Abstract
Endobronchial metastasis occurs in only 2%–5% of non-pulmonary cancers. Here we report on an 84-year-old woman who presented with breathlessness and light-headedness while on holiday in Australia, 2 years post-treatment for endometrial cancer. Initial CT pulmonary angiogram identified a soft tissue mass in the left hemithorax. A chest radiograph performed after repatriation was consistent with a large left pleural effusion, but bedside ultrasound showed a lobulated mass involving the left hemidiaphragm. A pleural procedure in the traditional ‘triangle of safety’ would have resulted in inadvertent puncture of the underlying mass. Serial imaging confirmed the mass was rapidly progressing, and metastatic malignant mixed Mullerian endometrial carcinoma was diagnosed by endobronchial biopsy. A tunnelled intrapleural catheter was inserted for symptom relief, and the patient deteriorated and died at home 2 weeks later. To our knowledge, this is the first case of endobronchial metastasis from malignant mixed Mullerian tumour of the uterus.
Keywords: respiratory medicine, radiology, gynecological cancer
Background
Endobronchial metastasis is rare, occurring in only 2%–5% of non-pulmonary cancers, and to our knowledge this is the first case of endobronchial metastasis from malignant mixed Mullerian tumour (MMMT) of the uterus. However, as well as the interest of rarity, this case highlights the importance of using bedside ultrasound before performing pleural procedures.
Case presentation
An 84-year-old woman presented with breathlessness and light-headedness while on holiday in Australia in 2015. She had a chronic cough productive of mucoid sputum, but no history of weight loss, haemoptysis, chest pain or fever. Medical history included right breast ductal carcinoma in situ (resected in 2009) and stage IIIC endometrial carcinoma. The latter was treated with total abdominal hysterectomy and bilateral salpingo-oophorectomy in 2012, followed by standard adjuvant treatment. Six cycles of adjuvant chemotherapy with carboplatin and paclitaxel were given (completed in May 2013). She then underwent radical radiotherapy to the pelvis (45 Gy in 25 fractions in June 2013) with subsequent brachytherapy to vaginal vault (10 Gy in 2 fractions), completing treatment in July 2013.
Investigations
A CT pulmonary angiogram (CTPA) excluded pulmonary emboli, but revealed a soft tissue mass in the left hemithorax, extending below the diaphragm.
On being repatriated to the UK, her admission chest radiograph was reported as showing ‘a large left-sided pleural effusion causing mediastinal shift towards the right’ (figure 1A). Bedside ultrasound, however, showed a large lobulated mass on the left side involving the left hemidiaphragm, with thickened and irregular pleura (figure 1B). Appreciable pleural fluid was only localised superiorly, at the second intercostal space in the axilla. Subsequent CT of the chest and abdomen confirmed the presence of the mass in the left hemithorax, with a large left pleural effusion located superiorly above the mass and causing mediastinal shift to the right (figure 1C). The mass extended through the left hemidiaphragm into the left upper quadrant (figure 1D), and had rapidly progressed over 20 days since the original CTPA. There were no features of pelvic recurrence of the endometrial cancer.
Figure 1.
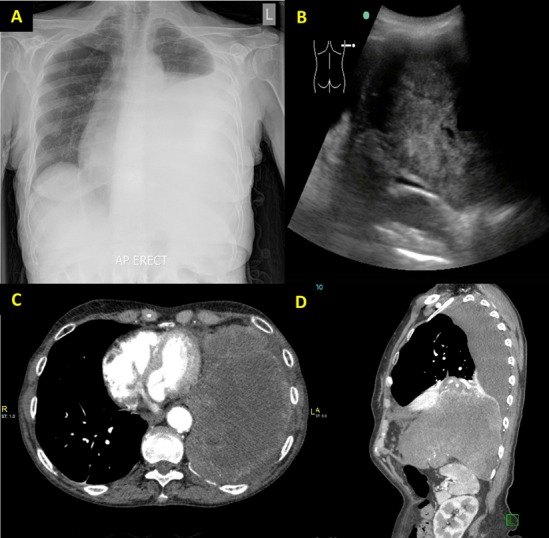
(A) Posteroanterior chest radiograph reported as ‘large left-side pleural effusion causing mediastinal shift towards the right’. (B) Bedside ultrasound showing a large lobulated mass on the left side. (C) CT (axial view) showing a large lobulated soft tissue mass in the left hemithorax. (D) CT (sagittal view) of the thorax showing the mass had infiltrated through the left hemidiaphragm into the left upper quadrant.
