Abstract
Purpose:
To compare two mild-to-moderate group exercises and treatment as usual (TAU) for improvements in physical function and depressive symptoms.
Methods:
Patients with heart failure (HF) (n = 70, mean age = 66 yr, range = 45 – 89 yr) were randomized to 16-wk of Tai Chi (TC), resistance band (RB) exercise, or TAU.
Results:
Physical function differed by group from baseline to follow-up, measured by distance walked in the 6-min walk test (6MWT) (F = 3.19, P = .03). TC demonstrated a non-significant decrease of 162 ft [95% CI, 21 to −345, P = .08] while RB’s distance walked remained stable with a non-significant increase of 70 ft [95% CI, 267 to −127, P = .48]. TAU significantly decreased by 205 ft [95% CI, −35 to −374, P = .02] and no group differences occurred over time in end systolic volume (ESV) (P = .43) and left ventricular function (LVEF) (P = .67). However, groups differed over time in the Beck Depression Inventory (BDI) (F = 9.2, P < .01). Both TC and RB groups improved (decreased) by 3.5 points [95% CI, 2 - 5] (P < .01). TAU decreased insignificantly 1 point [95% CI, −1 to 3] (P = .27).
Conclusions:
TC and RB participants avoided a decrease in physical function decrements as seen with TAU. No groups changed in cardiac function. TC and RB groups both saw reduced depression symptoms compared with TAU. Thus, both TC and RB avoided a decrease in physical function and improved their psychological function when compared to TAU.
Condensed Abstract:
Tai Chi (TC), resistance band (RB) exercise, and treatment as usual (TAU) were compared in 70 heart failure patients. TC and RB group’s physical function remained stable, while TAU showed declines. TC and RB groups had reduced depression symptoms compared with TAU. None of the groups changed in cardiac function.
Heart failure (HF) is a worldwide public health problem associated with considerable morbidity, mortality and diminished quality of life.1 Although medications can improve some symptoms, individuals with HF with either preserved or reduced ejection fraction (HFpEF, HFrEF) continue to experience debilitating symptomatology, including exercise intolerance. In addition to physical symptoms, depressive symptoms are present in up to 30% of HF patients,2, 3 and are associated with increased mortality, clinical events, hospitalization, and general health care use.4 Yet the efficacy of antidepressant therapy in patients with coronary heart disease has been limited.5 The goal of exercise interventions in this chronic disease group is primarily to improve symptoms and the quality and duration of life 6. Research literature suggests vigorous exercise improves cardiorespiratory fitness 7, and can produce substantial reductions in depression symptoms in patients with HF 8–10. However, many exercise intervention studies consist of participants that are younger than the typical HF patient, with little comorbidity. The HF-ACTION study included participants with a median age of 59 yr (range 51-67 yr), and excluded patients with major comorbidities or limitations that could interfere with exercise training and/or with devices that limited the ability to achieve target heart rates 11. Meanwhile, over 80% of HF patients are > 65 yr of age and approximately 50% are > 80 yr 12. Many patients with HF have limited capacity for vigorous exercise due to comorbidities such as sarcopenia 13, anemia, 14 obesity, diabetes, chronic obstructive lung disease (COPD), peripheral artery disease, and advanced age 15, 16.
In contrast to conventional exercise, tai chi (TC) is composed of low-impact, mindfully meditative movements with integrated breathing techniques that generate a mild to moderate workout 17. Many TC interventions have been studied specifically in elderly and frail cohorts and are well tolerated across fitness levels 18. Research suggests that practicing TC is effective for reducing depression symptoms in a broad range of patients with HF, as compared to treatment as usual 17, 19. Meanwhile, resistance exercise is effective for increasing muscle strength, endurance, physical function (six minute walk test [6MWT]), and promoting favorable arterial remodeling 20. However, there are few if any studies that have examined resistance exercise for effects on depression symptoms in patients with HF
Moreover, few studies have investigated whether TC differs from more conventional exercises for reducing depression symptoms, particularly in patients with HF. A small study (n = 16) examined effects of TC versus aerobic exercise in patients with HF and HFpEF, finding that TC was more effective in reducing depression symptoms 21.
