Short abstract
Objectives
We conducted a cross-sectional study to explore the effect of a hypothetical tobacco retail price increase on smoking habit change intention, and the role of smoking duration and intensity in smoking change intention.
Methods
In 2016 and 2017, we collected questionnaire data from 36,698 residents aged over 18 years in Songjiang district, Shanghai. Chi-square tests and weighted logistic regression were used for data analyses.
Results
The prevalence of current smoking was 19.78% (men: 48.36% and women: 0.22%). A total of 10.83% (men: 10.89% and women: 2.04%) and 9.39% of smokers (men: 9.42% and women: 6.12%) expressed the intention to smoke less or quit, respectively, given tobacco retail price increases. If the current tobacco retail price doubled, 75% of smokers stated that they would smoke less and 60% of smokers would consider quitting. Smokers with longer smoking duration and lower smoking intensity were more sensitive to tobacco price increases and more likely to change their smoking habits.
Conclusions
An increase in tobacco retail prices could induce some smokers to change their smoking behavior, particularly those with longer smoking duration and lower smoking intensity. A tobacco retail price increase is recommended, which should apply to all cigarette brands.
Keywords: Smoking duration, smoking intensity, tobacco retail price, current smoker, habit change, China
Background
Smoking has negative health effects and is the single largest preventable cause of morbidity and mortality worldwide.1,2 The World Health Organization has estimated that over 1 billion people have tobacco smoking addiction, that 5 million people die from tobacco-related diseases each year and that this figure will rise to over 8 million by 2030 if current trends continue.3,4 Tobacco smoking is a recognized risk factor for many chronic diseases5–7 and is associated with heavy health, economic, and social costs in all countries.8
Raising tobacco prices by increasing excise taxes and enacting tobacco control laws by prohibiting smoking in public places are the most effective ways of reducing smoking rates and the associated health burden.9–11 According to the International Agency for Research on Cancer,12 higher tobacco consumption costs are strongly associated with lower smoking prevalence and reduced tobacco consumption. Research on US adults demonstrates that a 10% tobacco price increase results in a 3% to 5% decrease in cigarette demand.13 In 2011, a study in Jiangxi, China, indicated that 45% of smokers would smoke fewer cigarettes and 5% would attempt to quit smoking if the retail cigarette price increased by 50%. Therefore, a tax-induced cigarette price increase may be a key policy option to promote smoking cessation.14,15
The 2010 Global Adult Survey indicated that 300 million adults in China are current smokers, and 1 million deaths are attributable to tobacco consumption each year.7,8,15–19 Because of the heavy disease burden of smoking, China introduced a cigarette tax increase in 2009; however, the tax changes have been absorbed at the producer level and have had no impact on tobacco price.18 This was a missed opportunity to investigate how tobacco price increases affect changes in smoking habits among smokers in China. Studies in Western countries have demonstrated that smokers who are younger, and have lower incomes and lower smoking intensity, are more sensitive to tobacco price increases.20 However, there are limited data on relationships between smoking duration, intensity, tobacco retail price increases, and smoking habit change in China.
We conducted a cross-sectional study in Shanghai, China. We investigated smoking prevalence, the effect of a hypothetical tobacco retail price increase on smoking habits, and the role of smoking duration and smoking intensity in the effect of the price increase on smoking habits.
Methods
Study population
This cross-sectional study was conducted in Songjiang district, Shanghai, from June 2016 to October 2017. Songjiang district is located in southwestern Shanghai and had a population of 1.76 million in 2016. We used a multistage sampling method to recruit participants from the 15 subdistricts of Songjiang. In stage one, we purposively selected 4 of the 15 Songjiang subdistricts: ZS, XQ, SS, and MG. In stage two, 9, 18, 4, and 16 neighborhood committees were randomly selected from XQ, ZS, SS, and MG subdistricts. In stage 3, we recruited all individuals aged over 18 years who had lived in Songjiang for 5 years or longer from each of the 47 selected neighborhood committees. A total of 37,543 residents were sampled and invited to participate in this study. Each participant provided written informed consent before the questionnaire interview. A final total of 36,698 residents completed the interview and were included in the final analysis.
Data collection
Data collection was carried out using interviews. These utilized self-designed Android pad-assisted software that allows paperless data input. The interviewer read out every question to participants and entered their responses onto the forms on the pad. Each interview lasted approximately 30 minutes. The questionnaire was designed by the School of Public Health, Fudan University, and comprised four parts. Part A contained 8 demographic questions. Part B contained 10 items to collect information about tobacco-related chronic disease. Part C assessed 36 health-related behaviors (tobacco use, alcohol consumption, tea drinking, and sleep habits). We designed 14 questions to collect information about tobacco use: Q1: Have you smoked at least one cigarette every day for over 6 months?; Q2: How old were you when you smoked your first cigarette?; Q3: How many cigarettes do you usually smoke each day?; Q4: Do you still smoke now?; Q5: How old were you when you quit smoking?; Q6: What is your monthly expense for tobacco purchases?; Q7: What is your average monthly income?; Q8: What is the retail price per pack for the tobacco you usually smoke?; Q9: If the tobacco retail price increased, at what price per pack would you consider smoking less?; Q10: If the tobacco retail price increased, at what price per pack would you consider quitting smoking?; Q11: Have you ever tried to quit smoking for over 24 hours in the last year?; Q12: How many times have you tried to quit smoking in recent years?; Q13: Do you live with anyone who has smoked in the last year?; Q14: Do you work with anyone who has smoked in the last year? Part D contained personal contact information for the investigator and the participant.
