Abstract
A 73-year-old-male patient with hypertension and grade 3B chronic kidney disease underwent radical nephrectomy in the year 2000. As the renal function gradually worsened, the patient was started on hemodialysis in 2003. Eleven years after nephrectomy, the metastases were pointed out. The patient received sunitinib as first-line therapy. Thereafter, as the metastatic lesions became larger, we initiated nivolumab therapy (3 mg/m2 every 2 weeks). After 52 weeks, the metastatic lesions continued showing complete response (CR). No adverse effects were observed during nivolumab treatment.
Introduction
Immune checkpoint inhibitors (ICI) have shown survival benefits in patients with metastatic renal cell cancer (RCC). Nivolumab is a monoclonal antibody that targets programmed cell death-1 and has been approved for the treatment of mRCC after the failure of tyrosine kinase inhibitors (TKIs) based on the results of a phase III trial.1 However, patients on dialysis were excluded from this pivotal trial, and there is very limited evidence on the efficacy and tolerability of nivolumab in patients with renal impairment. We report a case of complete response to nivolumab in an mRCC patient undergoing hemodialysis, and also describe the pharmacokinetic profile of ICI during dialysis.
Case presentation
A 73-year-old-male patient with hypertension and grade 3B chronic kidney disease underwent radical nephrectomy in the year 2000. Pathological diagnosis revealed the case to be clear cell carcinoma (pT1a, G2>G1). As the renal function gradually worsened, the patient was started on hemodialysis in 2003. Eleven years after nephrectomy, metastasis to the psoas muscle and multiple lung and axillary lymph nodes were diagnosed. The patient received sunitinib as first-line therapy. After 48 months of sunitinib, metastatic legions were enlarged and new lung lesions appeared. Therefore, he was switched to axitinib as the second-line therapy for 34 months. Thereafter, as the metastatic lesions became larger, we initiated nivolumab therapy (3 mg/m2 every 2 weeks) (Fig. 1). Computed tomography (CT) scans at 12 weeks after initiating nivolumab therapy showed reduced metastatic lesions. After 36 weeks, all metastatic lesions disappeared (Fig. 2). After 52 weeks, the metastatic lesions continued showing complete response (CR) (Fig. 3). No adverse effects were observed during nivolumab treatment.
Fig. 1.
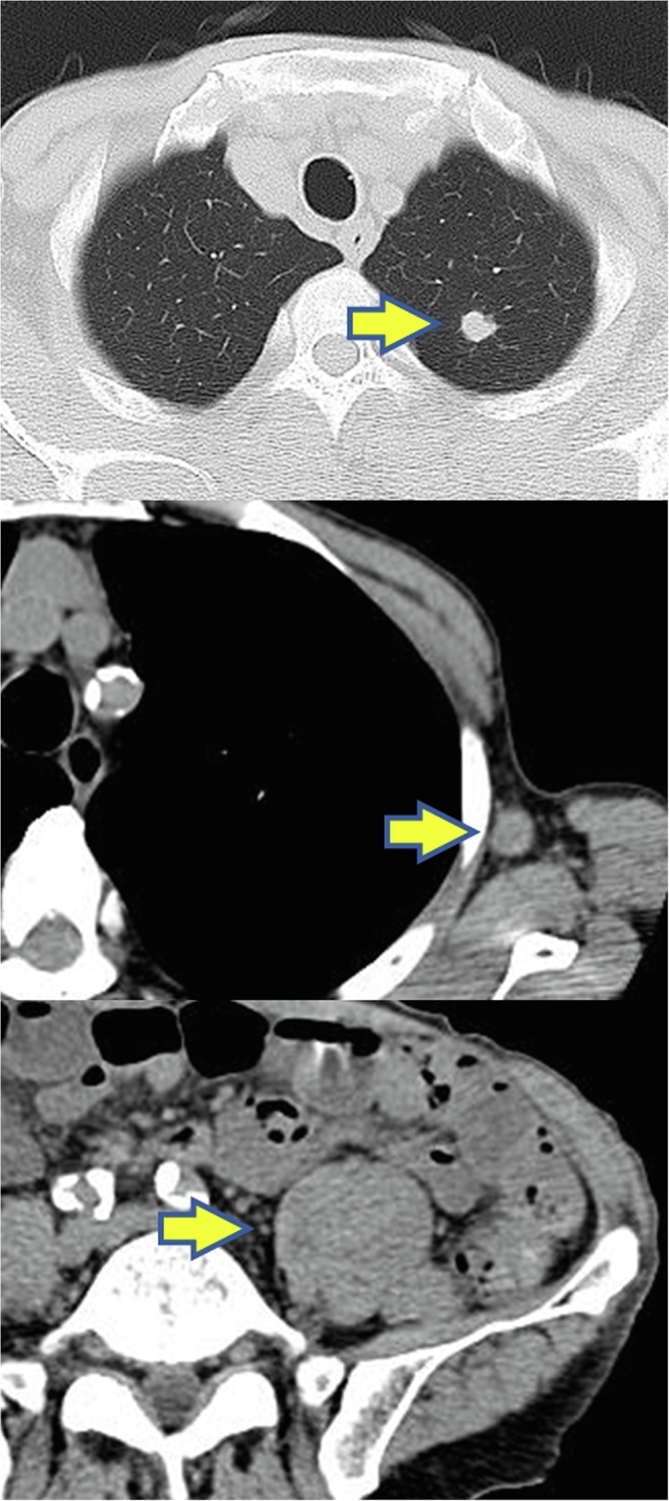
Before treatment of nivolumab.
Fig. 2.
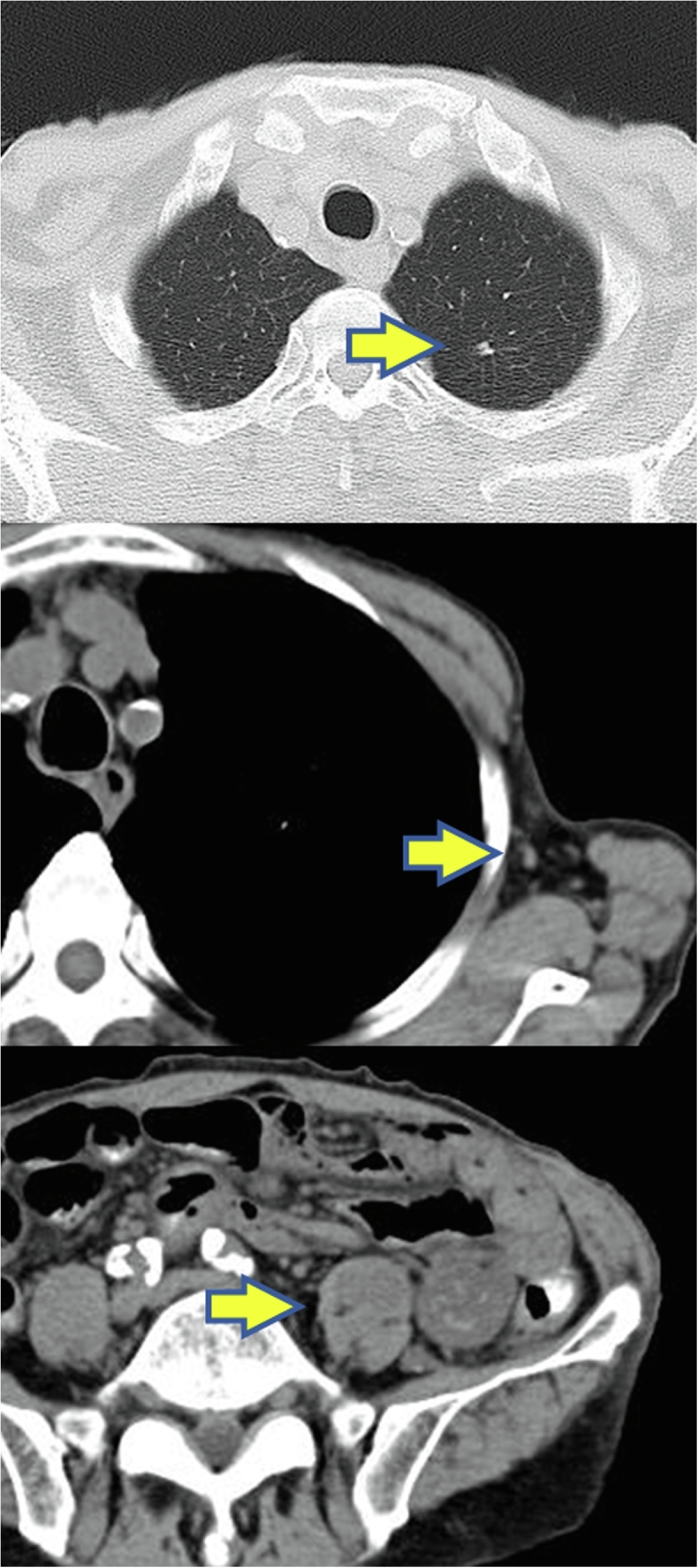
36 weeks after nivolumab. All metastatic lesions showed disappearance.
