Short abstract
Objective
Work-related stress is a public health issue. Stress has multiple physical and psychological consequences, the most serious of which are increased mortality and cardiovascular morbidity. The ThermStress protocol was designed to offer a short residential thermal spa program for work-related stress prevention that is compatible with a professional context.
Methods
Participants will be 56 male and female workers aged 18 years or above. All participants will undergo a 6-day residential spa program comprising psychological intervention, physical activity, thermal spa treatment, health education, eating disorder therapy and a follow-up. On six occasions, participants’ heart rate variability, cardiac remodelling and function, electrodermal activity, blood markers, anthropometry and body composition, psychology and quality of life will be measured using questionnaires and bone parameters.
Results
This study protocol reports the planned and ongoing research for this intervention.
Discussion
The ThermStress protocol has been approved by an institutional ethics committee (ANSM: 2016 A02082 49). It is expected that this proof of concept study will highlight the effect of a short-term specific residential thermal spa program on the prevention of occupational burnout and work-related stress. The findings will be disseminated at several research conferences and in published articles in peer-reviewed journals.
Trial Registration: ClinicalTrials.gov (NCT 03536624, 24/05/2018)
Keywords: Stress, burnout, prevention, heart rate variability, spa bath, work, biomarkers
Introduction
Stress at work is both a public health issue and an economic issue.1,2 The main consequences of stress on health are increased cardiovascular morbidity and mortality.3 Stress particularly affects autonomic nervous system functioning.4 One of the main cardiovascular health effects of stress is deregulation of the sympathovagal balance.5 The most common measures of autonomic nervous system activity are heart rate variability (HRV) and electrodermal activity.6 Conveniently, there are non-intrusive and pain-free measures of HRV and electrodermal activity.7 Some genetic polymorphisms linked with stress, such as polymorphism of angiotensin converting enzymes8–11 or of serotonin,12–14 are also associated with cardiovascular risk. Stress also causes arterial ischemic pathology15 via complex mechanisms involving changes in arterial endothelial and microvascular atherosclerosis.15 These microvascular changes are linked to systemic inflammation caused by stress,16 and changes within the hypothalamic–pituitary axis (e.g. dehydroepiandrosterone sulphate (DHEAS),17,18 cortisol,17,18) and at a central level (e.g. neuropeptide Y,19 brain-derived natriuretic factor (BDNF),20). Stress can also lead to obesity through inappropriate eating behaviours.21 Stressed individuals also find it difficult to lose weight.22 Possible biological mechanisms that link obesity and stress involve the action of stress on leptin,23 an anorectic hormone secreted by adipose tissue and proposed as a biomarker of stress.24 Stress, particularly stress at work, is responsible for multiple somatic diseases.25,26 For example, long-term mental stress can have negative effects on bone tissue, leading to osteoporosis and increased bone fracture risk.27 Therefore, an assessment of the association between bone parameters and stress is needed. Moreover, our program may modify bone parameters and decrease bone fracture risk.6,28 More interestingly, peripheral quantitative computed tomography (pQCT) can be used to measure muscles and intra- and inter-muscular fat content,29–31 which can also be modified by our program32 and may be biomarkers of stress. Many stress biomarkers are secreted by adipose tissue.33 Moreover, it has been demonstrated that limb composition reflects total body composition, particularly fat.29–31
The psychological consequences of stress are numerous and include dissatisfaction, anxiety, depression and burnout.26 Non-pharmacological methods of stress management include psychological interventions, physical activity34,35 and therapy for stress-induced eating disorders.36 Several psychological interventions have demonstrated positive effects on work-related stress, such as cognitive-behavioural therapy,37 acceptance and commitment therapy38,39 and mindfulness.40,41 The benefits of any type of physical activity on the physical and mental health of individuals at any age are indisputable.42
A recent systematic review highlighted the effects of balneotherapy (bathing in mineral springs) and spa therapy on stress biomarkers. This review of 15 studies (684 subjects) emphasised the potential benefits of such treatment on cortisol levels.43 In France, there are five spa resorts that specialise in the treatment of psychosomatic disorders. The usual duration for a residential thermal program in these resorts is 3 weeks. Previous research has demonstrated the positive effects of a 3-week spa therapy intervention on burnout.44 However, a shorter residential thermal spa program may be more compatible with a professional context because of the availability of individuals. In addition, it would be useful to focus on work-related stress prevention (i.e. before the state of burnout).
Objective
This ThermStress proof of concept study was developed to provide a new approach to the management of stress disorders. The main aim of the study is to assess the ability of a short residential spa program to increase HRV and manage work-related stress.
Methods
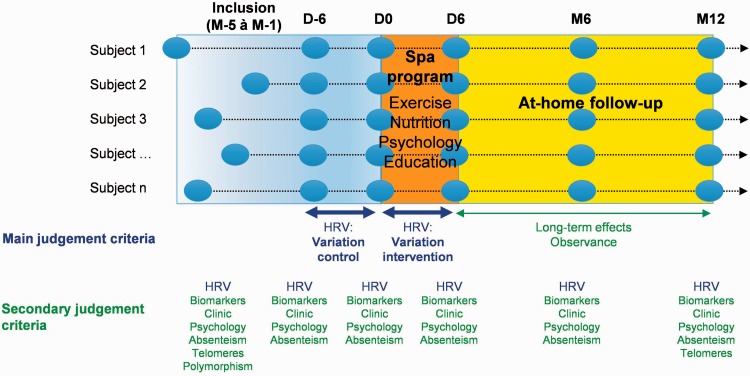
Protocol design: This 1-year study with repeated measures on six occasions (inclusion (one to five months prior to the beginning of the spa program – M-1 to M-5), 6 days before the start (D-6), at the start (D0), at the end of the spa program (D6), at 6 months (M6) and at 12 months (M12)), will allow us to explore the effect of a specific short-term residential thermal spa program on the prevention of occupational burnout and work-related stress in workers, focusing on measures of well-being and cardiovascular morbidity. Each participant will undergo a 6-day residential spa program comprising psychological intervention, physical activity, thermal spa treatment, health education and eating disorder therapy and a follow-up. Each participant will be his/her own control and we will compare variations in parameters between intervention/control periods (short-term variations: D6/D0 and D0/D6; long-term variations: inclusion/D0 compared with D0/M6–M12) (Figure 1).
