Abstract
Introduction
Wearable accelerometers can be used to evaluate waking and sleeping movements. Although a correlation between accelerometer data captured at the wrist and waist has been reported, it has not been evaluated in patients with low back pain. Therefore, this study aimed to evaluate correlations between movement measured at the wrist and waist, using wearable accelerometers, in patients with low back pain.
Methods
Twenty patients with chronic low back pain and 20 healthy volunteers were enrolled. Two identical accelerometers were simultaneously worn by each participant, one on the nondominant wrist and the other at the waist, for 1 week. We compared the mean number of active movements and mean total amount of movement between the wrist and the waist to evaluate daytime and sleep activities. During sleep, we also evaluated sleep efficiency and time awake after sleep onset.
Results
In daytime activity, the mean number of active movements and mean total amount of movement was greater for the wrist than for the waist, and the amount of waist movements relative to wrist movements was significantly lower in patients with low back pain than in healthy volunteers (p < 0.05). Despite these differences, the mean number of active movements and mean total amount of movement at the wrist and waist were strongly correlated in both groups. During sleep, although there was no difference in either measured sleep efficiency at the wrist or waist or time awake after sleep onset, measurements were strongly correlated in both groups.
Conclusions
A strong correlation between movement data at the wrist and waist during both daytime activities and sleep was identified in patients with low back pain. Therefore, a wearable accelerometer worn on the wrist can reliably measure the movement of patients with low back pain, simplifying data capture for clinical and research purposes and improving patient comfort.
Keywords: wearable accelerometers, low back pain, validation study, amount of movements, sleep efficiency, physical activity, waist movement, wrist movement
Introduction
Recently, the use of wearable sensors to capture an individual's movements and physical activity has attracted attention in health outcome measurements1). Among them, accelerometers are often used in the objective assessment of physical activity patterns in interventional, clinical, and epidemiological studies2). In early studies, the accelerometer was mainly worn at the waist and hip joints, close to the center of gravity3). To address issues such as deterioration in wearing compliance and malfunction during sleeping, in recent years, wristwatch-type accelerometers that are easy to wear, comfortable, and have high wearing compliance even for long periods are being used for research in various applications4,5). Wristwatch-type wearable accelerometers, used to objectively evaluate patients with low back pain (LBP), are expected to measure the amount of activity. It evaluates the change in the amount of activity caused by pain, but optimal placement of accelerometers for reliable data capture remains an issue of debate6,7). Some studies reported a correlation between accelerometer data captured at the wrist and other parts in healthy participants8-10). However, it is unknown whether the measured value of the painful waist, which is considered to indicate the amount of activity to be evaluated, correlates with the measured value of the painless wrist.
Therefore, the current study aimed to evaluate the difference in movements measured at the wrist and waist between healthy volunteers and patients with LBP. Another objective was to evaluate the difference and correlation between movements measured at the wrist and waist of patients with LBP and determine whether wristwatch-type wearable terminals can accurately identify the amount of activity even in patients with LBP.
Materials and Methods
Participants and procedures
The study was approved by the ethics committee of our institution. All participants were informed of the purpose of the study and provided written consent. The study participants were divided into two groups based on the presence of LBP, which was defined as pain in the back at the level of the waist: the LBP group, which included those with chronic LBP with an average daily pain intensity >5/10 on a visual analog scale (VAS) (n = 20), and the control group, which included healthy volunteers without LBP (n = 20). Patients with neurological deficits were excluded from the LBP group, and patients on sleep-inducing drugs were excluded from both groups.
Physical activity measures
The objective physical activity of participants was evaluated using the Micro Motion Logger actigraph (Ambulatory Monitoring Inc., Ardsley, NY, USA), a waterproof, omnidirectional accelerometer (size, 2.5 × 0.9 cm; weight, 14 g). Acceleration is transduced by a piezoelectric element with a sensitivity of 0.01 G/min, and these voltages are recorded and averaged in 1-min epochs. Two identical actigraphs were simultaneously worn by each participant, one on the nondominant wrist and the other at the waist (on a waist band), for 1 week. Data could thus be evaluated for sleeping and waking activities. Data were collected and analyzed using the dedicated Action-W software (version 2.4.15) and the University of California, San Diego scoring algorithm11).
