Abstract
Background
Moderate fitness levels and habitual exercise have a protective effect for cardiovascular disease, stroke, type 2 diabetes, and all-cause mortality. The Apple Watch displays exercise completed at an intensity of a brisk walk or above using a green “exercise” ring. However, it is unknown if the exercise ring accurately represents an exercise intensity comparable to that defined as moderate-intensity. In order for health professionals to prescribe exercise intensity with confidence, consumer wearable devices need to be accurate and precise if they are to be used as part of a personalized medicine approach to disease management.
Objective
The aim of this study was to examine the validity and reliability of the Apple Watch for measuring moderate-intensity exercise, as defined as 40-59% oxygen consumption reserve (VO2R).
Methods
Twenty recreationally active participants completed resting oxygen consumption (VO2rest) and maximal oxygen consumption (VO2 max) tests prior to a series of 5-minute bouts of treadmill walking at increasing speed while wearing an Apple Watch on both wrists, and with oxygen consumption measured continuously. Five-minute exercise bouts were added until the Apple Watch advanced the green “exercise” ring by 5 minutes (defined as the treadmill inflection speed). Validity was examined using a one-sample t-test, with interdevice and intradevice reliability reported as the standardized typical error and intraclass correlation.
Results
The mean %VO2R at the treadmill inflection speed was 30% (SD 7) for both Apple Watches. There was a large underestimation of moderate-intensity exercise (left hand: mean difference = -10% [95% CI -14 to -7], d=-1.4; right hand: mean difference = -10% [95% CI -13 to -7], d=-1.5) when compared to the criterion of 40% VO2R. Standardized typical errors for %VO2R at the treadmill inflection speed were small to moderate, with intraclass correlations higher within trials compared to between trials.
Conclusions
The Apple Watch threshold for moderate-intensity exercise was lower than the criterion, which would lead to an overestimation of moderate-intensity exercise minutes completed throughout the day.
Keywords: smartwatch; wearables; technology; physical activity; cardiovascular health, Apple Watch
Introduction
Background
Physical activity is well documented as a beneficial intervention for the prevention and treatment of chronic disease, while physical inactivity is an independent risk factor for the development of lifestyle-related chronic diseases, such as cardiovascular disease [1,2]. To be considered “physically active” it is recommended that adults accumulate >150 minutes of moderate or 75 minutes of vigorous-intensity physical activity (MVPA) over the course of a week to provide them with substantial health benefits [3]. Given that the average adult expends approximately four metabolic equivalents walking at a moderate pace [4], they would therefore need to walk at this pace for 125 minutes/week, or 30 minutes on most days of the week, to meet the minimum recommendations. Although these physical activity guidelines are strongly recommended by governments across the world [5-7], many people do not achieve them [8-11]. However, physical activity interventions that have incorporated technology-based support have shown promise in developing compliance to physical activity guidelines [12,13], possibly through reinforcement to develop habit-forming behaviors [14].
Although valid and reliable tools for measuring physical activity are available for researchers, such as the ActiGraph [15], it is the quantified-self movement [16] that has led to the increasing popularity of consumer wearable technology, with estimates indicating sales of over 200 million by 2021, including the Apple Watch [17]. Having contemporary instruments to integrate into exercise prescription and physical activity promotion that fit into people’s lifestyles is imperative. Although evidence on the validity and reliability of modern wearable devices with integrated screens to measure exercise and physical activity is increasing, no study has examined the accuracy of the Apple Watch for measuring MVPA.
Apple is one of the world’s most valuable companies (by market value) [18] and has changed a number of industries through disruptive devices (eg, iPod, iPhone). The Apple Watch, which was released in 2015, has reportedly become the highest selling wearable/smartwatch to date, with more than 12 million units reported to have been sold [19,20]. The widespread use of the Apple Watch would therefore allow physical activity interventions to reach a large proportion of the population. Additionally, the Apple Watch provides potential for data to be collected from, and returned to, the individual, to provide immediate individualized feedback via the wearable’s screen to promote behavior change and be shared with others, such as a clinician. However, Apple provides little detail on how the Apple Watch measures “exercise.” It appears that the built-in accelerometer is mostly used to measure physical activity throughout the day [21,22], although heart rate measurement is used periodically when walking [22]. Daily physical activity data is displayed within the “Activity” app, with a visual representation of the accumulated duration of “exercise” displayed as a green ring on the screen of the watch. Given that Apple refers to this as the “exercise” ring and that 30 minutes is the daily goal [23], it is reasonable to suggest that Apple views this as representative of the daily goal of 30 minutes of MVPA for adults, as recommended by numerous guidelines [5-7]. Although Apple states that, “every full minute of movement that equals or exceeds the intensity of a brisk walk counts toward your daily exercise goal” [23], it is not clear how this measure of MVPA compares to the criterion measure of moderate-intensity exercise, oxygen consumption reserve (VO2R: [VO2max - VO2rest] x exercise intensity + VO2rest).
