Abstract
Background
Smartphone ownership is rising at a stunning rate. Moreover, smartphones prove to be suitable for use in health care due to their availability, portability, user-friendliness, relatively low price, wireless connectivity, far-reaching computing capabilities, and comprehensive memory. To measure vital signs, smartphones are often connected to a mobile sensor or a medical device. However, by using the white light-emitting diode as light source and the phone camera as photodetector, a smartphone could be used to perform photoplethysmography (PPG), enabling the assessment of vital signs.
Objective
The objective of this meta-analysis was to evaluate the available evidence on the use of smartphone apps to measure heart rate by performing PPG in comparison with a validated method.
Methods
PubMed and ISI Web of Knowledge were searched for relevant studies published between January 1, 2009 and December 7, 2016. The reference lists of included studies were hand-searched to find additional eligible studies. Critical Appraisal Skills Programme (CASP) Diagnostic Test Study checklist and some extra items were used for quality assessment. A fixed effects model of the mean difference and a random effects model of Pearson correlation coefficient were applied to pool the outcomes of the studies.
Results
In total, 14 studies were included. The pooled result showed no significant difference between heart rate measurements with a smartphone and a validated method (mean difference −0.32; 99% CI −1.24 to 0.60; P=.37). In adults, the Pearson correlation coefficient of the relation between heart rate measurement with a smartphone and a validated method was always ≥.90. In children, the results varied depending on measuring point and heart rate. The pooled result showed a strong correlation that was significant (correlation coefficient .951; 95% CI 0.906-0.975; P<.001). The reported limits of agreement showed good agreement between a smartphone and a validated method. There was a moderately strong significant negative correlation between the year of publication of the included studies and the mean difference (r=−.69; P<.001).
Conclusions
Smartphone apps measuring heart rate by performing PPG appear to agree with a validated method in an adult population during resting sinus rhythm. In a pediatric population, the use of these apps is currently not validated.
Keywords: mobile applications, heart rate, photoplethysmography, electrocardiography, oximetry, meta-analysis
Introduction
Background
Smartphone ownership rises year by year. Advanced economies still have the highest smartphone ownership rates. Smartphone ownership in countries with an emerging and developing economy, however, is rising at a stunning rate [1].
Due to their availability, portability, user-friendliness, relatively low price, wireless connectivity, far-reaching computing capabilities, and comprehensive memory, smartphones prove to be suitable for use in health care [2-4]. A wide offer of health and medical applications exist from diagnostic tools over professional education to apps supporting patients and health consumers [3,5]. In the field of cardiological literature, there has been a growing interest in mobile apps since 2003 [6].
Measuring Vital Signs
Most of the studies focus on measuring vital signs using a smartphone. To this end, smartphones are mostly connected to a mobile sensor or medical device [6]. A majority of smartphones receive the information through built-in Bluetooth technology. They often process the information before transferring data to a server. At server level, the information can be further processed, organized, and analyzed to create a report for the user [2,4]. Hence, this type of monitoring requires several sensors or a separate device, which can be quite expensive [4].Another way to measure heart rate is by utilizing a pulse oximeter using photoplethysmography (PPG). In total, 2 key components are essential to create a PPG waveform: a light source to illuminate the subcutaneous tissue and a photodetector to detect the changes in light intensity [7]. Jonathan en Leahy demonstrated that a smartphone could be used to perform PPG. The white light-emitting diode can be used as light source and the phone camera as photodetector. The 2 components should be positioned next to each other for reflection mode PPG; in comparison, in transmission mode PPG, the photodetector is placed opposite to the light source [8].
The PPG waveform is influenced by many factors enabling the assessment of vital signs, for example, oxygen saturation, blood pressure, respiratory rate, and heart rate. Promising results show the ability to screen for pathologies related to peripheral vascular disease [7-9]. The purpose of this review was to analyze the available evidence on measuring heart rate by performing PPG using smartphones in comparison with a validated method.
Methods
Literature Search and Selection Criteria
We conducted a systematic literature search of PubMed and ISI Web of Knowledge from January 1, 2009 to December 7, 2016, with the following search key: (smartphone* OR phone* OR ((Applic* OR App*) AND (mobile OR electronic OR software)) OR PPG OR Photoplethysmograph* OR Rheograph*) AND (Electrocardiogr* OR ECG OR EKG or Oximet*) AND ((rate* AND (heart OR pulse)) OR tachycardia* OR beat* OR complex* OR arrhythmia* OR fibrillation*). Only papers in English, German, French, or Dutch were included. The reference lists of included studies were hand-searched to find additional eligible studies.
Studies were included if the measurement of heart rate was conducted with the photo camera of a smartphone by PPG; the measurements were made at a finger, toe, or earlobe; the measurements of the smartphone were compared with an electrocardiogram (ECG), a pulse oximeter, or another validated method to determine heart rate. Studies were excluded if the measurement was conducted with a mobile sensor or medical device connected to a smartphone; the paper did not have heart rate as one of the outcomes; no abstract or full text was available.
Data Extraction and Outcome Measures
Data were extracted by the first author and reviewed by all authors.
Following are study and intervention characteristics extracted from the included studies: first author, study country, study year, sample size, baseline characteristics of participants, age of the participants (mean or range), type of smartphone used, control instrument, duration and conditions of the measurement, and primary outcome measures. The primary outcome measures were the mean difference between heart rate measured by a smartphone and a validated method, the correlation coefficient of the relation between heart rate measurements made by both methods, and the 95% limits of agreement derived from a Bland-Altman plot.
Overall, 1 author was contacted to receive missing data about the heart rate measurements; 2 authors were contacted because of a lack of clarity about the data; and 7 authors were contacted to get access to the full text of the paper; but 2 authors failed to respond to that last request.
Study Quality
Study quality was appraised using the Critical Appraisal Skills Programme (CASP) Diagnostic Test Study checklist [10]. In addition, the included studies were evaluated by extra considerations described in the study of Hanneman [11]. The first was an appraisal tool developed for diagnostic studies. The checklist covered 3 sections: the validity of the results, the actual results, and the utility of the results. With the exception of the questions focusing on the actual results, the topics described were relevant for a method comparison study design. The 9 remaining questions were answered by “yes,” “can’t tell,” or “no.” One question was adapted so that “yes” always indicated a positive answer and “no” a negative answer. “Can’t tell” was answered when there was not enough information found in the study to answer the question. The checklist gave an indication of the quality per section and did not focus on a total score. The latter focused on specific considerations for a method comparison study design. The considerations were converted in 5 questions. These questions were also answered by “yes,” “can’t tell,” or “no.”
The quality assessment was performed by the first author and reviewed by the other authors.
Statistical Methods
In total, 3 different statistics were described, and 2 of them were used for estimation of the pooled result. The first was the mean difference between heart rate measured by a smartphone and a validated method. In case of absence of a mean value and standard deviation in the original paper, it was calculated manually where possible on the basis of the original data.
The second was the Pearson correlation coefficient calculated from the relation between heart rate measured by a smartphone and a validated method. The P value was calculated manually out of the correlation coefficient and sample size if not described in the original paper.
The third were the 95% limits of agreement. They were derived from a Bland-Altman plot. Lower and upper limits were calculated starting from the mean difference by respectively subtracting and adding up the standard deviation of the mean difference between both methods, multiplied by a factor of 1.96. In 2 studies, they were calculated manually starting from the mean difference and the described limit of agreement.
The pooled result was estimated using a fixed- or random-effects model. Statistical heterogeneity was tested using the chi-squared test where a significant result indicated statistical heterogeneity. To quantify inconsistency, the I² of Higgins was used. In case of statistical heterogeneity, a random-effects model was used for pooling the results. Due to the small number of included studies, it was not possible to explore heterogeneity by subgroup analysis or meta-regression [12].
Pearson correlation was used to analyze the relation between different variables (publication year, mean heart rate, and sample size) and the mean difference. The scatter plots of these correlations were drawn.
Statistical analyses were performed using Review Manager Version 5.3 (The Cochrane collaboration, Copenhagen: Denmark: The Nordic Cochrane Centre, 2014), MedCalc 17.4 (MedCalc Software, Ostend: Belgium, 2017), and Microsoft Office Excel 2007 (Microsoft, 2007). Statistical significance level was set at 5%, except for mean difference where statistical significance level was set at 1%.
