Abstract
Objectives:
To investigate whether adverse childhood experiences (ACEs) are important determinants of sexual debut and HIV testing.
Design:
Adolescents (age 10-16; N=2,089) from rural Malawi were interviewed in 2017-2018 for the baseline wave of a longitudinal study of childhood adversity and HIV risk.
Methods:
Respondents were interviewed in their local language. Surveys captured 13 lifetime childhood adversities (using the ACE – International Questionnaire); sexual debut; and previous HIV testing. We used multivariate regression models to test whether adversity, measured both cumulatively and separately, predicted HIV risk.
Results:
For each additional adversity, there was a significant rise in the odds of sexual debut (OR 1.13, CI 1.07-1.20) and HIV testing (OR 1.10, CI 1.04-1.16).
Conclusions:
Preventing HIV among all young people necessitates a paradigm shift that recognizes the importance of early life social determinants in structuring HIV risk.
Keywords: HIV, adolescents, childhood adversity, HIV testing, sexual debut
Introduction
Almost two million adolescents (defined by the UN as 10-19 years) were living with HIV in 2015, a quarter million of whom were newly infected [1]. Without new approaches to prevention, the number of adolescents living with HIV is predicted to grow [1]. Greater attention to structural determinants – such as childhood adversity – may be one way to reverse the trend.
Adverse childhood experiences (ACEs) are potentially important determinants of HIV risk [2]. Evidence now links ACEs to early sexual debut, risky sexual behavior, and sexually transmitted infections (STI) [3-5]. Moreover, their influence can be powerful: globally, adults with four or more ACEs have on average a six-fold increase in the odds of an STI [6].
Few studies have measured ACEs in HIV-endemic countries. The key exceptions suggest ACEs influence subsequent HIV risk [7-11]. For example, a recent study from Malawi suggests that there is a dose-response relationship between cumulative adversity and both infrequent condom use and having multiple sexual partners among youth aged 19-24 [11]. Moreover, a study in South Africa suggests that ACEs begin to negatively impact these sexual behaviors as early as adolescence [10]. Despite these recent studies, research on adversity and HIV risk remains scarce - particularly in low-income counties (LICs) where childhood adversity is likely to be common. Moreover, there have been no studies looking at how adversity impacts HIV testing, an integral part of an HIV prevention package [12, 13]. As the first step on the HIV care cascade, HIV testing is also necessary to link HIV-positive adolescents to lifesaving treatment.
Our study investigates whether individual and cumulative ACEs are associated with sexual debut and HIV testing among adolescents in Malawi. We extend previous work by focusing on a younger developmental period (early adolescence, defined as 10-14 [14]), and by considering the impact of a wide range of ACEs on both a preventive behavior (HIV testing) and an HIV risk factor (early sexual debut).
Methods
Sample and data collection:
This study builds on the Malawi Longitudinal Study of Families and Health (MLSFH, est. 1998) [15], a longitudinal cohort from three rural districts (Mchinji, Balaka, and Rumphi). In each MLSFH household, we interviewed adolescent members age 10-16 (N=2,089) and their primary caregiver. Face-to-face interviews took place at their home and in their local language (Chewa, Yao or Tumbuka) during 2017-2018. Further detail on the sample and response rate (99%) are reported elsewhere [16]. IRB approval was obtained from Stony Brook University and the National Health Science Research Committee in Malawi.
Measures:
Lifetime adversity was measured using a standardized instrument developed by the WHO [17]. The Adverse Childhood Experiences – International Questionnaire (ACE-IQ) captures a broad array of 13 individual, family, peer and community experiences (see Table 1), and has shown good psychometric properties among Malawian adolescents [18]. We used a binary coding measure: any affirmative answer (regardless of frequency) was coded as exposure that type of ACE. ACEs were considered both separately and as part of a cumulative measure; the latter was operationalized by summing the number of adversities reported (ranging from 0-13).
Table 1.