Objective of This Study
Given the scale of smartwatch use around the world and the increasing attention on personalized medicine, the validity of the Apple Watch for measuring moderate-intensity exercise is important to examine. Establishing the validity of the Apple Watch would ensure that individuals are able to measure their own MVPA accurately and that health professionals have confidence in the data that their clients are sharing with them. Establishing the intradevice and interdevice reliability of the Apple Watch is also important so that daily measures can be compared, and that user preference for wearing the Watch on the left or right wrist does not introduce bias. Therefore, the aim of this study was to examine the validity and reliability of the Apple Watch for quantifying moderate-intensity exercise compared with directly measured VO2R.
Methods
Study Design and Participants
The study used a repeated measures design with each participant completing two main trials. Prior to the main trials, maximal oxygen consumption (VO2max) and resting oxygen consumption (VO2rest) were measured in all participants. The study was approved by the Department of Sport, Health and Exercise Science Ethics Committee (approval number 1516076) at the University of Hull. Given the paucity of data on the Apple Watch at the time of study commencement, the sample size was estimated based on a previous study [24].
Recruitment
Participants were recruited from the University of Hull and local community via written promotional material or personal communication. Inclusion criteria stated that participants were aged between 18 and 50 years, and exclusion criteria were: (1) men and women classified as moderate or high-risk according to the American College of Sports Medicine (ACSM) risk classification criteria, (2) those unable to walk on a motorized treadmill, (3) current smokers, (4) BMI >30, and (5) those currently taking medication that alters the heart rate in response to exercise (eg, beta blockers). Inclusion and exclusion criteria were established with the aim of recruiting low-risk individuals, based on the ACSM risk classification criteria used at the commencement of the study.
Data Collection
Anthropometric
Participants were asked if they had voided before attending the session; if not, they were instructed to do so. Participants were then instructed to remove all clothing and nude body mass was measured to the nearest 0.1 kg using digital scales (WB-100MA Mark 3, Tanita Corporation, Tokyo, Japan). The mean of two measurements was used for further analysis. Stretch stature was measured using a wall-mounted stadiometer (Holtain Ltd, Dyfed, Wales, UK) and according to the methods of the International Society for the Advancement of Kinanthropometry [25].
Familiarization
Following medical screening and admission to the study, participants were familiarized with the tasks required of them during the main trials. This familiarization session consisted of the participant practicing “hopping on” and “hopping off” the treadmill, as well as walking at a number of dedicated speeds. This familiarization procedure was repeated at three of the speeds used in the main trials (ie, 3, 4.5, 6 km/hour).
Resting Oxygen Consumption
VO2rest was measured 30 minutes prior to, and in the same session, as VO2 max in a temperature-controlled laboratory. Participants lay supine on a bed with their head on a pillow for approximately 22 minutes. Oxygen consumption was measured continuously from expired air using a breath-by-breath online gas analysis system (Cortex Metalyzer 3B, GmbH, Germany). The analyzer was calibrated prior to each test using room air and known gas concentrations of oxygen and carbon dioxide. Volume was calibrated using a 3-liter syringe.
During the 22 minutes of measurement, the laboratory lights were turned off and all other laboratory activity was stopped. Prior to commencement of the measurement period, participants were instructed to relax as much as possible but to avoid going to sleep; they were not permitted to close their eyes. For analysis of the data, we discarded the first 10 minutes of data to allow for habituation and the last 2 minutes of data to allow for expectation effects. The mean of the remaining 10 minutes of data was taken as the VO2rest. Although we are not aware of any standardized method for measuring VO2rest for the purpose of calculating VO2R, we developed our method based on that reported by Miller et al [26].
Maximal Oxygen Consumption
Maximal oxygen consumption was determined on a motorized treadmill (h/p/cosmos, Pulsar, Nussdorf-Traunstein, Germany) using an incremental protocol that commenced at 3 km/hour and a 1% gradient and increased 0.5 km/hour in speed every 30 seconds until volitional fatigue. Oxygen consumption was measured continuously from expired air using the same breath-by-breath system as described above for VO2rest.