Results
Study Identification and Selection
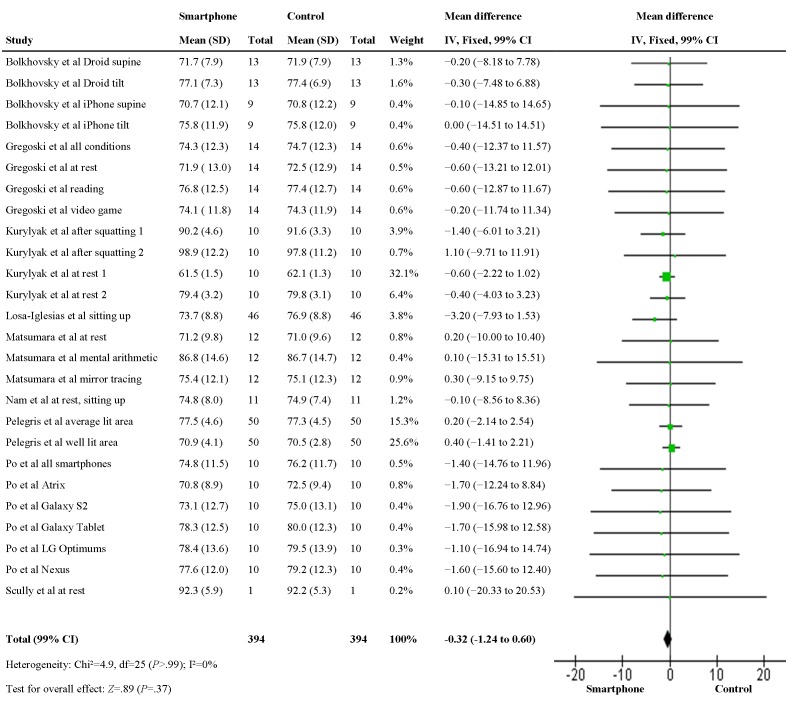
Figure 1 shows a diagram of the search and selection strategy. Initially, 1637 studies were found in 2 databases. First, 312 duplicates—identical studies found in both databases—were removed, followed by 1245 studies on the basis of an irrelevant title. The abstract of the remaining 80 studies was screened of which 55 were excluded for not fulfilling the selection criteria [4,13-66]. The 25 remaining studies were reviewed by reading the full text [8,67-90]. An additional 10 studies were excluded for not fulfilling the selection criteria [8,67,71,72,74,76,81,83,84,86]. For 2 studies, the full text could not be retrieved [69,77]. One paper was added after hand-searching the reference list of the included studies [91]. A total of 14 studies was used for this review and meta-analysis [68,70,73,75,78-80,82,85,87-91].
Figure 1.
Search and selection strategy.
Study Characteristics
Table 1 presents the characteristics of the included studies. In total, 5 studies reported findings on North American participants [68,73,85,89,90], 6 on Western European participants [70,78-80,87,91], and 3 on East Asian participants [75,82,88]. The oldest studies dated from 2010 and the most recent from 2016. Sample sizes varied from 1 to 68, with a median of 24. In total, 8 studies studied an adult population [70,73,78,80,82,85,87,91] and 2 an infant population [75,90], and 4 studies did not mention the age of the participants [68,79,88,89]. In 9 studies, the reference instrument was an ECG [68,70,75,78,79,82,85,89,90]; in 4 studies, a pulse oximeter [80,87,88,91]; and in 1 study, both [73]. The duration of the measurement varied between 10 s and 5 min. Of the selected studies, 2 did not mention the duration of the measurement [89,90]. A total of 5 studies tried to evoke variations in heart rate [68,73,78,82,91], 2 studies controlled the breathing of the participants during measurement [85,89], 1 paper made measurements in different lighting conditions [87], and 1 paper made measurements during different heart rhythms [90]. Overall, 8 studies studied another outcome besides heart rate, namely heart rate variability parameters [68,78,79], other vital parameters [85,89], and other outcomes [70,82,88].
Table 1.
Characteristics of included studies.
| Author, year, and country | Sample size and age (range or mean [SD]) | Smartphone | Control | Duration and conditions measurement | Outcome measure |
| Bolkhovsky et al, 2012, United States [68] | 22 subjects, age not specified | Motorola Droid, iPhone 4S | ECGa | 2 × 2 min: supine and sitting up in tilt position (iPhone 4S, n=9); 2 × 5 min: supine and sitting up in tilt position (Motorola Droid, n=13) | Heart rate, heart rate variability |
| Drijkoningen et al, 2014, Belgium [70] | 28 adults with sinus rhythm during electrophysiological examination, age not specified | Samsung Galaxy S4 | ECG | 60 s | Heart rate, premature atrial ectopic beats identification |
| Gregoski et al, 2012, United States [73] | 14 adults, 18-59 years | Motorola Droid | ECG, pulse oximeter | 3 × 5 min: sitting, at rest, reading, and playing a video game | Heart rate |
| Ho et al, 2014, Taiwan [75] | 40 children undergoing ECG monitoring, 3 days to 15 years | iPhone 4S | ECG | 3 × 20 s at finger (or toe) and earlobe | Heart rate |
| Koenig et al, 2016, Germany [78] | 68 adults (45 patients from a cardiologic outpatient ambulance and 23 healthy controls), 51.7 (18.83) years | iPhone 4S | ECG | 5 min: at rest 2 min: after 3 min of physical exercise (only controls) | Heart rate, heart rate variability |
| Kurylyak et al, 2012, Italy [91] | 10 adults, 26-60 years | HTC HD2, iPhone 4, Nokia 5800, Samsung Galaxy S i9000 | Pulse oximeter | 2 × 60 s (per smartphone): at rest and after 60 s squatting | Heart rate |
| Lagido et al, 2014, Portugal [79] | 43 heart failure patients, age not specified | Sony Xperia S | ECG | At rest | Heart rate, heart rate variability |
| Losa-Iglesias et al, 2016, Spain [80] | 46 healthy adults, 39.3 (7.35) years | Samsung Galaxy Note | Radial pulse, pulse oximeter | 3 × 10-30 s: at rest (resting 10 min before measurements) | Heart rate |
| Matsumara et al, 2013, Japan [82] | 12 students, 21-24 years | iPhone 4S | ECG | 3 × 3 min: at rest (resting 7 min before measurement), during mental arithmetic, and during mirror tracing | Heart rate, normalize pulse volume |
| Nam et al, 2016, United States [85] | 11 healthy nonsmoking adults, 20-40 years | HTC One M8 | ECG | 3 × 2 min: breathing at frequencies from 0.1 to 0.5 Hz at increments of 0.1 Hz, breathing at 1 Hz and spontaneous breathing | Heart rate and breathing rate |
| Pelegris et al, 2010, UK [87] | 50 adults, 21-55 years | HTC Tattoo | Pulse oximeter | 2 × 9 s: well-lit room and average lit room | Heart rate |
| Po et al, 2015, China [88] | 10 subjects, age not specified | Samsung Galaxy Nexus, LG Optimus P920, Samsung Galaxy S2, Samsung Galaxy Tablet 7.0, Motorala Atrix | Pulse oximeter | 1 × 20 s | Heart rate and root mean square distortion of heart rate |
| Scully et al, 2012, United States [89] | 1 subject, age not specified | Motorola Droid | ECG | 1 × ?: spontaneous breathing 3 × 2 min: breathing at 0.2, 0.3, and 0.4 Hz |
Heart rate, respiration rate, oxygen saturation |
| Wackel et al, 2014, United States [90] | 26 children undergoing an electrophysiology study under general anesthesia, 5-17 years | iPhone 5 | ECG | 2 × ?: during baseline heart rate (34 measurements in 17 children) 2 × ?: during sustained supraventricular tachycardia (38 measurements during 21 supraventricular tachycardia in 18 children) |
Heart rate |
aECG: electrocardiogram.
Study Quality
Table 2 presents the quality assessment of the included studies. The quality assessment questions are listed in Textbox 1. All studies had a clear study question and compared the measurements of the smartphone with an appropriate reference standard. Due to the type of test, it was not possible that the measurement of the reference standard influenced the measurement of the smartphone. Also, both methods did measure the same outcome simultaneously. Totally, 5 studies made a clear description of the disease status of the participants [70,73,80,82,90]. Just over half of the studies described the methods for performing the test in sufficient detail [68,70,73,75,78,80,82,85]. Half of the studies provided enough information about the participants to conclude that the results may be applicable to the population of interest [73,75,78,80,82,85,90]. All studies had the same relevant outcome and performed their measurements in a similar way. All but one [82] studies acknowledged that the sample size was small. In 6 studies, the authors made an effort to measure a wide range of the possible physiological values of heart rate [68,73,78,82,90,91]. Only 3 studies used a cutoff value for the clinical acceptable difference between the measurements made by the 2 methods [73,75,80].