Figure 1.
The ThermStress protocol. M-5: 5 months before the study; M-1: 1 month before the study.
HRV: heart rate variability.
Selection criteria
Inclusion criteria: Volunteers will be workers aged 18 years to retirement, with a stress visual analogue scale score greater than 50 mm, who wish to follow a residential spa thermal program to manage work-related stress. Participants must have had a stable weight during the last 3 months and have no uncontrolled cardiac, hepatic, renal or endocrine diseases.32 In compliance with human ethics guidelines, participants must be covered by social health insurance and must sign consent forms.
Exclusion criteria: Potential participants will be excluded if major treatment and/or protocol deviations are observed. Other exclusion criteria are drugs and medical conditions that significantly affect the primary outcome of HRV (e.g. alpha or beta-blockers; arrhythmias or conduction disorders such as bundle branch block, atrioventricular heart block).45
Power analysis: The rationale for the sample size estimation is based on HRV, which is a biomarker of both stress and morbidity/mortality.46,47 In particular, within multiple parameters of HRV, we considered log low frequency (LF)/high frequency (HF) HRV for sample size calculation because it is the parameter that traditionally represents sympathovagal balance, together with global HRV (see description of LF/HF below in the description of the primary outcome section).4,46 A log LF/HF with low values is associated with good autonomic nervous system adaptation. Based on previous work,48 we assumed a statistical power greater than 80%, a two-sided type I error of 5% and an individual correlation coefficient set at 0.5 (each subject as his/her own control). Based on the results of a pilot study, we assumed that our response will promote an absolute decrease of the log LF/HF by 20% (with a standard deviation of 45%).49 Therefore, we need to include n = 43 subjects. Finally, to take into account lost to follow-up, it is proposed to include 56 subjects.
Participants: Participants will be male and female volunteers aged 18 years to retirement. Following ethics committee approval, and based on our calculation, 56 volunteers will be enrolled to account for potential dropouts. All participants will be given written information regarding the project and will have to sign consent forms before enrolment. Workers will be recruited by the spa centres using flyers and website announcements. Participants will also be recruited using advertisements provided by the CHU of Clermont-Ferrand or by the Clermont Auvergne University.
Intervention programs: Participants will attend a short-term residential spa program lasting 6 days, which combines psychological intervention, physical activity, thermal spa treatment, health education and eating disorder therapy. Physical activity will be diverse (endurance, strength, circuit training) to offer a personalised program compatible with the desires of each participant. The benefits of all types of physical activity on the physical and mental health of individuals of any age are indisputable. Psychological interventions will include various validated therapies for work-related stress, such as cognitive-behavioural therapy, acceptance and commitment therapy and mindfulness. Details on intervention components are shown in Table 1 and the agenda of the intervention program is shown in Table 2.
Table 1.
Description of intervention components.
| Intervention | Dose | Description |
|---|---|---|
| Spa treatment | 6 × 120 min | Spa treatment is a combination of spa bath (i.e. thermal mud, jets), spa shower (i.e. hydromassage) and body massage |
| Psychological workshop | 6 × 120 min | Cognitive-behavioural therapy, acceptance and commitment therapy, and mindfulness |
| Nutrition workshop | 4 × 90 min | Participants must understand: concept of energetic balance, calculation of energy intake, calculation of energy expenditure (of physical activity, thermic effect of food), effects of stress on energy intake (quantity and type of intake), effects of physical activity on food intake regulation, cooking sessions (to cook healthy meals) |
| +1 breakfast | During the breakfast session, participants will be provided with information and advice related to the preparation of a healthy breakfast | |
| Supervised physical activity | 5 × 120 min | Supervised physical activity will be delivered every day by a qualified exercise physiologist. Physical activity will be delivered as circuit training and will include resistance and aerobic training |
| Biomarkers of Stress workshop | 1 × 90 min | Understanding the purpose of biological changes owing to stress and burnout |
Table 2.
Agenda of the intervention program.
| Sunday | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | |
|---|---|---|---|---|---|---|---|
| 7h30–8h00 | Breakfast | Breakfast | Breakfast with dietician | Breakfast | Breakfast | Breakfast | |
| 8h15–10h15 | Spa treatment | Spa treatment | Spa treatment | Spa treatment | Spa treatment | Spa treatment | |
| 10h30–12h30 | Psychological workshop | Psychological workshop | Psychological workshop | Psychological workshop | Psychological workshop | Psychological workshop | |
| 12h45–13h45 | Lunch | Lunch | Lunch | Lunch | Lunch | Lunch | |
| 13h55–15h25 | * | Nutrition workshop | Nutrition workshop | Biomarkers of Stress workshop | Nutrition workshop | Nutrition workshop | |
| 15h25–15h30 | * | Collation† | Collation† | Collation† | Collation† | Collation† | |
| 15h30–17h30 | * | Supervised physical activity | Supervised physical activity | Supervised physical activity | Supervised physical activity | Supervised physical activity | |
| 17h30–19h30 | Free time | Free time | Free time | Free time | Free time | Free time | |
| 19h30–20h30 | Dinner | Dinner | Dinner | Dinner | Dinner | Dinner |
Arrival of participants at their desired time on Sunday afternoon.
Collation is any kind of healthy combination, such as fruits/yogurt or any other low glycaemic index carbohydrates and protein sources.
Follow-up: After the intervention phase of the study, participants will undergo a 1-year at-home follow-up.
Measurements: Each participant will undergo a battery of tests (described below). Data collection will be performed six times, as previously described, except for dual-energy X-ray absorptiometry (DXA) and pQCT, which will be performed at inclusion and after 12 months, and cardiac remodelling and function, which will be performed at inclusion and after 6 months. Table 3 outlines all the study outcomes.