Exercise Protocol
For the 24 hours prior to each trial, participants were instructed to avoid exercise and maintain their normal diet, and for three hours prior to each trial avoid food and caffeinated drinks. On two separate occasions (mean 6 days apart, SD 3) participants completed a series of 5-minute bouts of walking on a treadmill at a gradient of 1%. Each bout was followed by 5-minutes of seated rest. On both occasions, the first 5-minute walking bout was conducted at 3 km/hour, with the treadmill speed increased for each successive 5-minute bout by 0.5 km/hour (ie, 3.5, 4). Exercise bouts were continued until at least 6 km/hour was completed, and until the Apple Watch indicated that all 5-minutes of that bout was at a sufficient intensity to accumulate 5-minutes of the green “exercise” ring, as displayed within the Activity app. The treadmill speed at which this occurred was defined as the “treadmill inflection speed.” During each 5-minute period of exercise, oxygen consumption and heart rate were recorded by an online gas analysis system (as described previously), a Polar chest strap (Polar T31, Polar Electro, OY, Finland), and an Apple Watch (described below) worn on each wrist. During each 5-minute period of exercise, participants were instructed to maintain their normal gait and were not permitted to hold the treadmill handrails. Immediately at the cessation of each 5-minute exercise period, participants were instructed to grasp the treadmill handrails and straddle the treadmill belt. Once the treadmill belt was stationary, a chair was placed on the treadmill and the participant was instructed to sit. During the recovery period participants were required to sit motionless with each hand resting on the treadmill handrail. This was done to ensure that no activity during the recovery period contributed to the green “exercise” ring. Five minutes of seated rest was provided to enable each Apple Watch to update the green “exercise” ring. In pilot testing it was observed that the Apple Watch completed its update within a maximum of 5 minutes of rest following exercise. The mean oxygen consumption of the last three minutes at the treadmill inflection speed for each watch was used for later analysis.
Two first-generation (Series 0) Apple Watches running watchOS 2.0.1 were used to estimate moderate-intensity exercise. Each Apple Watch was paired to an iPhone 6 running iOS 9.1. Following each 5-minute rest period the number of “exercise” minutes, as measured by each of the Apple Watches, was manually recorded from the Activity app.
Moderate-intensity exercise is defined by the ACSM as that which elicits an oxygen consumption of between 40% and 59% of VO2R. By rearranging the equation provided by the ACSM (see below) [3] and substituting target volume of oxygen (VO2) for the measured oxygen consumption at the treadmill inflection speed, the percentage of VO2R at the treadmill inflection speed (exercise intensity in the equation) can be calculated: Target VO2= (VO2max - VO2rest) x exercise intensity + VO2rest.
Statistical Analyses
Data were checked for normality using the Shapiro-Wilk test and graphical methods, and were found to be plausible. The VO2R during Trial 2 was used to assess the validity of the Apple Watch for measuring moderate-intensity exercise, with VO2R during both Trial 1 and 2 used to assess the interdevice and intradevice reliability. A one-sample t-test was used to test if the mean %VO2R at the treadmill inflection speed for each Apple Watch was different from 40%, which is the lower limit of moderate-intensity exercise. A custom-designed Excel spreadsheet was used to examine differences between left and right Apple Watches for treadmill inflection speed and %VO2R [27]. Pearson product-moment correlation was used to assess the association between VO2max and the %VO2R at the treadmill inflection speed. Based on the linear association between VO2max and %VO2R, linear regression was used to estimate the VO2 max and treadmill speed required for the Apple Watch to accurately measure moderate-intensity exercise. Interdevice and intradevice reliability is reported as the standardized typical error and intraclass correlation. Standardized typical error was doubled prior to assessing its magnitude [28]. Standardized effect size is reported as Cohen’s d using the between-subject pooled SD as the denominator. The scale of magnitudes used to evaluate Cohen’s d was: 0-0.19 trivial; 0.2-0.59 small; 0.6-1.19 moderate; 1.2-1.99 large; >2.0 very large [28]. Uncertainty in the population estimates are reported as 95% CIs.
Results
Twenty (10 male, 10 female) recreationally active participants (mean age 32 years [SD 10]; body mass 71.4 kg [SD 14.2]; stature 174.5 cm [SD 7.2]) provided written informed consent to undertake a maximal exercise test and the research exercise protocol. Participants had their cardiovascular risk assessed using the ACSM risk classification guidelines [3], with all participants classified as low risk.
The mean VO2max and VO2rest, as measured using the online gas analysis system, were 45 mL/kg/minute (SD 10) and 3.4 mL/kg/minute (SD 0.6), respectively. The mean treadmill “inflection” speeds that were required to advance the Apple Watch green exercise ring by 5 minutes were 5.6 km/hour (SD 0.5) and 5.6 km/hour (SD 0.5) for the left and right Apple Watches, respectively (mean difference: 0 km/hour [95% CI -0.1 to 0.2], d=0.05 [trivial]). The mean %VO2R at the treadmill inflection speed for the left and right Apple Watches were 30% (SD 7) and 30% (SD 7), respectively (mean difference: 0% [95% CI -1 to 2], d=0.02 [trivial]). When compared to the criterion threshold of 40% VO2R, this represents a large underestimation in the ability of the Apple Watch to measure moderate-intensity exercise (left: mean difference = -10 [95% CI -14 to -7], d=-1.4 [large]; right: mean difference = -10 [95% CI -13 to -7], d=-1.5 [large]). The %VO2R at the treadmill inflection speed for each participant and each watch is displayed, together with the mean and 95% CI for both watches, in Figure 1.