The overall goal of this investigation was to compare TC, RB exercise, and TAU for changes in physical, cardiac, and psychological function. Associated with the primary aims of our investigation, we hypothesized that mild-to-moderate exercise practices including TC and RB would be more effective in improving physical and cardiac function compared with TAU but would not differ from each other. Associated with our secondary aim, we hypothesized that TC would be more effective than RB and TAU for reducing depressive symptoms.
METHODS
This study was approved by the VA San Diego Healthcare System (VASDHS) and University of California at San Diego (UCSD) Institutional Review Boards, and informed consent was obtained from all participants included in the study. All procedures performed were in accordance with the 1964 Helsinki declaration and its later amendments. Patients were recruited from VASDHS and UCSD Healthcare System (between 2010 – 2015). At baseline and immediately after the 16-wk intervention, physical and cardiac function, and depression symptoms were measured. This was a randomized trial and the study coordinator determined group allocation using computer generated randomization algorithms and was responsible for all patient correspondence such as group assignment and testing appointments. Recruitment, and assessment personnel were naïve to participant group assignment. Our original study protocol compared TC with health education. However, in response to NIH grant reviewers’ suggestions and discussions with the NIH granting agency the health education group was replaced with another mild exercise intervention, to examine whether TC practice went beyond conventional exercise for outcomes, including depression symptoms. We also included a treatment as usual control group in the study design as a comparator of the typical disease course, in the absence of these interventions.
PARTICIPANTS
Inclusion criteria were diagnosis with American Heart Association/ American College of Cardiology Classification Stage C symptomatic HF (both HFpEF and HFrEF) for at least 3 mo, clinically stable (not having been hospitalized for a 3-mo period), on stable doses of neurohormonal blocking agents and diuretics for at least 3 mo, no cardiac surgeries for at least 6 mo, not in an exercise program, ≥40 yr of age. Exclusion criteria included presence of a psychiatric diagnosis other than major depression including psychosis, bipolar disorder and practicing TC within the previous year.
ASSESSMENTS
The following assessments were administered pre- and post-intervention period. Six-minute walk-test was used to assess physical functional capacity. It is a reliable and reproducible method to assess the severity of heart failure in patients, having high predictive value 22. Patients were instructed to walk as far as possible within 6-min in a straight corridor. The task was performed in a 25-ft walkway, blocked off from foot-traffic. This method has been regularly used by our group for similar studies 17, 23. Research assistants blinded to the participant’s group assignment remained at one end of the hall recording the distance. Standardized encouragement was given at 3-min into the task, i.e. “you are doing good”; “you have 3 more minutes left”. Echocardiography was performed by blinded assessors at UCSD Medical Center. All pre- and post-intervention echocardiograms were quantitatively analyzed by the same physician, who was also blinded to group allocation. Briefly, pulsed doppler spectral recordings were obtained from 4 X 4-mm sample volume placed at the tips of the mitral leaflets and in the pulmonary vein and that were adjusted to yield the maximal amplitude velocity signals. Images were digitized to obtain endocardial contours and LV cavity areas at end systole from the apical 4- and 2-chamber views. This method has been shown to be a reliable method of assessing LV function and predicting mortality in patients with HF.24 Ejection fractions were derived from biplane apical (2- and 4-chamber) views with use of modified Simpson’s rule algorithm 25. Depression symptoms were assessed with the 21-item Beck Depression Inventory −1A (BDI), which is recommended for measurement of depression in patients with cardiovascular disease, with reliability and capacity to discriminate between depressed and non-depressed participants with broad applicability for research and clinical practice 26. Cronbach’s alpha = .86 for the current study.
GROUP INTERVENTIONS
The intervention groups were Yang-style Tai Chi Chuan-Short Form (first third), and RB training (based on the Center for Disease Control’s “Move” program). RB exercise was chosen as a comparison to TC due to the psychosocial and mild-to-moderate physical exertion level similarities. Both exercises can be led by an experienced instructor, performed in a group, and provided at medical care or senior centers with minimal equipment and thus easily disseminated. Participants attended TC or RB training twice/wk for 60 min/session for 16-wk. TC and RB participants were asked to practice at home for 10-20 min/day, on non-class days. Descriptions of TC and RB class content are provided (SDC1). The TC instructor is a certified holistic health practitioner with > 10 yr of experience teaching TC to chronically ill and older adults. The RB instructor has her master’s degree in nutrition and taught physical fitness for 10 yr. Both groups were asked to exercise at a perceived exertion rating of “moderate difficult”, according to the Borg scale 27. Classes for the 2 groups were held on different days of the week at different locations within the University to avoid cross-contamination. Written materials were provided to support home practice for both groups. All participants continued to receive usual care, including regular visits to their cardiologist, primary care physicians, and other health specialists. TAU participants did not receive an active intervention.