Definitions and index calculation
We defined a current smoker as someone who had smoked at least one cigarette every day for 6 months or more over their whole lifetime and still smoked at the time of the study. The prevalence of current smoking was calculated as the number of current smokers divided by the total number of participants. Smoking duration was defined as the time interval (year) between age at investigation and age at smoking onset for current smokers, and classified into four groups: <20, 20 to 29, 30 to 39, and ≥40 years. Smoking intensity was defined as the number of cigarettes smoked per day and categorized as 1 to 9, 10 to 19, and ≥20 cigarettes. Monthly income was recorded in Chinese RMB (1 Chinese RMB = 0.15 USD) and divided into four groups: <1500 RMB, 1500 to 2499 RMB, 2500 to 4999 RMB, and >5000 RMB). Monthly cost of smoking was categorized as <200 RMB, 200 to 499 RMB, 500 to 999 RMB, and ≥1000 RMB. The tobacco price per pack was classified into four groups: <10 RMB, 10 to 19 RMB, 20 to 49 RMB, and >50 RMB). We included two categories of smoking habit change: smoke less (smoke fewer cigarettes per day) and quit smoking. We used A, B, and C, respectively, to indicate smokers’ answers to Q8 (current tobacco price per pack), Q9 (the hypothetical tobacco price that would prompt smokers to smoke less), and Q10 (the hypothetical tobacco price that would prompt smokers to stop smoking). The formula ((B−A)/A) was calculated to determine the price increase amount that would prompt a smoker to smoke less. Similarly, the formula ((C−A)/A) was calculated to determine the price increase amount that would prompt a smoker to stop smoking.
Data analysis
Data analysis was performed using SAS software, version 9.2 (SAS Institute Inc., Cary, NC, USA). We described the data using frequency counts and proportions (rate) for qualitative variables and means and standard deviations for quantitative variables. We use the chi-square test to examine sex differences in current smoking prevalence and sex differences in tobacco consumption patterns. Weighted logistic regression was used to calculate the odds ratios (OR) and 95% confidence intervals (95% CI) for smokers who would smoke less (‘no smoke less’ as reference) or quit smoking (‘no quit’ as reference) given tobacco retail price increases. Sex, smoking duration, smoking intensity, monthly income and costs, and tobacco price per pack were adjusted in the multivariate logistic regression. All covariables were changed into dummy variables except for sex; references were set as <20 years for smoking duration, 10 to 19 cigarettes per day for smoking intensity, <1500 RMB for monthly income, <200 RMB for monthly smoking costs, and <10 RMB for tobacco price per pack. Figures were produced to describe the relationship between hypothetical tobacco retail price increase and change in smoking habits, and to explore whether smokers with longer smoking duration and lower smoking intensity were more sensitive to tobacco retail price changes. A P-value of less than 0.05 (two-tailed) was considered statistically significant.
Results
The 36,698 participants included 14,912 men (40.63%). The age ranged from 18 to 92 years; the mean age (±standard deviation) was 56.37 ± 11.29 years.
Prevalence of current smoking
For the 36,698 residents, the current smoking prevalence was 19.78%. The prevalence of current smoking in men (48.36%) was significantly higher than that in women (0.22%) (χ2 = 923.51, P < 0.01).
Tobacco consumption patterns
Over 72% of current smokers had smoked cigarettes for 30 years or more; 63% of smokers smoked over 20 cigarettes per day; more than 76% of smokers spent 200 to 999 RMB on cigarette smoking each month; and 96.06% of current smokers usually paid less than 50 RMB for tobacco per pack. In comparison with female current smokers, male current smokers tended to have longer smoking duration, higher smoking intensity, and higher monthly smoking costs, but tended to buy cheaper tobacco brands. (Table 1)
Table 1.