Figure 1.
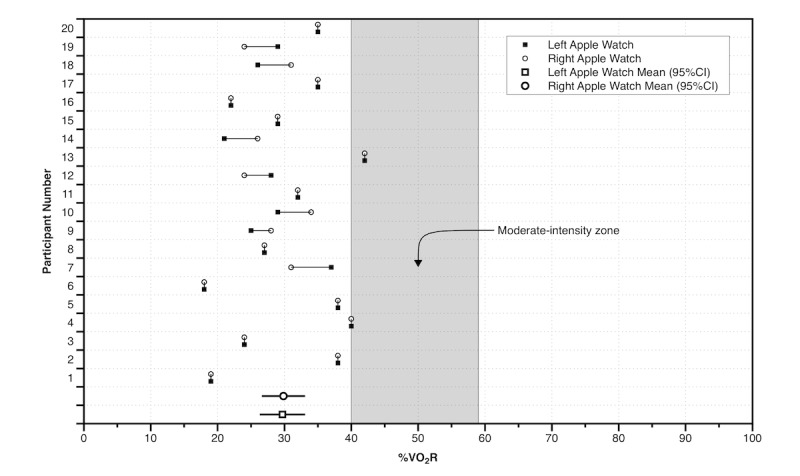
The oxygen consumption reserve (%VO2R) at the treadmill inflection speed for each participant and each watch compared with the moderate-intensity zone.
There was a very large negative correlation between %VO2R at the treadmill inflection speed and VO2max for the left Apple Watch (Figure 2), and a large negative correlation between %VO2R at the treadmill inflection speed and VO2max for the right Apple Watch (Figure 3). Participants with a higher VO2max were exercising at a lower percentage of their VO2R at the treadmill inflection speed (Figures 2 and 3). For the Apple Watch to accurately measure moderate-intensity exercise (40-59% VO2R), based on the regression equation for the left Watch, the user would need a VO2max between 16 (95% CI -3 to 36) and 35 (95% CI 19 to 50) mL/kg/minute. Based on within-participant linear regression analyses using the VO2R at each speed, we estimate that to achieve 40% of VO2R, participants would need to walk at a mean treadmill speed of 7.7 km/hour (95% CI 6.7 to 8.6) at 1% incline; which is 2.1 km/hour faster than that predicted by the Apple Watch. Only one participant had a comparable treadmill speed estimate for 40% VO2R between the Apple Watch and the online gas analysis system. Interdevice and intradevice reliability statistics for both treadmill speed and VO2R are displayed in Table 1.
Figure 2.
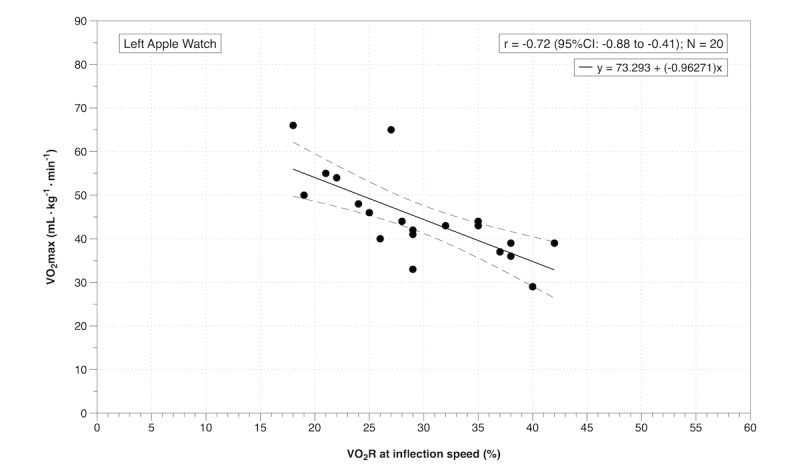
Pearson correlation between oxygen consumption reserve (%VO2R) at the treadmill inflection speed and maximal oxygen consumption (VO2max) for the left Apple Watch.
Figure 3.