STATISTICAL ANALYSES
Analyses were performed using SPSS version 24 (IBM Corp). Skewed data distribution was determined by the Kolmogorov-Smirnov test. All continuous variables approximated a normal distribution with skewness and kurtosis < 1.0. Baseline differences between groups were examined using analysis of variance for continuously measured variables and χ2 statistics for non-continuous variables. Mixed-effects models were used to analyze the efficacy of TC compared with RB exercises and TAU over 16 wk of treatment 28. The analysis for each outcome consisted of a model that included treatment, time, and treatment × time interaction as fixed effects with a heterogeneous covariance matrix. Post hoc analyses were performed to make specific group comparisons with repeated measures ANCOVA using estimated mean imputation.
RESULTS
Of 135 individuals screened for eligibility (see Figure 1, flow diagram) 70 patients were enrolled into the study with a median age of 66 yr (range, 45 – 89 yr) and 89% were male. BDI scores averaged 10 ± 7.3 suggesting that the cohort’s scores were at the cut-off for clinically significant elevation of depression symptoms (> 10) 29. Participants were assigned to TC (n = 25), RB training (n = 22) or TAU groups (n = 23) (Table 1).
Figure 1:
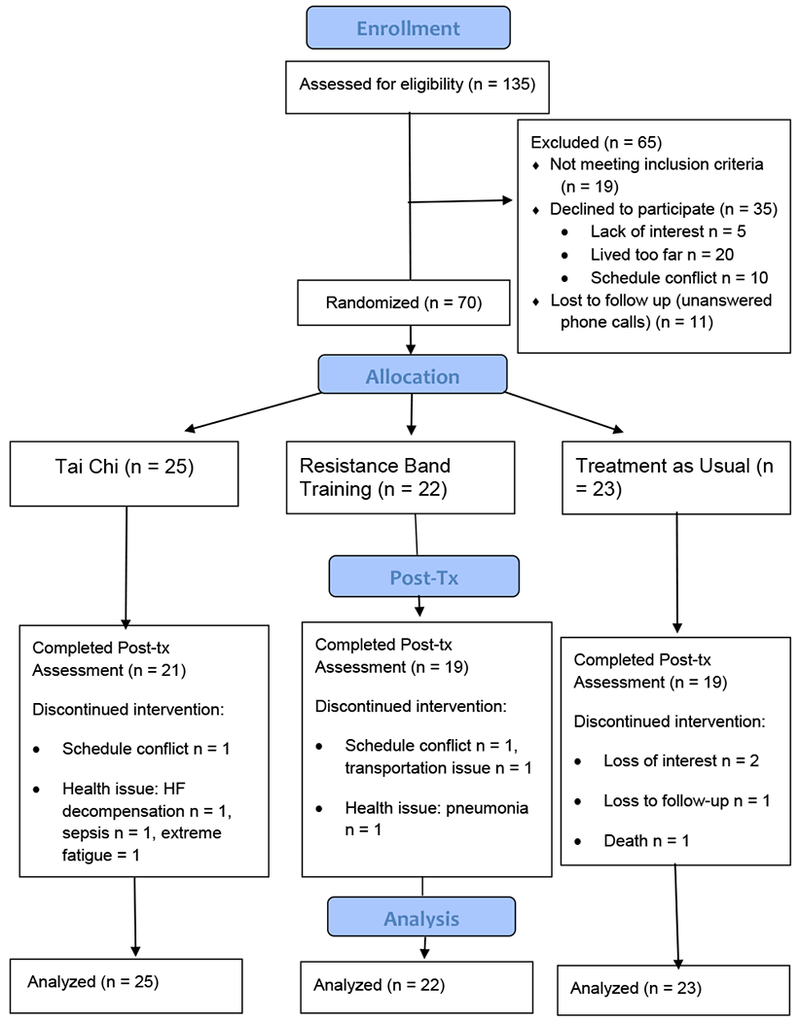
Participant Flow Diagram
Table 1.