Tobacco consumption patterns for male and female current smokers in Songjiang, Shanghai, China.
| Variables | Current smoker (7260) |
Male smoker (7211) |
Female smoker (49) |
|||
|---|---|---|---|---|---|---|
| n | Proportion (%) | n | Proportion (%) | n | Proportion (%) | |
| Smoking duration (years)a | ||||||
| <20 | 683 | 9.41 | 662 | 9.18 | 21 | 42.86 |
| 20–29 | 1306 | 17.99 | 1293 | 17.93 | 13 | 26.53 |
| 30–39 | 2556 | 35.21 | 2548 | 35.33 | 8 | 16.33 |
| ≥40 | 2715 | 37.40 | 2708 | 37.55 | 7 | 14.29 |
| Smoking intensity (cigarettes/day)a | ||||||
| 1–9 | 636 | 8.76 | 626 | 8.68 | 10 | 20.41 |
| 10–19 | 2006 | 27.63 | 1991 | 27.61 | 15 | 30.61 |
| ≥20 | 4618 | 63.61 | 4594 | 63.71 | 24 | 48.98 |
| Monthly income (RMB)a | ||||||
| <1500 | 549 | 7.56 | 536 | 7.43 | 13 | 26.53 |
| 1500–2499 | 3008 | 41.43 | 2995 | 41.53 | 13 | 26.53 |
| 2500–4999 | 2609 | 35.94 | 2592 | 35.95 | 17 | 34.69 |
| ≥5000 | 1094 | 15.07 | 1088 | 15.09 | 6 | 12.24 |
| Monthly cost of smoking (RMB)a | ||||||
| <200 | 1135 | 15.63 | 1120 | 15.53 | 15 | 30.61 |
| 200–499 | 3913 | 53.90 | 3895 | 54.01 | 18 | 36.73 |
| 500–999 | 1625 | 22.38 | 1616 | 22.41 | 9 | 18.37 |
| ≥1000 | 587 | 8.09 | 580 | 8.04 | 7 | 14.29 |
| Tobacco price per pack (RMB) | ||||||
| <10 | 1926 | 26.53 | 1911 | 26.50 | 15 | 30.61 |
| 10–19 | 3633 | 50.04 | 3615 | 50.13 | 18 | 36.73 |
| 20–49 | 1415 | 19.49 | 1404 | 19.47 | 11 | 22.45 |
| ≥50 | 286 | 3.94 | 281 | 3.90 | 5 | 10.20 |
aThe difference between male and female current smokers was statistically significant (P < 0.01).
Smoking habit change intention among current smokers
Of 7,260 current smokers, 10.83% (men: 10.89%; women: 2.04%) stated that they would smoke less given a hypothetical tobacco retail price increase, and 9.39% (men: 9.42%; women: 6.12%) would quit smoking. Logistic regression analysis demonstrated that smokers who had smoked for 30 to 39 years or ≥40 years, with smoking intensity of ≥20 cigarettes per day, and who purchased more expensive tobacco brands were less likely to smoke less given a tobacco price change. Similarly, smokers who had smoked for 30 to 39 years and or ≥40 years, with smoking intensity of ≥20 cigarettes per day, and who purchased more expensive tobacco brands were also less likely to stop smoking given a tobacco price change (Table 2).
Table 2.
Proportion of current smokers intending to smoke less or quit smoking given a hypothetical tobacco retail price increase by smoking patterns in Songjiang, Shanghai, China.
| Variables | Groups | Smoke less if tobacco retail price increases |
LR (a)
|
LR (b)
|
Quit smoking if tobacco retail price increases |
LR (a) |
LR (b) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Proportion (%) | OR | 95% CI | OR | 95% CI | n | Proportion (%) | OR | 95% CI | OR | 95% CI | ||
| Smoking duration (years) | <20 | 92 | 13.47 | Ref | Ref | 89 | 13.03 | Ref | Ref | ||||
| 20–29 | 166 | 12.71 | 0.94 | 0.71–1.23 | 0.95 | 0.71–1.26 | 140 | 10.72 | 0.80 | 0.60–1.06 | 0.81 | 0.60–1.08 | |
| 30–39 | 278 | 10.88 | 0.78 | 0.61–1.01 | 0.76 | 0.58–0.99 | 257 | 10.05 | 0.75 | 0.58–0.97 | 0.71 | 0.54–0.94 | |
