Abstract
Objective.
To determine associations of adverse childhood experiences (ACE) with adult health care utilization in an underserved, low-income population.
Methods.
Questionnaires on ACE were completed by 38,200 adults (mean age 54), two-thirds African American, recruited from community health centers (CHCs) across 12 Southeastern states. Odds ratios (ORs) and accompanying 95% confidence intervals (CIs) were computed.
Results.
The percentages reporting emergency room visits and doctor’s office visits, with high chronic disease index scores, rose monotonically (ptrend<.001) with rising ACE score. Odds ratios (CIs) for those with four or more vs. zero ACEs were 1.37 (95% CI 1.27–1.47) for 1–10 times and 1.80 (95% CI 1.29–2.52) for more than 10 times ER visits, 1.37 (95% CI 1.18–1.59) for over 10 doctor’s visits, and 2.29 (95% CI 2.06–2.54) for three or more chronic diseases.
Conclusions.
High ACE levels were associated with greater chronic disease burden and greater health care utilization in adulthood. Long-lasting effects from ACE on the health care of underserved populations are indicated. There is an urgent need to train health care providers, patients, and their families on ACE effects and treatments for better health care outcomes.
Keywords: Adverse childhood experiences, ACE, health care utilization, low-income population
Adverse childhood experiences (ACEs) are common, with several reports describing ACEs in over 50% of U.S. population groups.1–5 In the national Behavioral Risk Factor Surveillance Survey, 59% of respondents reported having at least one adverse childhood experience (ACE), and 9% reported five or more ACEs.6–7 In a population-based study from Canada, 72% reported at least one ACE, with 16% reporting three or more.8 Given the prevalence of ACE, a growing number of studies are assessing the effects of ACE exposure on health late into adulthood.
Adverse childhood experiences (ACE) have subsequent impacts on adult health.1–5 The range of adverse health outcomes in adulthood linked to exposure to ACEs include substance abuse,9–11 depression,11–12 cardiovascular disease,7,13–14 diabetes,7,15 cancer,5,16–19 and overall mortality.1,6 Adverse childhood experiences (ACE) effects on adverse health outcomes may be mediated in part through poorer health risk behaviors, with repeated reports of a graded response between the intensity of the ACE experience with the intensity of the risk behavior, and a call for an expanded definition of adversity.20–26
Given the impact on chronic disease burden, ACEs are expected also to affect health care utilization.25,27 The Ontario Health Survey reports that for each additional adverse childhood experience the odds increased for general practitioner use (OR 1.12), health professional use (OR 1.19), and emergency room use (OR 1.29).8 Adverse childhood experiences (ACE) may lead to increased utilization resulting in increased health care costs.8,27–29
It is well known that child maltreatment is more likely to occur in families afflicted by poverty,30–33 and poverty is also associated with poor adult health outcomes.34–39 Given the impact that poverty has on increased burden of disease and its associated health care costs and utilization, it is important to understand other factors that may lead to these untoward health outcomes in underserved populations. Thus, the purpose of our analysis was to determine the relationship of factors associated with adverse childhood experiences and health utilization in a predominantly low-income population drawn from underserved rural as well as urban neighborhoods across the southeastern United States. The analyses also enabled examination of potential differences in ACE effects between Blacks and Whites. Understanding the factors associated with health care utilization may allow for strategies to improve health readiness.
Methods
Study population.
We conducted this analysis using data from the Southern Community Cohort Study (SCCS), a multi-year prospective cohort study of adults, two-thirds African American and the remainder mainly non-Hispanic White enrolled at ages 40–79 during 2002–2009 from 12 Southern states (Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia and West Virginia). Most (85%) of the cohort was recruited at community health centers (CHCs), institutions providing basic health care and preventative services in medically underserved areas, with 15% selected from general population rosters in the same states. Details of the SCCS enrollment have been described previously.40–41 Direct recruitment through CHCs included a large, lower-income, vulnerable segment of society often not included in prior research. The Vanderbilt University Medical Center and Meharry Medical College Institutional Review Boards approved this study and study participants gave their consent.
Survey instruments.
An extensive questionnaire was administered upon enrollment via computer-assisted personal interviews at community health centers or via self-completed questionnaires from the general population sample. The SCCS baseline questionnaire acquired information on the following: demographic characteristics; personal medical history; family medical history; health insurance; emergency room utilization; primary care office visits, hospital utilization; prevalent medical conditions (including chronic diseases); and other miscellaneous factors. Follow-up questionnaires were administered periodically by mail after enrollment. Copies of the questionnaires are available online at https://www.southerncommunitystudy.org/uploads/5/2/7/5/52750661/male_sccs_fu2_survey.pdf. Although much shorter in length than the baseline questionnaire, the follow-up questionnaires offered the opportunity to ascertain additional information not collected at baseline. In the second follow-up questionnaire, initiated in 2012 and concluded in 2015, we included the following 10 questions regarding adverse childhood experiences (ACE) (questionnaire accessed from cdc.gov May 29th, 2012):
When you were growing up, during the first 18 years of life:
Did a parent or other adult in the household often swear at you, insult you, put you down, or humiliate you OR act in any way that made you afraid that you might be physically hurt?
Did a parent of other adult in the household often push, grab, slap, or throw something at you OR ever hit you so hard that you had marks or ever injured?
Did an adult person at least five years older than you ever touch or fondle you or have you touch their body in a sexual way OR try to or actually have oral, anal, or vaginal sex with you?
Did you often feel that no one in your family loved you or thought you were important or special OR your family didn’t look out for each other, feel close to each other, or support each other?
Did you often feel that you didn’t have enough to eat, had to wear dirty clothes, and had no one to protect you OR your parents were too drunk or high to take care of you or take you to the doctor if you needed it?
Were your parents ever separated or divorced?
Was your mother or stepmother often pushed, grabbed, slapped, or had something thrown at her OR sometimes or often kicked, bitten, hit with a fist, or hit with something hard? OR ever repeatedly hit over at least a few minutes or threatened with a gun or knife?
Did you live with anyone who was a problem drinker or alcoholic OR who used street drugs?
Was a household member depressed or mentally ill or did a household member attempt suicide?
Did a household member go to prison?