Table 3.
Outcomes.
| Variables | Type of measure | Measurement modality | References |
|---|---|---|---|
| Biomarkers of stress and cardiovascular risk | Skin conductance | Wrist band electrodes – Movisens | 7 |
| Blood flow velocity | Laser speckle contrast imaging | 78,79 | |
| Myocardial longitudinal strain | Speckle-tracking echocardiography | 85,86 | |
| Genetic polymorphisms | Polymorphism of angiotensin converting enzymes | Blood cells | 8–11 |
| Polymorphism of serotonin | Blood cells | 12–14 | |
| Demographics | Age, gender, qualification, personal work status, ethnicity, life and occupational events | Questionnaire | 4 |
| Clinical measurements | Height, weight, blood pressure, heart rate, waist circumference | ||
| Body composition | Muscle mass, fat mass, bone structure | Impedance meter | 80 |
| Densitometry X-ray absorption | 6 | ||
| Peripheral quantitative computed tomography | 73–75 | ||
| Quantitative ultrasound | 81 | ||
| Psychology and quality of life | Depression | Hamilton Anxiety Rating Scale | 62 |
| Anxiety | Hamilton Anxiety Rating Scale | 62 | |
| State–Trait Anxiety Inventory | 60,61 | ||
| General health | General Health Questionnaire (SF-12) | 71 | |
| Stress, fatigue, sleep | Visual analogue scale | 4 | |
| Burnout | Maslach Burnout Inventory | 59 | |
| Mindfulness | Freiburg Mindfulness Inventory | 22,23 | |
| Coping | Brief COPE Questionnaire | 63 | |
| Emotions | Emotion Regulation Questionnaire | 64 | |
| Perception of work | Karasek’s Job Content Questionnaire | 65 | |
| Self-efficacy | Perceived Self-efficacy Scale | 66 | |
| Addiction to work | Work Addiction Risk test | 67 | |
| Alexithymia | Toronto Alexithymia Scale | 68,82,83 | |
| Illness perception | Brief Illness Perception Questionnaire, adapted for stress at work | 69,84 | |
| Metacognition | Metacognitions Questionnaire-30 | 70 | |
| Lifestyle | E.g., smoking, alcohol consumption, coffee consumption, food intake | Questionnaires | 4 |
| Physical activity | Recent Physical Activity Questionnaire | 72 | |
| Alloplastic load | HbA1c, HDLc and LDLc, TG | Ethylenediaminetetraacetic acid tube | 6 |
| Cortisol | Dry tube, serum isolation and deep-freezing | 17,85 | |
| DHEAS | Dry tube, serum isolation and deep-freezing | 17,85 | |
| Leptin | Dry tube, serum isolation and deep-freezing | 6 | |
| BDNF | Dry tube, serum isolation and deep-freezing | 20,86,87 | |
| Pro-inflammatory cytokines: IL-1β, IL-6, IL-1, TNFα | Dry tube, serum isolation and deep-freezing | 6 | |
| NPY | Dry tube, serum isolation and deep-freezing | 19 | |
| Telomere length | Blood; Southern blot or polymerase chain reaction analyses | 88 | |
| Heart rate variability | Holter | 89 | |
| Skin conductance – electrodermal activity | Wristband electrodes | 89 |
A total of 25 mL of blood will be sampled (i.e. 100 mL in 1 year). HbA1c: haemoglobin A1c; HDLc: high-density lipoprotein cholesterol; LDLc: low-density lipoprotein cholesterol; TG: triglycerides; DHEAS: dehydroepiandrosterone sulphate; BDNF: brain-derived neurotrophic factor; IL: interleukin; TNFα: tumour necrosis factor α; NPY: neuropeptide Y.
Primary outcome: To assess the ability of a short residential spa program to manage work-related stress and increase HRV, a biomarker of both stress and morbidity/mortality.46,47
Heart rate variability: HRV parameters will be assessed over 26 hours using a heart rate transmitter belt simply positioned on the chest, with a 26-hour recording time, a beat per minute within a 25 to 240 range and respiratory rate within a 3 to 70 range (Zephyr™ BioHarness™ BT, Zephyr Technology, Annapolis, USA). The HRV data will be examined according to the recommendations of the European Society of Cardiology and the North American Society (Task Force).50 HRV will be explored in time and frequency domains.51 A methodology developed by our team will also be used.52 Premature atrial and ventricular beats will be automatically discarded and visually checked. In the time domain, R-R intervals, standard deviation of R-R intervals, square root of the mean squared difference of successive R-R intervals (rMSSD), and number of adjacent N-N differing by more than 50 ms divided by the total number of N-N intervals (pNN50) will be analysed. The rMSSD and pNN50 are associated with HF power and hence parasympathetic activity. In the spectral domain, we will analyse LF power (0.04–0.15 Hz), an index of both sympathetic and parasympathetic activity, and HF power (0.15–0.4 Hz), representing the most efferent vagal (parasympathetic) activity to the sinus node. Very low frequency (VLF; 0.003–0.04 Hz) partially reflects thermoregulatory mechanisms, fluctuation in activity of the renin–angiotensin system and the function of peripheral chemoreceptors. LF and HF will also be assessed in normalised units (nu), which represent the relative value of each power component in proportion to the total power minus the VLF component. Thus, LFnu and HFnu are considered to represent best sympathetic and parasympathetic activity, respectively.53 The LF/HF ratio (i.e. the sympathovagal balance) will also be calculated.46
Secondary outcomes: Secondary outcomes will be (1) to demonstrate an improvement in perceived stress and other stress biomarkers following the short residential spa program, (2) to study the influence of genetic polymorphisms on stress and on the response to our stress management program, (3) to examine the relationship between subjective (questionnaire responses) and objective (biomarker) variables, (4) to propose a salient biomarker or a salient composite index of biomarkers of stress and (5) to study the effect on stress of observance to the program at follow-up.
