Short abstract
Tumours in the olecranon are rare. A 62-year-old man presented with a 3-week history of pain in his right elbow that was relieved using routine painkillers. Persistent pain resulted in a reduction of the range of motion in the elbow and pain in the extensor and flexor groups of muscles of the forearm, which resulted in the patient seeking medical assistance. Radiography showed a round, radiolucent focus in the depth of the distal ulna. Computed tomography imaging of the thorax demonstrated one solid soft tissue mass. Histological investigation showed the cancer was a poorly differentiated adenocarcinoma. The patient received local radiotherapy and systemic chemotherapy, but he died of his primary disease 3 months later.
Keywords: Olecranon metastasis, lung adenocarcinoma, local radiotherapy
Introduction
Tumours in the olecranon are rare.1 Primary bone tumours around the elbow represent < 1% of all skeletal tumours.1 Distal bony involvement to the appendicular skeleton occurs less frequently and the incidence of olecranon metastasis is extremely rare in all cancers; so far no more than 10 cases have been reported in literature.2 This case report describes an olecranon metastasis in a patient with lung carcinoma.
Case report
In May 2017, a 62-year-old man that worked as a road cleaner was admitted to the outpatient department of the Second Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang Province, China complaining of pain in the right elbow. He reported a 3-week history of pain, erythema and oedema in the right elbow joint, which impaired his sleep. The patient did not report any preceding trauma. He also reported increasing pain and erythema in the elbow, with mild oedema developing in the preceding 2 weeks.
On examination of the right elbow, the posterior elbow was erythematous, tense and grossly engorged. The pulp of the right elbow was exquisitely painful to palpation, and his range of motion and function were impeded. The right forearm pulp was also erythematous and oedematous, but less severely. There were no signs of trauma.
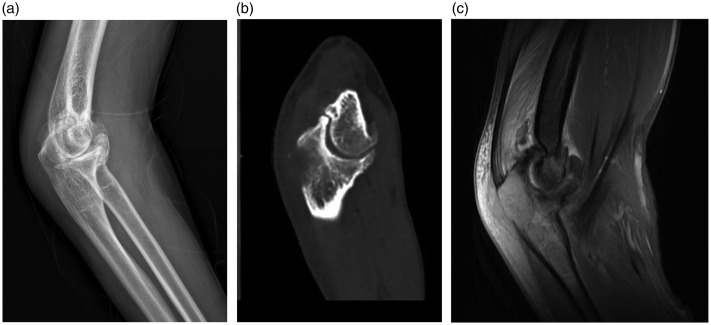