Prevalence and adjusted relative odds of HIV-related behaviors by reported adverse childhood experience among adolescents in Malawi aged 10-16 (N=2085)
| Adverse Childhood Experiences | Sexual Debut | HIV testing | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| mean | SD | n | % | Model 1 aOR (95% CI) |
n | % | Model 1 aOR (95% CI) |
||||
| Cumulative ACEs | |||||||||||
| Continuous score (0-13) | 5.12 | 2.35 | 1.13 (1.07-1.20) | 1.10 (1.04-1.16) | |||||||
| n | % | n | % | Model 2 aOR (95% CI) |
Model 3 aOR (95% CI) |
n | % | Model 2 aOR (95% CI) |
Model 3 aOR (95% CI) |
Model 4 aOR (95% CI) |
|
| Individual Abuse & Neglect | |||||||||||
| Emotional neglect | 1792 | 86 | 421 | 24 | 1.56 (1.02-2.36) | 1.27 (0.83-1.95) | 360 | 20 | 1.30 (0.92-1.82) | 1.11 (0.78-1.57) | 1.11 (0.78-1.57) |
| Emotional abuse | 1105 | 53 | 283 | 26 | 1.07 (0.83-1.38) | 0.67 (0.49-0.92) | 209 | 19 | 1.12 (0.87-1.43) | 0.79 (0.58-1.06) | 0.79 (0.58-1.06) |
| Physical neglect | 677 | 32 | 160 | 24 | 1.44 (1.11-1.87) | 1.08 (0.80-1.45) | 146 | 22 | 1.16 (0.91-1.48) | 0.90 (0.68-1.20) | 0.90 (0.68-1.20) |
| Physical abuse | 1110 | 53 | 254 | 23 | 1.09 (0.86-1.39) | 0.74 (0.56-0.98) | 194 | 17 | 0.82 (0.65-1.03) | 0.55 (0.42-0.72) | 0.55 (0.42-0.72) |
| Sexual abuse | 136 | 7 | 69 | 51 | 4.21 (2.74-6.48) | 3.44 (2.15-5.48) | 42 | 31 | 1.51 (1.02-2.22) | 1.12 (0.73-1.72) | 1.12 (0.73-1.72) |
| Family Dysfunction | |||||||||||
| Substance abuser in household | 467 | 22 | 122 | 26 | 1.28 (0.97-1.68) | 0.92 (0.67-1.27) | 115 | 25 | 1.62 (1.23-2.11) | 1.37 (1.01-1.86) | 1.37 (1.01-1.86) |
| Someone in the household with mental health issues | 137 | 7 | 33 | 24 | 1.29 (0.82-2.02) | 0.91 (0.56-1.47) | 38 | 28 | 1.48 (0.99-2.22) | 1.18 (0.77-1.79) | 1.18 (0.77-1.79) |
| Incarcerated household member | 269 | 13 | 71 | 26 | 1.08 (0.77-1.52) | 0.76 (0.53-1.10) | 75 | 28 | 1.79 (1.29-2.48) | 1.51 (1.06-2.14) | 1.50 (1.05-2.13) |
| Domestic violence | 1231 | 59 | 291 | 24 | 1.28 (1.00-1.63) | 0.83 (0.61-1.13) | 248 | 20 | 1.15 (0.91-1.46) | 0.80 (0.58-1.09) | 0.80 (0.58-1.09) |
| Parents dead or divorced | 1057 | 51 | 266 | 25 | 1.30 (1.02-1.65) | 1.01 (0.77-1.33) | 237 | 22 | 1.43 (1.12-1.81) | 1.24 (0.96-1.60) | 1.24 (0.96-1.60) |
| Peer | |||||||||||
| Bullied | 654 | 31 | 188 | 29 | 1.62 (1.26-2.07) | 1.23 (0.92-1.65) | 141 | 22 | 1.25 (0.97-1.60) | 0.93 (0.68-1.26) | 0.93 (0.68-1.26) |
| Community | |||||||||||
| Community violence | 1842 | 88 | 439 | 24 | 1.77 (1.04-3.00) | 1.30 (0.76-2.23) | 374 | 20 | 1.59 (1.06-2.39) | 1.28 (0.84-1.96) | 1.28 (0.84-1.96) |
| Collective violence | 186 | 9 | 65 | 35 | 1.68 (1.15-2.47) | 1.22 (0.82-1.83) | 48 | 26 | 1.67 (1.17-2.40) | 1.30 (0.88-1.93) | 1.30 (0.88-1.93) |
Note: Models 1-4 control for age, gender, SES and region. Model 2 runs separate multivariate logistic regressions for each type of adversity. Model 3 builds off Model 2 but with an additional control for the continuous ACE score. Model 4 further controls for sexual debut. Bolded values represent those that are statistically significant (<0.05).