Baseline Subject Characteristics
| Total | TC | RB | TAU | P value | |
|---|---|---|---|---|---|
| n | 70 | 25 | 22 | 23 | |
| Age, yr | 66 ± 10 | 63 ± 9 | 65 ± 9 | 67 ±7 | .52 |
| Sex, male | 89 | 92 | 86 | 87 | .81 |
| Race, white | 68 | 68 | 82 | 54 | .29 |
| LVEF | 46 ± 14 | 44 ± 13 | 46 ± 14 | 46 ± 12 | .85 |
| HFpEF, n | 43 | 44 | 45 | 37 | .79 |
| BMI, kg/m2 | 32 ± 8 | 32 ± 8 | 33 ± 8 | 31 ± 6 | .64 |
| Marital, married | 30 | 32 | 23 | 29 | .57 |
| 6MWT, ft | 943 ± 336 | 938 ± 359 | 875 ± 407 | 1011 ± 336 | .41 |
| BDI | 9 ± 7 | 10 ± 6 | 12 ± 8 | 8 ± 6 | .17 |
Abbreviations: BDI = Beck Depression Index; BMI = body mass index; HFpEF = heart failure with preserved ejection fraction; LVEF = left ventricular ejection fraction; 6MWT = six-minute walk test; RB, resistance band; tai chi; TAU; TC, treatment as usual.
Data are reported as mean ± SD or n (%).
Independent t-tests and Kruskal-Wallis tests were used to evaluate group differences.
TREATMENT FIDELITY AND ADHERENCE
Of 70 participants enrolled, 16% dropped out (TC: n = 4; RB: n = 3; TAU: n = 4) and 59 participants completed the study (n = 21, 19 and 19 respectively). There were no group differences in drop-out rates (P = .81). TC participants attended a median of 87% of classes (28 sessions), and practiced a median of 74 min/wk. Whereas, the RB group attended a median of 81% of classes (26 classes) and practiced a median of 61 min/wk. There were no differences between the two active intervention groups for class attendance (P = .76) or practice time outside of class (P = .86). There were no differences in age, sex, %LVEF, 6MWT, HFpEF or HFrEF sub-types, BDI, scores between those who dropped out from those who completed the study (P’s > .10). There were no serious adverse events associated with the study.
PHYSICAL AND CARDIAC FUNCTION
Fixed effect group differences from pre- to post-intervention period were found with a mixed model analysis, with 6MWT as the dependent variable (group x time interaction, F = 3.19, P = .03) (Figure 2). Estimated fixed effects revealed TAU significantly declined in distance walked by 205 ft [95% CI, −35 to −374, P = .02] and the RB group with a slight increase of 70 ft [95% CI, 267 to −127, P = .48] and TC trending for a significant decrease of 162 ft [95% CI, 21 to −345, P =.08]. Post hoc analyses revealed only RB and TAU group differences (η2= .087, P = .05). There were no differences between RB and TC (η2 = .023, P = .33), or between TC and TAU (η2 = .009, P = .51). Also, there were no fixed effect group differences over time in cardiac function measured with ESV (P = .43) and %LVEF (P = .67).
Figure 2.
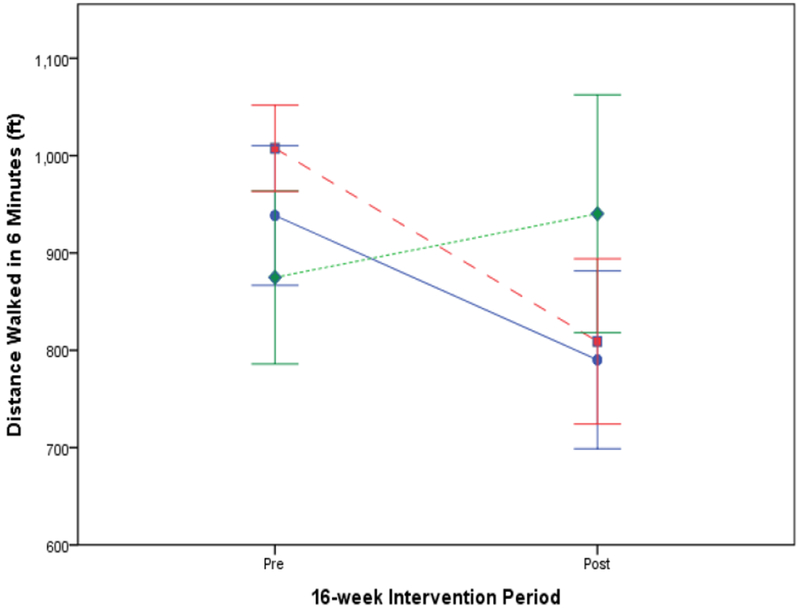
Changes in 6-min walk test (mean ± SE) from baseline to post-16-wk intervention period in patients with heart failure trained in tai chi (TC) (circles), resistance bands (RB) (diamonds) exercise or treatment as usual (TAU) controls (squares).