Outcome measures
Outcome measures included items reported in previous studies to allow comparisons4,11-13). The zero-crossing mode (ZCM) indicates the number of movements in a 1-min epoch, and the proportional-integrating mode (PIM) indicates the total amount of movement in a 1-min epoch. For the ZCM, the signal voltage from the accelerometer is compared to the reference voltage, with each zero-crossing generating an activity count (range, 0-255). The PIM provides a high-resolution measurement (range, 0-65,000) of the area under the rectified analog signal, designed to quantify more sedentary levels of motion. We compared the mean active count (MAC) in ZCM and PIM between the wrist and the waist to evaluate daytime activity. During sleep, we again evaluated the MAC of the ZCM and PIM as well as the sleep efficiency (SE) and wake after sleep onset (WASO).
Statistical analyses
Differences in the MAC of the ZCM and PIM for daytime activities captured by the wrist and waist accelerometers were evaluated using Mann-Whitney U test, and the correlation between the two sets of data were evaluated using the nonparametric Spearman's rho (ρ) correlation coefficient in both the LBP and control groups. Additionally, the MAC waist-to-wrist ratio of the ZCM and PIM in the LBP group was compared to that of the control group using the Mann-Whitney U test. Similarly, to analyze sleep data, differences in the MAC of the ZCM and PIM during sleep and the SE and WASO were evaluated using Mann-Whitney U test, and the correlation between the two sets of data were evaluated using the nonparametric Spearman's rho (ρ) correlation coefficient in both the LBP and control groups. Statistical significance was set at p < 0.05. All statistical analyses were performed using the JMPⓇ 12 software (SAS Institute, Cary, NC, USA). All data are reported as the mean ± standard deviation, unless otherwise indicated.
Results
Patient demographics
Our study group included 20 patients (12 men and eight women) with LBP, with a mean age of 66.3 ± 11.3 years (range, 37-88 years) and 20 healthy volunteers (10 men and 10 women), with a mean age of 63.0 ± 24.3 (range, 27-94 years). There was no significant difference in age between the two groups. LBP diagnoses included lumbar spondylosis, lumbar spondylolisthesis, lumbar degenerative disk disease, and degenerative lumbar scoliosis. The average VAS score of LBP was 8.1 ± 1.8 (range, 5-10). The relevant demographics of our patient group are summarized in Table 1.
Table 1.
Demographic Data.
| Patients with low back pain | Healthy volunteer | p value | |
|---|---|---|---|
| No. of patients | 20 | 20 | |
| Age, mean (range), yr | 66.3±11.3 (37−88) | 63.0±24.3 (27−94) | 0.44 |
| Gender (Male/Female) | 12/8 | 10/10 | |
| Visual analog scale (low back pain) | 8.1±1.8 | ||
| Diagnosis | |||
| Lumbar spondylosis | 9 (45%) | ||
| Lumbar spondylolisthesis | 7 (35%) | ||
| Lumbar degenerative disc disease | 2 (10%) | ||
| Degenerative lumbar scoliosis | 2 (10%) |
Daytime analysis
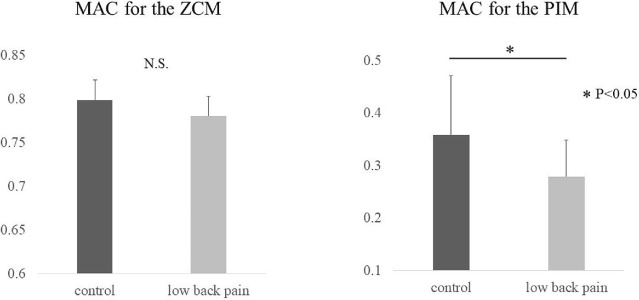
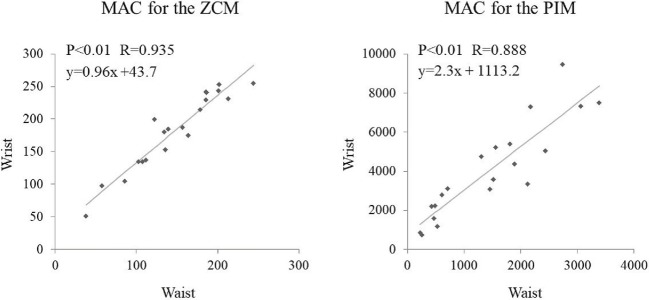
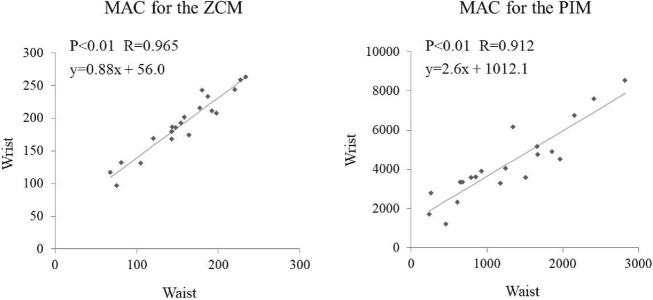
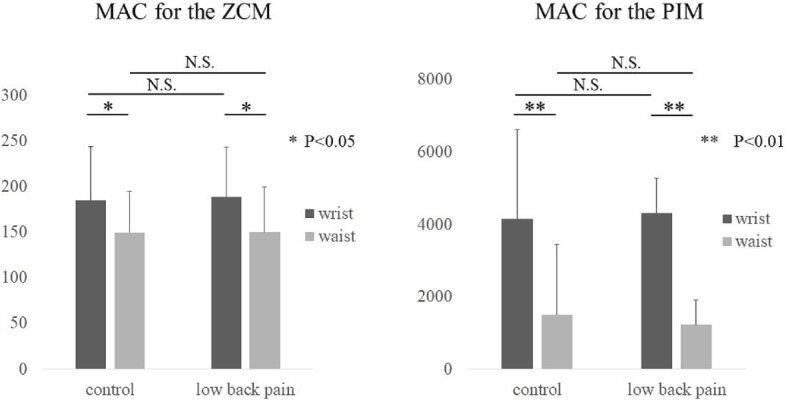