Response to each ACE item was recorded as a yes or no. A total ACE score was determined by the sum of all “yes” responses, with the maximum possible ACE score of 10. The ACE score was categorized as 0 (no events), 1 (a single event), 2 (two events), 3 (three events), and 4 (four or more events). This questionnaire is a slight modification of the original Felitti questionnaire,3 including three expanded questions on household dysfunction (family support, separation, and divorce) while allowing for the same yes/no responses. This brief 10-point questionnaire was particularly useful for inclusion in the follow-up studies of the Southern Community Cohort Study (SCCS) being conducted with the extensive SCCS questionnaire sent by mail to over 43,000 low-income people who had participated in the baseline study up to 12 years earlier. No formal validation of this questionnaire had been carried out by the time of this study, but a test-retest reliability was carried out by the Felitti co-authors.42
The second follow-up questionnaire also updated health care utilization (including emergency room visits, doctor’s office visits, and hospitalizations), exposure (including current smoking status), health status (including current weight), and health services utilization (including cancer screening).
Statistical analyses.
We utilized data from the 40,584 SCCS participants who completed the second follow-up questionnaire, among whom 40,240 answered the ACE exposure questions. Because of the small numbers of participants in other racial/ethnic groups, we restricted the analyses to the 38,200 African Americans and Whites. In this group, we assessed the variables described below.
Dependent variables.
Three health care-related dependent variables were examined and were categorized as follows:
emergency department (ED) visits in last year (none, one to 10 times, and over 10 times; with none as the reference);
doctor’s office visits last year (none, one to five times, six-10 times, and 11 or more times; with none as the reference); and
current source of medical care (community health center or free clinic; private doctors’ office; emergency room; hospital including Veterans Affairs (VA) or other source; no source; with private doctors’ office as the reference).
Covariates.
The following variables were examined as covariates:
age (in years, at age of interview): three groups (40 – 49, 50 – 59, and 60 – 79 years; with 40–49 year group as the reference);
gender (male vs. female; with male as the reference);
race (White vs. Black; with White as the reference);
education: three groups (less than high school, high school, and more than high school; with less than high school as the reference);
household annual income: four groups (<$15,000, $15,000 – $24,999, $25,000 – $49,999, and ≥$50,000; with <$15,000 as the reference);
marital status (married or living as married with a partner; separated or divorced; single, never been married; widowed; with married or living as married with a partner as the reference);
current smoking (yes vs. no; with no as the reference);
severe obesity (BMI<35; BMI≥35; with BMI< 35 as the reference);
recruitment source (community health center v. general population—mailed and telephoned interview; with general population as the reference);
neighborhood deprivation index (NDI) calculated based on a composite of indices for the census tracts of the participants’ residences at cohort entry (index has been described previously43); and
a chronic disease index (CDI) (using chronic conditions from the Elixhauser comorbidity measures that were available for the SCCS database, and which we categorized to represent the overall disease burden of participants. This burden was trichotomized into the categories used in our analyses to balance the number of participants in each group). The CDI was a summary score based on having a history of diabetes (y=1;n=0); chronic obstructive pulmonary disease (COPD) (y=1;n=0); depression (y=1;n=0); stroke (y=1;n=0); myocardial infarction (y=1;n=0); hypertension (y=1;n=0); cancer (y=1;n=0); and high cholesterol (y=1;n=0). The index was valued from 0 to 8 and was divided into three groups: summary score equal to 0 as group ‘0’, summary score equal 1 or 2 as group ‘1’, and summary score equal 3 – 8 as group ‘2’. Group 0 was used as the reference.
The dependent variables were tested separately for their association with the ACE score categories (0, 1, 2, 3, four or more) by logistic regression models. The model was adjusted with the neighborhood deprivation index, age, gender, race (ref=White), education (ref= less than high school), household annual income (ref=less than $15,000), marital status (ref=married/living with a partner), current smoker (ref=no), severe obesity (ref=BMI<35), chronic disease index (ref=group 0), and recruitment source (ref=general population). We used complete case analysis for all modeling, and kept all variables in each model, regardless of statistical significance; thus the estimates of odds ratios were adjusted for all variables in the model.
Results
Distribution of ACE scores in the population.
A total of 38,200 SCCS participants (African Americans and Whites) completed the ACE questionnaire, and provided information enabling the computation of ACE scores. At least one adverse childhood experience was reported by 54% of adult men and 60% of adult women (Table 1). Adverse experiences were reported across all ACE domains queried, with women reporting at least one event within the categories of abuse (20%), neglect (21%) and household dysfunction (34%), respectively. Corresponding percentages of men were 17%, 14%, and 32%, respectively.
TABLE 1.
PERCENTAGES OF ADULT MEN AND WOMEN RESPONDING “YES” TO THE 10 CHILDHOOD ABUSE QUESTIONS ASKED (N=38200)
| ACE question | Male | Female | pa |
|---|---|---|---|
| N= 12,785 | N= 25,415 | ||
| Abuse | |||
| Verbal abuse | 17 | 20 | <.0001 |
| Physical abuse | 15 | 17 | <.0001 |
| Sexual abuse | 8 | 18 | <.0001 |
| Neglect | |||
| Emotional, unloved | 14 | 21 | <.0001 |
| Unfed, unclothed, neglected | 8 | 8 | .31 |
| Household dysfunction | |||
| Parents separated or divorced | 32 | 34 | .004 |
| Mother had been abused | 11 | 13 | <.0001 |
| Live with alcoholic or drug user | 21 | 25 | <.0001 |
| Depression/mental illness in household | 11 | 16 | <.0001 |
| Household member in prison | 13 | 11 | <.001 |
| Total (answered yes to any question) | 54 | 60 | <.0001 |
Notes:
Chi-Square test
Among all respondents, 22% reported one event, 11% reported two events, 7% reported three events, and 18% reported four or more ACE events (Table 2). The chi-square tests showed that the ACE score group (0, 1, 2, 3, four or more) was associated (p<.0001) with most of the variables in Table 2, with participants who reported having four or more ACEs being more often younger, female, poorer, and separated/divorced. Few differences, however, were seen by education level and recruitment source. The racial differences were such that Blacks were somewhat more likely to report any ACE but less likely to report four or more such experiences.
TABLE 2.