Table 2.
Study quality according to Critical Appraisal Skills Programme Diagnostic Test study checklist and extra considerations. Y indicates yes; N indicates no; and C indicates can’t tell.
| Study | Validity of results | Utility of results | Extra considerations | |||||||||||||
|
|
Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q9 | Q10 | Q11 | E1 | E2 | E3 | E4 | E5 | ||
| Bolkhovsky et al | Y | Y | Y | Y | N | Y | C | Y | Y | Y | Y | N | Y | N | ||
| Drijkoningen et al | Y | Y | Y | Y | Y | Y | C | Y | Y | Y | Y | N | N | N | ||
| Gregoski et al | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | ||
| Ho et al | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | N | N | Y | ||
| Koenig et al | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | N | Y | N | ||
| Kurylyak et al | Y | Y | Y | Y | N | N | C | Y | Y | Y | Y | N | Y | N | ||
| Lagido et al | Y | Y | Y | Y | N | N | C | Y | Y | Y | Y | N | C | N | ||
| Losa-Iglesias et al | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | N | Y | ||
| Matsumara et al | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | N | ||
| Nam et al | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | N | N | N | ||
| Pelegris et al | Y | Y | Y | Y | N | N | C | Y | Y | Y | Y | N | N | N | ||
| Po et al | Y | Y | Y | Y | N | N | C | Y | Y | Y | Y | N | N | N | ||
| Scully et al | Y | Y | Y | Y | N | N | C | Y | Y | Y | Y | N | N | N | ||
| Wackel et al | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | N | Y | N | ||
Quality assessment questions.
Critical Appraisal Skills Programme Diagnostic study checklist
-
Validity of results
Was there a clear question for the study to address?
Was there a comparison with an appropriate reference standard?
Did all patients get the diagnostic test and reference standard?
Is there no possibility that the results of the test have been influenced by the results of the reference standard?
Is the disease status of the tested population clearly described?
Were the methods for performing the test described in sufficient detail?
-
Utility of results
Can the results be applied to your patients/the population of interest?
Can the test be applied to your patient or population of interest?
Were all outcomes important to the individual or population considered?
Extra considerations
Do both methods measure the same outcome?
Do both methods measure the outcome simultaneous?
Did the investigators motivate their choice for the sample size?
Did the investigators test both methods in different conditions to simulate the possible physiological range of values?
Did the investigators set up cutoff values for the clinical acceptable difference between both methods?
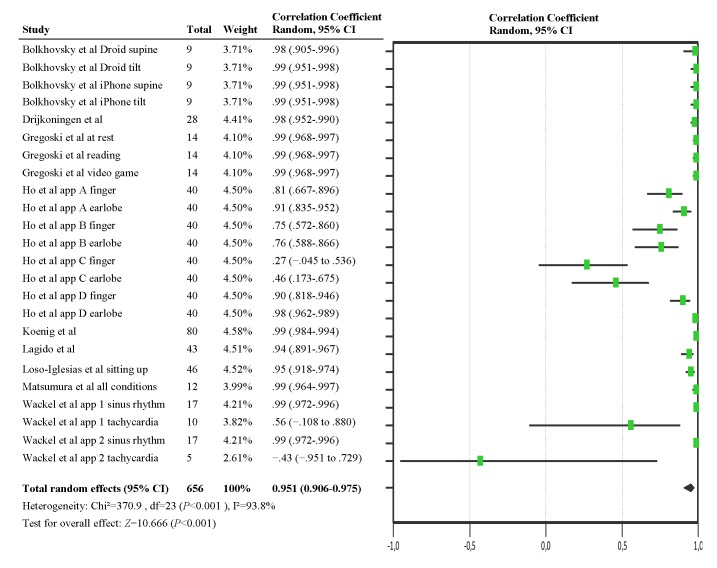
Primary Outcome: Heart Rate
The mean difference between heart rate measured by a smartphone and a validated method was analyzed in a fixed-effects model (Figure 2). This statistic was reported in 7 studies [68,73,80,82,88,89,91]. For 2 studies, it was calculated manually out of the original data [85,87]. In 2 studies, the mean difference was consistently positive [82,89]; and in 5 studies, negative [73,80,85,87,88]. In 2 studies, the mean difference was negative, except for 1 condition where there was no difference [68] or the mean difference was positive [91]. The pooled estimate of the 9 included studies suggested that there is no difference between both methods (mean difference −0.32; 99% CI −1.24 to 0.60; P=.37). No statistical heterogeneity was observed among the studies (I²=0%; P>.99).
Figure 2.
Forest plot for the meta-analysis of mean difference.
Table 3 shows the correlation coefficient of the relation between heart rate measurement with a smartphone and a validated reference method. This statistic was reported in 9 studies [68,70,73,75,78-80,82,90]. Previous research stated that the correlation between 2 methods that measure heart rate should be ≥.90 to be considered as valid [92]. In 7 studies, the correlation coefficient was always ≥.90 and the result was statistical significant [68,70,73,78-80,82]. The 2 studies that studied a pediatric population showed more variation in their results. In 1 , the correlation coefficients were remarkably lower during periods of tachycardia, namely .56 and −.43 [90] and not statistical significant for the latter. In 1 paper, the correlation coefficient was only ≥.90 in 2 of the 4 apps. In 1 of these 2 apps, this was just the case for measurements at the earlobe [75].
Table 3.
Results for heart rate: Pearson correlation coefficient.
| Study | Conditions (sample size) | r a | r ≥.90? | P valueb |
| Bolkhovsky et al | iPhone supine (9) | >.99 | Yes | <.001c |
|
|
iPhone tilt (9) | >.99 | Yes | <.001c |
|
|
Droid supine (13) | .98 | Yes | <.001c |
|
|
Droid tilt (13) | >.99 | Yes | <.001c |
| Drijkoningen et al | Not specified (28) | .98 | Yes | <.001 |
| Gregoski et al | At rest (14) | .99 | Yes | <.001c |
|
|
Reading (14) | .99 | Yes | <.001c |
|
|
Video game (14) | .99 | Yes | <.001 |
| Ho et al | App A finger (40) | .81 | No | <.001 |
|
|
App A earlobe (40) | .91 | Yes | <.001 |
|
|
App B finger (40) | .75 | No | <.001 |
|
|
App B earlobe (40) | .76 | No | <.001 |
|
|
App C finger (40) | .27 | No | .10 |
|
|
App C earlobe (40) | .46 | No | .003 |
|
|
App D finger (40) | .90 | Yes | <.001 |
|
|
App D earlobe (40) | .98 | Yes | <.001 |
| Koenig et al | 80 randomly chosen intervals at rest or after exercise (68) | >.99 | Yes | <.001c |
| Lagido et al | At rest (43) | .94 | Yes | <.001c |
| Losa-Iglesias et al | Sitting up (46) | .95 | Yes | <.001 |
| Matsumura et al | All conditions (12) | .99 | Yes | <.001c |
| Wackel et al | App 1 sinus rhythm (17) | .99 | Yes | <.001c |
|
|
App 1 tachycardia (10 succeeded attempts) | .56 | No | .01c |
|
|
App 2 sinus rhythm (17) | .99 | Yes | <.001c |
|
|
App 2 tachycardia (5 succeeded attempts) | −.43 | No | .09c |
ar value of Pearson correlation coefficient.
bP value calculated with Pearson correlation.
cData based on own calculations.
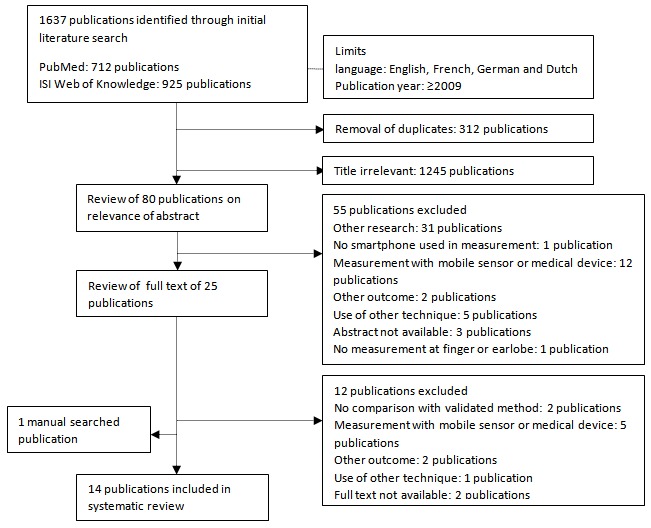
The correlation between heart rate measurements made by a smartphone and a control instrument was analyzed in a random-effects model (Figure 3). The pooled correlation coefficient made the assumption that on average measurements made by a smartphone are highly correlated to those made by a control instrument (correlation coefficient .951; 95% CI 0.906-0.975; P<.001). Of note, statistical heterogeneity was high (I²=93.8%; P<.001), indicating variability across the studies.
