Short abstract
Paraneoplastic limbic encephalitis (PLE) in association with clear cell renal cell carcinoma has never been reported in China. We herein describe a 54-year-old man with a 1-week history of headache and a 3-day history of psychiatric symptoms. Slight nuchal rigidity was found by physical examination. Imaging studies of the head were normal. Blood and cerebrospinal fluid antibody testing were both positive for N-methyl-D-aspartic acid antibodies. Subsequent contrast-enhanced computed tomography revealed a 5.2- × 4.2-cm left kidney mass with intense enhancement. Emergent laparoscopic nephron-sparing surgery was successfully performed. Immunohistochemistry revealed clear cell renal cell carcinoma. The patient’s status improved after the surgery, and he was discharged after 1 month of hospitalization. At the 6-month follow-up, magnetic resonance imaging showed no recurrence, and the patient was living independently. This case indicates the potential effect of nephron-sparing surgery in the treatment of PLE. Tumor screening should be performed early in patients with suspected PLE. Early surgical resection of the primary tumor can improve patients’ prognosis.
Keywords: Paraneoplastic limbic encephalitis, paraneoplastic syndrome, nephron-sparing surgery, renal cell carcinoma, N-methyl-D-aspartic acid antibody, psychiatric symptom, case report
Introduction
Paraneoplastic limbic encephalitis (PLE) is a rare neuropsychiatric condition related to malignancies without direct neoplastic invasion into the nervous system (<1%).1 Corsellis et al.2 first found that PLE is associated with malignant tumors in 1968. The syndrome of PLE is typically characterized by an altered mental status, subacute cognitive dysfunction, memory impairment, sleep disturbances, seizures, and psychiatric features that include depression, anxiety, and hallucinations. The diagnosis of PLE should be based on the presence of cancer and a classical neurological syndrome with well-characterized onconeural antibodies.3 Therefore, the diagnosis is often difficult; PLE is usually diagnosed in the weeks to months following a diagnosis of neoplasia because similar symptoms are caused by many other diseases. Signs of a neurologic disorder may also be the first manifestation of an unrecognized malignancy.4
An association between limbic encephalitis and renal cell carcinoma is extremely rare. Two cases of limbic encephalopathy related to renal cell carcinoma were first diagnosed at autopsy.5 Subsequently, Bell et al.6 and Harrison et al.7 each reported one case of renal cell carcinoma that was associated with limbic encephalitis and cured with radical nephrectomy. We herein describe a patient with renal cell carcinoma in whom the clinical progression of PLE was reversed using nephron-sparing surgery. To our knowledge, this is the first case of PLE cured with nephron-sparing surgery in China.
Case report
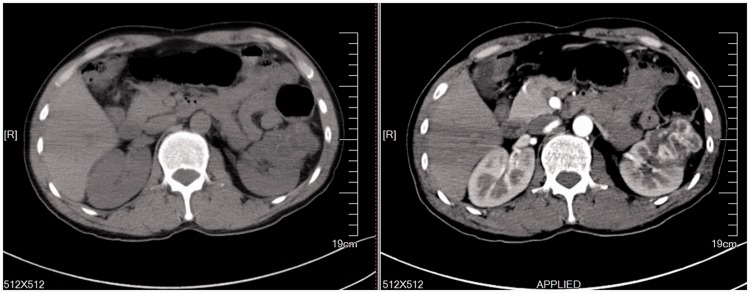
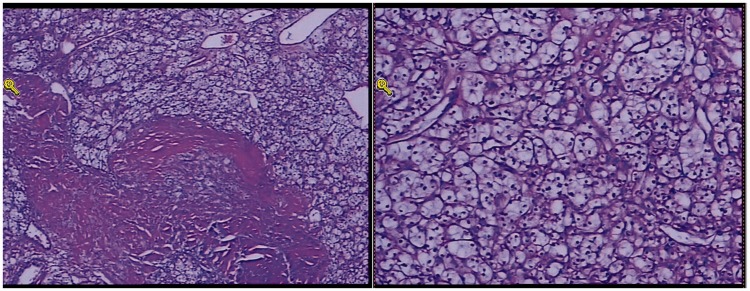
A 54-year-old man presented with a 1-week history of headache and a 3-day history of mental disorder. The headache manifested in the whole head with mild to moderate distending pain. The mental disorder included dysphoria, excitement, and speaking gibberish. Slight nuchal rigidity was found by physical examination. Imaging studies of the head were normal. Two cerebrospinal fluid examinations indicated a normal pressure, glucose level and chloride level. After 1 week of treatment with antivirals and nutritional, neurologic, and immunomodulatory treatments, the symptoms worsened. Blood and cerebrospinal fluid antibody testing were both positive for N-methyl-D-aspartic acid (NMDA) antibodies. The possibility of PLE was suspected. Therefore, a computed tomography scan was performed to assess for an occult tumor. Computed tomography revealed a 5.2- × 4.2-cm left kidney mass with intense enhancement (Figure 1). Emergent laparoscopic nephron-sparing surgery was successfully performed. Pathological examination showed Fuhrman grade 2 clear cell renal cell carcinoma measuring 5.5 × 5.0 × 4.0 cm (Figure 2). The symptoms of PLE gradually improved, and the patient was discharged after 1 month. At the 6-month follow-up, no recurrence was found and the patient was living independently.