PERCENTAGE DISTRIBUTION OF ACE SCORES ACCORDING TO DEMOGRAPHIC INDICES AND RECRUITMENT SOURCE
| Variables | ACE score | |||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4+ | ||
| N=16701 | N=8823 | N=4590 | N=2940 | N=7186 | pa | |
| All | 42 | 22 | 11 | 7 | 18 | |
| Age (Years, mean±SD) | 54.8±9.0 | 52.9±8.5 | 52.1±8.1 | 51.3±7.9 | 50.4±7.5 | |
| Age group | ||||||
| 40 to 49 (N=15964) | 33 | 22 | 12 | 9 | 23 | <.0001 |
| 50 to 59 (N=14990) | 43 | 22 | 12 | 7 | 17 | |
| 60 to 79 (N=9286) | 54 | 22 | 9 | 5 | 10 | |
| Race | ||||||
| White (N=13997) | 42 | 19 | 11 | 7 | 21 | <.0001 |
| African American (N=24203) | 42 | 24 | 12 | 7 | 16 | |
| Gender | ||||||
| Male (N=13480) | 45 | 22 | 11 | 7 | 14 | <.0001 |
| Female (N=26760) | 40 | 22 | 12 | 8 | 20 | |
| Household Income ($/Y) | ||||||
| Less than $15,000 (N=17360) | 37 | 22 | 11 | 8 | 22 | <.0001 |
| $15,000 – <$25,000 (N=7599) | 41 | 23 | 12 | 7 | 18 | |
| $25,000 – <$50,000 (N=6380) | 44 | 23 | 11 | 7 | 15 | |
| $50,000 + (N=5979) | 49 | 22 | 11 | 6 | 11 | |
| Education | ||||||
| < High School (N=8770) | 40 | 23 | 11 | 7 | 18 | .046 |
| High School (N=12299) | 42 | 22 | 11 | 7 | 18 | |
| > High School (N=18332) | 41 | 22 | 12 | 7 | 18 | |
| Marital status | ||||||
| Married/living with a partner (N=15245) | 47 | 21 | 11 | 6 | 15 | <.0001 |
| Separated/divorced (N=11572) | 34 | 22 | 12 | 9 | 22 | |
| Widowed (N=6725) | 38 | 23 | 12 | 8 | 19 | |
| Single (N=5994) | 47 | 21 | 10 | 7 | 15 | |
| Neighborhood deprivation index group (Quartile) | ||||||
| Q1 (N=5272) | 45 | 21 | 11 | 7 | 17 | <.0001 |
| Q2 (N=6922) | 41 | 21 | 12 | 7 | 19 | |
| Q3 (N=8884) | 42 | 21 | 11 | 7 | 19 | |
| Q4 (N = 18394) | 40 | 23 | 12 | 7 | 17 | |
| Recruitment Source | ||||||
| Community Health Center(N=30753) | 40 | 22 | 11 | 8 | 19 | <.0001 |
| General population(N=9485) | 47 | 21 | 11 | 7 | 14 | |
Notes:
Chi-Square test
Emergency room visits and ACE score.
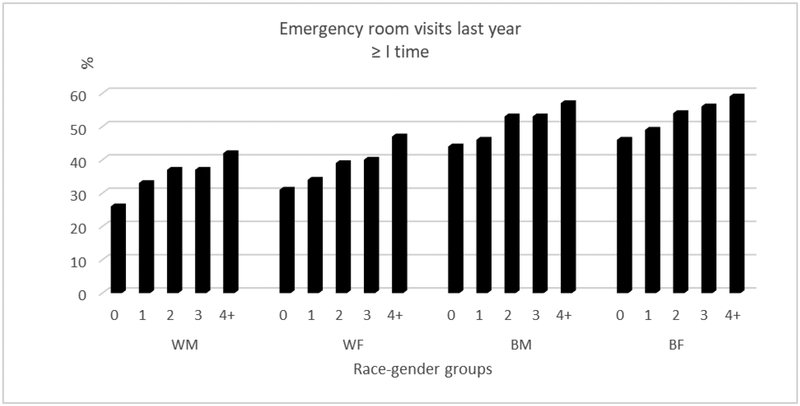
The percentage of emergency room visits in the past year (once or more than once) rose steadily with increasing ACE score in race-gender groups (Figure 1). The prevalence of emergency room visits was nearly 16% higher in Whites and 13% higher in Blacks among those reporting four or more compared with no ACEs.
Figure 1.
Relationship between adverse childhood experiences with emergency room visits (≥ 1 time) in the past year by race-gender groups.
Notes:
WM: White male
WF: White female
BM: Black male
BF: Black female
Doctor’s office visits and ACE score.
The percentage with 11 or more doctor’s office visits in the past year rose steadily with increasing ACE score among all race-gender groups, with prevalence nearly double in Whites (16% vs. 7% in males, 18% vs. 10% in females), and elevated to a somewhat lesser extent among Blacks (13% vs. 9% in males, 15% vs. 11% in females) reporting four or more compared with no ACEs (Table 3).
TABLE 3.