Anthropometry: The following anthropometric measures will be obtained according to the recommendations of the International Society for the Advancement of Kinanthropometry54: standing height (m) and body mass (kg), waist circumference (cm), and lower limb bone length/breadth (cm).54
Body composition: Body composition (muscle mass and fat mass) will be measured using DXA (DXA, QDR-4500A, Hologic, Inc., Waltham, MA, USA).6 and impedancemeter.80
Biomarkers of stress and cardiovascular risk: Skin conductance will be measured using wristband electrodes with sampling rates at 2, 4, 8, 16 and 32 Hz during phases 1 to 3. The SC sensor (Q-Sensor®-Affectiva®, Massachusetts Institute of Technology, USA) is set on a wristband and has a 24-hour battery life when logging. In addition, it measures wrist movements with a built-in 3-axis accelerometer.
Blood flow velocity and myocardial longitudinal strain will be measured using speckle echocardiography (Vivid Q, GE Healthcare Biosciences, Piscataway, NJ, USA). All 2-dimensional (2D), time-motion, Doppler and 2D-strain acquisitions and measurements will be performed according to recent guidelines.55,56 Left ventricular (LV) volumes and ejection fractions will be measured using Simpson’s biplane method.57 LV mass will be calculated using the Devereux formula and indexed for height (Cornell adjustment). Pulsed Doppler LV transmitral velocities, including early and atrial waves, will be obtained using the apical 4-chamber view. Tissue Doppler imaging measures of myocardial systolic, early diastolic and atrial velocities will be assessed at the mitral annulus level in the apical 4- and 2-chamber views. The early transmitral flow velocity to the early diastolic tissue velocity ratio was used as an index of LV filling pressure. 58 Left atrium volume will be assessed using apical 4- and 2-chamber views. A graduation of LV diastolic dysfunction will be obtained according to recent guidelines. 58 2D cine-loops (frame rate >70 ips) of at least five cycles will be recorded in the short-axis views (base, mid, apex), as well as in the apical 4-, 3- and 2-chamber views. 2D-strain analysis will be performed post-processing using EchoPAC 201TM software (GE Healthcare Biosciences, Piscataway, NJ, USA). Longitudinal and circumferential strains and strain rates, as well as apex and base rotations, will be directly obtained from the six-segment model. Twist mechanics will be computed from apical and basal rotational data using dedicated software (Scilab, Paris, France). For each view, the three cardiac cycles displaying the best image quality will be selected. Blood pressure and heart rate will be continuously monitored, and the systolic meridional wall stress, an index of afterload, will be calculated. LV end-diastolic volumes will also be obtained as a preload index.
Endocrine assays: Blood samples will be collected by a qualified paediatric nurse after participants have fasted overnight. Blood will be collected using a venepuncture at the brachial vein. After collection, blood will be centrifuged and aliquots will be stored (−80°) for subsequent analysis.
(triglycerides,6 cholesterol,6 low-density lipoprotein cholesterol,6 high-density lipoprotein cholesterol,6 glycaemia,6 insulin,6 ultra-sensitive C-reactive protein,6 cortisol,17,18 DHEAS17,18) as well as all other biochemical measures (leptin,6 brain-derived neurotrophic factor,20,87 interleukin-1b,6 interleukin-6,6 interleukin-1,6 tumour necrosis factor a,6 and neuropeptide Y19) will be assessed in the biochemistry laboratory of Clermont-Ferrand University Hospital. All analyses will be conducted by the same technician. Polymorphism of the angiotensin converting enzyme8-11 and polymorphism of serotonin12-14 will be measured from blood cells, as welll as telomere length.88
Complementary measures: Questionnaire measures of the following variables will be obtained: stress and fatigue (visual analogue scale of 100 mm),4 burnout (Maslach Burnout Inventory),59 depression and anxiety (Hospital Anxiety and Depression Scale,60 State–Trait Anxiety Inventory (STAI-Y),61 7-item Hamilton Anxiety Rating Scale),62 mindfulness (Freiburg Mindfulness Inventory),22 coping strategies (Brief COPE Questionnaire),63 emotions (Emotion Regulation Questionnaire),64 perception of work (Karasek’s Job Content Questionnaire),65 self-efficacy (Perceived Self-efficacy Scale),66 addiction to work (Work Addiction Risk test),67 alexithymia (20-item Toronto Alexithymia Scale),68 illness perception (Brief Illness Perception Questionnaire, adapted for stress at work),69 metacognition (Metacognitions Questionnaire-30),70 general health (12-item General Health Questionnaire (SF-12)),71 lifestyle (e.g. smoking, alcohol consumption)4 and physical activity (Recent Physical Activity Questionnaire).72
Bone parameters: Bone microarchitecture will be measured using pQCT (XCT 3000 Stratec Medizintechnik Pforzheim, Germany).73–75 Bone mineral content (BMC) (g/cm), volumetric cortical and trabecular BMC (mg/cm3), total area (mm2), cortical and trabecular area (mm2) and density (g/cm2), and bone strength (mm3) will be assessed at the distal (4%) and proximal (66%) sites of the non-dominant tibia and radius. A planar scout scan was first conducted to determine the anatomical reference line for both the radius and tibia. Tomographic slices of 2 mm thickness were obtained at the 4% and 66% sites measured distally. Scan speed and voxel size were 20 mm/s and 0.4 mm, respectively. To ensure measurement quality, calibration checks will be performed by scanning a standard phantom with known densities prior to each scan. To calculate BMC, volumetric cortical BMC, volumetric trabecular BMC, cortical bone area, cortical density, trabecular area, trabecular density and stress strain index will be analysed using the Stratec pQCT manufacturer’s software. Contour mode 1 with a threshold of 180 mg/cm3 will be used to separate soft tissue and bone to analyse trabecular bone. Cortical bone will be identified and removed using a constant default threshold of 710 mg/cm3. A contour mode 3 with peel mode 1 at a threshold of 40 mg/cm3 will be used to assess muscle and fat cross-sectional areas.
