Abstract
Enamel opacity on anterior teeth can be prejudicial for the aesthetic appearance of affected patients. Patients with molar incisor hypomineralisation, for example, present opacities that can range from discrete white mottling to extensive yellow-brown discolourations. They can request a treatment to improve their aesthetic conditions. Many techniques have been considered to manage this condition. Wright developed a technique called etch–bleach–seal, which showed promising results for the management of anterior enamel opacities. The aims of this report are to present this technique and to analyse its benefits and inconveniences.
Keywords: dentistry and oral medicine, mouth, paediatrics
Background
Enamel opacity is the clinical evidence of a development deficiency of the mineral content of the enamel.1 These defects can be the result of different types of anomalies (eg, fluorosis, amelogenesis imperfecta, molar incisor hypomineralisation (MIH), sequelae of trauma to the primary teeth).2 Paediatric dentists are increasingly faced with MIH.3 MIH is defined as a hypomineralisation of systemic origin of one to four permanent first molars frequently associated with affected incisors.4 5 The prevalence of MIH lies somewhere between 2.8% and 25%.3 The aetiology appears to be multifactorial, including environmental, medical, systemic and genetic factors.6–9 Opacities can range from discrete white mottling to generalised yellow-brown discolourations.10
Abstention is a possible choice.5 But the occurrence of MIH causing small white defects to yellow-brown opacity on the anterior sector may have psychological impact on young patients.10 Treatment should be considered if the patient requests it, but the benefit balance risk should also be considered.5 Composite resin restoration after removing the defect with a bur is a possible solution.11 The macroabrasion technique, also called mega-abrasion or megabrasion, was described by Magne11 and consists of selectively eliminating opacity by using invasive instrumentation (drilling/sandblasting). This involves a composite restoration. Megabrasion is indicated for all enamel defects but is a poor conservative approach.11 12 Yellow-brown MIH defects can be managed using this technique, which yields a complete aesthetic restoration, but there is no tissue preservation. In children and adolescents, non-invasive conservative therapeutic approaches (also called minimally invasive dentistry) must first be considered.13 14
Microabrasion is a non-invasive option. It consists of applying an acid–abrasive gel, which reshapes part of the enamel (maximum, 200 µm of depth). This is a combination of chemical and mechanical abrasion, and this technique is a good approach for light-to-moderate fluorosis.15 16 However, in MIH, due to the deep localisation of the defect, microabrasion does not often improve the aesthetic, particularly when the opacity is yellow-brown (author opinion; lack of publication).
Another conservative approach is infiltration with resin-based material, Icon (DMG, Hamburg, Germany).13 17 This technique was first described for the treatment of proximal enamel caries by erosion and then infiltration. On anterior teeth, the first step is to use hydrochloric acid to eliminate the surface layer and to allow access to the body of the lesion. The second step is an infiltration of the defect with Icon Resin Infiltrant. The aim is to modify the refractive index (IR Icon=1.44) close to the healthy enamel to improve the aesthetic. This treatment is indicated for external white opacities (fluorosis).17 In MIH, resin infiltration may slightly improve the aesthetic when the opacity is small and white. However, for yellow-brown defects, this technique does not yield good results (author opinion; lack of publication).
The etch–bleach–seal technique is also part of the conservative approach.18 The etch–bleach–seal allows tissue preservation, which is particularly interesting for our young patients. This technique was proposed for yellow-to-brown opacities.18 It is the only approach that acts on the colour of the defect.
There is a lack of publications about conservative approaches to treat anterior teeth affected by MIH, and their aesthetic gain and impact.
The aim of this article is to present the etch–bleach–seal technique and to propose some improvements to the original protocol, based on three case reports.
Case presentation
In this article, we report the case of three patients followed in the paediatric department of the Hospital of Nantes (France).