| ≥40 | 250 | 9.21 | 0.65 | 0.51–0.84 | 0.59 | 0.44–0.78 | 196 | 7.22 | 0.52 | 0.40–0.68 | 0.46 | 0.34–0.62 | |
| Smoking intensity (cigarettes/day) | 1–9 | 270 | 13.46 | Ref | Ref | 239 | 11.91 | Ref | Ref | ||||
| 10–19 | 71 | 11.16 | 0.81 | 0.61–1.07 | 0.87 | 0.65–1.16 | 64 | 10.06 | 0.83 | 0.62–1.11 | 0.85 | 0.63–1.15 | |
| ≥20 | 445 | 9.64 | 0.69 | 0.58–0.81 | 0.68 | 0.57–0.81 | 379 | 8.21 | 0.66 | 0.56–0.78 | 0.68 | 0.56–0.82 | |
| Sex | Male | 785 | 10.89 | Ref | Ref | 679 | 9.42 | Ref | Ref | ||||
| Female | 1 | 2.04 | 0.17 | 0.02–1.24 | 0.14 | 0.02–1.05 | 3 | 6.12 | 0.63 | 0.19–2.03 | 0.52 | 0.16–1.68 | |
| Monthly income (RMB) | <1500 | 68 | 12.39 | Ref | Ref | 53 | 9.65 | Ref | Ref | ||||
| 1500–2499 | 328 | 10.90 | 0.87 | 0.66–1.14 | 0.89 | 0.67–1.19 | 276 | 9.18 | 0.95 | 0.67–1.29 | 1.01 | 0.74–1.38 | |
| 2500–4999 | 277 | 10.62 | 0.84 | 0.63–1.12 | 0.78 | 0.59–1.04 | 262 | 10.04 | 1.05 | 0.77–1.43 | 0.98 | 0.71–1.34 | |
| ≥5000 | 113 | 10.33 | 0.82 | 0.59–1.12 | 0.76 | 0.55–1.07 | 91 | 8.32 | 0.85 | 0.59–1.21 | 0.80 | 0.55–1.16 | |
| Monthly cost of smoking (RMB) | <200 | 115 | 10.13 | Ref | Ref | 108 | 9.52 | Ref | Ref | ||||
| 200–499 | 454 | 11.60 | 1.16 | 0.94–1.45 | 1.22 | 0.97–1.54 | 392 | 10.02 | 1.06 | 0.85–1.33 | 1.10 | 0.86–1.40 | |
| 500–999 | 165 | 10.15 | 1.00 | 1.78–1.29 | 1.19 | 0.89–1.60 | 141 | 8.68 | 0.90 | 0.69–1.18 | 1.06 | 0.78–1.44 | |
| ≥1000 | 52 | 8.86 | 0.86 | 0.61–1.22 | 1.19 | 0.80–1.79 | 41 | 6.98 | 0.72 | 0.49–1.04 | 1.03 | 0.66–1.58 | |
| Tobacco price per pack (RMB) | <10 | 215 | 11.16 | Ref | Ref | 188 | 9.76 | Ref | Ref | ||||
| 10–19 | 420 | 11.56 | 1.04 | 0.87–1.24 | 0.97 | 0.80–1.16 | 370 | 10.18 | 1.05 | 0.87–1.26 | 0.95 | 0.78–1.15 | |
| 20–49 | 143 | 10.11 | 0.90 | 0.72–1.12 | 0.76 | 0.58–1.00 | 119 | 8.41 | 0.85 | 0.67–1.08 | 0.71 | 0.53–0.95 | |
| ≥50 | 8 | 2.80 | 0.23 | 0.11–0.47 | 0.22 | 0.11–0.46 | 5 | 1.75 | 0.17 | 0.07–0.40 | 0.16 | 0.06–0.38 | |
LR (a): univariate logistic regression; LR (b): multivariate logistic regression; OR: odds ratio; CI: confidence interval.
Relationship between smoking duration, smoking intensity, tobacco price increase, and smoking habit change
If the current tobacco retail price doubled, 75% of current smokers stated that they would smoke less, and 60% stated that they would consider quitting smoking (Table 3).
Table 3.
Percentage of current smokers intending to smoke less or quit smoking given a hypothetical tobacco retail price increase in Songjiang, Shanghai, China.
| Percentage of current smokers | Intention to smoke less |
Intention to quit |
||
|---|---|---|---|---|
| Amount of price increase (T) | 95% CI of T | Amount of price increase (T) | 95% CI of T | |
| 99 | 6.14 | 6.25–10.50 | 9.00 | 5.67–40.47 |
| 95 | 2.33 | 2.00–3.50 | 4.00 | 4.00–5.35 |
| 90 | 1.50 | 1.33–1.86 | 2.33 | 1.33–3.00 |
| 75 | 1.00 | 0.88–1.14 | 1.42 | 1.14–1.50 |
| 50 | 0.43 | 0.37–0.49 | 0.67 | 0.50–0.88 |
| 25 | 0.22 | 0.20–0.25 | 0.33 | 0.23–0.35 |
| 10 | 0.09 | 0.07–0.10 | 0.17 | 0.13–0.20 |
| 5 | 0.05 | 0.00–0.07 | 0.09 | 0.07–0.11 |
CI: confidence interval.