Bone densitometry will be conducted using DXA (QDR-4500A, Hologic, Inc., Waltham, MA, USA). Bone mineral density (g/cm2), BMC (g) and bone area (cm2) will be determined for each participant. The DXA measurements will be taken for the whole body, the lumbar spine (L2–L4) and the non-dominant hip (including the femoral neck, and the trochanteric and intertrochanteric regions). All DXA scans will be conducted by the same technician and quality assurance checks will be performed routinely. The in-vivo coefficient of variation is 0.5%.
Statistical analysis: Statistical analysis will be performed using Stata software (version 13; StataCorp LP, College Station, TX, USA). All statistical tests will be two-sided and p < 0.05 will be considered significant. After testing for normal distribution (Shapiro–Wilk test), data will be treated either by parametric or non-parametric analyses according to statistical assumptions.
Mixed models will be used to analyse longitudinal data for fixed effects (before and after the residential thermal program), time-point evaluation and group × time interaction taking into account between- and within-participant variability (as random effects). A Sidak’s type I error correction will be applied to take into account multiple comparisons. The normality of residuals will be examined using the Shapiro–Wilk test. If necessary, a logarithmic transformation will be used to achieve normality for the dependent outcome. Multivariable analyses will be carried out with adjustment for covariates fixed according to epidemiological relevance and physical activity. Particular attention will be paid to the covariates ‘time between inclusion and beginning of the intervention’ (variable for each subject) and ‘time between beginning of the intervention and the follow-up’ (fixed for each subject).
Analysis of non-repeated data will be performed using analysis of variance (ANOVA) or Kruskal–Wallis tests. When appropriate (omnibus p-value less than 0.05), a post-hoc test for multiple comparisons will be used: the Tukey–Kramer test following ANOVA and the Dunn test following the Kruskal–Wallis test. Categorical variables will be compared using chi-squared or Fisher’s test. The Marascuilo procedure will be performed for multiple comparisons. Relations between quantitative outcomes will be analysed using correlation coefficients (Pearson or Spearman, according to statistical distribution). Fisher’s z transformation and William’s T2 statistic will be used to compare correlations between variables and within a single group of subjects.
A sensitivity analysis will be used to study the statistical nature of missing data (random or non-random); that is, baseline characteristics of participants with complete follow-up and those lost to follow-up will be compared using the aforementioned statistical tests. Even if random-effects models permit the analysis of data when a participant is lost to follow-up, the most appropriate imputation data method according to the statistical nature of missing data (multiple imputation data, last observation carried out (LOCF)) will be applied. More precisely, if a participant drops out of the study before it ends, then his or her last observed score on the dependent variable is used for all subsequent (i.e. missing) observation points if the LOCF imputation approach is used.
Confidentiality: Data will be stored in the principal investigator’s office on a password-protected computer only accessible to members of our research team. In the electronic database, participants’ names will be replaced with numeric identity codes. Blood samples will also be labelled with the numeric identity codes and samples will be stored in our laboratories. Only aggregate results will be reported, ensuring participants’ anonymity.
Radiation: Both DXA and pQCT provide measures of body composition and bone properties by exposing participants to low-level radiation: 0.0056 mSv from DXA scans (whole body, lumbar and hip) and 0.0014 mSv from pQCT scans (tibia and radius measures).76 Over the duration of the study, the effective dose of 0.014 mSv will be administered.
Ethics approval and consent to participate: The ThermStress protocol complies with the ethics guidelines for clinical research (Declaration of Helsinki) and has been approved by an ethics committee (CPP Tours Région centre Ouest 1, France - ANSM: 2016 A02082 49). The protocol has also been registered with the database ClinicalTrials.gov (NCT03536624). In accordance with ethical considerations, the chief investigator will be responsible for ensuring that participants understand the potential risks and benefits of study participation. Moreover, the chief investigator will be responsible for obtaining written consent from participants. The results will be disseminated at several research conferences and published in peer-reviewed journals.
Concluding remarks
The ThermStress protocol was designed to provide a better understanding of the effect of a short residential spa program to improve HRV and prevent work-related stress. The idea is to adapt a 3-week thermal cure for occupational burnout to a 6-day program, which is more accessible to workers and hopefully will produce similar results for work-related stress and burnout prevention. The long-term success of lifestyle interventions such as those proposed in work-related stress prevention depends on treatment observance (psychology, physical activity, nutrition).77 We previously demonstrated that spa programs can play a major role in prompting sustainable lifestyle changes.28 This shorter program may lead to better treatment observance during the 1-year follow-up, as psychological interventions, physical activity and diet will be supervised in the spa resort and participants will be accompanied by health care professionals. Findings from this protocol are expected to offer a more appropriate thermal program for burnout and work-related stress prevention that is accessible to the public.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
The study is integrally funded by the Région Auvergne Rhône-Alpes by the University Hospital of Clermont-Ferrand, by the European Regional Development Fund (FEDER, Fonds Europeen de Développement Economique et Régional) and by the spa resort of Néris-les-Bains. The funding source had no role in the design, conduct, or reporting of the study. The authors wish to thank Ms Frédérique BRIAT for her commitment to setting up and monitoring the program. The authors wish also to thank Mr Bertrand BLOYER for promoting a short residential thermal spa program to prevent work-related stress/burnout.
References
- 1.Quine L. Workplace bullying in NHS community trust: staff questionnaire survey. BMJ 1999; 318: 228–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Plus de 3 millions de Français au bord du burn-out. Le Monde. 2014. (24 janvier).