Patient 1
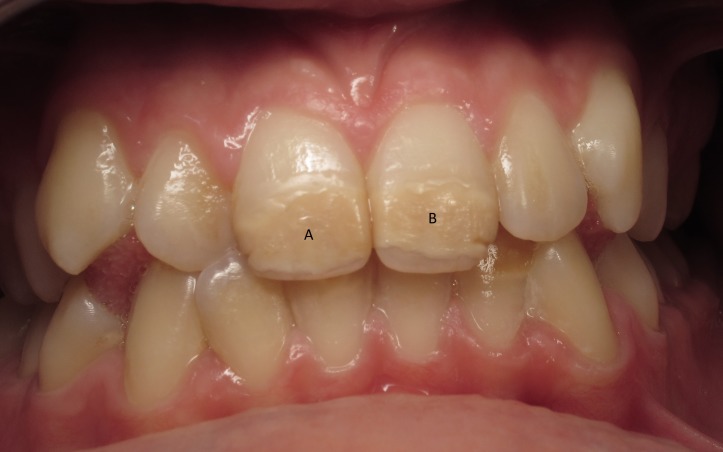
An 11-year-old boy who was unsatisfied with the appearance of his anterior teeth, due to an MIH yellow-brown defect, particularly in the upper central incisors (figure 1).
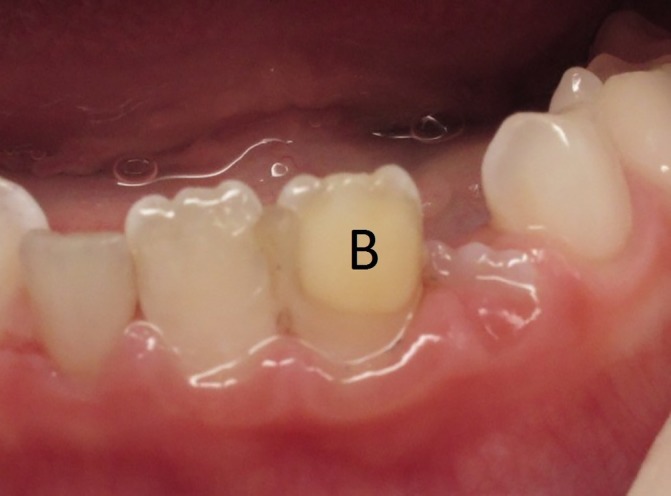
Figure 1.
Patient 1: initial clinical situation before treatment (A,B: the central area defects are brown).
Patient 2
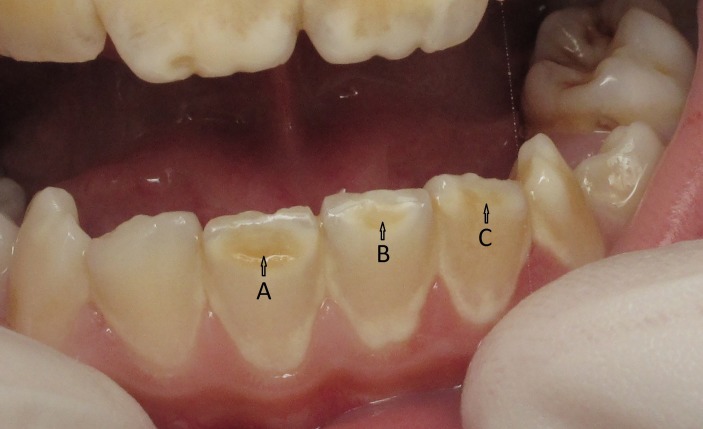
A 12-year-old girl who also presented a yellow-brown defect due to MIH but on three of the lower incisors, with aesthetic concern (figure 2).
Figure 2.
Patient 1: initial clinical situation before treatment (A,B: the central area defects are brown).
