Abstract
Renal actinomycosis is a rare clinical entity. Diagnosis is usually made after resection. A 36-year-old male presented with uro-cutaneous fistula and left xanthogranulomatous pyelonephritis. He was offered left open radical nephrectomy. Intra-operatively, there was “woody” inflammation of the left kidney fistulizing to the splenic flexure of the colon. We successfully resected it and a segment of the colon that had fistulized. His tissue cultures grew Actinomyces odontolyticus. Post-operatively, he received 6 weeks of intravenous beta-lactam antibiotic. He recovered well without any complications. In conclusion, renal actinomycosis can be challenging to diagnose, operate and eradicate. Perioperative considerations are presented for successful management.
Keywords: Actinomycosis, Infection, Pyelonephritis xanthogranulomatous, Urinary fistula, Kidney calculi, Disease management
Introduction
Actinomycosis is a rare, chronic granulomatous disease caused by gram-positive anaerobic bacteria with Actinomyces israelii being the main human pathogen.1 It is mostly a disease of middle-aged patients affecting males more than females.1 As commensal inhabitants of the oral cavity and the gastrointestinal tract, Actinomyces acquires pathogenicity via breached or necrotic tissue. Infections can lead to granulomatous tissue, extensive reactive fibrosis, necrosis, abscess formation, draining sinuses and fistulas.1 The infection most commonly affects cervicofacial area in half the cases, followed by the abdomen then the lungs.1 Factors that predispose to abdominal actinomycosis include recent abdominal surgery, trauma, neoplasia, or a perforated viscus.
In abdominal actinomycosis, the appendix and ileocecal valve tend to be involved most commonly.1 Multiple reports of abdominopelvic actinomycosis have been associated with the use of intrauterine contraceptive devices. Renal actinomycosis is even less commonly encountered. Classically, the disease remains localized as the infection spreads contiguously, disregarding tissue planes.2 It is a disease that requires a high index of suspicion to diagnose; and on most occasions diagnosed after a surgical intervention for suspected malignancy.2 It also has a tendency to mimic tuberculosis. Therefore, failure of improvement on medical therapy should raise suspicion of actinomycosis. Here, we present an unusual case of renal actinomycosis presenting as a uro-cutaneous fistula and an asymptomatic staghorn calculus.
Case report
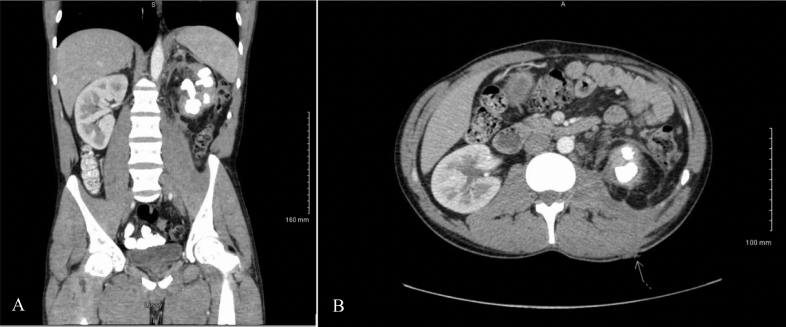
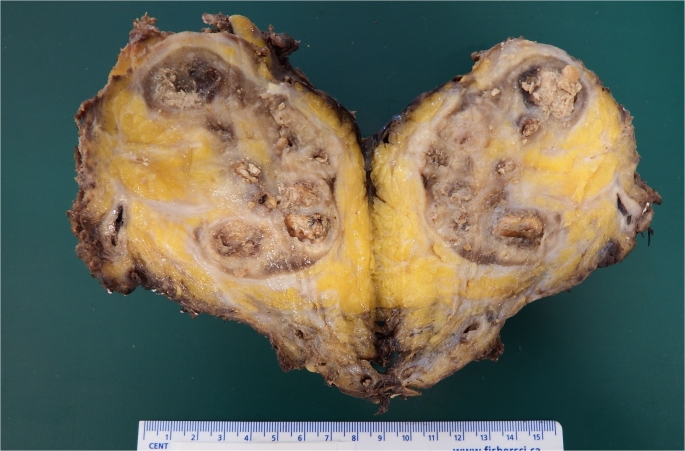
A healthy 36-year-old male, who is a smoker and works as a cook, presented to the emergency department with left lumbar abscess, which was incised and drained at the bedside. He was treated with several courses of antibiotics by his family physician. Three months later, he was referred back to the emergency department for a non-healing wound draining pus. His urinalysis showed 100 leukocytes per microliter, 25 erythrocytes per microliter, and it was negative for nitrites. He had white blood cell count of 13.2 × 109 and a hemoglobin of 123 g per liter. His serum creatinine was 71 μmol per liter with normal serum electrolytes. A Computed Tomography (CT) scan was obtained and showed a left xanthogranulomatous pyelonephritis (XGP) with a staghorn calculus in addition to a uro-cutaneous fistula (Fig. 1). The wound was swabbed, and the culture grew Proteus mirabilis. He was referred to tertiary stone center for management. Renal scan showed minimal (5%) left renal function. He was referred to infectious diseases for preoperative antibiotics and was started on doxycycline 100mg PO BID based on the antimicrobial susceptibility of Proteus mirabilis. He was offered left open radical nephrectomy to remove the source of the infection and definitively manage the uro-cutaneous fistula. In addition to pre-op doxycycline, he also received bowel preparation with magnesium citrate. Intra-operatively, he received ampicillin, gentamycin and metronidazole. Left open radical nephrectomy was performed. Intra-operatively, the “woody” appearance of the inflammatory mass was noticed (Fig. 2). The colon together with its mesentery was plastered to the psoas muscle and the kidney making tissue planes very difficult to dissect. Colon mobilization was started at the iliac crest, where there was minimal inflammation. Intra-operatively, a nephro-colic fistula was discovered, and the help of a gastro-intestinal surgeon was requested to resect the affected colon with primary anastomosis. Since he was already bowel prepped, there was no need for a diverting colostomy. Once the kidney was removed, the renal fossa was irrigated with tobramycin. The renal tissue was sent for culture in addition to pathology. The stone was sent for analysis. A closed-suction drainage was placed.