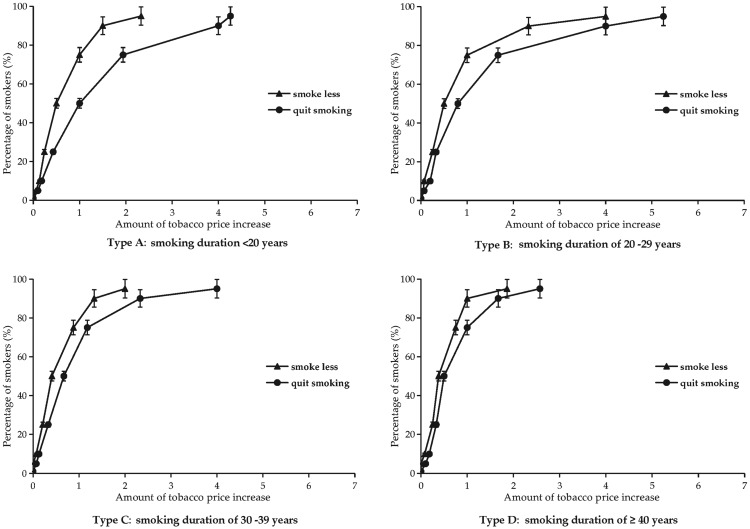
Figure 1 shows data for those current smokers who stated that they would be willing to change their smoking habits given a tobacco price increase. Smokers who had smoked for ≥40 years were much more sensitive to tobacco price increases, and a doubled retail price increase would prompt 90% of smokers to attempt to smoke less and 70% of smokers to attempt to quit. In contrast, for smokers who had smoked for a shorter period such as 20 to 29 years, a doubled retail price increase would only prompt 60% of smokers to attempt to smoke less and 50% to attempt to quit (Figure 1).
Figure 1.
Percentage of smokers intending to smoke less or quit smoking given a hypothetical tobacco retail price increase by smoking duration in Songjiang, Shanghai, China.
Tobacco retail price increase = values of formulas ((B−A)/A) and ((C−A)/A), where A = current tobacco price per pack, B = estimated tobacco price that would persuade smokers to smoke less, and C = estimated tobacco price that would persuade smokers to stop smoking.
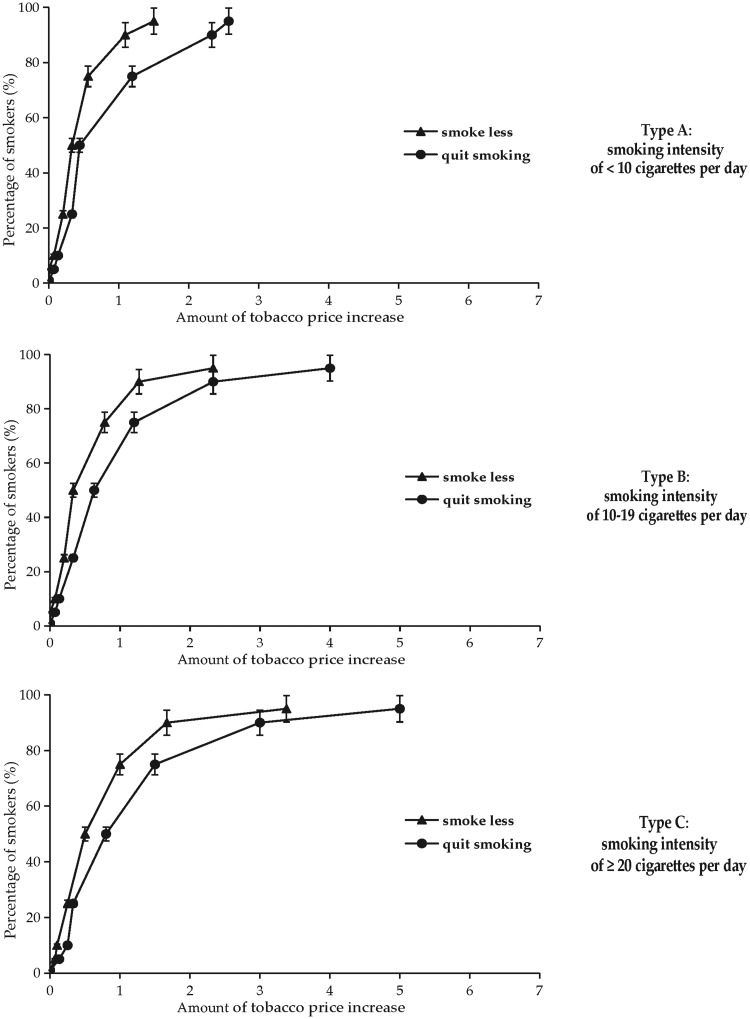
Figure 2 shows that smokers who smoked fewer than 10 cigarettes per day were more sensitive to tobacco price increases, and a doubled retail price increase would prompt 82% of smokers to attempt to smoke less and 60% to attempt to quit. In contrast, smokers who smoked ≥20 cigarettes per day were more tolerant to tobacco price increases; a doubled retail price increase would prompt 60% of smokers to smoke less and 47% to quit smoking (Figure 2).
Figure 2.
Percentage of smokers intending to smoke less or quit smoking given a hypothetical tobacco retail price increase by smoking intensity in Songjiang, Shanghai, China.