- 3.Backe EM, Seidler A, Latza U, et al. The role of psychosocial stress at work for the development of cardiovascular diseases: a systematic review. Int Arch Occup Environ Health 2012; 85: 67–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dutheil F, Boudet G, Perrier C, et al. JOBSTRESS study: comparison of heart rate variability in emergency physicians working a 24-hour shift or a 14-hour night shift - a randomized trial. Int J Cardiol 2012; 158: 322–325. [DOI] [PubMed] [Google Scholar]
- 5.Tsuji H, Larson MG, Venditti FJ, Jr, et al. Impact of reduced heart rate variability on risk for cardiac events. The Framingham Heart Study. Circulation 1996; 94: 2850–2855. [DOI] [PubMed] [Google Scholar]
- 6.Courteix D, Valente-Dos-Santos J, Ferry B, et al. Multilevel approach of a 1-year program of dietary and exercise interventions on bone mineral content and density in metabolic syndrome - the RESOLVE randomized controlled trial. PLoS One 2015; 10: e0136491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dutheil F, Chambres P, Hufnagel C, et al. ‘Do Well B.': design Of WELL Being monitoring systems. A study protocol for the application in autism. BMJ Open 2015; 5: e007716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Montgomery H, Clarkson P, Barnard M, et al. Angiotensin-converting-enzyme gene insertion/deletion polymorphism and response to physical training. Lancet 1999; 353: 541–545. [DOI] [PubMed] [Google Scholar]
- 9.Henrion D, Benessiano J, Philip I, et al. The deletion genotype of the angiotensin I-converting enzyme is associated with an increased vascular reactivity in vivo and in vitro. J Am Coll Cardiol 1999; 34: 830–836. [DOI] [PubMed] [Google Scholar]
- 10.Gard PR. The role of angiotensin II in cognition and behaviour. Eur J Pharmacol 2002; 438: 1–14. [DOI] [PubMed] [Google Scholar]
- 11.Thayer JF, Merritt MM, Sollers JJ, 3rd, et al. Effect of angiotensin-converting enzyme insertion/deletion polymorphism DD genotype on high-frequency heart rate variability in African Americans. Am J Cardiol 2003; 92: 1487–1490. [DOI] [PubMed] [Google Scholar]
- 12.Hariri AR, Drabant EM, Weinberger DR. Imaging genetics: perspectives from studies of genetically driven variation in serotonin function and corticolimbic affective processing. Biol Psychiatry 2006; 59: 888–897. [DOI] [PubMed] [Google Scholar]
- 13.Hariri AR, Weinberger DR. Functional neuroimaging of genetic variation in serotonergic neurotransmission. Genes Brain Behav 2003; 2: 341–349. [DOI] [PubMed] [Google Scholar]
- 14.McCaffery JM, Bleil M, Pogue-Geile MF, et al. Allelic variation in the serotonin transporter gene-linked polymorphic region (5-HTTLPR) and cardiovascular reactivity in young adult male and female twins of European-American descent. Psychosom Med 2003; 65: 721–728. [DOI] [PubMed] [Google Scholar]
- 15.Proietti R, Mapelli D, Volpe B, et al. Mental stress and ischemic heart disease: evolving awareness of a complex association. Future Cardiol 2011; 7: 425–437. [DOI] [PubMed] [Google Scholar]
- 16.Elenkov IJ, Iezzoni DG, Daly A, et al. Cytokine dysregulation, inflammation and well-being. Neuroimmunomodulation 2005; 12: 255–269. [DOI] [PubMed] [Google Scholar]
- 17.Lac G, Dutheil F, Brousse G, et al. Saliva DHEAS changes in patients suffering from psychopathological disorders arising from bullying at work. Brain Cogn 2012; 80: 277–281. [DOI] [PubMed] [Google Scholar]
- 18.Danhof-Pont MB, van Veen T, Zitman FG. Biomarkers in burnout: a systematic review. J Psychosom Res 2011; 70: 505–524. [DOI] [PubMed] [Google Scholar]
- 19.Krystal JH, Neumeister A. Noradrenergic and serotonergic mechanisms in the neurobiology of posttraumatic stress disorder and resilience. Brain Res 2009; 1293: 13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karege F, Perret G, Bondolfi G, et al. Decreased serum brain-derived neurotrophic factor levels in major depressed patients. Psychiatry Res 2002; 109: 143–148. [DOI] [PubMed] [Google Scholar]
- 21.Sinha R, Jastreboff AM. Stress as a common risk factor for obesity and addiction. Biol Psychiatry 2013; 73: 827–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robinson E, Hunger JM, Daly M. Perceived weight status and risk of weight gain across life in US and UK adults. Int J Obes (Lond) 2015; 39: 1721–1726. [DOI] [PubMed] [Google Scholar]
- 23.Haleem DJ. Investigations into the involvement of leptin in responses to stress. Behav Pharmacol 2014; 25: 384–397. [DOI] [PubMed] [Google Scholar]
- 24.Konishi N, Otaka M, Odashima M, et al. Systemic stress increases serum leptin level. J Gastroenterol Hepatol 2006; 21: 1099–1102. [DOI] [PubMed] [Google Scholar]
- 25.Kawakami N, Haratani T. Epidemiology of job stress and health in Japan: review of current evidence and future direction. Ind Health 1999; 37: 174–186. [DOI] [PubMed] [Google Scholar]
- 26.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA 2007; 298: 1685–1687. [DOI] [PubMed] [Google Scholar]