Early sexual debut is a consistent indicator of HIV risk [19]. Debut was defined by the question “Have you ever had sexual intercourse? By sexual intercourse I mean penetrative vaginal sex.” Given that our sample was 10-16, there was no need to further differentiate by age of debut. HIV testing is a protective behaviour [12, 13]. Adolescents reported their lifetime history of HIV testing; we treated this as a dichotomous outcome.
Finally, we measured age (continuous), gender, quintile of socioeconomic status (SES, reported by the caregiver), and home district.
Analyses:
Data to test the hypothesized association between adversity and HIV risk were available from 2,085 adolescents. We described the sample characteristics and modelled their association with cumulative adversity using linear regression. We used logistic regression to examine the dose-response relationship between cumulative adversity and both sexual debut and HIV testing (Model 1 in Table 1). In a second set of analyses, we examined whether specific types of adversity predicted HIV risk, running separate logistic regressions for each type of adversity (Model 2). However, focusing on one type of adversity fails to account for the clustering of adversity, and may overestimate the impact of that risk factor. To identify specific types of adversity that have a unique influence on health, we need to take these other adversities into account [20]. Thus in the third set of analyses, we continued to examine separate adversities, but additionally adjusted for the cumulative ACE score (Model 3). Finally, to investigate if sexual debut mediated the association between adversity and HIV testing, we re-estimated the specification in Model 3 controlling for sexual debut (Model 4). All models controlled for age, gender, SES, and district; standard errors were adjusted for household clustering. Analyses were run using Stata v13.
Results
As reported elsewhere [16], adolescents experienced an average of 5 (of 13) ACEs. The sample was 13.25 years old on average, and age had a positive association with cumulative adversity (beta 0.08, 95% CI 0.03-0.14). Females (49%) reported lower cumulative adversity (beta −0.25, CI −0.45, −0.05). SES quintile was not significantly associated with adversity. Emotional neglect was the most commonly reported adversity (86%); sexual abuse was the least (7%, Table 1).
Prevalence of sexual debut and HIV testing during early adolescence
One fifth of the sample had sexually debuted (27% of boys, 16% of girls). Similarly, one fifth reported a previous HIV test, with no difference by gender.
Relative odds of sexual debut and HIV testing by cumulative adversity
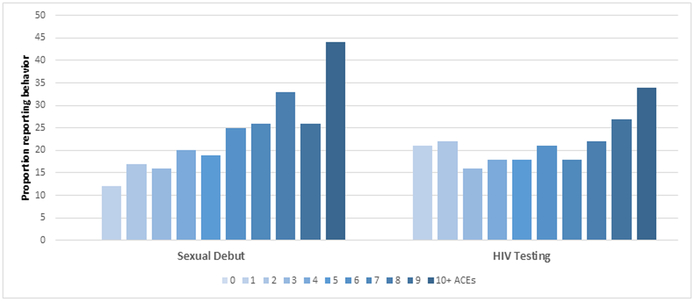
There was a clear gradient between adversity and risk behavior (see Figure 1). In adjusted analyses, each additional adversity was associated with a significant rise in the odds of sexual debut (adjusted OR (aOR) 1.13, CI 1.07-1.20; Table 1, Model 1). Cumulative adversity similarly demonstrated a significant association with HIV testing (aOR 1.10, CI 1.04-1.16).
Figure 1.