Tobacco retail price increase = values of formulas ((B−A)/A) and ((C−A)/A), where A = current tobacco price per pack, B = estimated tobacco price that would persuade smokers to smoke less, and C = estimated tobacco price that would persuade smokers to stop smoking.
Discussion
We found that the prevalence of current smoking was 19.78%. In contrast with findings from a 2013 migrant dynamics monitoring survey in China16,21 (54.50% of men and 3.70% of women were current smokers) and the Global Adult Tobacco Survey22 in 2012 (prevalence of current smoking was 52.90% for men and 2.35% for women), smoking prevalence was lower for both Songjiang men (48.36%) and women (0.22%) in this study. This lower prevalence could be attributed to both the implementation of the new Shanghai Tobacco Control Regulation, which was enacted in 2016,23 and the public health education and intervention on smoking cessation in Shanghai.17 The Shanghai Tobacco Control Regulation stipulates that all public places in Shanghai should be smoke free and that all violators (including smokers and the owners of public places) will be punished by the government. In addition, more individuals have become aware of the negative physical effects of tobacco use in recent years and have stopped smoking.24 However, the findings highlight the high prevalence of current smoking in men, particularly those with a high school education and those aged 40 to 69 years; future tobacco control measures should be focused on this population.25
Previous studies have shown that male smokers in China have smoked for longer than smokers in Western countries. Long smoking duration is related to short life expectancy and high risk of multiple diseases.26 In the USA and Australia, reported smoking duration is 29 and 26 years on average, respectively, which is about half the smoking duration of Chinese male smokers.27,28 In the present study, over 72% of current smokers in Shanghai had smoked cigarettes for over 30 years, which is consistent with other research findings from China.29 We also found that 63% of current smokers in Shanghai consumed over 20 cigarettes per day, and 96.06% of current smokers usually bought cigarettes costing less than 50 RMB per pack. Tobacco contains multiple carcinogens that have adverse effects on health, and continued tobacco use leads to nicotine dependency. Low tobacco prices result in high affordability. Long duration and high intensity of smoking induce heavy nicotine dependence. All these factors make smoking cessation difficult.
Some studies have demonstrated a lower smoking cessation rate in China, with over 80% of smokers expressing no intention to quit smoking.22 In the present study, only 10.83% of current smokers expressed the intention to smoke less and 9.39% of current smokers expressed the intention to quit smoking given a hypothetical tobacco retail price increase, which is consistent with previous studies.30 Logistic regression analysis also demonstrated that smokers with longer smoking duration and higher smoking intensity, and who purchased more expensive tobacco brands, had lower intention to change their smoking habits. This may result from a combined effect of high nicotine dependency induced by long-term heavy smoking and more tobacco affordability owing to lower tobacco retail prices in China. These findings are consistent with previous evidence,20 and indicate that increasing smoking cessation among Shanghai smokers will take considerable time, resources, and effort. Therefore, we suggest that health-related institutions should provide intense, repeated education to smokers about the adverse health effects of smoking and the benefits of quitting smoking to decrease the high smoking prevalence among male smokers.
Many studies have shown that increased consumer tobacco costs are strongly associated with lower smoking prevalence and reduced tobacco consumption.12–14 A recent review estimated that the average demand elasticity for tobacco was −0.4 for high income countries,12,31 and that young people tend to be more sensitive to tobacco price increases. The present study indicated that some current smokers might change their smoking habits if tobacco retail prices increased; a doubled tobacco retail price change might induce 75% of smokers to smoke less and 60% to consider quitting smoking. Koszegi32 showed that smokers with lower incomes are more sensitive to cigarette price changes, and a study in Jiangxi Province15 demonstrated that smokers who spend a higher proportion of their monthly income on cigarettes are more sensitive to tobacco retail price changes. Our findings show that smoking behavior change intentions prompted by increased tobacco prices were influenced by duration and intensity of smoking. Smokers with longer smoking duration, and smokers who smoked fewer cigarettes per day, were more sensitive to tobacco price increases. We recommend that policy makers consider using excise tax measures to increase tobacco retail prices, which may induce some smokers to smoke less or quit (particularly smokers with have smoked for longer and who smoke less).
The use of price-minimizing strategies is associated with fewer quit attempts and overall reduced smoking cessation.33 Smokers faced with higher cigarette prices might seek cheaper tobacco brands or purchase tobacco in bulk, and smokers using multiple price-minimizing strategies are less likely to attempt to quit and less sensitive to tobacco price increases.34 Given the low tobacco retail prices and wide tobacco retail price range (8 to 100 RMB per pack) in Shanghai, we recommend that tobacco retail price increase measures need to apply to all cigarette brands to prevent smokers switching to cheaper brands. The use of large, unexpected tobacco retail price increases may strongly affect heavily addicted smokers, but may offset tobacco affordability and discourage smoking consumption.