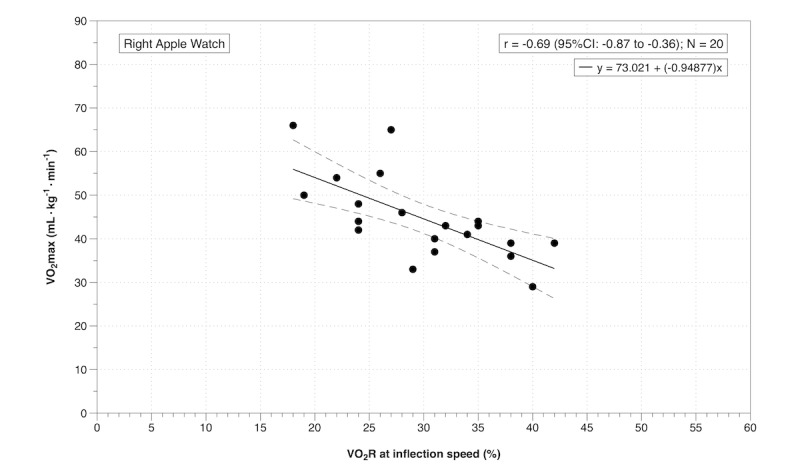
Pearson correlation between oxygen consumption reserve (%VO2R) at the treadmill inflection speed and maximal oxygen consumption (VO2max) for the right Apple Watch.
Table 1.
Intradevice and interdevice reliability for both treadmill speed and oxygen consumption reserve (VO2R) for left and right Apple Watches.
| Parameter | Trial 1 Left vs Trial 1 Right |
Trial 2 Left vs Trial 2 Right |
Trial 1 Left vs Trial 2 Left |
Trial 1 Right vs Trial 2 Right |
|
| Speed |
|
|
|
|
|
|
|
Standardized typical error (95% CI) | 0.41 (0.31 to 0.60) | 0.54 (0.41 to 0.79) | 0.53 (0.40 to 0.79) | 0.64 (0.49 to 0.92) |
|
|
Qualitative interpretation | Moderate | Moderate | Moderate | Large |
|
|
Intraclass correlation (95% CI) | 0.87 (0.70 to 0.95) | 0.79 (0.55 to 0.91) | 0.80 (0.55 to 0.92) | 0.73 (0.45 to 0.88) |
| VO2R |
|
|
|
|
|
|
|
Standardized typical error (95% CI) | 0.2 (0.15 to 0.29) | 0.33 (0.25 to 0.50) | 0.48 (0.36 to 0.71) | 0.37 (0.28 to 0.54) |
|
|
Qualitative interpretation | Small | Moderate | Moderate | Moderate |
|
|
Intraclass correlation (95% CI) | 0.97 (0.92 to 0.99) | 0.91 (0.78 to 0.96) | 0.83 (0.61 to 0.93) | 0.89 (0.75 to 0.95) |
Discussion
Principal Findings
This is the first study to investigate the validity and reliability of the Apple Watch for measuring moderate-intensity exercise (the green “exercise” ring) compared to the criterion measure of VO2R. The Apple Watch largely underestimated the walking speed required to elicit the lower bound of moderate-intensity exercise (40% VO2R), which is an important part of individualized [3] and population-based [29] exercise prescription guidelines. The standardized typical error, a measure of the “typical” test-retest variability presented in units of SD [28], was small to moderate with no mean difference between the left and right watches for the mean treadmill inflection speed or %VO2R for the lower limit of moderate-intensity exercise [3].
For less fit individuals (<35 mL/kg/minute), using the Apple Watch to monitor moderate-intensity exercise is more likely to have the expected and desired improvements to fitness or clinical outcomes than for fitter individuals. However, for those that are fitter (>35 mL/kg/minute) it appears from our data that individuals would not meet the expectations of the lower end (40% VO2R) of the moderate-intensity range [3], with the Apple Watch underestimating the threshold for moderate-intensity exercise, and therefore overestimating the number of minutes of moderate-intensity exercise an individual had completed. Thompson et al [30] recently came to a similar conclusion, reporting that commercially-available wearable devices for self-monitoring of physical activity overestimate MVPA by a factor of 5-to-7-fold because they capture all physical activity, including normal moderate-to-vigorous lifestyle activities. However, other recent studies have reported that Fitbit devices (Fitbit One and Fitbit Flex) underestimate MVPA [31,32], although in these studies the wearable device was compared against another wearable device (ActiGraph), not direct laboratory-measured moderate-intensity exercise as we have done in our study. In our study only two participants achieved a %VO2R within the moderate-intensity exercise zone (Figure 1). Apart from the impact this may have on the expected physiological adaptations and fitness, it also has potential implications for morbidity and mortality risk, as moderate fitness levels and habitual exercise have a protective effect for cardiovascular disease, stroke, type 2 diabetes, and all-cause mortality [33].