DEPRESSION SYMPTOMS
There were fixed effect group differences over time for BDI scores (group x time interaction, F = 9.2, P < .01) (Figure 3). Estimated fixed effects revealed a decrease in BDI scores by TC [95% CI, 2 - 5, P < .01] and RB groups [95% CI, 1 to 5, P < .01] of 3.5 points, while the TAU group decreased by 1 point [95% CI, −1 to 3] (P = .27). Post hoc analyses revealed both TC (η2 = .096, P = .039) and RB (η2 = .11, P = .034) groups differed from TAU over time. There were no differences between TC and RB (η2 = .014, P = .45).
Figure 3.
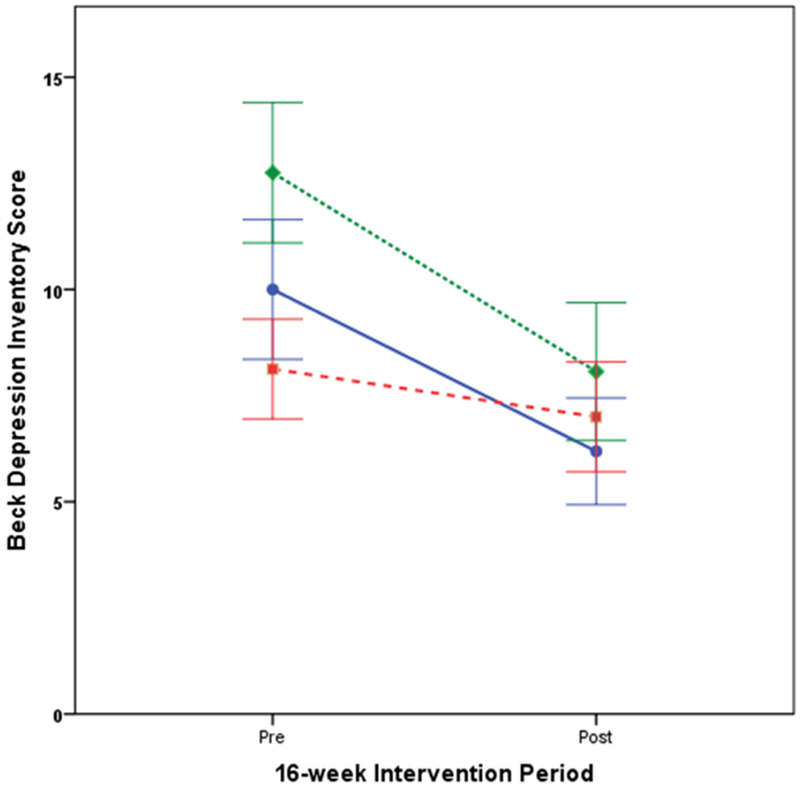
Changes in Beck Depression Inventory-IA scores (mean ± SE) from baseline to post-16-wk intervention period in patients with heart failure trained in tai chi (TC; circles), resistance band (RB; diamonds) exercise or treatment as usual (TAU; squares).
DISCUSSION
The present investigation sought to compare TC, RB exercise, and TAU for changes in physical, cardiac, and psychological function. Over the 16-wk study, attrition was 18% which was slightly better than the 20% drop-out rate that was predicted. There were no differences in drop-out rates among the 3 groups, and no differences between intervention groups in class attendance or practice times, with median class attendance > 80%, and reported median practice times of > 1 hr/wk. There were no serious adverse events associated with the study. The median age of the participants was 66 yr, an age group representative of most HF patients.