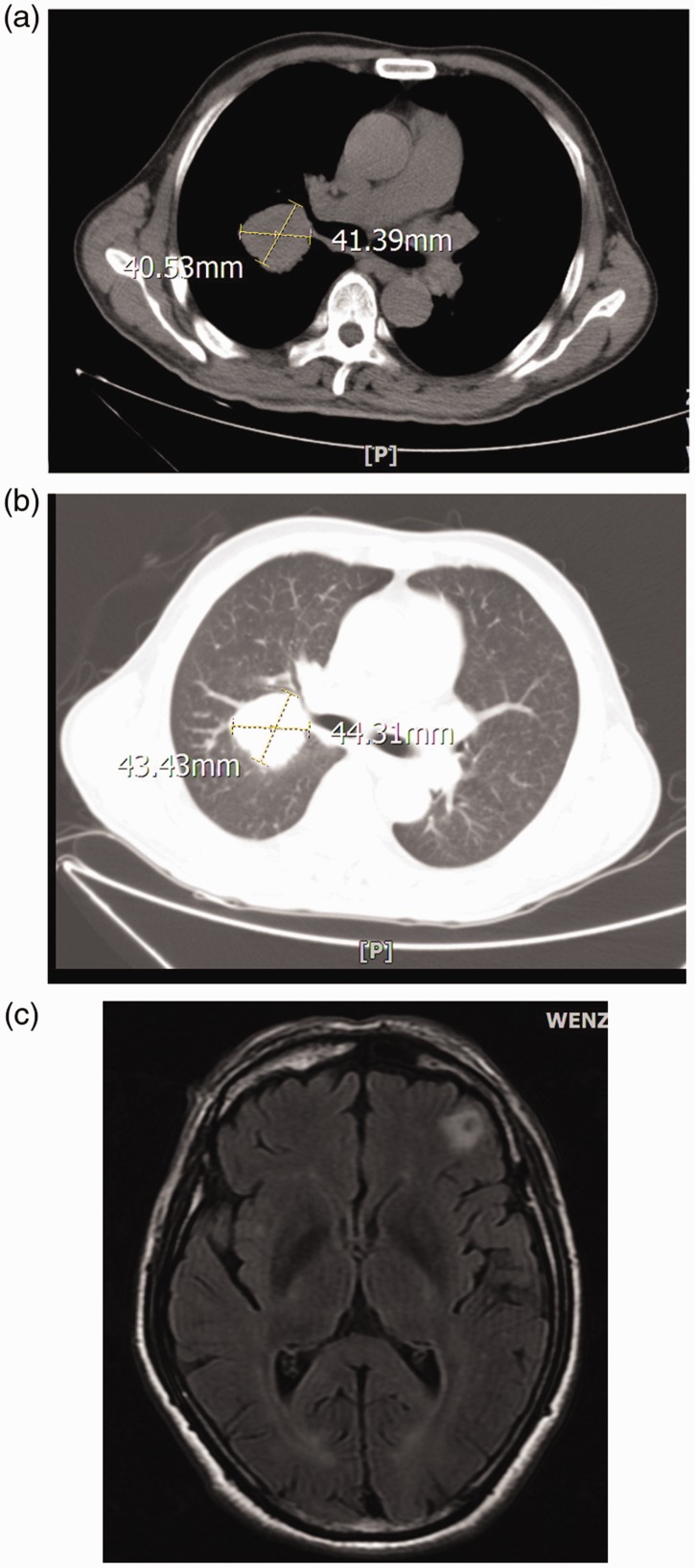
Radiography showed a round, radiolucent focus in the depth of the distal ulna, with an irregular, opaque shadow in the central part. Moreover, periosteal reaction could be found on the X-ray (Figure 1a). Computed tomography (CT) and magnetic resonance imaging (MRI) scans of the patient showed osteolytic lesions in the olecranon with destruction of cortical bone (Figures 1b and 1c). A blood test showed the carbohydrate antigen 72-4 level was 54.27 U/ml (normal range, 0.0–6.9 U/ml) and the cytokeratin fragment level was 6.70 ng/ml (normal range, 0.1–3.3 ng/ml). As a consequence of the erythematous and oedematous symptoms, the infectivity index was also evaluated, including leukocyte count, C-reactive protein and erythrocyte sedimentation rate, which were all higher than normal. In the absence of trauma, the patient was diagnosed with osteolytic metastases from a primary lung cancer, which was confirmed after the CT scans of the chest. CT imaging of the thorax demonstrated one solid soft tissue mass (approximately 4 cm × 4 cm) with undefined margins and a heterogeneous signal intensity (Figures 2a and 2b). MRI of the brain showed a tumour, which was most probably a metastatic carcinoma (Figure 2c).
Figure 1.
Diagnostic imaging of the elbow of a 62-year-old man that was admitted to the outpatient department complaining of a 3-week history of pain in the right elbow. The X-ray (a), computed tomography (b) and magnetic resonance imaging (c) scans showed osteolytic lesions in the olecranon with irregular destruction of the cortical bone and evidence of periosteal reaction.
Figure 2.
Diagnostic imaging of the thorax and brain of a 62-year-old man that was admitted to the outpatient department complaining of a 3-week history of pain in the right elbow. Computed tomography scans (a and b) of the thorax showed one solid soft tissue mass (approximately 4 cm × 4 cm) with undefined margins. Magnetic resonance imaging of the brain (c) showed a round, radiolucent focus in the frontal lobe, with an irregular, opaque shadow in the central part.