Figure 1.
Computed tomography image showing renal cell carcinoma in the left kidney.
Figure 2.
Hematoxylin and eosin-stained sections showing clear cell renal cell carcinoma.
Discussion
The malignancies most frequently related to PLE are small cell lung cancer and testicular cancer.8 An association between PLE and renal cell carcinoma is extremely rare. To our knowledge, our report describes the first case of PLE cured with nephron-sparing surgery in a Chinese patient with renal cell carcinoma. As many as 10% to 40% of patients with renal cell carcinoma have paraneoplastic syndromes.9 However, endocrine or neuroendocrine effects rather than neurologic symptoms are often present in these patients. These paraneoplastic syndromes include high blood pressure, anemia, fever, weight loss, cachexia, polycythemia, abnormal liver function, hypercalcemia, high blood sugar, rapid blood sedimentation, neuromuscular disease, amyloidosis, excessive breast disease, and coagulopathies. The occurrence rate of central and peripheral nervous syndromes is only 0.5% to 1.0% in patients with renal cell carcinoma.10 These syndromes are not associated with the tumor stage. These neurological syndromes are frequently the main complaint associated with a potential tumor, and the physician’s awareness of these syndromes may contribute to the early diagnosis of cancer.11
Limbic encephalitis is a type of inflammation in the limbic system, which is involved in motivation, memory behavior, and emotion. The etiology and mechanism of PLE remain unclear, but the main theory is an autoimmune mechanism. Antigens located in the central nervous system may be similar to antigens detected ectopically in malignancies. An assay of antibodies to onconeural antigens in the serum or cerebrospinal fluid may help to diagnose PLE. However, negative classic antibody and cerebrospinal fluid results do not rule out the diagnosis of PLE. Studies have shown that only approximately 60% of patients are positive for antibodies.12 Antibody-positive patients can be initially divided into two groups. The first group comprises patients with antibodies to intracellular neural antigens (including antibodies to Hu, Ma2, and amphiphysin). The second group comprises patients with antibodies to neural cell membrane antigens (including antibodies to NMDA receptors and voltage-gated potassium channels). There are also reports of PLE associated with other antibodies that cannot be classified into these two groups.13 The detection of specific antibodies takes time, but it is helpful for diagnosis and treatment. Compared with disorders involving antibodies to intracellular antigens, immunotherapy has a stronger curative effect on disorders involving antibodies to neural cell membrane antigens.14 Additionally, if the clinician highly suspects PLE, imaging examination of the thorax, abdomen, and pelvis should be done early. Initial imaging findings are often normal, in which case a positron emission tomography scan may be useful.15 Treatment of PLE consists of tumor resection and immunotherapy involving steroids, intravenous immunoglobulin, or plasma exchange. The present case indicates that if PLE is diagnosed early, emergent nephron-sparing surgery for renal cell carcinoma can effectively treat the limbic encephalitis.