PERCENTAGE DISTRIBUTION OF ADULT HEALTH CARE FACILITY USAGE VARIABLES AMONG WHITE MEN, WHITE WOMEN, BLACK MEN AND BLACK WOMEN - BY ACE SCORE
| Health care facility usage behaviors | ACE score | |||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4+ | pa | |
| Doctor’s office visit last year | ||||||
| White males | N=2390 | N=941 | N=461 | N=300 | N=715 | |
| None | 12 | 11 | 10 | 11 | 11 | <.0001 |
| 1 – 5 times | 67 | 62 | 62 | 59 | 55 | |
| 6 – 10 times | 14 | 16 | 19 | 19 | 18 | |
| ≥ 11 times | 7 | 11 | 8 | 11 | 16 | |
| White females | N=3302 | N=1601 | N=987 | N=700 | N=2087 | |
| None | 6 | 7 | 8 | 7 | 7 | <.0001 |
| 1 – 5 times | 65 | 62 | 58 | 53 | 54 | |
| 6 – 10 times | 18 | 20 | 21 | 23 | 21 | |
| ≥ 11 times | 10 | 11 | 12 | 17 | 18 | |
| Black males | N=3044 | N=1789 | N=879 | N=493 | N=980 | |
| None | 14 | 16 | 13 | 16 | 15 | <.001 |
| 1 – 5 times | 61 | 58 | 58 | 56 | 53 | |
| 6 – 10 times | 16 | 16 | 17 | 17 | 19 | |
| ≥ 11 times | 9 | 10 | 12 | 10 | 13 | |
| Black females | N=6074 | N=3603 | N=1797 | N=1092 | N=2504 | |
| None | 6 | 7 | 6 | 7 | 8 | <.0001 |
| 1 – 5 times | 63 | 60 | 58 | 55 | 53 | |
| 6 – 10 times | 21 | 22 | 23 | 25 | 25 | |
| ≥ 11 times | 11 | 12 | 13 | 13 | 15 | |
| Current source of medical care | ||||||
| White males | N=2348 | N=919 | N=449 | N=287 | N=695 | |
| Community health center or free clinic | 10 | 15 | 14 | 15 | 20 | <.0001 |
| Private doctor’s office | 75 | 69 | 67 | 62 | 55 | |
| Emergency room | 1 | 1 | 1 | 1 | 2 | |
| Hospital or other source | 12 | 12 | 15 | 14 | 17 | |
| No source | 2 | 3 | 3 | 6 | 5 | |
| White females | N=3349 | N=1604 | N=986 | N=688 | N=2067 | |
| Community health center or free clinic | 18 | 21 | 21 | 25 | 28 | <.0001 |
| Private doctor’s office | 77 | 73 | 71 | 66 | 62 | |
| Emergency room | 1 | 1 | 1 | 1 | 2 | |
| Hospital or other source | 3 | 3 | 4 | 5 | 6 | |
| No source | 2 | 2 | 3 | 3 | 3 | |
| Black males | N=3114 | N=1775 | N=844 | N=487 | N=947 | |
| Community health center or free clinic | 30 | 32 | 32 | 30 | 33 | <.0001 |
| Private doctor’s office | 41 | 37 | 34 | 32 | 29 | |
| Emergency room | 4 | 5 | 5 | 7 | 7 | |
| Hospital or other source | 22 | 23 | 25 | 28 | 27 | |
| No source | 3 | 3 | 4 | 3 | 5 | |
| Black females | N=6195 | N=3633 | N=1775 | N=1098 | N=2418 | |
| Community health center or free clinic | 34 | 36 | 38 | 36 | 37 | <.0001 |
| Private doctor’s office | 55 | 53 | 50 | 49 | 47 | |
| Emergency room | 2 | 2 | 2 | 4 | 4 | |
| Hospital or other source | 7 | 7 | 8 | 8 | 10 | |
| No source | 2 | 2 | 2 | 3 | 3 | |
| Chronic disease index | ||||||
| White males | N=2455 | N=971 | N=472 | N=308 | N=744 | |
| Group 0 (index=0) | 22 | 19 | 19 | 19 | 17 | <.0001 |
| Group 1 (index=1,2) | 53 | 55 | 54 | 51 | 47 | |
| Group 2 (index=3,4,5,6,7,8) | 24 | 26 | 27 | 31 | 35 | |
| White females | N=3460 | N=1659 | N=1030 | N=727 | N=2171 | |
| Group 0 (index=0) | 21 | 20 | 15 | 14 | 12 | <.0001 |
| Group 1 (index=1,2) | 54 | 53 | 56 | 54 | 49 | |
| Group 2 (index=3,4,5,6,7,8) | 25 | 27 | 29 | 32 | 39 | |
| Black males | N=3366 | N=1929 | N=937 | N=535 | N=1067 | |
| Group 0 (index=0) | 24 | 27 | 25 | 27 | 23 | .29 |
| Group 1 (index=1,2) | 56 | 53 | 54 | 53 | 56 | |
| Group 2 (index=3,4,5,6,7,8) | 19 | 20 | 21 | 21 | 21 | |
| Black females | N=6692 | N=3880 | N=1923 | N=1184 | N=2689 | |
| Group 0 (index=0) | 16 | 17 | 17 | 17 | 14 | <.0001 |
| Group 1 (index=1,2) | 62 | 60 | 58 | 54 | 55 | |
| Group 2 (index=3,4,5,6,7,8) | 22 | 23 | 24 | 29 | 31 | |
Notes:
Chi-Square test
Source of medical care and ACE score.
Most individuals reported that their usual source of medical care was a private doctors’ office, although Blacks were more likely than Whites to report community clinics or, especially for men, hospitals. The use of private doctors’ offices declined as the ACE exposure increased, and the percentage selection was significantly lower in participants with four or more ACE exposures than that with no ACE exposure in all race-gender groups (White men: 55% vs. 75%; White women: 62% vs. 77%; Black men: 29% vs. 41%; Black women: 47% vs. 55%; all p<.0001) (Table 3).
Chronic Disease Index and ACE score.
The Chronic Disease Index (CHI) indicated that among those with no ACEs about half of the participants reported one or two chronic diseases and about one fourth reported three or more comorbid conditions at cohort entry. The percentage with three or more chronic diseases increased with rising ACE exposure, with the increase significantly higher than among those with no ACE exposure in all groups except Black men (Table 3).
Odds of type of health care use and ACE scores.
Table 4 shows adjusted ORs and CIs of health care facility usage behaviors according to ACE score after adjustment for the multiple covariates in the regression model. The odds of having an emergency room visit one to 10 times, or more than 10 times in the past year, rose steadily with increasing ACE score, with ORs of being a participant with four or more vs. no ACEs of 1.37 (95% CI 1.27–1.47) for one to 10 times, and 1.80 (95% CI 1.29–2.52) for more than 10 times. The odds of having 11 times or more visits to the doctor’s office last year rose with increasing ACE score, with ORs of being a participant with four or more vs. no ACEs of 1.37 (95% CI 1.18–1.59). The odds of having one or two, or more than two, chronic diseases rose steadily with increasing ACE score, with ORs of having one or two chronic diseases among those with four or more vs. no ACEs of 1.40 (95% CI 1.27–1.53), and with ORs of having more than two chronic disease participants among those with four or more vs. no ACEs of 2.29 (95% CI 2.06–2.54). Relative to choosing a private doctors’ office, the odds of choosing a community health center/free clinic, emergency room, hospital/other source, or even no source rose with increasing ACE score, with ORs among those with four or more vs. no ACEs of 1.22 (95% CI 1.12–1.32), 1.50 (95% CI 1.21–1.86), 1.50 (95% CI 1.34–1.69), 1.44 (95% CI 1.16–1.77) for choosing community health center/free clinic, emergency room, hospital/other source, and no source, respectively.