Prevalence of sexual debut and HIV testing by ACE score among adolescents in Malawi aged 10-16 (N=2085)
Relative odds of sexual debut and HIV testing by type of adversity
Eight of the 13 types of adversity were significantly associated with sexual debut (Table 1, Model 2). Sexual abuse demonstrated the strongest association (aOR 4.21, CI 2.74-6.48). Sexual debut was reported by over half (51%) of adolescents who experienced sexual abuse, compared to 20% of adolescents who did not experience sexual abuse. We also tested whether separate adversities retained an independent association with sexual debut after controlling for cumulative adversity (Model 3). Sexual abuse was the only type of adversity to retain a strong positive association with sexual debut (aOR 3.44, CI 2.15-5.48).
Five of the 13 adversities were associated with HIV testing. Two (a household member experiencing either substance abuse or incarceration) remained as significant positive associations after controlling for cumulative adversity. Physical abuse had a significant negative association with HIV testing after controlling for cumulative adversity. Finally, adding a control for sexual debut did not noticeably change the odds associated with HIV testing (Model 4).
Discussion
We find that early sexual debut is more likely among adolescents who have already experienced substantial adversity in their young lives. This is consistent with the literature on adversity and sexual behavior in high-income contexts, and adds weight to the emerging literature in lower-resource contexts [9-11]. Moreover, research has shown that children growing up in difficult circumstance are exposed to multiple, overlapping adversities [20], and that they often influence outcomes through a common causal chain [21, 22]. We too find that cumulative adversity demonstrates a clear risk gradient, as expected.
In the context of HIV epidemic, however, most studies have focused only on a single type of adversity (e.g., orphanhood [23, 24]). This study therefore examined whether single adversities have a unique influence on sexual debut. At first glance, eight of the thirteen types of adversity appear related to sexual debut. When adjusting for cumulative adversity, however, only one type of adversity emerges as a significant independent predictor: sexual abuse. This broadly suggests that focusing on one type of adversity can overestimate its impact; in many cases, the observed association may instead be due to the accumulation of non-specific ACEs.
Our findings suggest that sexual violence may be an exception. In a South African study, sexual abuse was associated with much larger effect sizes across most HIV risk factors (e.g., number of partners) when compared to emotional or physical abuse [9]. Among adults in the Philippines, sexual abuse was the strongest (and one of the only) independent predictors of early sexual debut [25]. However, other studies – such as the previously mentioned study of youth in Malawi [11] – have not observed a distinct association between sexual violence and HIV risk (condom use or multiple partners).
Longitudinal studies are needed to assess whether sexual abuse is indeed a unique, powerful determinant of sexual risk. If so, interventions that tackle sexual abuse should be prioritized. The THRIVE strategies, developed by the WHO, offer a starting point for reducing both sexual abuse and other forms of child maltreatment [26]. These seven evidence-based strategies range from the national-level (e.g., laws criminalizing sexual abuse), to the household-level (parenting programs), to the individual-level (cash-transfers). The next step is adaption and evaluation of these approaches in LICs.
We also found that adolescents with a history of adversity were more likely to report HIV testing, which is somewhat surprising. We could find only one other study examining ACEs and HIV testing: in three Africa countries, adults who had experienced child abuse were more likely to have taken an HIV test [27]. One potential explanation is that individuals who experience a large burden of adversity tend to have higher self-perceived HIV risk [4]; this in turn may motivate HIV testing [28, 29]. Clearly, more work needs to be done to understand what is motivating HIV testing, as this may provide important insights on how we can increase HIV testing rates among adolescents.
Strengths of this study include use of a standardized instrument to measure a range of ACEs, a large community sample, and a focus on adolescents. Studies of adversity and sexual debut in adult populations rely on retrospective recall, and there is evidence of substantial bias in the reporting of adversity [30]. Among adolescents, we can more accurately capture ACEs, early sexual initiation, and HIV testing – though this approach does not fully eliminate recall bias or allow for temporal ordering. The cross-sectional nature of the data are a limitation, however we note that similar associations between cumulative ACEs and risky sexual behavior have been reported in prospective trials [e.g., 10, 31]. The cross-sectional nature is particularly limiting in exploring the relationship between sexual abuse and sexual debut. Early sexual debut is not always voluntary: a prior study in Malawi found that 38% of girls (age 12-19) reported that their first sexual experience was coerced or forced [32]. Longitudinal data is needed to better characterize the above relationships (and are forthcoming as part of this project).