Measuring load in an individual is complicated with a variety of methods available to monitor internal and external load [34]. The Apple Watch does not substantially overestimate or underestimate heart rate [24] and has moderate interdevice variability of maximal heart rate when worn on each wrist [35]. Therefore, using a continuous combination of internal (heart rate) and external (accelerometer) training load measures [34,36] rather than using the accelerometer plus periodic use of heart rate as is currently used, may improve the accuracy of the green exercise ring and provide a greater personalization of the data available to an individual. Given the wide range of VO2R responses observed at the treadmill speed that the Apple Watch determined to be “exercise” (<20% to >40%), and the variability between left and right Watches (Figure 1), it is clear that the Apple Watch needs to provide a more appropriate measure of the individualized response to exercise. This would not only enable more tailored feedback and exercise prescription, it would likely improve the physiological adaptations to any training and the associated cardiometabolic and musculoskeletal improvements for chronic disease prevention and treatment [33]. Better compliance to guidelines [13] and improved disease management and confidence [37] have been reported in healthy and chronic disease populations when technology-based support is incorporated. However, consumer and health professionals need to have confidence that any wearable device can both consistently and accurately measure the exercise intensity for individuals of all fitness levels.
The reliability data (Table 1) suggest that the reliability of VO2R at the point where the Apple Watch determines that “exercise” has started (the treadmill inflection speed) is better within trials (interdevice) than between trials (intradevice). This finding would suggest that physical activity measurements are more reliable within the same training session or activity compared to between different training sessions or activities. The implication is that health professionals can be confident that the ability of the Apple Watch to measure physical activity (as used in the current study) is not adversely affected by the wrist (left or right) on which an individual wore the watch within a given training session or activity.
Strengths and Limitations
The main strength of our study is that this is the first investigation to examine the validity of the Apple Watch for measuring aspects of exercise related to the achievement of daily MVPA. The main limitation of this study is that we did not have direct access to the algorithms used by the Apple Watch for determining the exercise intensity at which the green “exercise” ring advances. Unfortunately, Apple does not publish these algorithms, probably due to commercial reasons. However, this is a limitation with most commercially-available wearable devices and is not restricted to the Apple Watch. A second limitation is that our data were derived from first generation Apple Watches. Although the method Apple uses to determine “exercise” using the Activity app has changed slightly with the periodic measurement of heart rate during walking [21,22], it is unclear how this would affect the validity of the Apple Watch for measuring MVPA. Further studies are required using the latest generation of Apple Watch for this to be determined. The exercise protocols used in our study were also constrained to linear walking on a treadmill. Movement patterns used by people outside of the laboratory while wearing an Apple Watch may result in different physiological responses and different determinations of “exercise” by the Apple Watch. Fourth, although our primary measure was VO2R, there are a number of factors that can influence the oxygen cost of exercise, such as economy [38,39]. For example, economy has been reported to be affected by age, such that older adults have less economy when walking compared to younger people [40]. The mean age of our participants was 32 years (SD 10), which places our participants midway between the young and old adults participating in the study of Martin et al [40]. Although factors such as economy and age should be taken into account when interpreting our results, the use of %VO2R as a relative measure of oxygen cost means that between-individual comparisons should still be meaningful.
Conclusions
The Series 0 Apple Watch underestimates the threshold for moderate-intensity exercise compared to the criterion measure of VO2R, which would result in an overestimation of the amount of MVPA undertaken throughout the day. This effect is more pronounced in fitter individuals.
Acknowledgments
GA, JB, and ACB designed the study. GA and JB collected the data. GA, JB, and ACB analyzed the data. GA, JB, and ACB prepared and revised the manuscript.
Abbreviations
- ACSM
American College of Sports Medicine
- MVPA
moderate-vigorous physical activity
- VO2
volume of oxygen
- VO2max
maximal oxygen consumption
- VO2R
oxygen consumption reserve
- VO2rest
resting oxygen consumption
Footnotes
Conflicts of Interest: None declared.
References
- 1.Haskell WL, Lee I, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007 Aug;39(8):1423–34. doi: 10.1249/mss.0b013e3180616b27.00005768-200708000-00027 [DOI] [PubMed] [Google Scholar]
- 2.Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, Khunti K, Yates T, Biddle SJH. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012 Nov;55(11):2895–905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 3.Pescatello LS. American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. 9th edition. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2014. [Google Scholar]
- 4.Brooks AG, Gunn SM, Withers RT, Gore CJ, Plummer JL. Predicting walking METs and energy expenditure from speed or accelerometry. Med Sci Sports Exerc. 2005 Jul;37(7):1216–23. doi: 10.1249/01.mss.0000170074.19649.0e.00005768-200507000-00020 [DOI] [PubMed] [Google Scholar]
- 5.Australian Government Department of Health Evidence Summary. Australia's physical activity and sedentary behaviour guidelines: guidelines evidence summary http://www.health.gov.au/internet/main/publishing.nsf/Content/health-pubhlth-strateg-phys-act-guidelines/$File/Guideline .