TABLE 4.
ADJUSTEDa ODDS RATIOS (AND 95% CI) OF HEALTH CARE FACILITY USAGE BEHAVIOR PREVALENCE ACCORDING TO ACE SCORE
| Health care facility usage behaviors | ACE score | |||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ≥4 | P for trend | |
| Emergency room visits last year (relative to never) | ||||||
| 1–10 times | 1.0 (ref) | 1.07 (1.01–1.15) | 1.30 (1.20–1.41) | 1.25 (1.13–1.37) | 1.37 (1.27–1.47) | <.0001 |
| >10 times | 1.0 (ref) | .85 (.58–1.23) | 1.32 (.87–2.02) | 1.50 (.95–2.38) | 1.80 (1.29–2.52) | <.0001 |
| Doctor’s office visits last year (relative to never) | ||||||
| 1–5 times | 1.0 (ref) | .95 (.86–1.07) | 1.01 (.87–1.16) | .91 (.77–1.07) | .90 (.80–1.02) | .020 |
| 6–10 times | 1.0 (ref) | 1.01 (.89–1.15) | 1.17 (1.00–1.38) | 1.18 (.98–1.43) | 1.11 (.97–1.28) | .09 |
| ≥ 11 times | 1.0 (ref) | 1.06 (.92–1.22) | 1.22 (1.02–1.46) | 1.21 (.98–1.49) | 1.37 (1.18–1.59) | <.0001 |
| Current source of medical care (relative to private doctors’ office) | ||||||
| Community health center/free clinic | 1.0 (ref) | 1.10 (1.02–1.19) | 1.15 (1.04–1.26) | 1.21 (1.08–1.36) | 1.22 (1.12–1.32) | <.0001 |
| No source | 1.0 (ref) | 1.20 (.98–1.47) | 1.34 (1.05–1.71) | 1.49 (1.12–1.97) | 1.44 (1.16–1.77) | <.0001 |
| Emergency room | 1.0 (ref) | 1.00 (.81–1.25) | 1.13 (.87–1.48) | 1.61 (1.22–2.13) | 1.50 (1.21–1.86) | <.0001 |
| Hospital/other source | 1.0 (ref) | 1.06 (.96–1.18) | 1.27 (1.11–1.45) | 1.36 (1.16–1.59) | 1.50 (1.34–1.69) | <.0001 |
| Chronic disease index (relative to index=0) | ||||||
| Index=1 (1–2) | 1.0 (ref) | 1.05 (.97–1.13) | 1.18 (1.07–1.30) | 1.17 (1.03–1.32) | 1.40 (1.27–1.53) | <.0001 |
| Index=2 (3–8) | 1.0 (ref) | 1.14 (1.04–1.25) | 1.34 (1.19–1.51) | 1.63 (1.42–1.88) | 2.29 (2.06–2.54) | <.0001 |
Notes:
The model was adjusted by age, race, gender, education, household annual income, marital status and neighborhood deprivation index plus current smoker, severe obesity, recruitment source and chronic disease index. For chronic disease index, the model adjusted by all above variables except chronic disease index.
Differences in ACE scores by race and gender.
When the regression modelling was performed within strata defined by race and gender, the patterns between ACE score and emergency room visits in the past year were generally similar among Blacks and Whites, and among men and women. Odds ratios for emergency room visits among those with four or more vs. no ACEs were 1.40 (95% CI 1.28–1.54) for one to 10 times and 1.51 (95% CI 1.02–2.22) for more than 10 times in Blacks, 1.32 (95% CI 1.18–1.47) for one to 10 times and 3.90 (95% CI 1.75–8.67) for more than 10 times in Whites, 1.40 (95% CI 1.28–1.52) for one to 10 times and 1.87 (95% CI 1.23–2.83) for more than 10 times in women and 1.31 (95% CI (1.15–1.49) for one to 10 times and 1.68 (95% CI 0.95–2.97) for more 10 times in men. The patterns between ACE score and Chronic Disease Index (CDI) were similar among Blacks and Whites, and among men and women. Odds ratios for having three or more chronic diseases among those with four or more vs. no ACEs were 1.98 (95% CI 1.73–2.27) in Blacks, 2.72 (95% CI 2.30–3.20) in Whites, 2.43 (95% CI 2.14–2.77) in women, and 2.02 (95% CI 1.68–2.42) in men. Relative to private doctors’ office visits, the patterns between ACE score and choosing community health center/free clinic, choosing hospital/other source, choosing emergency room, or no source were similar among Blacks and Whites, and among men and women [Tables 5 and 6 are available upon request].
Discussion
Our analyses continue to expand the literature on the impact of ACEs on adult disease and health status, with our survey providing new information on ACE associations in underserved populations. In a low-income cohort recruited mainly through community health centers from across 12 southern states (Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia, and West Virginia), we found that adults in their 40s through 70s who reported greater exposure to ACEs had a higher chronic disease burden and greater health care utilization. Similar to data obtained through the Behavioral Risk Factor Surveillance System (BRFSS) studies in the United States general population, where 59% of respondents reported having at least one ACE,6–7 in the SCCS population we found that 54% of men and 60% of women also experienced at least one ACE. The consistent findings between these populations on ACE exposure percentages add validity to the data we report here.
We found rising numbers of doctors’ visits, greater use of emergency rooms, and higher chronic disease index scores with rising ACE scores. High numbers of doctors’ visits were nearly twice as common among those with ACE scores of four or more vs. zero. The percentages of participants reporting visiting emergency departments during the past year peaked at ≥57% of Black men and women with ACE scores of four or more. Similarly, the percentages reporting that emergency rooms were their usual source for medical care rose with ACE score, reaching 7% among Black men with ACE scores of four or more (Table 3). The increase in emergency department utilization rates may also lead to an increase in hospitalization rates, higher health care costs and delayed intervention or treatments.29 Additionally, the lower utilization of primary care services, given their high chronic disease burden, makes ACE victims potentially more vulnerable to worsened health status. These findings are consistent with prior work demonstrating the association of high ACE score with poorer overall health status.44–46
Early life trauma would be expected to increase Emergency Department visits in early life, and this pattern may continue into adulthood. What we find of great interest is that these experiences in childhood and adolescence seem to have long-term consequences in that they associate with health care utilization way beyond adolescence, since the youngest of the SCCS participants surveyed for ACEs was 43 years old. Our findings that the increase of the emergency department utilization increases with ACE exposure may also represent the need for training of emergency medicine physicians and staff to respond to trauma. Patients who experience greater childhood trauma may have difficulty sustaining long-term provider relationships with primary care physicians, and (furthermore) these physicians are unlikely to screen for childhood trauma (see http://www.jabfm.org/content/29/3/303.full.pdf). Patients exposed to childhood trauma (ACErs) may welcome screening for childhood trauma by their primary care physicians.