Patient 3
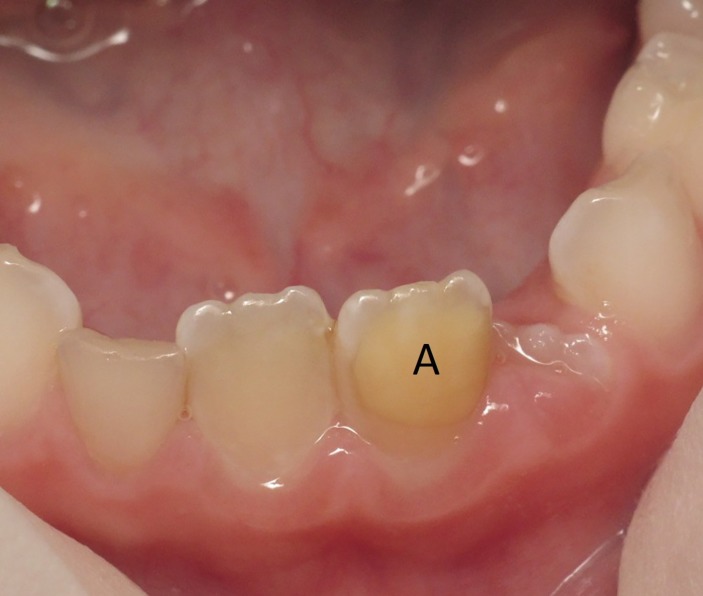
A 7-year-old girl who had a large yellow-brown defect due to MIH localised on the left lower central incisor, with aesthetic concern (figure 3).
Figure 3.
Patient 3: initial clinical situation before treatment (A: the defect is yellow, with clearly defined limits).
Treatment
The etch–bleach–seal technique was first described by Wright.18 He indicated this technique for treating yellow-brown enamel opacities. The aetiology of those opacities was not detailed, but the two case reports look like MIH.
This technique requires a rubber dam, a rubber cup and flour of pumice, 37% phosphoric acid, 5% sodium hypochlorite, a cotton applicator and sealant.
The clinical procedure described by Wright requires three steps.18
First step: tooth preparation
The teeth are cleaned with flour of pumice using a rubber cup to remove all plaque and any extrinsic surface discolourations. The teeth are then isolated with a rubber dam, and each tooth is ligatured to protect soft tissues and to allow a complete access to the lesions.
Second step: etch and bleach
To allow better penetration of the bleaching agent, the enamel surface is etched for 60 s with 37% phosphoric acid. After rinsing, 5% sodium hypochlorite is applied to the entire surface of the defect using a cotton applicator. The bleach is continuously reapplied to the tooth as it evaporates. The discolouration can be observed to diminish over 5 to 10 min. If little or no change has occurred in 10 min, the tooth should be re-etched for 60 s, rinsed and bleached another time for 10 min.
The goal of this stage is to achieve localised bleaching on a vital tooth using sodium hypochlorite. The goal is to remove coloured proteins from the enamel surface at the origin of these brown and yellow opacities.
Moreover, the use of sodium hypochlorite does not cause dental sensitivity or gingival irritation, which may be a problem with peroxide-based bleaching materials.18–20 Furthermore, sodium hypochlorite is easy to implement.
Third step: etch and seal
To prevent organic material from re-entering the porous and hypomineralised enamel, the etched and bleached teeth can be sealed after achieving the optimal bleach result. Sealing of the hypomineralised enamel is accomplished by rinsing and drying the tooth to remove all bleaching agent, etching the tooth for 30 s with 37% phosphoric acid, rinsing with water and treating the enamel surface with flow sealant.
The first interest of this step is, by using a low viscosity resin, to allow easier infiltration of an affected surface to prevent the infiltration of coloured proteins. Furthermore, the modification of the refraction index allowed by the flow sealant yields aesthetic gain.
For patient 1
The etch–bleach–seal technique alone allowed the modification of the yellow-brown opacities into white defects, which were more easily accepted by our 11-year-old boy. He was much more satisfied with his anterior tooth appearance (figure 4).
Figure 4.
Patient 1: clinical situation after the etch–bleach–seal technique (C,D: note the colour change of the central area defect: brown to yellow-white).