- 6.Bull F, Biddle SJH, Buchner D, Ferguson RA, Foster C, Fox KR, Haskell WL, Mutrie N, Murphy M, Reilly J, Riddoch C, Skelton D, Stratton G, Tremblay M, Watts C. Physical activity guidelines in the UK: Review and recommendations. 2010. May, https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/213743/dh_128255.pdf .
- 7.U.S. Department of Health and Human Services. 2018. Physical activity guidelines for Americans https://health.gov/paguidelines/pdf/paguide.pdf . [DOI] [PubMed]
- 8.Marcus BH, Dubbert PM, Forsyth LH, McKenzie TL, Stone EJ, Dunn AL, Blair SN. Physical activity behavior change: issues in adoption and maintenance. Health Psychol. 2000 Jan;19(1S):32–41. doi: 10.1037/0278-6133.19.suppl1.32. [DOI] [PubMed] [Google Scholar]
- 9.Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S.: adults compliance with the Physical Activity Guidelines for Americans. Am J Prev Med. 2011 Apr;40(4):454–61. doi: 10.1016/j.amepre.2010.12.016.S0749-3797(11)00012-2 [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. 2018. Prevalence of insufficient physical activity http://www.who.int/gho/ncd/risk_factors/physical_activity_text/en/
- 11.Zhao G, Ford ES, Li C, Mokdad AH. Compliance with physical activity recommendations in US adults with diabetes. Diabet Med. 2008 Feb;25(2):221–7. doi: 10.1111/j.1464-5491.2007.02332.x.DME2332 [DOI] [PubMed] [Google Scholar]
- 12.Fjeldsoe BS, Miller YD, Marshall AL. MobileMums: a randomized controlled trial of an SMS-based physical activity intervention. Ann Behav Med. 2010 May;39(2):101–11. doi: 10.1007/s12160-010-9170-z. [DOI] [PubMed] [Google Scholar]
- 13.Hurling R, Catt M, Boni MD, Fairley BW, Hurst T, Murray P, Richardson A, Sodhi JS. Using Internet and mobile phone technology to deliver an automated physical activity program: randomized controlled trial. J Med Internet Res. 2007;9(2):e7. doi: 10.2196/jmir.9.2.e7. http://www.jmir.org/2007/2/e7/ v9i2e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gardner B, Lally P. Does intrinsic motivation strengthen physical activity habit? Modeling relationships between self-determination, past behaviour, and habit strength. J Behav Med. 2013 Oct;36(5):488–97. doi: 10.1007/s10865-012-9442-0. [DOI] [PubMed] [Google Scholar]
- 15.Migueles JH, Cadenas-Sanchez C, Ekelund U, Delisle NC, Mora-Gonzalez J, Löf M, Labayen I, Ruiz JR, Ortega FB. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017 Sep;47(9):1821–1845. doi: 10.1007/s40279-017-0716-0.10.1007/s40279-017-0716-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.King AC, Glanz K, Patrick K. Technologies to measure and modify physical activity and eating environments. Am J Prev Med. 2015 May;48(5):630–8. doi: 10.1016/j.amepre.2014.10.005.S0749-3797(14)00582-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.IDC. 2017. Dec 20, IDC Forecasts Shipments of Wearable Devices to Nearly Double by 2021 as Smart Watches and New Product Categories Gain Traction https://www.idc.com/getdoc.jsp?containerId=prUS43408517&pageType=PRINTFRIENDLY .
- 18.Forbes. [2017-07-25]. The World's Most Valuable Brands https://www.forbes.com/powerful-brands/list/
- 19.Canalys. 2016. Apple shipped two-thirds of all smart watches in 2015 https://www.canalys.com/static/press_release/2016/media-alert-05022016-apple-shipped-two-thirds-all-smart-watches-2015.pdf .
- 20.Canalys. 2017. Feb 07, [2017-07-25]. Apple Watch has its best quarter and takes nearly 80% of total smartwatch revenue in Q4 https://www.canalys.com/newsroom/media-alert-apple-watch-has-its-best-quarter-and-takes-nearly-80-total-smartwatch-revenue-q .
- 21.Apple. 2018. [2017-12-27]. Get the most accurate measurements using your Apple Watch https://support.apple.com/en-au/HT207941 .
- 22.Apple. 2018. [2017-12-27]. Your heart rate. What it means, and where on Apple Watch you'll find it https://support.apple.com/en-au/HT204666 .
- 23.Apple. 2018. [2017-07-24]. Use the Activity app on your Apple Watch https://support.apple.com/en-gb/HT204517 .