Figure 3.
Forest plot for the meta-analysis of Pearson correlation coefficient.
Table 4 shows the 95% limits of agreement for the MD between measurements with a smartphone and a validated method. This statistic was reported in 4 studies [80,82,85,88]. For 2 studies, it was calculated manually [68,73]. In all studies, the limits of agreement did not exceed 10 beats per minute.
Table 4.
Results for heart rate: 95% limits of agreement.
| Study | Conditions (sample size) | 95% LOAa (BPMb), control—smartphone |
| Bolkhovsky et al | iPhone supine (9) | −0.4 to 0.2c |
|
|
iPhone tilt (9) | −0.3 to 0.3c |
|
|
Droid supine (13) | −3.4 to 3.0c |
|
|
Droid tilt (13) | −1.7 to 1.1c |
| Gregoski et al | Video game (14) | −3.9 to 3.7c |
| Loso-Iglesias et al | Sitting up (46) | −8.5 to 2.0 |
| Matsumura et al | All conditions (12) | −1.0 to 1.4 |
| Nam et al | At rest, sitting up (11) | −5.6 to 5.5 |
| Pot et al | Average all smartphones (10) | −4.1 to 1.2 |
aLOA: limits of agreement.
bBPM: beats per minute.
cData based on own calculations.
Correlations With the Mean Difference
The correlation between the mean heart rate measured by a validated method, the sample size of the included studies, and the year of publication of the included studies and the mean difference was analyzed in Figures 4-6, respectively. Correlations between the mean difference and the mean heart rate measured by a validated instrument (r=.13) and sample size (r=−.06) were not significant. However, data showed a moderately strong correlation between the year of publication and the mean difference (r=−.69; P<.001).
Figure 4.
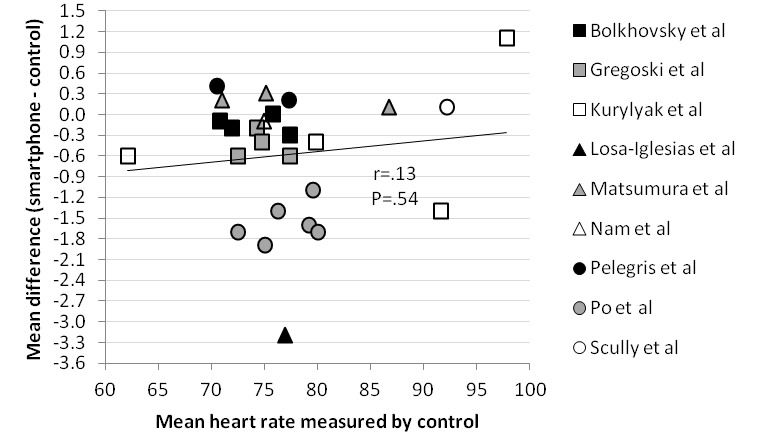
Scatter plot comparing correlation between mean heart rate measured by control and mean difference.
Figure 6.
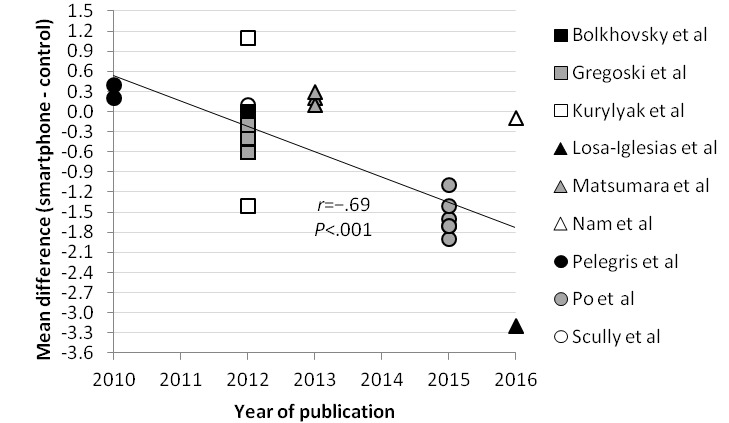
Scatter plot comparing correlation between year of publication and mean difference.
Figure 5.
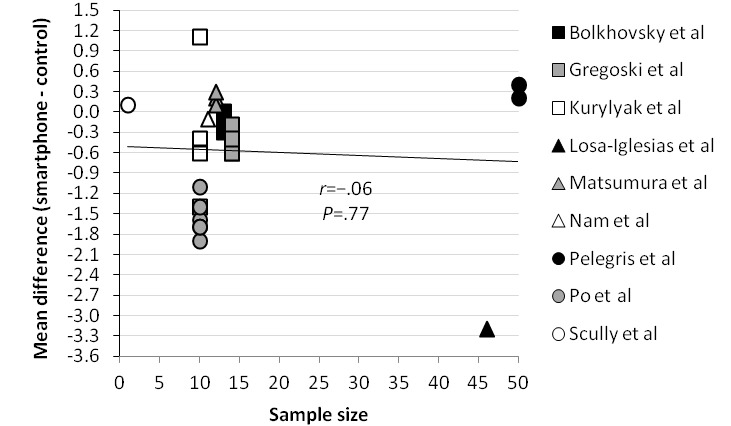
Scatter plot comparing correlation between sample size and mean difference.
Discussion
Principal Findings
The meta-analysis of the mean difference showed no statistical difference between the measurement of heart rate by a smartphone and a validated method (mean difference −0.32; 99% CI −1.24 to 0.60; P=.37). The pooled correlation coefficient between heart rate measurement by a smartphone and a validated method was more than .90 and statistically significant (correlation coefficient .951; 95% CI 0.906-0.975; P<.001). Reported 95% limits of agreement had a narrow range and therefore showed good agreement between a smartphone and a validated method. These results suggest that a smartphone app deriving heart rate from a PPG signal could be used as an alternative for already validated methods such as an ECG or pulse oximeter in an adult population in resting sinus rhythm. However, the significant negative correlation between the year of publication of the included studies and the mean difference (r=−.69; P<.001) suggests that smartphone technology for measuring heart rate did not improve over time. There was no significant correlation between the mean difference and the mean heart rate measured by a validated method (r=.13; P=.54) or the sample size of the included studies (r=−.06; P=.77), which suggests that smartphone results are consistent for heart rate measurements between 60 and 100 beats per minute.
Considerations
First, the results of the studies in a pediatric population showed that it is not advisable yet to use these apps in children. A possible cause is that because of the smaller size of children’s fingertips, the pulsatile flow may be less consistently detected. The use of the earlobe as a measuring point may present a possible solution. Children may also have difficulties in containing the appropriate pressure on the camera lens and keeping their finger motionless to make a good measurement [73,75,90].
A second issue is heart rate measurement during periods of arrhythmia [4]. The low correlation between measurements with a smartphone and a validated method during periods of supraventricular tachycardia in children suggests that current apps do not give adequate results during periods of extremely high heart rates [90]. Moreover, the smartphone apps in the studies used PPG, calculating the heart rate on basis of the pulse rate. Hence, the results may not be accurate enough during periods of arrhythmia with variations in pulse rate and amplitude due to heart rhythm irregularities [4,82]. A solution is to improve sensitivity and specificity of the apps for deviant heart rhythms depending on the purpose of the apps [62].
Third, previous research stated that heart rate measurement can be susceptible to environmental or human factors such as ambient light, motion [4,93], or skin color [7]. In total, 3 studies reported about lighting conditions [87,88,91]. In these studies, ambient light did not seem to have an influence, but it should still be taken into account. On the basis of this review, it is not possible to say something about the influence of motion, as none of the included studies tested whether accurate pulse rate is measurable by the smartphone apps during exercise. However, several studies do mention this limitation in their discussion. Wearable devices using PPG possibly provide better results during exercise [94]. Only 1 paper mentioned to have included participants with a variety of skin colors but did not make a comparison between different skin types [73]. Hereby, we cannot come to a conclusion about the topic in this review. When using PPG to measure heart rate, it should be taken into account to use a proper light wavelength that gives equal results for people with different skin types [95].