From our primary aims, we hypothesized that mild exercise practices including TC and RB would be more effective in improving physical and cardiac function compared with TAU but would not differ from each other. However, at the end of 16 wk we failed to see improvements from baseline in physical function, measured with the 6MWT by any of the groups. Instead, we found physical function did not decline in the TC and RB group, and that RB and TAU differed significantly from each other over time. This may suggest that RB can hamper HF related physical function decline. Our findings illustrate that the intensity and mode of exercise used in this study does not generate the level of effect on exercise capacity that has been seen in studies with higher intensity aerobic exercise 30. Our findings correspond with Yeh et al, (2011) whose study included 100 patients with HF and found no significant differences in change in 6MWT distance when comparing TC with a health education control group 31. Also, our results corresponded with the literature in that RB had better outcomes on the 6MWT then TAU controls 32. Of note, the RB group had a lower functional capacity (6MWT) at baseline (albeit not significantly lower) than TAU and TC, and thus the magnitude of improvement by the RB group may have been influenced by a lower baseline state.
Our hypothesis that TC and RB would improve cardiac function compared with TAU was also not supported, since there were no changes in %LVEF and ESV in any of the groups over time. This agrees with the literature suggesting that more vigorous exercise interventions have a greater likelihood of improving cardiovascular function 7. Our physical and cardiac function findings should be replicated due to the small sample size, but particularly regarding physical function which may be impacted by the older age of the participants and acute and chronic HF comorbidities (e.g. claudication, COPD, diabetic neuropathy) that can impact 6MWT results.
From our secondary aim, we hypothesized that TC would be more effective than RB and TAU for reducing depressive symptoms. This hypothesis was partially supported in that TC was superior to TAU for reducing depressive symptoms over time. This is consistent with our previously published work and findings from other investigators, observing that TC practice is associated with depression symptom reductions in patients with HF 17, 33. However, RB was also superior to TAU and did not differ from TC in reducing depressive symptoms. The present investigation extends prior research by including RB as a conventional exercise condition and suggests that various mild-to-moderate exercises can reduce symptoms of depression in patients with heart failure. These findings may be clinically relevant since elevated depression symptoms in cardiovascular diseases such as HF are related to greater risk of cardiovascular hospitalization and mortality 34, 35;36. More study is needed to determine the influence of exercising in groups on depression, since both interventions were group based.
A main limitation of the study includes a modest sample size resulting in limited statistical power. This precluded the inclusion of important covariates that may also influence physical and cardiac function, depression symptoms, and ultimately lessens the certainty of the findings presented. Also, because of the small sample-size we could not adequately address differences between HFpEF and HFrEF. However, both groups are known to experience reduced physical function 37 and depression 38. Therefore, the findings relating to physical function and depression are likely relevant to both groups. Other limitations include, lack of measures for range of motion and exercise progression. Also, we had a small number of women in our study, since most patients were recruited from the Veterans hospital. Additionally, it is unclear from patient records specifically how many were taking anti-depressants.
CONCLUSION
In sum, this study found that 2 different types of mild-to-moderate exercise training was associated with reduced depression symptoms and a potential reduction of functional decline. Importantly, patients were willing to come into a facility for group exercise when specifically recruited from cardiac clinics. Future research is needed to replicate and expand upon our findings to more fully understand the mechanisms by which mild-to-moderate exercise may reduce functional decline and depression symptoms.
Supplementary Material
Acknowledgments:
The protocol for the parent study can be found at clinicaltrial.gov Clinical Trial number: NCT01625819. ORCID#: 0000-0001-7633-2034
Funding: This research was supported by R01HL096784
Footnotes
Conflicts of interest: The authors declare no conflicts of interest.