- 24.Wallen MP, Gomersall SR, Keating SE, Wisløff U, Coombes JS. Accuracy of heart rate watches: implications for weight management. PLoS One. 2016;11(5):e0154420. doi: 10.1371/journal.pone.0154420. http://dx.plos.org/10.1371/journal.pone.0154420 .PONE-D-15-55600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Norton K, Marfell-Jones M, Whittingham M, Kerr D, Carter L, Saddington K, Gore C. Anthropometric assessment protocols. In: Gore CJ, editor. Physiological Tests for Elite Athletes. Champaign, IL: Human Kinetics; 2000. [Google Scholar]
- 26.Miller WM, Spring TJ, Zalesin KC, Kaeding KR, Nori JKE, McCullough PA, Franklin BA. Lower than predicted resting metabolic rate is associated with severely impaired cardiorespiratory fitness in obese individuals. Obesity (Silver Spring) 2012 Mar;20(3):505–11. doi: 10.1038/oby.2011.262. doi: 10.1038/oby.2011.262.oby2011262 [DOI] [PubMed] [Google Scholar]
- 27.Hopkins WG. Spreadsheets for analysis of controlled trials with adjustment for a predictor. 2017. [2017-10-30]. http://www.sportsci.org/2017/wghxls.htm .
- 28.Hopkins WG. A New View of Statistics. 2016. [2017-07-25]. http://www.sportsci.org/resource/stats/
- 29.World Health Organization. 2010. Global recommendations on physical activity for health http://apps.who.int/iris/bitstream/10665/44399/1/9789241599979_eng.pdf .
- 30.Thompson D, Batterham AM, Peacock OJ, Western MJ, Booso R. Feedback from physical activity monitors is not compatible with current recommendations: a recalibration study. Prev Med. 2016 Oct;91:389–394. doi: 10.1016/j.ypmed.2016.06.017. https://linkinghub.elsevier.com/retrieve/pii/S0091-7435(16)30142-6 .S0091-7435(16)30142-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gomersall SR, Ng N, Burton NW, Pavey TG, Gilson ND, Brown WJ. Estimating physical activity and sedentary behavior in a free-living context: a pragmatic comparison of consumer-based activity trackers and ActiGraph accelerometry. J Med Internet Res. 2016 Sep 07;18(9):e239. doi: 10.2196/jmir.5531. http://www.jmir.org/2016/9/e239/ v18i9e239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sushames A, Edwards A, Thompson F, McDermott R, Gebel K. Validity and reliability of Fitbit Flex for step count, moderate to vigorous physical activity and activity energy expenditure. PLoS One. 2016;11(9):e0161224. doi: 10.1371/journal.pone.0161224. http://dx.plos.org/10.1371/journal.pone.0161224 .PONE-D-15-42907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singh MAF. Exercise comes of age: rationale and recommendations for a geriatric exercise prescription. J Gerontol A Biol Sci Med Sci. 2002 May;57(5):M262–82. doi: 10.1093/gerona/57.5.m262. [DOI] [PubMed] [Google Scholar]
- 34.Weaving D, Marshall P, Earle K, Nevill A, Abt G. Combining internal- and external-training-load measures in professional rugby league. Int J Sports Physiol Perform. 2014 Nov;9(6):905–12. doi: 10.1123/ijspp.2013-0444.2013-0444 [DOI] [PubMed] [Google Scholar]
- 35.Abt G, Bray J, Benson A. The validity and inter-device variability of the Apple Watch for measuring maximal heart rate. J Sports Sci. 2017 Nov 01;:1–6. doi: 10.1080/02640414.2017.1397282. [DOI] [PubMed] [Google Scholar]
- 36.Soligard T, Schwellnus M, Alonso J, Bahr R, Clarsen B, Dijkstra HP, Gabbett T, Gleeson M, Hägglund M, Hutchinson MR, Janse VRC, Khan KM, Meeusen R, Orchard JW, Pluim BM, Raftery M, Budgett R, Engebretsen L. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br J Sports Med. 2016 Sep;50(17):1030–41. doi: 10.1136/bjsports-2016-096581.50/17/1030 [DOI] [PubMed] [Google Scholar]
- 37.Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52. doi: 10.2196/jmir.3951. http://www.jmir.org/2015/2/e52/ v17i2e52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barnes KR, Kilding AE. Strategies to improve running economy. Sports Med. 2015 Jan;45(1):37–56. doi: 10.1007/s40279-014-0246-y. [DOI] [PubMed] [Google Scholar]
- 39.Bassett DR, Howley ET. Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med Sci Sports Exerc. 2000 Jan;32(1):70–84. doi: 10.1097/00005768-200001000-00012. [DOI] [PubMed] [Google Scholar]
- 40.Martin PE, Rothstein DE, Larish DD. Effects of age and physical activity status on the speed-aerobic demand relationship of walking. J Appl Physiol (1985) 1992 Jul;73(1):200–6. doi: 10.1152/jappl.1992.73.1.200. [DOI] [PubMed] [Google Scholar]