This study is the first to explore the relationship between smoking duration, smoking intensity, hypothetical tobacco retail price increases, and smoking habit change among smokers in China. A key study strength was the large sample size. We sampled 36,698 residents, about 6% of the total population in Songjiang; therefore, the sample can be considered representative at the municipal level. The data were collected using face-to-face interviews and an electronic questionnaire; these methods help to ensure good data quality and constitute another strength of this study.
There are some study limitations. First, the cross-sectional study design permits the calculation of prevalence but not of incidence. Second, we assessed intended smoking habit changes given hypothetical tobacco retail price increases; therefore, only smokers’ attitudes were measured, not actual behavioral changes. This necessarily limits the estimation of the real effects of tobacco price increases on smoking habit changes. Third, we measured only smoking duration and intensity to explore the effect of hypothetical tobacco retail price increases on smoking habit changes. Other factors (e.g., tobacco use knowledge, health status, education) may also affect the relationship between tobacco price increases and smoking habit changes. Fourth, other determinants of quitting, such as availability of support and smoking cessation therapies, were not assessed, which might have led to an overestimation of the effect of tobacco retail prices on smoking habit changes, particularly among smokers receiving smoking cessation therapies. To improve future studies on this topic, some of these additional factors should be investigated. Similar investigations in urban areas of Shanghai could provide more data to inform future tobacco control law legislation.
Conclusions
Increases in tobacco retail price may induce some smokers to change their smoking habits, particularly those with longer smoking duration and lower smoking intensity. Tobacco retail price increase measures need to apply to all cigarette brands to prevent smokers switching to cheaper brands. The use of large, unexpected tobacco retail price increases is recommended.
Acknowledgements
We thank all work group staff from Zhongshan, Xinqiao, Sheshan, and Maogang in Songjiang district for their contribution to data collection in the field. We also thank Professor Michael Engelgau (Centers for Disease Control and Prevention, USA) for providing suggestions and comments about this manuscript.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This study was supported by grants from the National Key R & D Program of China (2017 YFC 0907001). The funder had no role in study design, data collection and analysis, decision for publication, or preparation of the manuscript.
References
- 1.Mustafa ZM. Effects of cigarettes smoking on common carotid arteries intima media thickness in current smokers. Ozean J Applied Sci 2012; 5: 259–269. [Google Scholar]
- 2.Munire G, Onder O, Ahmet B, et al. The attitude toward tobacco dependence and barriers to discussing smoking cessation: a survey among Turkish general practitioners. Int J Public Health 2010; 55: 177–183. [DOI] [PubMed] [Google Scholar]
- 3.Khalid MA. Prevalence of tobacco use and exposure to environmental tobacco smoke among Saudi medical students in Riyadh, Saudi Arabia. J Community Health 2014; 39: 668–673. [DOI] [PubMed] [Google Scholar]
- 4.Mary RH, Linda S, Anne BP, et al. Attitude, barriers and facilitators to smoking cessation among central and eastern European nurses: a focus group study. Eur J Oncol Nurs 2018; 35: 39–46. [DOI] [PubMed] [Google Scholar]
- 5.McGhee SM, Ho LM, Lapsley HM, et al. Cost of tobacco related diseases including passive smoking in Hong Kong. Tob Control 2006; 15: 125–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Michael SS, Andrew DA, Floyd WT, et al. Impact of cigarette taxes on smoking prevalence from 2001-2015: a report using the behavioral and risk factor surveillance survey (BRFSS). PLoS One 2018; 19: e0204416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seulggie C, Jooyoung C, Kyuwoong K, et al. Effect of smoking cessation and reduction on the risk of cancer in Korean men: a population based study. Cancer Res Treat 2018; 50: 1114–1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang G, Wang Y, Wu Y, et al. The road to effective tobacco control in China. Lancet 2015; 385: 1019–1028. [DOI] [PubMed] [Google Scholar]
- 9.Regidor E, Pascual C, Carolina GG, et al. Impact of tobacco prices and smoke free policy on smoking cessation, by gender and educational groups: Spain, 1993-2012. Int J Drug Policy 2015; 26: 1215–1221. [DOI] [PubMed] [Google Scholar]
- 10.Frieden TR, Mostashari F, Kerker BD, et al. Adult tobacco use levels after intensive tobacco control measures: New York City, 2002–2003. Amer J Public Health 2005; 95: 1016–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaloupka FJ, Cummings KM, Morley CP, et al. Tax price and cigarette smoking: evidence from the tobacco documents and implications for tobacco company marketing strategies. Tob Control 2002; 11: i62–i72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.International Agency for Research on Cancer. Effectiveness of tax and price policies for tobacco control In: J Daniel. (ed.) Handbook of cancer prevention. Lyon, France: International Agency for Research on Cancer, 2011, p.i136. [Google Scholar]