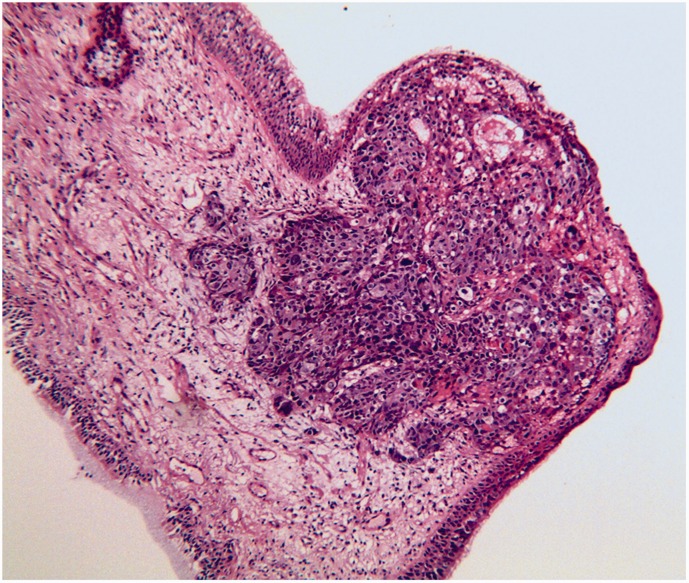
There was no surgical treatment available in our department, so the respiratory physicians oversaw the treatment regime and were responsible for the patient’s care. Routine haematoxylin and eosin staining of bronchoscopic specimens taken at the time of diagnosis were performed, followed by further immunohistochemical stains for a definitive diagnosis. The histological investigation showed the cancer was a poorly differentiated adenocarcinoma (Figure 3). The immunohistochemical stains showed that the specimen was negative for cytokeratin (CK)7, CK5/6, tumour protein p63, p40 protein, transcriptional intermediary factor-1, napsin A and Ki-67. The patient received local radiotherapy (Figure 4) and systemic chemotherapy. However, he died of his primary disease 3 months later.
Figure 3.
Representative photomicrograph of a histological section from a bronchoscopic specimen collected from a 62-year-old man that was admitted to the outpatient department complaining of a 3-week history of pain in the right elbow showing a poorly differentiated carcinoma. Haematoxylin and eosin, scale bar 20 µm. The colour version of this figure is available at: http://imr.sagepub.com.
Figure 4.
The right elbow of a 62-year-old man after 2 weeks of local radiotherapy showing pigmentation. The erythematous and oedematous symptoms had been relieved and the patient felt less pain.
The study was approved by the Ethical Board Review of the Second Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang, China (no. 20170345091) and was performed in accordance with the ethical standards of the Declaration of Helsinki of 1964. Written informed consent to publish this case report was obtained from the patient.
Discussion
Metastatic disease of the bone occurs more commonly than do primary sarcomas of the bone.3 The most common primary cancers come from the lung, breast, kidney, thyroid and prostate carcinomas.3 Metastasis to the olecranon is extremely rare in all cancers.2 Metastasis from renal cell carcinoma and multiple myeloma have been reported in the English literature.2 A case of a mucin-producing adenocarcinoma of the colon metastasising to the olecranon was reported previously.1 This current case report is the first to describe an olecranon tumour that had metastasized from a primary lung tumour. The patient had experienced 3 weeks of pain in the elbow joint without any preceding injury. Diagnosis was achieved using CT, MRI and routine pathology, which ruled out rheumatic diseases. The results of all rheumatological tests undertaken in the current case were repeatedly within normal ranges. The patient had achieved good pain relief using routine painkillers during the 3-week history of pain. When persistent pain resulted in a reduction in his range of motion in the elbow and pain in the extensor and flexor groups of the muscles of the forearm, he sought medical assistance.