Fig. 1.
Contrast-enhanced Computed Tomography images from initial presentation showing an atrophic left kidney with a staghorn stone on coronal image (A) and a urocutaneous fistula (arrow) on axial image (B).
Fig. 2.
Gross image of the resected left kidney showing the “woody” appearance.
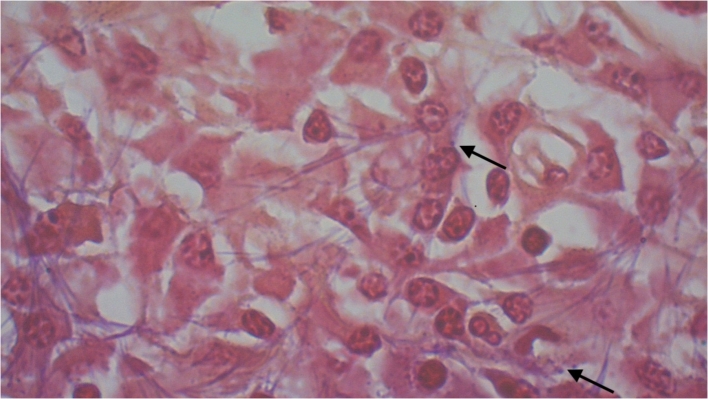
Pus from the left kidney obtained at the time of nephrectomy grew Actinomyces odontolyticus and Proteus mirabilis. Post-operatively, he was kept on intravenous meropenem for broad spectrum coverage against enteric pathogens given the nephro-colic fistula. He recovered without any complications and was discharged home with intravenous ertapenem for 6 weeks. The final pathology showed XGP with granulation tissue and fibrin deposits. Under oil immersion at 1000x magnification, Actinomyces could be seen (Fig. 3). Stone analysis showed calcium carbonate apatite.
Fig. 3.
A photo-micrograph of renal parenchymal sections stained with Gram stain showing thin filamentous branching gram-positive rods with apparent beading (black arrows). (X1000 Magnification).
Discussion
Renal Actinomycosis is rare and difficult to diagnose, requiring a high index of suspicion. There are less than 50 reported cases of renal actinomycosis in the published literature.3 It is notoriously difficult to isolate in cultures and classically have required Gram stain to look for Sulphur granules (Fig. 3). Literature regarding on optimal management of renal actinomycosis is scarce since the vast majority of cases were diagnosed after nephrectomy. Successful management with antibiotics has been reported in the literature in at least 10 patients, with resolution at follow up imaging.4 Valfour et al. reviewed several cases of different types of actinomycosis infections and recommended prolonged antibiotic therapy with a beta-lactam, such as penicillin G or amoxicillin for 6–12 months and surgical resection in more complex cases.5 However, given the nephro-colic fistula in the present case, antibiotics alone were unlikely to effectively manage it. Resection of the chronically infected kidney together with the source of the continuous contamination from the colon lead to control of the infection and identification of actinomyces in the cultures leading to its appropriate treatment with long-term antibiotics.
For a successful surgical management, we have the following suggestions. Pre-operative considerations include open rather than laparoscopic approach, bowel preparation, and pre-operative antibiotics. Intra-operatively, it is important to start the dissection where there is no inflammation such that surgical planes are easy to dissect. Another important aspect is to ask for assistance from gastro-intestinal surgeon in case of nephro-colic fistulas. Sending tissues and purulent materials for aerobic and anaerobic cultures are important to identify pathogens and perform antibacterial susceptibility testing. Finally, copiously irrigating the renal fossa with an antibiotic solution will decrease risk of abdominal abscess formation. Leaving a closed drainage system will further help decrease formation of intra-abdominal collections. Post-operatively, it is important to continue antibiotics according to sensitivities of pathogens that grow in cultures. Abdominal imaging studies may be performed to rule out recurrence of abscess formation.
Declaration of competing interest
None declared.
Acknowledgement
The authors greatly appreciate the surgical assistance and leadership of Dr Simon Tanguay from the Division of Urology, Royal Victoria Hospital Foundation.
References
- 1.Wong V.K., Turmezei T.D., Weston V.C. Actinomycosis. BMJ. 2011 Oct 11;343:d6099. doi: 10.1136/bmj.d6099. [DOI] [PubMed] [Google Scholar]
- 2.Dayan K., Neufeld D., Zissin R. Actinomycosis of the large bowel: unusual presentations and their surgical treatment. Eur J Surg. 1996;162(8):657–660. [PubMed] [Google Scholar]
- 3.Crosse J.E., Soderdahl D.W., Schamber D.T. Renal actinomycosis. Urology. 1976;7:309–311. doi: 10.1016/0090-4295(76)90466-0. [DOI] [PubMed] [Google Scholar]
- 4.Dhanani N.N., Jones D.M., Grossman H.B. Medical management of renal actinomycosis. J Urol. 2004;171(6 Pt 1):2373–2374. doi: 10.1097/01.ju.0000124452.80578.3c. [DOI] [PubMed] [Google Scholar]
- 5.Valour F., Senéchal A., Dupieux C. Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infect Drug Resist. 2014;7:183–197. doi: 10.2147/IDR.S39601. [DOI] [PMC free article] [PubMed] [Google Scholar]