Fig. 3.
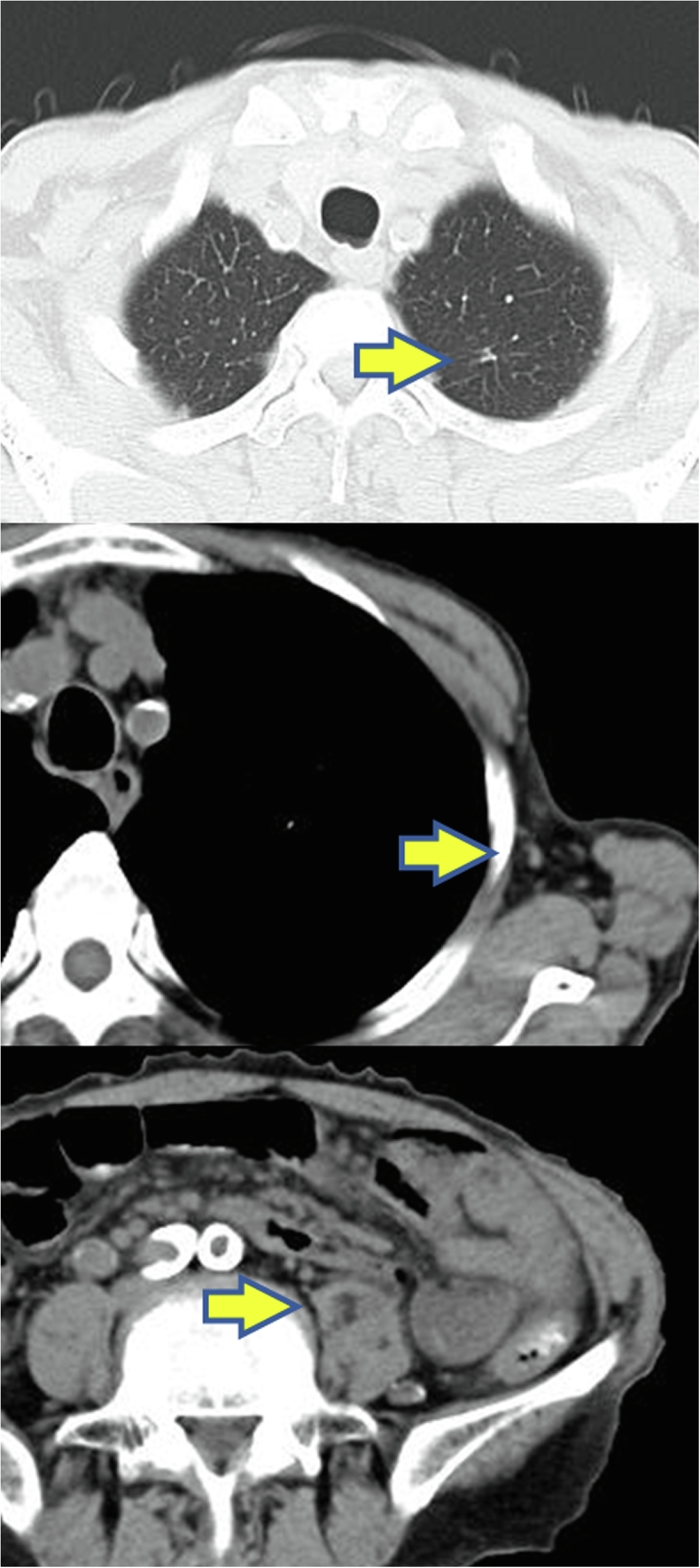
52 weeks after nivolumab. The metastasis lesion continues disappearing.