Bone metastasis is one of the most common complications among lung cancer survivors.4 However, metastasis to the olecranon is extremely rare.2 Some patients with bone metastases may suffer from skeletal-related events, that is, pathological fracture, spinal cord compression and malignant hypercalcemia.5 These patients often suffer a dramatic decline of quality of life due to pain and physical limitations.6 Therefore, surgery or radiotherapy will be required to solve the bone-related symptoms to improve the quality of life.7 Surgeons have used internal fixation and cement to control local stability and reduce patient pain,8 but this approach does not kill the tumour or improve the survival rate. Radiotherapy combined with chemotherapy is the main treatment approach for cancer with metastases.9 This approach can kill tumour cells, both local and disseminated, reducing the development of new bone metastases or the progression of existing bone metastases and delaying the occurrence of skeletal-related events. In this current case, the patient received local radiotherapy and systemic chemotherapy, which relieved the symptoms of the elbow, but did not prolong overall survival. It is generally considered that tumours of the skeletal system have a low sensitivity to cytotoxic drugs.10 A previous study showed that skeletal-related events were significantly decreased with bisphosphonate therapy than without bisphosphonate among patients with nonsmall-cell lung cancer.7 Bisphosphonates can inhibit the activity of osteoclasts and decrease the dissolution and destruction of trabecular bone,11 thereby preventing a variety of skeletal-related events caused by tumour metastasis.
This current case report did not obtain pathology for the elbow joint because of the risk of infection. If an operation had been undertaken, the wound would have healed tight, increasing the patient's pain and expense. Therefore, pain relief medicine, local radiotherapy and systemic chemotherapy were administered.
In conclusion, when pain, erythema and oedema are the first symptoms in the olecranon, metastasis from a lung tumour should be considered.
Acknowledgements
The authors thank the patient and his family for their participation.
Authors’ contributions
L.Y.C. and S.X.D. designed the research; L.Y.C. and H.C. performed the research; S.X.D. and H.C. analysed the data; L.Y.C., S.X.D. and H.C. wrote the paper. All authors read and approved the final manuscript.
Declaration of conflicting interest
The authors declare that there are no conflicts of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Kularatne U, James SL, Evans N, et al. Tumours and tumour mimics in the olecranon. Clin Radiol 2015; 70: 760–773. [DOI] [PubMed] [Google Scholar]
- 2.Culleton S, de Sa E, Christakis M, et al. Rare bone metastases of the olecranon. J Palliat Med 2008; 11: 1088–1091. [DOI] [PubMed] [Google Scholar]
- 3.Leeson MC, Makley JT, Carter JR. Metastatic skeletal disease distal to the elbow and knee. Clin Orthop Relat Res 1986; 206: 94–99. [PubMed] [Google Scholar]
- 4.Hirano Y, Oda M, Tsunezuka Y, et al. Long-term survival cases of lung cancer presented as solitary bone metastasis. Ann Thorac Cardiovasc Surg 2005; 11: 401–404. [PubMed] [Google Scholar]
- 5.Shimada Y, Saji H, Yoshida K, et al. Prognostic factors and the significance of treatment after recurrence in completely resected stage I non-small cell lung cancer. Chest 2013; 143: 1626–1634. [DOI] [PubMed] [Google Scholar]
- 6.Santini D, Barni S, Intagliata S, et al. Natural history of non-small-cell lung cancer with bone metastases. Sci Rep 2015; 5: 18670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ulas A, Bilici A, Durnali A, et al. Risk factors for skeletal-related events (SREs) and factors affecting SRE-free survival for nonsmall cell lung cancer patients with bone metastases. Tumour Biol 2016; 37: 1131–1140. [DOI] [PubMed] [Google Scholar]
- 8.Kim YI, Kang HG, Kim TS, et al. Palliative percutaneous stabilization of lower extremity for bone metastasis using flexible nails and bone cement. Surg Oncol 2014; 23: 192–198. [DOI] [PubMed] [Google Scholar]
- 9.National Comprehensive Cancer Network®. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Non-Small Cell Lung Cancer, https://www.nccn.org/professionals/physician_gls/default.aspx (2019).
- 10.Shiono S, Harada M, Abiko M, et al. A case of recurrent lung cancer with bone metastases treated with tegafur-uracil and zoledronic acid for long-term survival. Gan To Kagaku Ryoho 2014; 41: 757–759 [In Japanese, English abstract]. [PubMed] [Google Scholar]
- 11.Sugiura H, Yamada K, Sugiura T, et al. Predictors of survival in patients with bone metastasis of lung cancer. Clin Orthop Relat Res 2008; 466: 729–736. [DOI] [PMC free article] [PubMed] [Google Scholar]