Fourth, it was remarkable that in the included studies the mean difference became more and more negative over time. A plausible explanation is that every paper focuses on (a) certain type(s) of smartphone model(s) or app(s). Consequently, the results cannot be automatically projected to other smartphones and apps [4]. The use of certain smartphones or apps could lead to better results.
Strengths and Limitations
First of all, to the best of our knowledge, this was the first systematic review and meta-analysis evaluating smartphone apps using PPG to measure heart rate. A comprehensive search strategy was used, including every paper investigating smartphone apps deriving heart rate measurement from a PPG signal. At last, there was a focus on different statistics for assessing agreement between methods.
Nevertheless, there were some limitations of the included studies. First, the methodological quality was often low, reflected by the fact that only 3 studies scored 12 or more out of 14 on the quality assessment questions [73,80,82].
Second, most of the mean heart rates that were reported lay between 70 and 80 beats per minute. As a result, it was not possible to investigate whether smartphones could be used to measure the higher physiological ranges of heart rate.
Third, only 8 of the included studies [68,70,73,78,80,82,85,88] used the most appropriate method to determine agreement between the 2 methods, the Bland-Altman plot [96,97]. Of these studies, only 2 mentioned a conclusion of the results, which were in line with the findings of the review [70,78]. A consideration about this method is that it is not easy to determine good agreement [96]. In the literature, no description was found of the maximum heart rate deviation to be clinical relevant. A deviation of under 10 beats per minute has no important clinical implications but does indicate small alterations when repeating the measures. The other methods can support the findings but have their limitations. A Pearson correlation gives information about the relation between methods, but a high correlation does not necessarily mean that the 2 methods agree [97,98]. When using a mean difference, poor agreement can be hidden by looking at the mean difference, without exploring the individual values (eg, an overestimation of high heart rates in combination with an underestimation of low heart rates will also give a mean difference of 0) [97].
A fourth and last limitation is a high statistical heterogeneity between studies on the level of correlation coefficients. This is likely attributable to clinical heterogeneity caused by differences in patient characteristics (eg, adults vs children), the conditions in which the heart rates were measured (eg, at sinus rhythm vs during a period of tachycardia), and which smartphone or app was used [12].
All these factors may influence the generalizability of the results.
In addition, there were some limitations specific to the review. The data were extracted by the first author only; however, they were thoroughly reviewed by the other authors, of which one is specialized in cardiology. In addition, 2 studies were excluded because the full text could not be retrieved [69,77]; the results described in the abstracts of those studies agreed with the pooled results, so their exclusion would probably have a minimal effect.
Conclusions
This meta-analysis suggests that heart rate measured by smartphone apps performing PPG agrees with a validated method in an adult population in resting sinus rhythm, provided that during measurement the measuring point was kept still and that appropriate pressure was maintained. In a pediatric population, the use of these apps can currently not be supported, especially not during periods of tachycardia. Future research with a larger and more diverse study population should be conducted. The technology should also be tested in more varied clinical situations evoking variations in normal heart rate and during arrhythmias.
Abbreviations
- CASP
Critical Appraisal Skills Programme
- ECG
electrocardiogram
- PPG
photoplethysmography
Footnotes
Authors' Contributions: BDR made most of the contributions to conception and design, to the acquisition of data, and to analysis and interpretation of data. The other authors played an important role in acquiring missing data and revising it critically for important intellectual content. All authors reviewed and approved the data and the final text.
Conflicts of Interest: None declared.
References
- 1.Poushter J. Pewglobal. 2016. [2017-01-06]. Smartphone Ownership and Internet Usage Continues to Climb in Emerging Economies http://www.pewglobal.org/2016/02/22/smartphone-ownership-rates-skyrocket-in-many-emerging-economies-but-digital-divide-remains/
- 2.Baig MM, GholamHosseini H, Connolly MJ. Mobile healthcare applications: system design review, critical issues and challenges. Australas Phys Eng Sci Med. 2015 Mar;38(1):23–38. doi: 10.1007/s13246-014-0315-4. [DOI] [PubMed] [Google Scholar]
- 3.Sarasohn-Kahn J. CHCF. 2010. [2017-08-06]. How Smartphones Are Changing Health Care for Consumers and Providers http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/PDF%20H/PDF%20HowSmartphonesChangingHealthCare.pdf .
- 4.Bruining N, Caiani E, Chronaki C, Guzik P, van der Velde E, Task Force of the e-Cardiology Working Acquisition and analysis of cardiovascular signals on smartphones: potential, pitfalls and perspectives: by the Task Force of the e-Cardiology Working Group of European Society of Cardiology. Eur J Prev Cardiol. 2014 Nov;21(2 Suppl):4–13. doi: 10.1177/2047487314552604.21/2_suppl/4 [DOI] [PubMed] [Google Scholar]
- 5.Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res. 2012;14(5):e128. doi: 10.2196/jmir.1994. http://www.jmir.org/2012/5/e128/ v14i5e128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martínez-Pérez B, de la Torre-Diez I, López-Coronado M, Herreros-González J. Mobile apps in cardiology: review. JMIR Mhealth Uhealth. 2013;1(2):e15. doi: 10.2196/mhealth.2737. http://mhealth.jmir.org/2013/2/e15/ v1i2e15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Allen J. Photoplethysmography and its application in clinical physiological measurement. Physiol Meas. 2007 Mar;28(3):R1–39. doi: 10.1088/0967-3334/28/3/R01.S0967-3334(07)14869-3 [DOI] [PubMed] [Google Scholar]
- 8.Jonathan E, Leahy M. Investigating a smartphone imaging unit for photoplethysmography. Physiol Meas. 2010 Nov;31(11):N79–83. doi: 10.1088/0967-3334/31/11/N01.S0967-3334(10)53334-3 [DOI] [PubMed] [Google Scholar]
- 9.Elgendi M. On the analysis of fingertip photoplethysmogram signals. Curr Cardiol Rev. 2012 Feb;8(1):14–25. doi: 10.2174/157340312801215782. http://europepmc.org/abstract/MED/22845812 .CCR-8-1-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Critical Appraisal Skills Programme. 2016. 12 questions to help you make sense of a diagnostic test study http://docs.wixstatic.com/ugd/dded87_5f100f2d207a462a8dd552bfb6090d60.pdf .