Given the incentives to avoid unnecessary emergency department use, understanding the role of ACE in utilization of health services is important to the quality metrics being promulgated for primary care practices. Low emergency department utilization has been targeted as a key feature in identifying high-quality primary care.47 However, primary care practices that provide services for underserved and Black populations may have poor performance on the standard quality metrics if they are not adjusted for the proportion of patients with high ACE exposure.
Thus, the importance of educating health care providers or medical school students on understanding ACEs, identifying signs of ACEs related trauma impacts, and incorporating trauma informed care in practice in various service systems has been increasingly recognized.48–51 This includes education on use of appropriate screening tools, communication with patients or their families regarding the patients’ ACE experiences, helping patients to recognize the sources of their health or behavioral issues, and familiarity with local resources so as to make referrals accordingly (e.g., social service, psychiatry faculty).52 Beyond the clinical setting, community based interventions can also be implemented to educate individuals on active ACE coping skills, using approaches such as meditation and relying on social support53 to improve self-care and self-regulation. Such efforts can help to achieve more sustainable treatment results and improve long-term health outcomes.
In addition to the improvement in provider education, a greater emphasis on programs that support trauma-informed care should be developed. Trauma-informed care helps to identify and alleviate the adverse health outcomes associated with childhood trauma. This study supports the need for a trauma-based care model. Presumably, as these care models gain popularity, more providers will address ACE in their patients.
Despite the robustness of the findings, our study does have some limitations. One is that the ACE questionnaire, which was developed elsewhere,3,4,54 relies on self-report and recall of the exposure to adverse events. Although recall of ACE events may be limited, those participants who were able to recollect adverse childhood experiences likely indicate a stronger internalization of the experience. Additionally, recall of adult health behaviors is subject to misclassification; however, validation studies based on the SCCS population showed good reliability for a number of variables, including behavioral variables of self-reported smoking status and clinical variables of self-reported weight and diabetes diagnosis.40 Another limitation is that the Philadelphia ACE was not available in 2012 at the initiation of our study, and that the 10 questions used in this analysis were limited to address ACEs caused by neighborhoods (including items in the expanded ACE questions of PHIL ACE survey).
In spite of these limitations, our findings indicate that there is a significant association between ACE and adult health care utilization. High levels of ACE exposure are associated with greater chronic disease burden, greater emergency department utilization, greater hospital utilization, and no source of regular outpatient care. Adverse childhood experiences (ACE) thus may have important implications for the U.S. health care system and profound effects on the quality of care reported for underserved populations.
Conclusions and implications for health care and public health programs.
Adverse childhood experiences (ACEs) were common in the current SCCS study population, predominantly composed of low-income residents in the southern U.S. Long-term detrimental health consequences of ACEs were shown among individuals who had been exposed to such experiences through numbers of doctors’ visits, frequency of emergency room use, and chronic disease index scores, which all rose with higher ACE scores. These exposures have been found to have an impact on adult illness and therefore important effects on health care utilization. Given the observed detrimental effects on overall adult health, which were also reported in previous studies, future studies are warranted to address how to mitigate the negative impacts of ACEs, accelerate recovery, and build up resilience among individuals with ACEs.
These findings call for better strategies to mitigate the adult health effects of ACEs and to help prevent health care over-utilization. In the literature, patient- and family-centered primary care programs have shown better health care outcomes in adult populations, and this literature suggests that integration of behavioral intervention and medical treatment should be considered for health care providers, patients, and their families.55 Providers must become more aware of ACEs and their adverse health impacts across life stages, must be alert for patients possibly having had ACEs, and must be familiar with trauma-informed care and referral when needed. Patients need programs that improve their disease self-management skills and that use adaptive approaches to cope with daily stress; patients also must accept assistance from family members where possible. Currently there is a lack of structured and practical approaches for health care providers to engage patients and their families in improving patients’ self-management skills. Future research in this field can help to improve the quality of health care and overall wellbeing of individuals who have had ACEs.
List of Abbreviations
- ACE
Adverse Childhood Experiences
- BMI
Basal Metabolic Index
- CDI
Chronic Disease Index
- CHCs
Community Health Centers
- CI
Confidence Interval
- COPD
Chronic Obstructive Pulmonary Disease
- OR
Odds Ratio
- SCCS
Southern Community Cohort Study
- VA
Veterans Affairs
Contributor Information
Margaret K. Hargreaves, Internal Medicine, Meharry Medical College, 1005 Dr. D.B. Todd Jr. Blvd, Nashville, TN 37208..
Charles P. Mouton, University of Texas Medical Branch..
William J. Blot, Vanderbilt University Medical Center..