References
- 1.Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Card Fail. 2017:23(8):628–651. [DOI] [PubMed] [Google Scholar]
- 2.Jiang W, Kuchibhatla M, Clary GL, et al. Relationship between depressive symptoms and long-term mortality in patients with heart failure. Am Heart J. 2007;154(1):102–108. [DOI] [PubMed] [Google Scholar]
- 3.Friedmann E, Thomas SA, Liu F, Morton PG, Chapa D, Gottlieb SS. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006;152(5):940 e941–948. [DOI] [PubMed] [Google Scholar]
- 4.Sherwood A, Blumenthal JA, Trivedi R, et al. Relationship of depression to death or hospitalization in patients with heart failure. Arch Intern Med. 2007;167(4):367–373. [DOI] [PubMed] [Google Scholar]
- 5.Thombs BD, de Jonge P, Coyne JC, et al. Depression screening and patient outcomes in cardiovascular care: a systematic review. JAMA. 2008;300(18):2161–2171. [DOI] [PubMed] [Google Scholar]
- 6.Bloom MW, Greenberg B, Jaarsma T, et al. Heart failure with reduced ejection fraction. Nat Rev Dis Primers. 2017;3:17058. [DOI] [PubMed] [Google Scholar]
- 7.Ismail H, McFarlane JR, Nojoumian AH, Dieberg G, Smart NA. Clinical outcomes and cardiovascular responses to different exercise training intensities in patients with heart failure: a systematic review and meta-analysis. JACC Heart Fail. 2013;1(6):514–522. [DOI] [PubMed] [Google Scholar]
- 8.Tu RH, Zeng ZY, Zhong GQ, et al. Effects of exercise training on depression in patients with heart failure: a systematic review and meta-analysis of randomized controlled trials. Eur J Heart Fail. 2014;16(7):749–757. [DOI] [PubMed] [Google Scholar]
- 9.Haykowsky MJ, Liang Y, Pechter D, Jones LW, McAlister FA, Clark AM. A meta-analysis of the effect of exercise training on left ventricular remodeling in heart failure patients: the benefit depends on the type of training performed. J Am Coll Cardiol. 2007;49(24):2329–2336. [DOI] [PubMed] [Google Scholar]
- 10.Blumenthal JA, Babyak MA, O’Connor C, et al. Effects of exercise training on depressive symptoms in patients with chronic heart failure: the HF-ACTION randomized trial. JAMA. 2012;308(5):465–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Connor CM, Whellan DJ, Lee KL, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301(14):1439–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Redfield MM, Jacobsen SJ, Burnett JC Jr., Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA. 2003;289(2):194–202. [DOI] [PubMed] [Google Scholar]
- 13.Bekfani T, Pellicori P, Morris DA, et al. Sarcopenia in patients with heart failure with preserved ejection fraction: Impact on muscle strength, exercise capacity and quality of life. Int J Cardiol. 2016;222:41–46. [DOI] [PubMed] [Google Scholar]
- 14.Ebner N, Jankowska EA, Ponikowski P, et al. The impact of iron deficiency and anaemia on exercise capacity and outcomes in patients with chronic heart failure. Results from the Studies Investigating Co-morbidities Aggravating Heart Failure. Int J Cardiol. 2016;205:6–12. [DOI] [PubMed] [Google Scholar]
- 15.Jolly K, Taylor R, Lip G, et al. The Birmingham Rehabilitation Uptake Maximisation Study (BRUM). Home-based compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence. Health Technol Assess. 2007;11(35):1–118. [DOI] [PubMed] [Google Scholar]
- 16.Stahrenberg R, Duvinage A, Mende M, et al. Determinants of submaximal exercise capacity in patients at risk for heart failure with preserved ejection fraction-results from the DIAST-CHF study. ESC Heart Fail. 2015;2(2):76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Redwine LS, Tsuang M, Rusiewicz A, et al. A pilot study exploring the effects of a 12-week t’ai chi intervention on somatic symptoms of depression in patients with heart failure. J Altern Complement Med. 2012;18(8):744–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang C, Collet JP, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic review. Arch Intern Med. 2004;164(5):493–501. [DOI] [PubMed] [Google Scholar]