To the best of our knowledge, this is the first case in which PLE was cured using nephron-sparing surgery for clear cell renal cell carcinoma in China. This case indicates the potential effect of nephron-sparing surgery in the treatment of PLE. Doctors should improve their understanding of this disease. Tumor screening should be performed early in patients suspected to have PLE. Early surgical resection of the primary tumor can improve patients’ prognosis.
Abbreviations
PLE, paraneoplastic limbic encephalitis; NMDA, N-methyl-D-aspartic acid.
Acknowledgements
We gratefully acknowledge Wanlong Tan at the Department of Urology of Nanfang Hospital for providing help with the manuscript writing.
Authors’ contributions
Data collection: Lai, Xie.
Data analysis: Zhu, Deng.
Manuscript writing: Zhu, Deng.
Manuscript interpretation and editing: Tan, Zhu.
All authors read and approved the final manuscript.
Availability of data and material
The data are contained within the manuscript, and any missing details will be available from the corresponding author on reasonable request.
Consent for publication
The patient provided written informed consent for his case report to be published.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Ethics approval and consent to participate
This report was approved by the Ethics Committee of The Affiliated Ganzhou Hospital of Nanchang University (201702654), and the patient provided informed consent.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Darnell RB, Posner JB. Paraneoplastic syndromes involving the nervous system. N Engl J Med 2003; 349: 1543–1554. [DOI] [PubMed] [Google Scholar]
- 2.Corsellis JA, Goldberg GJ, Norton AR. “Limbic encephalitis” and its association with carcinoma. Brain 1968; 91: 481. [DOI] [PubMed] [Google Scholar]
- 3.Graus F, Delattre JY, Antoine JC, et al. Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry 2004; 75: 1135–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lieberman FS, Schold SC. Distant effects of cancer on the nervous system. Oncology (Williston Park) 2002; 16: 1539–1548. [PubMed] [Google Scholar]
- 5.Newman NJ, Bell IR, McKee AC. Paraneoplastic limbic encephalitis: neuropsychiatric presentation. Biol Psychiatry 1990; 27: 529–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bell BB, Tognoni PG, Bihrle R. Limbic encephalitis as a paraneoplastic manifestation of renal cell carcinoma. J Urol 1998; 160(3 Pt 1): 828. [DOI] [PubMed] [Google Scholar]
- 7.Harrison JW, Cherukuri R, Buchan D. Renal cell carcinoma presenting with paraneoplastic hallucinations and cognitive decline from limbic encephalitis. J Gen Inter Med 2015; 30: 1037–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gultekin SH, Rosenfeld MR, Voltz R, et al. Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patients. Brain 2000; 123(Pt 7): 1481–1494. [DOI] [PubMed] [Google Scholar]
- 9.Hegemann M, Kroeger N, Stenzl A, et al. Rare and changeable as a chameleon: paraneoplastic syndromes in renal cell carcinoma. World J Urol 2018; 36: 849–854. [DOI] [PubMed] [Google Scholar]
- 10.Sadeghian H, Vernino S. Progress in the management of paraneoplastic neurological disorders. Ther Adv Neurol Disord 2010; 3: 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang I, Jaros J, Bega D. Paraneoplastic peripheral nervous system manifestations of renal cell carcinoma: a case report and review of the literature. Case Rep Neurol 2017; 9: 22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dalmau J, Rosenfeld M. Paraneoplastic syndromes of the CNS. Lancet Neurol 2008; 7: 327–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wessig C, Klein R, Schneider MF, et al. Neuropathology and binding studies in anti-amphiphysin-associated stiff-person syndrome. Neurology 2003; 61: 195–198. [DOI] [PubMed] [Google Scholar]
- 14.Rosenfeld MR, Titulaer MJ, Dalmau J. Paraneoplastic syndromes and autoimmune encephalitis: five new things. Neurol Clin Pract 2012; 2: 215–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenfeld MR, Dalmau J. Diagnosis and management of paraneoplastic neurologic disorders. Curr Treat Options Oncol 2013; 14: 528–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are contained within the manuscript, and any missing details will be available from the corresponding author on reasonable request.