References
- 1.Brown DW, Anda RF, Tiemeier H et al. Adverse Childhood Experiences and the risk of premature mortality. Am J Prev Med. 2009. November;37(5):389–96. 10.1016/j.amepre.2009.06.021 [DOI] [PubMed] [Google Scholar]
- 2.Dube SR, Felitti VJ, Dong M, et al. The impact of Adverse Childhood Experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med. 2003. September;37(3):268–77. 10.1016/S0091-7435(03)00123-3 [DOI] [PubMed] [Google Scholar]
- 3.Felitti VJ, Anda RF, Nordenberg D et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998. May;14(4):245–58. 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med. 1997. September;27(5):1101–19. 10.1017/S0033291797005588 [DOI] [PubMed] [Google Scholar]
- 5.Felitti VJ, Anda RF. The relationship of adverse childhood experiences to adult medical disease, psychiatric disorders, and sexual behavior: Implications for healthcare : Lanius RA, Vermetten E, Pain C, eds. The impact of early life trauma on health and disease: the hidden epidemic. Cambridge, United Kingdom: Cambridge University Press, 2010; 77–87. 10.1017/CBO9780511777042.010 [DOI] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Adverse Childhood Experiences reported by adults --- five states, 2009. MMWR Morb Mortal Wkly Rep. 2010. December 1;59(49):1609–13. [PubMed] [Google Scholar]
- 7.Gilbert LK, Breiding MJ, Merrick MT, et al. Childhood adversity and adult chronic disease: an update from ten states and the District of Columbia, 2010. Am J Prev Med. 2015. March;48(3):345–9. 10.1016/j.amepre.2014.09.006 [DOI] [PubMed] [Google Scholar]
- 8.Chartier MJ, Walker JR, Naimark B. Separate and cumulative effects of Adverse Childhood Experiences in predicting adult health and health care utilization. Child Abuse Negl. 2010. June;34(6):454–64. 10.1016/j.amepre.2014.09.006 [DOI] [PubMed] [Google Scholar]
- 9.Dube SR, Miller JW, Brown DW, et al. Adverse Childhood Experiences and the association with ever using alcohol and initiating alcohol use during adolescence. J Adolesc Health. 2006. April;38(4):444.e1–10. 10.1016/j.jadohealth.2005.06.006 [DOI] [PubMed] [Google Scholar]
- 10.Felitti VJ. [Origins of addictive behavior: evidence from a study of stressful chilhood experiences]. Prax Kinderpsychol Kinderpsychiatr. 2003. October;52(8):547–59. [PubMed] [Google Scholar]
- 11.Strine TW, Dube SR, Edwards VJ et al. Associations between Adverse Childhood Experiences, psychological distress, and adult alcohol problems. Am J Health Behav. 2012. May;36(3):408–23. 10.5993/AJHB.36.3.11 [DOI] [PubMed] [Google Scholar]
- 12.LaNoue M, Graeber D, de Hernandez BU, et al. Direct and indirect effects of childhood adversity on adult depression. Community Ment Health J. 2012. April;48(2):187–92. 10.1007/s10597-010-9369-2 [DOI] [PubMed] [Google Scholar]
- 13.Dong M, Giles WH, Felitti VJ, et al. Insights into causal pathways for ischemic heart disease: Adverse Childhood Experiences study. Circulation. 2004. September;110(13):1761–6. 10.1161/01.CIR.0000143074.54995.7F [DOI] [PubMed] [Google Scholar]
- 14.Poulton R, Caspi A, Milne BJ, et al. Association between children’s experience of socioeconomic disadvantage and adult health: a life-course study. Lancet. 2002. November;360 (9346):1640–5. 10.1016/S0140-6736(02)11602-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomas C, Hypponen E, Power C. Obesity and type 2 diabetes risk in midadult life: the role of childhood adversity. Pediatrics. 2008. May;121(5):e1240–9. 10.1542/peds.2007-2403 [DOI] [PubMed] [Google Scholar]
- 16.Brown DW, Anda RF, Felitti VJ et al. Adverse Childhood Experiences are associated with the risk of lung cancer: a prospective cohort study. BMC Public Health. 2010. January 19;10:20 10.1186/1471-2458-10-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brown MJ, Cohen SA. Association between abusive and non-abusive Adverse Childhood Experiences and diagnosis of cancer in Wisconsin, USA. J Community Med Health Educ. 2014. S2.008. [Google Scholar]
- 18.Brown MJ, Thacker LR, Cohen SA. Association between Adverse Childhood Experiences and diagnosis of cancer. PLoS One. 2013. June 11;8(6):e65524 10.1371/journal.pone.0065524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van der Meer LB, van Duijn E, Wolterbeek R R., et al. Adverse Childhood Experiences of persons at risk for Huntington’s disease or BRCA1/2 hereditary breast/ovarian cancer. Clin Genet. 2012. January;81(1):18–23. 10.1111/j.1399-0004.2011.01778.x [DOI] [PubMed] [Google Scholar]
- 20.Austin AE, Herrick HWB. The effect of Adverse Childhood Experiences on adult health: 2012 North Carolina Behavioral Risk Factor Surveillance System Survey. Raleigh, NC: State Center for Health Statistics Studies, 2014. Available at: https://schs.dph.ncdhhs.gov/schs/pdf/SCHS_Study_167_FIN_20140505.pdf. [Google Scholar]
- 21.Bonomi AE, Cannon EA, Anderson ML, et al. Association between self-reported health and physical and/or sexual abuse experienced before age 18. Child Abuse Negl. 2008 Jul;32(7):693–701. 10.1016/j.chiabu.2007.10.004 [DOI] [PubMed] [Google Scholar]
- 22.Campbell JA, Walker RL, Egede LE. Associations between Adverse Childhood Experiences, high-risk behaviors, and morbidity in adulthood. Am J Prev Med. 2016. March;50(3):344–52. 10.1016/j.amepre.2015.07.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cronholm PF, Forke CM, Wade R, et al. Adverse Childhood Experiences: expanding the concept of adversity. Am J Prev Med. 2015. September;49(3):354–61. 10.1016/j.amepre.2015.02.001 [DOI] [PubMed] [Google Scholar]
- 24.Finkelhor D, Shattuck A, Turner H et al. A revised inventory of Adverse Childhood Experiences. Child Abuse Negl. 2015. October;48:13–21. 10.1016/j.chiabu.2015.07.011 [DOI] [PubMed] [Google Scholar]
- 25.Kalmakis KA, Chandler GE. Health consequences of adverse childhood experiences: a systematic review. J Am Assoc Nurse Pract. 2015. August;27(8):457–65. 10.1002/2327-6924.12215 [DOI] [PubMed] [Google Scholar]
- 26.Mouton CP, Hargreaves MK, Liu J, et al. Adult cancer risk behaviors associated with Adverse Childhood Experiences in a low income population in the southeastern United States. J Health Care Poor Underserved. 2016. February;27(1):68–83. 10.1353/hpu.2016.0027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bonomi AE, Anderson ML, Rivara FP, et al. Health care utilization and costs associated with childhood abuse. J Gen Intern Med. 2008. March;23(3):294–9. 10.1007/s11606-008-0516-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hansagi H, Olsson M, Sjoberg S, et al. Frequent use of the hospital emergency department is indicative of high use of other health care services. Ann Emerg Med. 2001. June;37(6):561–7. 10.1067/mem.2001.111762 [DOI] [PubMed] [Google Scholar]