Acknowledgements:
The authors thank the staff (field supervisors, interviewers, counselors, and many others) at Invest in Knowledge International for their time, effort, and support of this project. In particular, we thank James Mwera for his oversight of the extensive data collection. Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R01HD090988. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Both authors participated in the concept and design of the paper. Kidman led the analysis and drafted the paper. Kohler collaborated on the interpretation of data and refinement of the manuscript.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest.
References
- 1.UNICEF. For every child, end AIDS–seventh stocktaking report. New York, NY: UNICEF; 2016. [Google Scholar]
- 2.Brown DW, Anda RF. Adverse childhood experiences: origins of behaviors that sustain the HIV epidemic. AIDS 2009; 23(16):2231–2233. [DOI] [PubMed] [Google Scholar]
- 3.Felitti Md FVJ, Anda Md MSRF, Nordenberg Md D, Williamson Ms PDF, Spitz Ms MPHAM, Edwards Ba V, et al. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine 1998; 14(4):245–258. [DOI] [PubMed] [Google Scholar]
- 4.Hillis SD, Anda RF, Felitti VJ, Marchbanks PA. Adverse childhood experiences and sexual risk behaviors in women: a retrospective cohort study. Family planning perspectives 2001:206–211. [PubMed] [Google Scholar]
- 5.Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Preventive Medicine 2003; 37(3):268–277. [DOI] [PubMed] [Google Scholar]
- 6.Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health 2017; 2(8):e356–e366. [DOI] [PubMed] [Google Scholar]
- 7.Jewkes RK, Dunkle K, Nduna M, Jama PN, Puren A. Associations between childhood adversity and depression, substance abuse and HIV and HSV2 incident infections in rural South African youth. Child Abuse & Neglect 2010; 34(11):833–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pence BW, Shirey K, Whetten K, Agala B, Itemba D, Adams J, et al. Prevalence of Psychological Trauma and Association with Current Health and Functioning in a Sample of HIV-infected and HIV-uninfected Tanzanian Adults. PloS one 2012; 7(5):e36304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gibbs A, Dunkle K, Washington L, Willan S, Shai N, Jewkes R. Childhood traumas as a risk factor for HIV-risk behaviours amongst young women and men living in urban informal settlements in South Africa: A cross-sectional study. PloS one 2018; 13(4):e0195369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meinck F, Orkin F, Cluver L. Does free schooling affect pathways from adverse childhood experiences via mental health distress to HIV risk among adolescent girls in South Africa: a longitudinal moderated pathway model. Journal of the International AIDS Society 2019; 22(3):e25262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.VanderEnde K, Chiang L, Mercy J, Shawa M, Hamela J, Maksud N, et al. Adverse childhood experiences and HIV sexual risk-taking behaviors among young adults in malawi. Journal of interpersonal violence 2018; 33(11):1710–1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Denison JA, O’Reilly KR, Schmid GP, Kennedy CE, Sweat MD. HIV Voluntary Counseling and Testing and Behavioral Risk Reduction in Developing Countries: A Meta-analysis, 1990–2005. AIDS Behav 2008; 12(3):363–373. [DOI] [PubMed] [Google Scholar]
- 13.Fonner VA, Denison J, Kennedy CE, O’Reilly K, Sweat M. Voluntary counseling and testing (VCT) for changing HIV-related risk behavior in developing countries. The Cochrane database of systematic reviews 2012; 9(9):CD001224–CD001224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.UN Children’s Fund (UNICEF). Adolescence, an Age of Opportunity: The State of the World’s Children 2011. In. New York: UNICEF; 2011. [Google Scholar]