Discussion
The pivotal study using nivolumab demonstrated clinical efficacy, as well as good tolerability. However, the inclusion criteria for the study specified a serum creatinine level of ≤1.5 × upper normal limit and a creatinine clearance of ≥40 mL/min, thereby excluding patients with moderate-to-severe renal impairment. Therefore, the efficacy and safety of nivolumab in patients on dialysis have not been established. Some reports have described nivolumab treatment for mRCC in patients with end-stage renal disease (ESRD).2,3 Most recently, Tachibana et al. reported the safety and efficacy of nivolumab in mRCC in seven patients with end-stage renal disease.4 One patient experienced a partial response and the objective response rate was 16.7%. They concluded that nivolumab therapy in for mRCC patients with ESRD might be a useful option for selected patients. To the best of our knowledge, this is the first report demonstrating complete response following nivolumab therapy after failure of TKIs in mRCC patients undergoing hemodialysis.
Patients with ESRD are often excluded from many clinical trials because of their altered pharmacokinetic state and comorbidities. With regard to vascular endothelial growth factor receptor TKIs and mTOR inhibitors, there is some evidence to suggest that mRCC patients on dialysis treated with these agents have similar outcomes in terms of both efficacy and safety as compared to those with normal or minimally impaired kidney functions. On the other hand, nivolumab is excreted after getting disintegrated in vivo by peptide and an amino acid. From the pharmacokinetic perspective, we consider that renal function does not affect the metabolism of nivolumab, and dose reduction is not necessary even in patients undergoing hemodialysis. In addition, nivolumab is a high-molecular-weight immunoglobulin G4 protein that is not cleared by hemodialysis. Kanz et al. reported that decompensated heart failure develops after using an anti-PD-1 antibody in patients with cardiac dysfunction (left ventricular ejection fraction of ≤45%).5 As patients undergoing hemodialysis often have cardiac dysfunctions, we carefully need to monitor these patients on anti-PD-1 therapy. The accumulation of pharmacokinetic data from these patients on ICI therapy will be necessary for the future.
Conclusion
We reported the case of a patient with mRCC patient on hemodialysis who was benefited from nivolumab. We consider that mRCC patients undergoing hemodialysis might be administered nivolumab following a standard protocol similar to that in patients with normal renal functions.
Consent
Written consent was obtained from the patient for this case report.
Declaration of competing interest
None.
Acknowledgments
The authors thank the patient for allowing us to publish this report.
References
- 1.Motzer R.J., Escudier B., McDermott D.F. Nivolumab versus everolimus in advanced renal-cell carcinoma. N Engl J Med. 2015;373:1803–1813. doi: 10.1056/NEJMoa1510665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carlo Maria I., Feldman Darren R. Response to nivolmab in a patient with metastatic clear cell renal cell carcinoma and end-stage renal disease on dialysis. Eur Urol. 2016;70:1082–1085. doi: 10.1016/j.eururo.2016.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ansari Jawaher, Ali Muhammnad, Farrag Asraf, Ali Arwa M., Alhamad Abdulaziz. Efficacy of nivolmab in a patient with metastatic renal cell carcinoma and end-stage renal disease on dialysis: case report and literature review. Case Reports in Immunology. 2018:4. doi: 10.1155/2018/1623957. Article ID 1623957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tachibana H., Kondo T., Ishihara H., Takagi T., Tanabe K. Safety and efficacy of nivolumab in patients with metastatic renal cell carcinoma and end-stage renal disease at 2 centers. Clin Genitourin Cancer. 2019;17:772–778. doi: 10.1016/j.clgc.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 5.Kanz Bridgette A., Pllack Megan H., Johnpulle Romany, Puzanov Igor, Horn Leora. Safety and efficacy of anti-PD-1 in patients with baseline cardiac, renal, or hepatic dysfunction. Journal for ImunnoTherapy of cancer. 2016;4:60. doi: 10.1186/s40425-016-0166-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