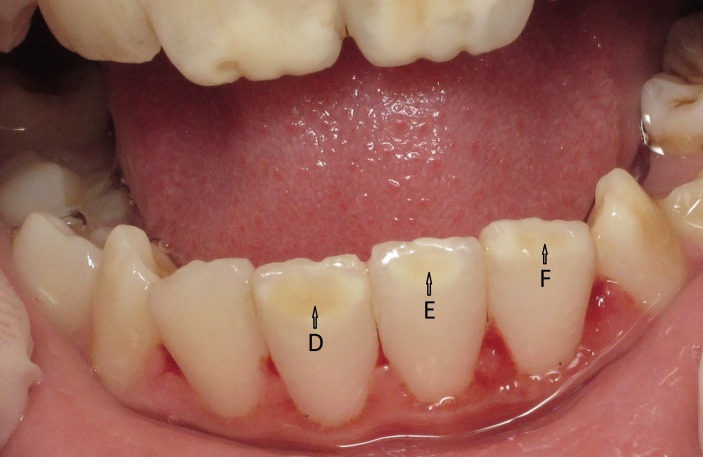
For patient 2
A microabrasion stage was first applied using Opalustre (Ultradent Products, South Jordan, Utah, USA) and was followed by the etch–bleach–seal technique. The result showed visible improvement, although the defect was still present (figure 5).
Figure 5.
Patient 2: clinical situation after microabrasion and the etch–bleach–seal technique (Note the colour change of the central area defect; D: yellow-brown to yellow-white, and E,F: yellow to yellow-white).
For patient 3
After a combination of microabrasion and the etch–bleach–seal technique, the result was still insufficient (figure 6). A second stage was performed with a combination of three techniques on a ‘microabrasion/etch–bleach step/Icon (DMG) infiltration’ order. We observe an improvement, with less colour contrast (figure 7).
Figure 6.
Patient 3: clinical situation after microabrasion and the etch–bleach–seal technique (B: The defect is white, with clearly defined limits; note the colour contrast between the defect and the adjacent tissue).
Figure 7.

Patient 3: clinical situation after microabrasion, the etch–bleach step and the Icon infiltration protocol (C: The defect had undefined limits at the bottom; note the absence of colour contrast between the defect and the adjacent tissue).
Outcome and follow-up
In young patients, treatment options should particularly consider age, cooperation and tissue preservation.
The etch–bleach–seal technique, microabrasion and Icon infiltration are non-invasive techniques. Their protocol is easily and quickly applied, and thus is particularly appropriate to gain a young patient’s cooperation.
Despite the simplicity of these three techniques, we need good patient cooperation; they require at least a 30 min appointment, which may be complicated for some young people. Those techniques require a rubber dam because of some aggressive materials used. However, sometimes, the stage of the tooth eruption prevents the setting up of a rubber dam. Consequently, treatment must be delayed. With all of these non-invasive techniques, the aesthetic gain is variable and depends on the depth and shape of the enamel defect.13 Indeed, it seems that the deeper the enamel defect is, the less aesthetic the result. Aesthetic gain is not guaranteed; thus, it seems important to inform our young patients and their parents regarding the possibility of failure.
The worst yellow-brown discolourations can be converted to a white discolouration, which are more aesthetically acceptable for the patient. However, this result should be announced to be understood, so that the patient does not expect a perfect result.
Discussion
After managing the risk of dental caries and functional treatment, the dentist treating MIH is generally faced with the goal of improving the aesthetics when the anterior sector is damaged. The internal localisation of MIH presents a real challenge to establishing a treatment plan in conformity with the notion of tissue preservation.13
The key point to obtaining a good result on anterior teeth is the accessibility of the entire defect. When we apply the original protocol described by Wright,18 we may not have access to the entire lesion and must then modify the Wright protocol.
Microabrasion can be done before the etch–bleach–seal technique. It seems to reduce opacities and to be compatible with tissue preservation and may allow better access to the lesion,13 which provides a better final result. On the downside, we sometimes have to use a flow composite because of the quantitative defects that microabrasion can create on soft enamel. Furthermore, in the case of yellow-brown discolourations, we do not manage to obtain a complete rehabilitation, as seen in patient 2, for whom the result was not perfect, even with visible improvement.