- 27.Wippert PM, Rector M, Kuhn G, et al. Stress and alterations in bones: an interdisciplinary perspective. Front Endocrinol (Lausanne) 2017; 8: 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Courteix D, Valente-Dos-Santos J, Ferry B, et al. Correction: multilevel approach of a 1-year program of dietary and exercise interventions on bone mineral content and density in metabolic syndrome - the RESOLVE randomized controlled trial. PLoS One 2015; 10: e0140307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Butner KL, Creamer KW, Nickols-Richardson SM, et al. Fat and muscle indices assessed by pQCT: relationships with physical activity and type 2 diabetes risk. J Clin Densitom 2012; 15: 355–361. [DOI] [PubMed] [Google Scholar]
- 30.Frank-Wilson AW, Johnston JD, Olszynski WP, et al. Measurement of muscle and fat in postmenopausal women: precision of previously reported pQCT imaging methods. Bone 2015; 75: 49–54. [DOI] [PubMed] [Google Scholar]
- 31.Sherk VD, Thiebaud RS, Chen Z, et al. Associations between pQCT-based fat and muscle area and density and DXA-based total and leg soft tissue mass in healthy women and men. J Musculoskelet Neuronal Interact 2014; 14: 411–417. [PMC free article] [PubMed] [Google Scholar]
- 32.Dutheil F, Lac G, Lesourd B, et al. Different modalities of exercise to reduce visceral fat mass and cardiovascular risk in metabolic syndrome: the RESOLVE randomized trial. Int J Cardiol 2013; 168: 3634–3642. [DOI] [PubMed] [Google Scholar]
- 33.Dutheil F, Gordon BA, Naughton G, et al. Cardiovascular risk of adipokines: a review. J Int Med Res 2018; 46: 2082–2095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med 2014; 44: 81–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hansen AM, Blangsted AK, Hansen EA, et al. Physical activity, job demand-control, perceived stress-energy, and salivary cortisol in white-collar workers. Int Arch Occup Environ Health 2010; 83: 143–153. [DOI] [PubMed] [Google Scholar]
- 36.Kiecolt-Glaser JK. Stress, food, and inflammation: psychoneuroimmunology and nutrition at the cutting edge. Psychosom Med 2010; 72: 365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van der Klink JJ, Blonk RW, Schene AH, et al. The benefits of interventions for work-related stress. Am J Public Health 2001; 91: 270–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bond FW, Bunce D. The role of acceptance and job control in mental health, job satisfaction, and work performance. J Appl Psychol 2003; 88: 1057–1067. [DOI] [PubMed] [Google Scholar]
- 39.Brinkborg H, Michanek J, Hesser H, et al. Acceptance and commitment therapy for the treatment of stress among social workers: a randomized controlled trial. Behav Res Ther 2011; 49: 389–398. [DOI] [PubMed] [Google Scholar]
- 40.Davies WR. Mindful meditation: healing burnout in critical care nursing. Holist Nurs Pract 2008; 22: 32–36. [DOI] [PubMed] [Google Scholar]
- 41.Cohen-Katz J, Wiley SD, Capuano T, et al. The effects of mindfulness-based stress reduction on nurse stress and burnout: a quantitative and qualitative study. Holist Nurs Pract 2004; 18: 302–308. [DOI] [PubMed] [Google Scholar]
- 42.Bhui KS, Dinos S, Stansfeld SA, et al. A synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism. J Environ Public Health 2012; 2012: 515874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Antonelli M, Donelli D. Effects of balneotherapy and spa therapy on levels of cortisol as a stress biomarker: a systematic review. Int J Biometeorol 2018; 62: 913–924. [DOI] [PubMed] [Google Scholar]
- 44.Blasche G, Leibetseder V, Marktl W. Association of spa therapy with improvement of psychological symptoms of occupational burnout: a pilot study. Forsch Komplementmed 2010; 17: 132–136. [DOI] [PubMed] [Google Scholar]
- 45.Elghozi JL, Girard A, Laude D. Effects of drugs on the autonomic control of short-term heart rate variability. Auton Neurosci 2001; 90: 116–121. [DOI] [PubMed] [Google Scholar]
- 46.Boudet G, Walther G, Courteix D, et al. Paradoxical dissociation between heart rate and heart rate variability following different modalities of exercise in individuals with metabolic syndrome: the RESOLVE study. Eur J Prev Cardiol 2017; 24: 281–296. [DOI] [PubMed] [Google Scholar]
- 47.Hufnagel C, Chambres P, Bertrand PR, et al. The need for objective measures of stress in autism. Front Psychol 2017; 8: 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Takada M, Ebara T, Kamijima M. Heart rate variability assessment in Japanese workers recovered from depressive disorders resulting from job stress: measurements in the workplace. Int Arch Occup Environ Health 2010; 83: 521–529. [DOI] [PubMed] [Google Scholar]
- 49.Ronser B. Fundamentals of Biostatistics. Belmont, CA: Duxbury Press, 1995. [Google Scholar]
- 50.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation 1996; 93: 1043–1065. [PubMed] [Google Scholar]
- 51.Tochikubo O, Ikeda A, Miyajima E, et al. Effects of insufficient sleep on blood pressure monitored by a new multibiomedical recorder. Hypertension 1996; 27: 1318–1324. [DOI] [PubMed] [Google Scholar]
- 52.Khalfa N, Bertrand PR, Boudet G, et al. Heart rate regulation processed through wavelet analysis and change detection: some case studies. Acta Biotheoretica 2012; 60: 109–129. [DOI] [PubMed] [Google Scholar]
- 53.Sandercock G. Normative values, reliability and sample size estimates in heart rate variability. Clin Sci (Lond) 2007; 113: 129–130. [DOI] [PubMed] [Google Scholar]
- 54.Marfell-Jones MJ, Stewart A, de Ridder J. International standards for anthropometric assessment. International Society for the Advancement of Kinanthropometry, 2012.