- 11.Hanneman SK. Design, analysis, and interpretation of method-comparison studies. AACN Adv Crit Care. 2008;19(2):223–34. doi: 10.1097/01.AACN.0000318125.41512.a3. http://europepmc.org/abstract/MED/18560291 .01256961-200804000-00017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deeks JJ, Higgins JP, Altman DG. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. UK: Cochrane Collaboration; 2011. [Google Scholar]
- 13.Weng J, Guo XM, Chen LS, Yuan ZH, Ding XR, Lei M. Study on real-time monitoring technique for cardiac arrhythmia based on smartphone. J Med Biol Eng. 2013;33(4):394. doi: 10.5405/jmbe.1278. [DOI] [Google Scholar]
- 14.Waks JW, Fein AS, Das S. Wide complex tachycardia recorded with a smartphone cardiac rhythm monitor. JAMA Intern Med. 2015 Mar;175(3):437–9. doi: 10.1001/jamainternmed.2014.7586.2091739 [DOI] [PubMed] [Google Scholar]
- 15.Tofield A. Cardiac arrhythmia challenge: a new app. Eur Heart J. 2013 Nov;34(44):3392. [PubMed] [Google Scholar]
- 16.Tan YY, Chung WY. Mobile health-monitoring system through visible light communication. Biomed Mater Eng. 2014;24(6):3529–38. doi: 10.3233/BME-141179.Y502781266514T62 [DOI] [PubMed] [Google Scholar]
- 17.Tabing A, Harrell T, Francisco G, Romero S. Supraventricular tachycardia diagnosed by smartphone electrocardiography. J Am Coll Cardiol. 2016 Apr;67(13):1237. doi: 10.1016/S0735-1097(16)31238-4. [DOI] [Google Scholar]
- 18.Su Y, Yin L, Al-Hakim L. Ephone: embedded cardiac care device in mobile phone. Sen Lett. 2011 Oct 01;9(5):1974–1978. doi: 10.1166/sl.2011.1542. [DOI] [Google Scholar]
- 19.Petersen CL, Chen TP, Ansermino JM, Dumont GA. Design and evaluation of a low-cost smartphone pulse oximeter. Sensors (Basel) 2013 Dec 06;13(12):16882–93. doi: 10.3390/s131216882. http://www.mdpi.com/resolver?pii=s131216882 .s131216882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peng RC, Zhou XL, Lin WH, Zhang YT. Extraction of heart rate variability from smartphone photoplethysmograms. Comput Math Methods Med. 2015;2015:516826. doi: 10.1155/2015/516826. doi: 10.1155/2015/516826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oster J, Behar J, Colloca R, Li Q, Li Q, Clifford G. Open source Java-based ECG analysis software and Android app for Atrial Fibrillation screening. Computing in Cardiology Conference (CinC); September 22-25, 2013; Zaragoza, Spain. 2013. [Google Scholar]
- 22.Orchard J, Freedman SB, Lowres N, Peiris D, Neubeck L. iPhone ECG screening by practice nurses and receptionists for atrial fibrillation in general practice: the GP-SEARCH qualitative pilot study. Aust Fam Physician. 2014 May;43(5):315–9. http://www.racgp.org.au/afp/2014/may/iphone-ecg-screening/ [PubMed] [Google Scholar]
- 23.Nyotowidjojo I, Erickson RP, Lee KS. Crowd-sourcing syncope diagnosis: mobile smartphone ECG apps. Am J Med. 2016 Apr;129(4):e17–8. doi: 10.1016/j.amjmed.2015.11.022.S0002-9343(15)30021-8 [DOI] [PubMed] [Google Scholar]
- 24.Nguyen HH, Van Hare GF, Rudokas M, Bowman T, Silva JN. SPEAR trial: smartphone pediatric electrocARdiogram trial. PLoS One. 2015;10(8):e0136256. doi: 10.1371/journal.pone.0136256. http://dx.plos.org/10.1371/journal.pone.0136256 .PONE-D-15-26592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li JP, Berry D, Hayes R. A mobile ECG monitoring system with context collection. 4th European Conference of the International Federation for Medical and Biological Engineering; November 23-27; Antwerp, Belgium. 2009. pp. 1222–1225. [DOI] [Google Scholar]
- 26.Lee J, Reyes BA, McManus DD, Mathias O, Chon KH. Atrial fibrillation detection using an iPhone 4S. IEEE Trans Biomed Eng. 2013 Jan;60(1):203–6. doi: 10.1109/TBME.2012.2208112. [DOI] [PubMed] [Google Scholar]
- 27.Landreani F, Martin-Yebra A, Casellato C, Frigo C, Pavan E, Migeotte P, Caiani EG. Beat-to-beat heart rate detection by smartphone's accelerometers: validation with ECG. IEEE 38th Annual International Conference of Engineering in Medicine and Biology Society (EMBC), 2016; August 16-20, 2016; Orlando, FL, USA. 2016. Aug, pp. 525–528. [DOI] [PubMed] [Google Scholar]
- 28.Kwon S, Lee J, Chung GS, Park KS. Validation of heart rate extraction through an iPhone accelerometer. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:5260–3. doi: 10.1109/IEMBS.2011.6091301. [DOI] [PubMed] [Google Scholar]
- 29.Kwon S, Kim H, Park KS. Validation of heart rate extraction using video imaging on a built-in camera system of a smartphone. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:2174–7. doi: 10.1109/EMBC.2012.6346392. [DOI] [PubMed] [Google Scholar]
- 30.Kirtava Z, Gegenava T, Gegenava M, Matoshvili Z, Kasradze S, Kasradze P. Mobile telemonitoring for arrhythmias in outpatients in the Republic of Georgia: a brief report of a pilot study. Telemed J E Health. 2012 Sep;18(7):570–1. doi: 10.1089/tmj.2011.0170. http://europepmc.org/abstract/MED/22827508 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karapetyan G, Barseghyan R, Sarukhanyan H, Agaian S. Development and validation of an improved smartphone heart rate acquisition system. Image Process Algorithms Syst XIII. 2015;9399 doi: 10.1117/12.2083381. https://www.spiedigitallibrary.org/conference-proceedings-of-spie/9399/1/Development-and-validation-of-an-improved-smartphone-heart-rate-acquisition/10.1117/12.2083381.short?SSO=1 . [DOI] [Google Scholar]
- 32.Jokic S, Krco S, Sakac D, Jokic ID, Delic V. Autonomic telemedical application for Android based mobile devices. Eleventh Symposium on Neural Network Applications in Electrical Engineering; September 20-22, 2012; Belgrade, Serbia. 2012. [DOI] [Google Scholar]
- 33.Jaworek J, Augustyniak P. A cardiac telerehabilitation application for mobile devices. Computing in Cardiology; September 18-21, 2011; Hangzhou, China. 2011. [Google Scholar]
- 34.Issac R, Ajaynath MS. CUEDETA: a real time heart monitoring system using Android smartphone. India Conference (INDICON); December 7-9, 2012; Kochi, India. Cuedeta: 2012. [DOI] [Google Scholar]
- 35.Işik AH, Güler I. Pulse oximeter based mobile biotelemetry application. Stud Health Technol Inform. 2012;181:197–201. [PubMed] [Google Scholar]
- 36.de Oliveira IH, Cene VH, Balbinot A. Portable electrocardiograph through Android application. 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), 2015; August 25-29, 2015; Milan, Italy. 2015. pp. 6780–3. [DOI] [PubMed] [Google Scholar]
- 37.Hadiyoso S, Usman K, Rizal A. Arrhythmia detection based on ECG signal using Android mobile for athlete and patient. 2015 3rd International Conference on Information and Communication Technology (ICoICT); May 27-29, 2015; Nusa Dua, Bali. 2015. [DOI] [Google Scholar]
- 38.Gradl S, Kugler P, Lohmuller C, Eskofier B. Real-time ECG monitoring and arrhythmia detection using Android-based mobile devices. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:2452–5. doi: 10.1109/EMBC.2012.6346460. [DOI] [PubMed] [Google Scholar]
- 39.Filipovic N, Stojanovic R, Lekic N, Caplanova A. Monitoring and analysis of vital physiological parameters using PDA devices. 24th International Conference Radioelektronika (Radioelektronika); April 15-16, 2014; Bratislava, Slovakia. 2014. [Google Scholar]
- 40.Filipovic N, Stojanovic R, Debevc M, Devedzic G. On line ECG processing and visualization using Android smartphone. 2nd Mediterranean Conference on Embedded Computing (Meco); June 15-20, 2013; Budva, Serbia. 2013. [DOI] [Google Scholar]
- 41.Fernandes B, Afonso JA, Simoes R. Vital signs monitoring and management using mobile devices. 6th Iberian Conference on Information Systems and Technologies; June 15-18, 2011; Chaves, Portugal. 2011. [Google Scholar]
- 42.Ferdman DJ, Liberman L, Silver ES. A smartphone application to diagnose the mechanism of pediatric supraventricular tachycardia. Pediatr Cardiol. 2015 Oct;36(7):1452–7. doi: 10.1007/s00246-015-1185-6.10.1007/s00246-015-1185-6 [DOI] [PubMed] [Google Scholar]