- 19.Barrow D, Bedford A, Ives G, O’Toole L, Channer K. An evaluation of the effects of Tai Chi Chuan and Chi Kung training in patients with symptomatic heart failure: a randomised controlled pilot study. Postgrad Med J. 2007;83(985):717–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mandic S, Myers J, Selig SE, Levinger I. Resistance versus aerobic exercise training in chronic heart failure. Curr Heart Fail Rep. 2012;9(1):57–64. [DOI] [PubMed] [Google Scholar]
- 21.Yeh GY, Wood MJ, Wayne PM, et al. Tai chi in patients with heart failure with preserved ejection fraction. Congest Heart Fail. 2013 2013;19(2):77–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lipkin D, Scriven AJ, Crake T, Poole-Wilson PA. Six minute walking test for assessing exercise capacity in chronic heart failure. Br Med J (Clin Res Ed). 1986;292(6521):653–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mills PJ, Dimsdale JE, Natarajan L, Ziegler MG, Maisel A, Greenberg BH. Sleep and health-related quality of life in heart failure. Congest Heart Fail. 2009;15(5):228–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Feigenbaum H Three-dimensional ultrasonic imaging of blood flow. Eur Heart J. 1999;20(8):551–552. [DOI] [PubMed] [Google Scholar]
- 25.Schiller N, Acquatella H, Ports TA, Drew D, Goerke J, Ringertz H, Silverman NH, Brundage B, Botvinick EH, Boswell R, Carlsson E, Parmley WW. Left ventricular volume from paired biplane two-dimensional echocardiography. Circulation. 1979;60(3):547–555. [DOI] [PubMed] [Google Scholar]
- 26.Wang YP, Gorenstein C. Psychometric properties of the Beck Depression Inventory-II: a comprehensive review. Rev Bras Psiquiatr. 2013;35(4):416–431. [DOI] [PubMed] [Google Scholar]
- 27.Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 28.Gueorguieva R, Krystal JH. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the Archives of General Psychiatry. Arch Gen Psychiatry. 2004;61(3):310–317. [DOI] [PubMed] [Google Scholar]
- 29.Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67(3):588–597. [DOI] [PubMed] [Google Scholar]
- 30.Davies EJ, Moxham T, Rees K, et al. Exercise based rehabilitation for heart failure. Cochrane Database Syst Rev. 2010(4):Cd003331. [DOI] [PubMed] [Google Scholar]
- 31.Yeh GY, McCarthy EP, Wayne PM, et al. Tai chi exercise in patients with chronic heart failure: a randomized clinical trial. Arch Intern Med. 2011;171(8):750–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jewiss D, Ostman C, Smart NA. The effect of resistance training on clinical outcomes in heart failure: A systematic review and meta-analysis. Int J Cardiol. 2016;221:674–681. [DOI] [PubMed] [Google Scholar]
- 33.Yeh G, Wood MJ, Lorell BH, Stevenson LW, Eisenberg DM, Wayne PM, Goldberger AL, Davis RB, Phillips RS. Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med Sci. 2004;117(8):541–548. [DOI] [PubMed] [Google Scholar]
- 34.Rutledge T, Reis VA, Linke SE, Greenberg BH, Mills PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48(8):1527–1537. [DOI] [PubMed] [Google Scholar]
- 35.Johnson TJ, Basu S, Pisani BA, et al. Depression predicts repeated heart failure hospitalizations. J Card Fail. 2012;18(3):246–252. [DOI] [PubMed] [Google Scholar]
- 36.Kato N, Kinugawa K, Shiga T, et al. Depressive symptoms are common and associated with adverse clinical outcomes in heart failure with reduced and preserved ejection fraction. J Cardiol. 2012;60(1):23–30. [DOI] [PubMed] [Google Scholar]
- 37.Dhakal BP, Malhotra R, Murphy RM, et al. Mechanisms of exercise intolerance in heart failure with preserved ejection fraction: the role of abnormal peripheral oxygen extraction. Circ Heart Fail. 2015;8(2):286–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hamo CE, Heitner JF, Pfeffer MA, et al. Baseline distribution of participants with depression and impaired quality of life in the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist Trial. Circ Heart Fail. 2015;8(2):268–277. [DOI] [PubMed] [Google Scholar]
- 39.Karmali KN, Davies P, Taylor F, Beswick A, Martin N, Ebrahim S. Promoting patient uptake and adherence in cardiac rehabilitation. Cochrane Database Syst Rev. 2014(6):Cd007131. [DOI] [PubMed] [Google Scholar]
- 40.Balady GJ, Ades PA, Bittner VA, et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the american heart association. Circulation. 2011;124(25):2951–2960. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