- 55.Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015; 28: 1–39.e14. [DOI] [PubMed] [Google Scholar]
- 56.Mor-Avi V, Lang RM, Badano LP, et al. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications: endorsed by the Japanese Society of Echocardiography. J Am Soc Echocardiogr 2011; 24: 277–313. [DOI] [PubMed] [Google Scholar]
- 57.Otterstad JE. Measuring left ventricular volume and ejection fraction with the biplane Simpson’s method. Heart 2002; 88: 559–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2016; 29: 277–314. [DOI] [PubMed] [Google Scholar]
- 59.Choron G, Dutheil F, Lesage FX. Are nurses burned out? Int J Nurs Stud 2016; 58: 80–81. [DOI] [PubMed] [Google Scholar]
- 60.Spiess K, Sachs G, Moser G, et al. Psychological moderator variables and metabolic control in recent onset type 1 diabetic patients–a two year longitudinal study. J Psychosom Res 1994; 38: 249–258. [DOI] [PubMed] [Google Scholar]
- 61.Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken) 2011; 63: S467–S472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hung CI, Liu CY, Wang SJ, et al. The cut-off points of the Depression and Somatic Symptoms Scale and the Hospital Anxiety and Depression Scale in detecting non-full remission and a current major depressive episode. Int J Psychiatry Clin Pract 2012; 16: 33–40. [DOI] [PubMed] [Google Scholar]
- 63.Endler NS, Parker JD. Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol 1990; 58: 844–854. [DOI] [PubMed] [Google Scholar]
- 64.Ioannidis CA, Siegling AB. Criterion and incremental validity of the emotion regulation questionnaire. Front Psychol 2015; 6: 247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Trousselard M, Dutheil F, Naughton G, et al. Stress among nurses working in emergency, anesthesiology and intensive care units depends on qualification: a Job Demand-Control survey. Int Arch Occup Environ Health 2016; 89: 221–229. [DOI] [PubMed] [Google Scholar]
- 66.Luszczynska A, Scholz U, Schwarzer R. The general self-efficacy scale: multicultural validation studies. J Psychol 2005; 139: 439–457. [DOI] [PubMed] [Google Scholar]
- 67.Robinson BE, Post P. Validity of the Work Addiction Risk Test. Percept Mot Skills 1994; 78: 337–338. [DOI] [PubMed] [Google Scholar]
- 68.Li S, Zhang B, Guo Y, et al. The association between alexithymia as assessed by the 20-item Toronto Alexithymia Scale and depression: a meta-analysis. Psychiatry Res 2015; 227: 1–9. [DOI] [PubMed] [Google Scholar]
- 69.Broadbent E, Petrie KJ, Main J, et al. The brief illness perception questionnaire. J Psychosom Res 2006; 60: 631–637. [DOI] [PubMed] [Google Scholar]
- 70.Wells A, Cartwright-Hatton S. A short form of the metacognitions questionnaire: properties of the MCQ-30. Behav Res Ther 2004; 42: 385–396. [DOI] [PubMed] [Google Scholar]
- 71.Amiel R, Lebigre F. [A new rapid test for the evaluation of mental health. Its use for early detections. Its importance in health surveys]. Ann Med Psychol (Paris) 1970; 1: 565–580. [PubMed] [Google Scholar]
- 72.Golubic R, May AM, Benjaminsen Borch K, et al. Validity of electronically administered Recent Physical Activity Questionnaire (RPAQ) in ten European countries. PLoS One 2014; 9: e92829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sornay-Rendu E, Boutroy S, Munoz F, et al. Cortical and trabecular architecture are altered in postmenopausal women with fractures. Osteoporos Int 2009; 20: 1291–1297. [DOI] [PubMed] [Google Scholar]
- 74.Boutroy S, Bouxsein ML, Munoz F, et al. In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 2005; 90: 6508–6515. [DOI] [PubMed] [Google Scholar]
- 75.Stein EM, Liu XS, Nickolas TL, et al. Abnormal microarchitecture and reduced stiffness at the radius and tibia in postmenopausal women with fractures. J Bone Miner Res 2010; 25: 2572–2581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Damilakis J, Adams JE, Guglielmi G, et al. Radiation exposure in X-ray-based imaging techniques used in osteoporosis. Eur Radiol 2010; 20: 2707–2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fappa E, Yannakoulia M, Pitsavos C, et al. Lifestyle intervention in the management of metabolic syndrome: could we improve adherence issues? Nutrition 2008; 24: 286–291. [DOI] [PubMed] [Google Scholar]
- 78.Puissant C, Abraham P, Durand S, et al. Reproducibility of non-invasive assessment of skin endothelial function using laser Doppler flowmetry and laser speckle contrast imaging. PLoS One 2013; 8: e61320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Souza EG, De Lorenzo A, Huguenin G, et al. Impairment of systemic microvascular endothelial and smooth muscle function in individuals with early-onset coronary artery disease: studies with laser speckle contrast imaging. Coron Artery Dis 2014; 25: 23–28. [DOI] [PubMed] [Google Scholar]
- 80.Pateyjohns IR, Brinkworth GD, Buckley JD, et al. Comparison of three bioelectrical impedance methods with DXA in overweight and obese men. Obesity (Silver Spring) 2006; 14: 2064–2070. [DOI] [PubMed] [Google Scholar]
- 81.Wu C, Gluer C, Lu Y, et al. Ultrasound characterization of bone demineralization. Calcif Tissue Int 1998; 62: 133–139. [DOI] [PubMed] [Google Scholar]
- 82.Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto Alexithymia Scale–I. Item selection and cross-validation of the factor structure. J Psychosom Res 1994; 38: 23–32. [DOI] [PubMed] [Google Scholar]
- 83.Bagby RM, Taylor GJ, Parker JD. The Twenty-item Toronto Alexithymia Scale–II. Convergent, discriminant, and concurrent validity. J Psychosom Res 1994; 38: 33–40. [DOI] [PubMed] [Google Scholar]
- 84.Broadbent E, Wilkes C, Koschwanez H, et al. A systematic review and meta-analysis of the Brief Illness Perception Questionnaire. Psychol Health 2015; 30: 1361–1385. [DOI] [PubMed] [Google Scholar]
- 85.Lesage FX, Choron G, and Dutheil F. Multifaceted Program to Reduce Job Strain in ICU Nurses. JAMA 2019; 321: 1410–1411. [DOI] [PubMed] [Google Scholar]
- 86.Karege F, Bondolfi G, Gervasoni N, et al. Low brain-derived neurotrophic factor (BDNF) levels in serum of depressed patients probably results from lowered platelet BDNF release unrelated to platelet reactivity. Biol Psychiatry 2005; 57: 1068–1072. [DOI] [PubMed] [Google Scholar]
- 87.Shimizu E, Hashimoto K, Okamura N, et al. Alterations of serum levels of brain-derived neurotrophic factor (BDNF) in depressed patients with or without antidepressants. Biol Psychiatry 2003; 54: 70–75. [DOI] [PubMed] [Google Scholar]
- 88.Epel ES, Blackburn EH, Lin J, et al. Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci U S A 2004; 101: 17312–17315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Elefteriou F, Ahn JD, Takeda S, et al. Leptin regulation of bone resorption by the sympathetic nervous system and CART. Nature 2005; 434: 514–520. [DOI] [PubMed] [Google Scholar]