- 13.Chaloupka FJ, Straif K, Leon ME. Effectiveness of tax and price policies in tobacco control. Tob Control 2011; 20: 235–238. [DOI] [PubMed] [Google Scholar]
- 14.Ahmed S, Franz GA. Raising taxes to reduce smoking prevalence in the US: a simulation of the anticipated health and economic impacts. Public Health 2008; 122: 3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang RP, Zhu LP, Yan W, et al. The influence of estimated retail tobacco sale price increase on smokers’ smoking habit in Jiangxi province, China: a cross-sectional study. Tob Induc Dis 2015; 13: 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zheng YT, Ji Y, Dong HB, et al. The prevalence of smoking, second hand smoke exposure, and knowledge of the health hazards of smoking among internal migrants in 12 provinces in China: a cross-sectional study. BMC Public Health 2018; 18: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu Y, Song HJ, Wang TY, et al. Determinants of tobacco smoking among rural to urban migrant workers: a cross-sectional survey in Shanghai. BMC Public Health 2018; 15: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao S, Zheng R, Hu TW. Can increases in the cigarette tax rate be linked to cigarette retail prices? Solving mysteries related to the cigarette pricing mechanism in China. Tob Control 2011; 21: 560–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang GH, Hu AG. Tobacco control and China’s future (In Chinese). Beijing, China: Economic Daily Press, 2011. [Google Scholar]
- 20.Centers for Disease Control and Prevention. Response to increases in cigarette prices by race/ethnicity, income, and age groups-United States, 1976–1993. MMWR 1998; 47: 605–609. [PubMed] [Google Scholar]
- 21.Yang XY, Anderson JG, Yang T. Impact of role models and policy exposure on support for tobacco control policies in Hangzhou, China. Am J Health Behav 2014; 38: 275–283. [DOI] [PubMed] [Google Scholar]
- 22.Chinese Center for Disease Control and Prevention. Global Adult Tobacco Survey (GATS) China 2010 country report. Beijing: China Sanxia Press, 2011. [Google Scholar]
- 23.Sun YW, Xu W, Ren WJ, et al. Study on the effect of evaluation of tobacco control in public places in Jing’an district of Shanghai in 2017. Chinese Journal of Health Education 2018; 34: 739–741. (In Chinese) [Google Scholar]
- 24.Azam B, Morvarid GS, Ziba RD, et al. Prevalence of home smoking bans and its determinants in families with infants. Int J Pediatr 2018; 6: 6989–6997. [Google Scholar]
- 25.Wang R, Jiang Y, Yao C, et al. Prevalence of tobacco related chronic diseases and its role in smoking cessation among smokers in a rural area of Shanghai, China: a cross sectional study. BMC Public Health 2019. doi: 10.1186/s12889-019-7110-9. [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 26.Gu DF, Kelly TN, Wu XG, et al. Mortality attributable to smoking in China. N Engl J Med 2009; 360: 150–159. [DOI] [PubMed] [Google Scholar]
- 27.Siahpush M, Heller G, Singh G. Lower levels of occupation, income and education are strongly associated with a longer smoking duration: multivariate results from the 2001 Australian National Drug Strategy Survey. Public Health 2005; 119: 1105–1110. [DOI] [PubMed] [Google Scholar]
- 28.Siahpush M, Singh GK, Jones PR, et al. Racial/ethnic and socioeconomic variations in duration of smoking: results from 2003, 2006 and 2007 Tobacco Use Supplement of the Current Population Survey. J Public Health (Oxf) 2010; 32: 210–218. [DOI] [PubMed] [Google Scholar]
- 29.Ferri CP, West R, Moriyama TS, et al. Tobacco use and dementia: evidence from the 1066 dementia population-based surveys in Latin America, China and India. Int J Geriatr Psychiatry 2011; 26: 1177–1185. [DOI] [PubMed] [Google Scholar]
- 30.Guo H, Sa ZH. Socioeconomic differentials in smoking duration among adult male smokers in China: results from the 2006 China Health and Nutrition Survey. PLoS One 2015; 10: e0117354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Louise M, Claire C, Robin Q, et al. The impact of an increase in excise tax on the retail price of tobacco in New Zealand. Tob Control 2016; 25: 458–463. [DOI] [PubMed] [Google Scholar]
- 32.Gruber J, Koszegi B. Tax incidence when individual are time-inconsistent: the case of cigarette taxes. J Public Econ 2004; 88: 1959–1988. [Google Scholar]
- 33.Andrea SL, Andrew JH, Richard OC, et al. How do price minimizing behaviors impact smoking cessation? Findings from the International Tobacco Control (ITC) Four Country Survey. Int J Environ Res Public Health 2011; 8: 1671–1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hyland A, Higbee C, Li Q, et al. Access to low-taxed cigarettes deters smoking cessation attempts. Amer J Public Health 2005; 95: 994–995. [DOI] [PMC free article] [PubMed] [Google Scholar]