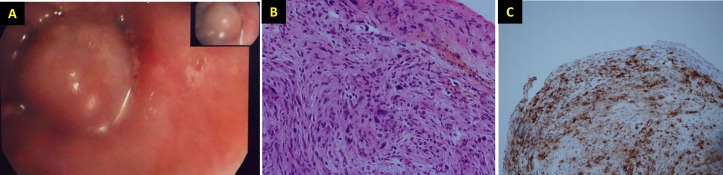
Pleural fluid cytology showed atypical cells with staining for cytoplasmic Wilms’ tumour 1 (WT1), suggesting pleural involvement by a malignant process. Subsequent bronchoscopy revealed a well-circumscribed, smooth-surfaced lesion occluding the lumen of the left main bronchus (figure 2A). Endobronchial biopsy confirmed a metastatic malignant mixed Mullerian endometrial carcinoma with sarcomatoid differentiation (figure 2B,C).
Figure 2.
(A) Image taken at bronchoscopy: well-circumscribed, smooth-surfaced lesion occluding the lumen of the left main bronchus, with no evidence of erosion through the bronchus. (B) Histology slide of the bronchial biopsy: malignant mixed Mullerian (also known as carcinosarcoma) endometrial carcinoma with rhabdoid heterologous differentiation (H&E stain). (C) Desmin immunostain is positive in the rhabdoid malignant cells.
Treatment
Substantial relief of breathlessness was initially achieved through ultrasound-guided therapeutic aspiration of a litre of blood-stained fluid. However, rapid reaccumulation of pleural fluid necessitated insertion of a tunnelled intrapleural catheter prior to discharge.
Outcome and follow-up
She declined progressively and died at home 2 weeks later with support from community palliative care team.
Discussion
Endobronchial metastasis occurs in only 2%–5% of non-pulmonary cancers, and to our knowledge this is the first case of endobronchial metastasis from MMMT of the uterus.
Uterine MMMT is a very rare and aggressive tumour, comprising only 1%–2% of all endometrial cancers. It carries a poor prognosis, with none surviving beyond 2 years for stage III and IV of the disease.1 It is often diagnosed at an advanced stage, with 85% of distant metastases occurring within 3 years of curative treatment,2 as in this case.
The presence of WT1 has been associated with poorer outcomes and higher grade tumours.3 Adjuvant pelvic radiotherapy has been found to decrease the risk of pelvic recurrence (as in our patient) and confer a longer mean time to distant metastases after hysterectomy.4
Although the chest radiographic features were suggestive of a massive effusion, blind pleural procedure in the traditional ‘triangle of safety’ would have resulted in inadvertent puncture of the underlying solid mass. This case illustrates the importance of using bedside ultrasound for pleural procedures, as recommended in the British Thoracic Society guidelines, to reduce the complication rate.
Learning points.
This case illustrates the importance of using bedside ultrasound for pleural procedures, as recommended in the British Thoracic Society guidelines, to reduce the complication rate.
Endobronchial metastasis occurs in only 2%–5% of non-pulmonary cancers.
A medical history of uterine malignant mixed Mullerian tumour should prompt careful evaluation, as although rare, it is aggressive when present.
Acknowledgments
Rand Hawari for providing the histology slidesand Louise Haine for the CT images
Footnotes
Contributors: VB: planned, designed, wrote, revised critically and approved the final manuscript. LP: wrote, revised critically and approved the final manuscript. RJB: supervised, revised critically and approved the final manuscript. JA: discussed planning, supervised, revised critically and approved the final manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Ho SP, Ho TH. Malignant mixed Mullerian tumours of the uterus-a ten-year experience. Singapore Med J 2002;43:452–6. [PubMed] [Google Scholar]
- 2. Lee YJ, Jung EJ, Lee SH, et al. Concurrent diagnosis of pulmonary metastasis of malignant mixed müllerian tumor and small cell lung cancer. Tuberc Respir Dis 2012;73:56–60. 10.4046/trd.2012.73.1.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dupont J, Wang X, Marshall DS, et al. Wilms Tumor Gene (WT1) and p53 expression in endometrial carcinomas: a study of 130 cases using a tissue microarray. Gynecol Oncol 2004;94:449–55. 10.1016/j.ygyno.2004.05.014 [DOI] [PubMed] [Google Scholar]
- 4. Callister M, Ramondetta LM, Jhingran A, et al. Malignant mixed Müllerian tumors of the uterus: analysis of patterns of failure, prognostic factors, and treatment outcome. Int J Radiat Oncol Biol Phys 2004;58:786–96. 10.1016/S0360-3016(03)01561-X [DOI] [PubMed] [Google Scholar]