar]
- Pérez-Escamilla R, Martinez JL, & Segura-Perez S (2016). Impact of the Baby-friendly Hospital Initiative on breastfeeding and child health outcomes: a systematic review. Maternal and Child Nutrition, 12(3), 402–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankar MJ, Sinha B, Chowdhury R, Bhandari N, Taneja S, Martines J, & Bahl R (2015). Optimal Breastfeeding Practices and Infant and Child Mortality- A Systematic Review and Meta-analysis. Acta Paediatrica, 104, 3–13. [DOI] [PubMed] [Google Scholar]
- SAS. (2014). Cary, NC: SAS Institute Inc. [Google Scholar]
- Schmied V, Beake S, Sheehan A, McCourt C, & Dykes F (2011). Women’s perceptions and experiences of breastfeeding support. Birth (Berkeley, Calif.), Vol 38, No 1, Pp 49–60., 14(7), 1–4. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, & Stewart AL (1991). The MOS social support survey. Soc Sci Med, 32(6), 705–714. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch R, & Lushene R (1970). Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consultant Psychologists Press. [Google Scholar]
- The American College of Obstetricians and Gynecologists. (2016). Committee opinion No. 658: Optimizing Support for Breastfeeding as Part of Obstetric Practice. [DOI] [PubMed]
- Tully KP, Stuebe AM, & Verbiest SB (2017). The fourth trimester: a critical transition period with unmet maternal health needs. American Journal of Obstetrics and Gynecology, 217(1), 37–41. 10.10167/j.ajog.2017.03.032 [DOI] [PubMed] [Google Scholar]
- United States Census Bureau. (2018). Quick Facts: Orange County, North Carolina. Retrieved March 27, 2019, from https://www.census.gov/quickfacts/orangecountynorthcarolina
- Van Cappellen P, Rice EL, Catalino LI, & Fredrickson BL (2018). Positive affective processes underlie positive health behaviour change. Psychology and Health, 33(1), 77–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, … Rollins NC (2016). Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet, 357(10017), 475–490. [DOI] [PubMed] [Google Scholar]
- Wouk K, Bauer AE, & Gottfredson NC (2018). How to implement directed acyclic graphs to reduce bias in addiction research. Addictive Behaviors, (September). [DOI] [PubMed] [Google Scholar]
- Wouk K, Chetwynd E, Vitaglione T, & Sullivan C (2016). Improving Access to Medical Lactation Support and Counseling: Building the Case for Medicaid Reimbursement. Maternal and Child Health Journal, 1–9. 10.1007/s10995-016-2175-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wouk K, Gottfredson NC, Tucker C, Pence BW, Meltzer-Brody S, Zvara B, … Stuebe AM (2018). Positive Emotions During Infant Feeding and Postpartum Mental Health. Journal of Women’s Health, 00(00), jwh.2017.6889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ystrom E, Niegel S, Klepp KI, & Vollrath ME (2008). The Impact of Maternal Negative Affectivity and General Self-Efficacy on Breastfeeding: The Norwegian Mother and Child Cohort Study. Journal of Pediatrics, 152, 68–72. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.