- 15.Kohler H-P, Watkins SC, Behrman JR, Anglewicz P, Kohler IV, Thornton RL, et al. Cohort Profile: The Malawi Longitudinal Study of Families and Health (MLSFH). International Journal of Epidemiology 2014:dyu049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kidman R, Piccolo LR, Kohler HP. Adverse Childhood Experiences: Prevalence and Association with Adolescent Health in Malawi. AJPM under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. Adverse Childhood Experiences International Questionnaire (ACE-IQ) In. Geneva. [Google Scholar]
- 18.Kidman R, Smith D, Piccolo LR, Kohler H-P. Psychometric evaluation of the Adversity Childhood Experience International Questionnaire (ACE-IQ) in Malawian adolescents. Child Abuse & Neglect 2019; 92:139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stöckl H, Kalra N, Jacobi J, Watts C. Is Early Sexual Debut a Risk Factor for HIV Infection Among Women in Sub-Saharan Africa? A Systematic Review. American Journal of Reproductive Immunology 2013; 69:27–40. [DOI] [PubMed] [Google Scholar]
- 20.Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, et al. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child abuse & neglect 2004; 28(7):771–784. [DOI] [PubMed] [Google Scholar]
- 21.Hatch SL. Conceptualizing and Identifying Cumulative Adversity and Protective Resources: Implications for Understanding Health Inequalities. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences 2005; 60(Special Issue 2):S130–S134. [DOI] [PubMed] [Google Scholar]
- 22.Anda RF, Butchart A, Felitti VJ, Brown DW. Building a framework for global surveillance of the public health implications of adverse childhood experiences. American journal of preventive medicine 2010; 39(1):93–98. [DOI] [PubMed] [Google Scholar]
- 23.Operario D, Underhill K, Chuong C, Cluver L. HIV infection and sexual risk behaviour among youth who have experienced orphanhood: systematic review and meta-analysis. Journal of the International AIDS Society 2011; 14(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palermo T, Peterman A. Are Female Orphans at Risk for Early Marriage, Early Sexual Debut, and Teen Pregnancy? Evidence from Sub-Saharan Africa. Studies in Family Planning 2009; 40(2):101–112. [DOI] [PubMed] [Google Scholar]
- 25.Ramiro LS, Madrid BJ, Brown DW. Adverse childhood experiences (ACE) and health-risk behaviors among adults in a developing country setting. Child Abuse & Neglect 2010; 34(11):842–855. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. INSPIRE: seven strategies for ending violence against children. In. Geneva: World Health Organization; 2016. [Google Scholar]
- 27.Richter L, Komárek A, Desmond C, Celentano D, Morin S, Sweat M, et al. Reported Physical and Sexual Abuse in Childhood and Adult HIV Risk Behaviour in Three African Countries: Findings from Project Accept (HPTN-043). AIDS Behav 2014; 18(2):381–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Musheke M, Ntalasha H, Gari S, Mckenzie O, Bond V, Martin-Hilber A, et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in Sub-Saharan Africa. BMC Public Health 2013; 13(1):220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.deGraft-Johnson J, Paz-Soldan V, Kasote A, Tsui A. HIV Voluntary Counseling and Testing Service Preferences in a Rural Malawi Population. AIDS Behav 2005; 9(4):475–484. [DOI] [PubMed] [Google Scholar]
- 30.Naicker SN, Norris SA, Mabaso M, Richter LM. An analysis of retrospective and repeat prospective reports of adverse childhood experiences from the South African Birth to Twenty Plus cohort. PloS one 2017; 12(7):e0181522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilson HW, Widom CS. An examination of risky sexual behavior and HIV in victims of child abuse and neglect: a 30-year follow-up. Health Psychology 2008; 27(2):149. [DOI] [PubMed] [Google Scholar]
- 32.Moore AM, Awusabo-Asare K, Madise N, John-Langba J, Kumi-Kyereme A. Coerced first sex among adolescent girls in sub-Saharan Africa: prevalence and context. African journal of reproductive health 2007; 11(3):62–82. [PMC free article] [PubMed] [Google Scholar]