Alternatively, the use of Icon after the etch–bleach–seal technique can be couple, but the result is not convincing for MIH, due to the shape and depth of the enamel defect. It appears that the infiltration of Icon failed to reach the entire defect and that the refractive index was consequently not modified.
The three techniques can also be combined in a ‘microabrasion/etch–bleach step/Icon infiltration’ order. We have obtained good results with this combination, which allows better access to the lesion. It appears to be our best choice for difficult cases, when we decide to use only non-invasive therapy. In patient 3 (a 7-year-old girl), we did not achieve complete aesthetic restoration, but the patient and her parents were satisfied with the result.
If the previous combination does not succeed to provide the patient an aesthetically acceptable restoration of the enamel defect, the next step may be the use of macroabrasion instead of microabrasion in the precedent combination to allow definitive access to the entire defect. In this case, the Icon infiltration can do its part and reaches the lesion in depth. This technique called deep infiltration was described by Attal and coworkers.14 The downside will of course be the need for a composite restoration due to the drilling or sandblasting, even if the loss of enamel tissue is reduced in comparison with entire removal of the defect using a bur.
This possible combination of therapeutic techniques had to be used, based on the enamel defect and the aetiology. It is then particularly important to know the physical properties of each enamel defect, to apply the appropriate treatment. A therapeutic gradient must match the less-invasive technique to the most superficial defect on one side and the more-aggressive technique to the deeper defect on the opposite side. Our job and responsibility are to apply this gradient to each case we have to treat.
The etch–bleach–seal technique is the only non-invasive approach indicated for the treatment of yellow-brown opacities.
The etch–bleach–seal technique is easy to apply, and the required materials are present in the dental office most of the time. However, the aesthetic gain is not guaranteed even if we respect the indication and stages. In case of MIH, the deepest localisation of the defect complicates the management, and restoration of the aesthetics is not complete.
In young patients, the etch–bleach–seal technique can be considered a first step for treating MIH yellow-brown opacities, but it had to be combined with other techniques, presented in this paper, to achieve better results.
Learning points.
The etch–bleach–seal technique may be indicated for the treatment of anterior yellow-brown opacities in molar incisor hypomineralisation (MIH).
The combination of three techniques ‘microabrasion/etch–bleach step/Icon infiltration’ may be useful for the treatment of anterior yellow-brown opacities in MIH.
The aesthetic gain is never guaranteed for anterior yellow-brown opacities in MIH.
Footnotes
TP' and IH contributed equally.
Contributors: IH and SLC have managed the patients. TP and IH have drafted the work. SDT and SLC revised it critically for important intellectual content.
Competing interests: None declared.