- 29.Walker EA, Unutzer J, Rutter C, et al. Costs of health care use by women HMO members with a history of childhood abuse and neglect. Arch Gen Psychiatry. 1999. July;56(7):609–13. 10.1001/archpsyc.56.7.609 [DOI] [PubMed] [Google Scholar]
- 30.Malat J, Oh HJ, Hamilton MA. Poverty experience, race, and child health. Public Health Rep. 2005. Jul-Aug;120(4):442–7. 10.1177/003335490512000411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scott Collins K, Schoen C, Joseph S, et al. Health concerns across a woman’s lifespan: the Commonwealth Fund 1998 survey of women’s health. New York, NY: The Commonwealth Fund, 1999. [Google Scholar]
- 32.Tomer JF. Adverse childhood experiences, poverty, and inequality: toward an understanding of the connections and the cures. World Economic Review. 20143:20–36. [Google Scholar]
- 33.Wade R Jr, Shea JA, Rubin D, et al. Adverse childhood experiences of low-income urban youth. Pediatrics. 2014. July;134(1):e13–20. 10.1542/peds.2013-2475 [DOI] [PubMed] [Google Scholar]
- 34.Font SA, Maguire-Jack K. Pathways from childhood abuse and other adversities to adult health risks: The role of adult socioeconomic conditions. Child Abuse Negl. 2016. January;51:390–9. 10.1016/j.chiabu.2015.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maguire-Jack K, Showalter K. The protective effect of neighborhood social cohesion in child abuse and neglect. Child Abuse Negl. 2016. February;52:29–37. 10.1016/j.chiabu.2015.12.011 [DOI] [PubMed] [Google Scholar]
- 36.National Research Council Committee on Future Directions for Behavioral and Social Sciences Research at the National Institutes of Health, Singer BH, Ryff CD, eds. New horizons in health: an integrative approach. Washington (DC): National Academies Press (US) National Academy of Sciences, 2001. [PubMed] [Google Scholar]
- 37.Wade R Jr, Cronholm PF, Fein JA, et al. Household and community-level Adverse Childhood Experiences and adult health outcomes in a diverse urban population. Child Abuse Negl. 2016. February;52:135–45. 10.1016/j.chiabu.2015.11.021 [DOI] [PubMed] [Google Scholar]
- 38.Williams DR. Race, socioeconomic status, and health. The added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–88. 10.1111/j.1749-6632.1999.tb08114.x [DOI] [PubMed] [Google Scholar]
- 39.Williams DR, Sternthal M. Understanding racial-ethnic disparities in health: sociological contributions. J Health Soc Behav. 2010. 51 Suppl:S15–27. 10.1177/0022146510383838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Signorello LB, Hargreaves MK, Blot WJ. The Southern Community Cohort Study: investigating health disparities. J Health Care Poor Underserved. 2010. February;21(1 Suppl):26–37. 10.1353/hpu.0.0245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Signorello LB, Hargreaves MK, Steinwandel MD, et al. Southern community cohort study: establishing a cohort to investigate health disparities. J Natl Med Assoc. 2005. July;97(7):972–9. [PMC free article] [PubMed] [Google Scholar]
- 42.Dube SR, Williamson DF, Thompson T, et al. Assessing the reliability of retrospective reports of adverse childhood experiences among adult HMO members attending a primary care clinic. Child Abuse Negl. 2004. July;28(7):729–37. 10.1016/j.chiabu.2003.08.009 [DOI] [PubMed] [Google Scholar]
- 43.Messer LC, Laraia BA, Kaufman JS, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006. November;83(6):1041–62. 10.1007/s11524-006-9094-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iniguez KC, Stankowski RV. Adverse Childhood Experiences and health in adulthood in a rural population-based sample. Clin Med Res. 2016. December;14(3–4):126–37. 10.3121/cmr.2016.1306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Salinas-Miranda AA, Salemi JL, King LM, et al. Adverse childhood experiences and health-related quality of life in adulthood: revelations from a community needs assessment. Health Qual Life Outcomes. 2015. August 11;13:123 10.1186/s12955-015-0323-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Springer KW, Sheridan J, Kuo D, et al. Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women. Child Abuse Negl. 2007. May;31(5):517–30. 10.1016/j.chiabu.2007.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shi L The impact of primary care: a focused review. Scientifica (Cairo). 2012;2012:432892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Flynn AB, Fothergill KE, Wilcox HC, et al. Primary care interventions to prevent or treat traumatic stress in childhood: a systematic review. Acad Pediatr. 2015. Sep-Oct 15(5):480–92. 10.1016/j.acap.2015.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leitch L Action steps using ACEs and trauma-informed care: a resilience model. Health Justice. 2017. December;5(1):5 10.1186/s40352-017-0050-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Oral R, Ramirez M, Coohey C, et al. Adverse childhood experiences and trauma informed care: the future of health care. Pediatr Res. 2016. January;79(1–2):227–33. 10.1038/pr.2015.197 [DOI] [PubMed] [Google Scholar]
- 51.Strait J, Bolman T. Consideration of personal Adverse Childhood Experiences during implementation of trauma-informed care curriculum in graduate health programs. Perm J. 2017;21 pii:16–061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Forstadt L, Cooper S, Andrews SM. Changing medicine and building community: Maine’s Adverse Childhood Experiences momentum. Perm J. 2015. Spring;19(2):92–5. 10.7812/TPP/14-169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chandler GE, Roberts SJ, Chiodo L. Resilience intervention for young adults with Adverse Childhood Experiences. J Am Psychiatr Nurses Assoc. 2015. Nov-Dec;21(6):406–16. 10.1177/1078390315620609 [DOI] [PubMed] [Google Scholar]
- 54.Edwards VJ, Anda RF, Nordenberg DF, et al. Bias assessment for child abuse survey: factors affecting probability of response to a survey about childhood abuse. Child Abuse Negl. 2001. February;25(2):307–12. 10.1016/S0145-2134(00)00238-6 [DOI] [PubMed] [Google Scholar]
- 55.Park M, Giap T, Lee M, et al. Patient- and family-centered care interventions for improving the quality of health care: A review of systematic reviews. Int J Nurs Stud. 2018. July 26;87:69–83. 10.1016/j.ijnurstu.2018.07.006 [DOI] [PubMed] [Google Scholar]