- 43.Cruz T, Brás S, Soares SC, Fernandes JM. Monitoring physiology and behavior using Android in phobias. Conf Proc IEEE Eng Med Biol Soc. 2015 Aug;2015:3739–42. doi: 10.1109/EMBC.2015.7319206. [DOI] [PubMed] [Google Scholar]
- 44.Choo KY, Ling HC, Lo YC, Yap ZH, Pua JS, Phan RC, Goh VT. Android based self-diagnostic electrocardiogram system for mobile healthcare. Technol Health Care. 2015;23 Suppl 2:S435–42. doi: 10.3233/THC-150980.THC980 [DOI] [PubMed] [Google Scholar]
- 45.Banos O, Damas M, Glossekotter P, Hermes A, Mende H, Pomares H, Rojas I. Physiodroid: an app for physiological data monitoring. International Work-Conference on Bioinformatics and Biomedical Engineering; March 18-20, 2013; Granada, Spain. 2013. [Google Scholar]
- 46.Amiri AM, Abhinav. Mankodiya K. m-QRS: an efficient QRS detection algorithm for mobile health applications. 17th International Conference on E-Health Networking, Application & Services (Healthcom); October 14-17, 2015; Boston, MA, USA. 2015. [DOI] [Google Scholar]
- 47.Abi Zeid Daou R, Aad E, Nakhle F, Hayek A, Borcsok J. Patient vital signs monitoring via Android application. 2015 International Conference on Advances in Biomedical Engineering (ICABME); Beirut, Lebanon; September 16-18, 2015. 2015. [DOI] [Google Scholar]
- 48.No authors listed ECG? There's an app for that! Harv Heart Lett. 2013 Mar;23(7):8. [PubMed] [Google Scholar]
- 49.Winkler S, Schieber M, Lücke S, Heinze P, Schweizer T, Wegertseder D, Scherf M, Nettlau H, Henke S, Braecklein M, Anker SD, Koehler F. A new telemonitoring system intended for chronic heart failure patients using mobile telephone technology--feasibility study. Int J Cardiol. 2011 Nov 17;153(1):55–8. doi: 10.1016/j.ijcard.2010.08.038.S0167-5273(10)00628-5 [DOI] [PubMed] [Google Scholar]
- 50.Vashist SK, Schneider EM, Luong JH. Commercial smartphone-based devices and smart applications for personalized healthcare monitoring and management. Diagnostics (Basel) 2014 Aug 18;4(3):104–28. doi: 10.3390/diagnostics4030104. http://www.mdpi.com/resolver?pii=diagnostics4030104 .diagnostics4030104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Saldarriaga AJ, Perez JJ, Restrepo J, Bustamante J. A mobile application for ambulatory electrocardiographic monitoring in clinical and domestic environments. 2013 Pan American Health Care Exchanges (PAHCE); 29 April-4 May, 2013; Medellin, Colombia. 2013. [DOI] [Google Scholar]
- 52.Plesnik E, Malgina O, Tasic JF, Zajc M. ECG signal acquisition and analysis for telemonitoring. 15th IEEE Mediterranean Electrotechnical Conference (MELECON 2010); April 26-28, 2010; Valletta, Malta. 2010. [DOI] [Google Scholar]
- 53.Mittal S. Smartphone-based electrocardiographic and cardiac implantable electronic device monitoring. Cardiol Rev. 2017;25(1):12–16. doi: 10.1097/CRD.0000000000000132.00045415-201701000-00005 [DOI] [PubMed] [Google Scholar]
- 54.Mattila J, Ding H, Mattila E, Särelä A. Mobile tools for home-based cardiac rehabilitation based on heart rate and movement activity analysis. Conf Proc IEEE Eng Med Biol Soc. 2009;2009:6448–52. doi: 10.1109/IEMBS.2009.5333540. [DOI] [PubMed] [Google Scholar]
- 55.Mateev H, Simova I, Katova T, Dimitrov N. Clinical evaluation of a mobile heart rhythm telemonitoring system. ISRN Cardiol. 2012;2012:192670. doi: 10.5402/2012/192670. doi: 10.5402/2012/192670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Madias JE. A proposal for monitoring patients with heart failure via “smart phone technology”-based electrocardiograms. J Electrocardiol. 2016;49(5):699–706. doi: 10.1016/j.jelectrocard.2016.06.001.S0022-0736(16)30066-8 [DOI] [PubMed] [Google Scholar]
- 57.Kumpusch H, Hayn D, Kreiner K, Falgenhauer M, Mor J, Schreier G. A mobile phone based telemonitoring concept for the simultaneous acquisition of biosignals physiological parameters. Stud Health Technol Inform. 2010;160(Pt 2):1344–8. [PubMed] [Google Scholar]
- 58.Kumar M, Veeraraghavan A, Sabharwal A. DistancePPG: Robust non-contact vital signs monitoring using a camera. Biomed Opt Express. 2015 May 01;6(5):1565–88. doi: 10.1364/BOE.6.001565. http://europepmc.org/abstract/MED/26137365 .1565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guzik P, Malik M. ECG by mobile technologies. J Electrocardiol. 2016;49(6):894–901. doi: 10.1016/j.jelectrocard.2016.07.030.S0022-0736(16)30108-X [DOI] [PubMed] [Google Scholar]
- 60.Gonzalez-Fernandez R, Mulet-Cartaya M, Lopez-Cardona JD, Lopez-Rodriguez R. A mobile application for cardiac rhythm study. Computing in Cardiology Conference (CinC); September 6-9, 2015; Nice, France. 2015. [DOI] [Google Scholar]
- 61.Garabelli P, Stavrakis S, Po S. Smartphone-based arrhythmia monitoring. Curr Opin Cardiol. 2017 Jan;32(1):53–57. doi: 10.1097/HCO.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 62.Freedman B. Screening for atrial fibrillation using a smartphone: is there an app for that? J Am Heart Assoc. 2016 Jul 21;5(7) doi: 10.1161/JAHA.116.004000. http://jaha.ahajournals.org/cgi/pmidlookup?view=long&pmid=27444507 .JAHA.116.004000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fang DJ, Hu JC, Wei XF, Shao H, Luo YE. A smart phone healthcare monitoring system for oxygen saturation and heart rate. International Conference on Cyber-Enabled Distributed Computing and Knowledge Discovery; October 13-15, 2014; Shanghai, China. 2014. [DOI] [Google Scholar]
- 64.de Lucena SE, Sampaio D, Mall B, Meyer M, Burkart MA, Keller FV. ECG monitoring using Android mobile phone and Bluetooth. 2015 IEEE International Instrumentation and Measurement Technology Conference (I2MTC) Proceedings; May 11-14, 2015; Pisa, Italy. 2015. [DOI] [Google Scholar]
- 65.Bal U. Non-contact estimation of heart rate and oxygen saturation using ambient light. Biomed Opt Express. 2015 Jan 01;6(1):86–97. doi: 10.1364/BOE.6.000086. http://europepmc.org/abstract/MED/25657877 .86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ahamed MA, Hasan MK, Alam MS. Design and implementation of low cost ECG monitoring system for the patient using smartphone. 2015 International Conference on Electrical & Electronic Engineering (ICEEE); November 4-6, 2015; Rajshahi, Bangladesh. 2015. pp. 261–264. [DOI] [Google Scholar]
- 67.Bobra NP, Wang ZB, Zhang WF, Luo A. A high-quality, low-energy, small-size system-on-chip (soc) solution enabling ECG mobile applications. 39th Annual Conference of the IEEE Industrial Electronics Society; November 10-13, 2013; Vienna, Austria. 2013. pp. 8406–8409. [DOI] [Google Scholar]
- 68.Bolkhovsky JB, Scully CG, Chon KH. Statistical analysis of heart rate and heart rate variability monitoring through the use of smart phone cameras. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:1610–3. doi: 10.1109/EMBC.2012.6346253. [DOI] [PubMed] [Google Scholar]
- 69.Cheatham SW, Kolber MJ, Ernst MP. Concurrent validity of resting pulse-rate measurements: a comparison of 2 smartphone applications, the polar H7 belt monitor, and a pulse oximeter with bluetooth. J Sport Rehabil. 2015 May;24(2):171–8. doi: 10.1123/jsr.2013-0145.2013-0145 [DOI] [PubMed] [Google Scholar]
- 70.Drijkoningen L, Lenaerts F, Van der Auwera J, Leysen K, Nuyens D, Vandervoort P, Grieten L. Validation of a smartphone based photoplethysmographic beat detection algorithm for normal and ectopic complexes. Computing in Cardiology 2014; September 7-10, 2014; Cambridge, MA, USA. 2014. [Google Scholar]