Patient consent: Guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Mastroberardino S, Campus G, Strohmenger L, et al. . An innovative approach to treat incisors hypomineralization (MIH): a combined use of casein phosphopeptide-amorphous calcium phosphate and hydrogen peroxide-a case report. Case Rep Dent 2012;2012:1–5. 10.1155/2012/379593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Seow WK. Developmental defects of enamel and dentine: challenges for basic science research and clinical management. Aust Dent J 2014;59(Suppl 1):143–54. 10.1111/adj.12104 [DOI] [PubMed] [Google Scholar]
- 3. Garg N, Jain AK, Saha S, et al. . Essentiality of early diagnosis of molar incisor hypomineralization in children and review of its clinical presentation, etiology and management. Int J Clin Pediatr Dent 2012;5:190–6. 10.5005/jp-journals-10005-1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Weerheijm KL. Molar incisor hypomineralisation (MIH). Eur J Paediatr Dent 2003;4:114–20. [PubMed] [Google Scholar]
- 5. Lygidakis NA, Wong F, Jälevik B, et al. . Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): an EAPD policy document. Eur Arch Paediatr Dent 2010;11:75–81. 10.1007/BF03262716 [DOI] [PubMed] [Google Scholar]
- 6. Alves dos Santos MP, Maia LC. Contemporary approach to dental caries molar incisor hypomineralization: morphological, aetiological, epidemiological and clinical considerations. InTech 2012. [Google Scholar]
- 7. Alaluusua S. Aetiology of molar-incisor hypomineralisation: a systematic review. Eur Arch Paediatr Dent 2010;11:53–8. 10.1007/BF03262713 [DOI] [PubMed] [Google Scholar]
- 8. Crombie F, Manton D, Kilpatrick N. Aetiology of molar-incisor hypomineralization: a critical review. Int J Paediatr Dent 2009;19:73–83. 10.1111/j.1365-263X.2008.00966.x [DOI] [PubMed] [Google Scholar]
- 9. Silva MJ, Scurrah KJ, Craig JM, et al. . Etiology of molar incisor hypomineralization - a systematic review. Community Dent Oral Epidemiol 2016;44:342–53. 10.1111/cdoe.12229 [DOI] [PubMed] [Google Scholar]
- 10. Leal SC, Oliveira TRM, Ribeiro APD. Do parents and children perceive molar-incisor hypomineralization as an oral health problem? Int J Paediatr Dent 2017;27:372–9. 10.1111/ipd.12271 [DOI] [PubMed] [Google Scholar]
- 11. Magne P. Megabrasion: a conservative strategy for the anterior dentition. Pract Periodontics Aesthet Dent 1997;9:389–95. [PubMed] [Google Scholar]
- 12. Amarlal D, Rayen R, Muthu MS. Macroabrasion in pediatric dentistry. J Clin Pediatr Dent 2006;31:9–13. 10.17796/jcpd.31.1.k106m4hu02318382 [DOI] [PubMed] [Google Scholar]
- 13. Denis M, Atlan A, Vennat E, et al. . White defects on enamel: diagnosis and anatomopathology: two essential factors for proper treatment (part 1). Int Orthod 2013;11:139–65. 10.1016/j.ortho.2013.02.014 [DOI] [PubMed] [Google Scholar]
- 14. Attal JP, Atlan A, Denis M, et al. . White spots on enamel: treatment protocol by superficial or deep infiltration (part 2). Int Orthod 2014;12:1–31. 10.1016/j.ortho.2013.12.011 [DOI] [PubMed] [Google Scholar]
- 15. Ardu S, Benbachir N, Stavridakis M, et al. . A combined chemo-mechanical approach for aesthetic management of superficial enamel defects. Br Dent J 2009;206:205–8. 10.1038/sj.bdj.2009.116 [DOI] [PubMed] [Google Scholar]
- 16. Rodrigues I, Simon J, Tirlet G, et al. . Utilisation de la micro-abrasion amélaire contrôlée. Revue Française d’Odontologie Pédiatrique 2006;4:106. [Google Scholar]
- 17. Muñoz MA, Arana-Gordillo LA, Gomes GM, et al. . Alternative esthetic management of fluorosis and hypoplasia stains: blending effect obtained with resin infiltration techniques. J Esthet Restor Dent 2013;25:32–9. 10.1111/j.1708-8240.2012.00527.x [DOI] [PubMed] [Google Scholar]
- 18. Wright JT. The etch-bleach-seal technique for managing stained enamel defects in young permanent incisors. Pediatr Dent 2002;24:249–52. [PubMed] [Google Scholar]
- 19. Sulieman MA. An overview of tooth-bleaching techniques: chemistry, safety and efficacy. Periodontol 2000 2008;48:148–69. 10.1111/j.1600-0757.2008.00258.x [DOI] [PubMed] [Google Scholar]
- 20. Matis BA, Cochran MA, Wang G, et al. . A clinical evaluation of two in-office bleaching regimens with and without tray bleaching. Oper Dent 2009;34:142–9. 10.2341/08-64 [DOI] [PubMed] [Google Scholar]