- 71.Flatt AA, Esco MR. Validity of the ithleteTM smart phone application for determining ultra-short-term heart rate variability. J Hum Kinet. 2013 Dec 18;39:85–92. doi: 10.2478/hukin-2013-0071. http://europepmc.org/abstract/MED/24511344 .jhk-39-85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Garabelli P, Stavrakis S, Albert M, Koomson E, Parwani P, Chohan J, Smith L, Albert D, Xie RS, Xie QY, Reynolds D, Po S. Comparison of QT interval readings in normal sinus rhythm between a smartphone heart monitor and a 12-lead ECG for healthy volunteers and inpatients receiving sotalol or dofetilide. J Cardiovasc Electrophysiol. 2016 Jul;27(7):827–32. doi: 10.1111/jce.12976. [DOI] [PubMed] [Google Scholar]
- 73.Gregoski MJ, Mueller M, Vertegel A, Shaporev A, Jackson BB, Frenzel RM, Sprehn SM, Treiber FA. Development and validation of a smartphone heart rate acquisition application for health promotion and wellness telehealth applications. Int J Telemed Appl. 2012;2012:696324. doi: 10.1155/2012/696324. doi: 10.1155/2012/696324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Haberman ZC, Jahn RT, Bose R, Tun H, Shinbane JS, Doshi RN, Chang PM, Saxon LA. Wireless smartphone ECG enables large-scale screening in diverse populations. J Cardiovasc Electrophysiol. 2015 May;26(5):520–6. doi: 10.1111/jce.12634. [DOI] [PubMed] [Google Scholar]
- 75.Ho CL, Fu YC, Lin MC, Chan SC, Hwang B, Jan SL. Smartphone applications (apps) for heart rate measurement in children: comparison with electrocardiography monitor. Pediatr Cardiol. 2014 Apr;35(4):726–31. doi: 10.1007/s00246-013-0844-8. [DOI] [PubMed] [Google Scholar]
- 76.Huang RY, Dung LR. Measurement of heart rate variability using off-the-shelf smart phones. Biomed Eng Online. 2016 Jan 29;15:11. doi: 10.1186/s12938-016-0127-8. https://biomedical-engineering-online.biomedcentral.com/articles/10.1186/s12938-016-0127-8 .10.1186/s12938-016-0127-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kanva AK, Sharma CJ, Deb S. Determination of spo(2) and heart-rate using smart-phone camera. Proceedings of The 2014 International Conference on Control, Instrumentation, Energy and Communication (CIEC); January 31-February 2, 2014; Calcutta, India. 2014. pp. 237–241. [DOI] [Google Scholar]
- 78.Koenig N, Seeck A, Eckstein J, Mainka A, Huebner T, Voss A, Weber S. Validation of a new heart rate measurement algorithm for fingertip recording of video signals with smartphones. Telemed J E Health. 2016 Aug;22(8):631–6. doi: 10.1089/tmj.2015.0212. [DOI] [PubMed] [Google Scholar]
- 79.Lagido RB, Lobo J, Leite S, Sousa C, Ferreira L, Silva-Cardoso J. Using the smartphone camera to monitor heart rate and rhythm in heart failure patients. IEEE-EMBS International Conference on Biomedical and Health Informatics (BHI); June 1-4, 2014; Valencia, Spain. 2014. pp. 556–559. [DOI] [Google Scholar]
- 80.Losa-Iglesias ME, Becerro-de-Bengoa-Vallejo R, Becerro-de-Bengoa-Losa KR. Reliability and concurrent validity of a peripheral pulse oximeter and health-app system for the quantification of heart rate in healthy adults. Health Informatics J. 2016;22(2):151–9. doi: 10.1177/1460458214540909.1460458214540909 [DOI] [PubMed] [Google Scholar]
- 81.Mateev H, Simova I, Katova T, Dimitrov N. Clinical evaluation of a mobile heart rhythm telemonitoring system. ISRN Cardiol. 2012;2012:192670. doi: 10.5402/2012/192670. doi: 10.5402/2012/192670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Matsumura K, Yamakoshi T. iPhysioMeter: a new approach for measuring heart rate and normalized pulse volume using only a smartphone. Behav Res Methods. 2013 Dec;45(4):1272–8. doi: 10.3758/s13428-012-0312-z. [DOI] [PubMed] [Google Scholar]
- 83.McManus DD, Chong JW, Soni A, Saczynski JS, Esa N, Napolitano C, Darling CE, Boyer E, Rosen RK, Floyd KC, Chon KH. Pulse-smart: Pulse-based arrhythmia discrimination using a novel smartphone application. J Cardiovasc Electrophysiol. 2016 Jan;27(1):51–7. doi: 10.1111/jce.12842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.McManus DD, Lee J, Maitas O, Esa N, Pidikiti R, Carlucci A, Harrington J, Mick E, Chon KH. A novel application for the detection of an irregular pulse using an iPhone 4S in patients with atrial fibrillation. Heart Rhythm. 2013 Mar;10(3):315–9. doi: 10.1016/j.hrthm.2012.12.001. http://europepmc.org/abstract/MED/23220686 .S1547-5271(12)01435-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nam Y, Kong Y, Reyes B, Reljin N, Chon KH. Monitoring of heart and breathing rates using dual cameras on a smartphone. PLoS One. 2016;11(3):e0151013. doi: 10.1371/journal.pone.0151013. http://dx.plos.org/10.1371/journal.pone.0151013 .PONE-D-15-39290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Papon MTI, Ahmad I, Saquib N, Rahman A. Non-invasive heart rate measuring smartphone applications using on-board cameras: a short survey. 2015 International Conference on Networking Systems and Security (NSysS); January 5-7, 2015; Dhaka, Bangladesh. 2015. [DOI] [Google Scholar]
- 87.Pelegris P, Banitsas K, Orbach T, Marias K. A novel method to detect heart beat rate using a mobile phone. Conf Proc IEEE Eng Med Biol Soc. 2010;2010:5488–91. doi: 10.1109/IEMBS.2010.5626580. [DOI] [PubMed] [Google Scholar]
- 88.Po LM, Xu XY, Feng LT, Li YM, Cheung KW, Cheung CH. Frame adaptive ROI for photoplethysmography signal extraction from fingertip video captured by smartphone. 2015 IEEE International Symposium on Circuits and Systems (ISCAS); May 24-27, 2015; Lisbon, Portugal. 2015. pp. 1634–1637. [DOI] [Google Scholar]
- 89.Scully CG, Lee J, Meyer J, Gorbach AM, Granquist-Fraser D, Mendelson Y, Chon KH. Physiological parameter monitoring from optical recordings with a mobile phone. IEEE Trans Biomed Eng. 2012 Feb;59(2):303–6. doi: 10.1109/TBME.2011.2163157. http://europepmc.org/abstract/MED/21803676 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wackel P, Beerman L, West L, Arora G. Tachycardia detection using smartphone applications in pediatric patients. J Pediatr. 2014 May;164(5):1133–5. doi: 10.1016/j.jpeds.2014.01.047.S0022-3476(14)00075-4 [DOI] [PubMed] [Google Scholar]
- 91.Kurylyak Y, Lamonaca F, Grimaldi D. Smartphone-based photoplethysmogram measurement. In: Duro RJ, López-Peña F, editors. Digital Image, Signal and Data Processing for Measurement Systems. Denmark: River Publishers; 2012. pp. 135–164. [Google Scholar]
- 92.Terbizan DJ, Dolezal BA, Albano C. Validity of seven commercially available heart rate monitors. Meas Phys Educ Exerc Sci. 2002 Dec;6(4):243–247. doi: 10.1207/S15327841MPEE0604_3. [DOI] [Google Scholar]
- 93.Boulos MN, Wheeler S, Tavares C, Jones R. How smartphones are changing the face of mobile and participatory healthcare: an overview, with example from eCAALYX. Biomed Eng Online. 2011;10:24. doi: 10.1186/1475-925X-10-24. http://www.biomedcentral.com/1475-925X/10/24 .1475-925X-10-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Parak J, Uuskoski M, Machek J, Korhonen I. Estimating heart rate, energy expenditure, and physical performance with a wrist photoplethysmographic device during running. JMIR Mhealth Uhealth. 2017 Jul 25;5(7):e97. doi: 10.2196/mhealth.7437. http://mhealth.jmir.org/2017/7/e97/ v5i7e97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fallow BA, Tarumi T, Tanaka H. Influence of skin type and wavelength on light wave reflectance. J Clin Monit Comput. 2013 Jun;27(3):313–7. doi: 10.1007/s10877-013-9436-7. [DOI] [PubMed] [Google Scholar]
- 96.van Stralen KJ, Jager KJ, Zoccali C, Dekker FW. Agreement between methods. Kidney Int. 2008 Nov;74(9):1116–20. doi: 10.1038/ki.2008.306. https://linkinghub.elsevier.com/retrieve/pii/S0085-2538(15)53488-1 .S0085-2538(15)53488-1 [DOI] [PubMed] [Google Scholar]
- 97.Zaki R, Bulgiba A, Ismail R, Ismail NA. Statistical methods used to test for agreement of medical instruments measuring continuous variables in method comparison studies: a systematic review. PLoS One. 2012;7(5):e37908. doi: 10.1371/journal.pone.0037908. http://dx.plos.org/10.1371/journal.pone.0037908 .PONE-D-12-05103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–10.S0140-6736(86)90837-8 [PubMed] [Google Scholar]