During daytime activity, the MAC of the ZCM was greater at the wrist (184.7 ± 59.1) than at the waist (149.5 ± 54.6) in the control group. This was similar in the LBP group, with a greater MAC of the ZCM at the wrist (188.5 ± 45.5) than at the waist (149.8 ± 49.6; p < 0.05). Likewise, the MAC of the PIM was greater at the wrist (4146.2 ± 2474.4) than at the waist (1495.4 ± 973.0) in the control group and greater at the wrist (4304.7 ± 1959.0) than at the waist (1222.5 ± 686.1) in the LBP group (p < 0.01; Fig. 1). There was no significant difference in the MAC of the ZCM and PIM between the two groups. Regarding the MAC ratio of the ZCM of the waist to the wrist, there was no significant difference in the LBP group (0.78 ± 0.02) compared with the control group (0.80 ± 0.02). Meanwhile, the MAC ratio of the PIM was significantly lower in the LBP group (0.28 ± 0.07) than in the control group (0.36 ± 0.11; p < 0.05; Fig. 2), i.e., the magnitude of waist movement relative to the wrist in the LBP group was less than that of the control group. Despite these differences in magnitude, the ZCM and PIM at the wrist and waist were strongly correlated in both groups (r = 0.935 and r = 0.888 for the ZCM and PIM in the control group; r = 0.965 and r = 0.912 in the LBP group, respectively; Fig. 3, 4).
Figure 1.
The number of movements in 1-min (ZCM) and total movement (PIM) were significantly greater at the wrist in both the control and low back pain groups during the day. MAC, mean active count; ZCM, zero-crossing mode; PIM, proportional-integrating mode
Figure 2.
The ratio of number of movements in 1-min (ZCM) and total movement (PIM) of the waist to the wrist was significantly lower in the low back pain group for PIM. MAC, mean active count; ZCM, zero-crossing mode; PIM, proportional-integrating mode
Figure 3.
There was a strong correlation between the number of movements in 1-min (ZCM) and total movement (PIM) measured at the waist and wrist for each control during the daytime. MAC, mean active count; ZCM, zero-crossing mode; PIM, proportional-integrating mode
Figure 4.
There was a strong correlation between the number of movements in 1-min (ZCM) and total movement (PIM) measured at the waist and wrist for each low back pain patient during the daytime. MAC, mean active count; ZCM, zero-crossing mode; PIM, proportional-integrating mode
Sleep time analysis
During sleep, the control group showed no difference in the MAC of the ZCM of the wrist (19.0 ± 7.5) and waist (14.3 ± 6.4), while the MAC of the PIM was greater at the wrist (319.4 ± 149.9) than at the waist (71.2 ± 34.7; p < 0.01). There was no difference in either the measured SE at the wrist (90.7 ± 5.2) or waist (93.2 ± 5.4) or WASO (35.2 ± 17.2 and 27.9 ± 18.1 at the wrist and waist, respectively). Although magnitudes were different between the wrist and waist, measurements were strongly correlated (Table 2; MAC for the ZCM, r = 0.681; MAC for the PIM, r = 0.762; SE, r = 0.541; and WASO, r = 0.567) in the control group. Similarly, in the LBP group, there was no difference in the MAC of the ZCM of the wrist (16.8 ± 5.9) and waist (14.5 ± 6.8), while the MAC of the PIM was greater at the wrist (273.2 ± 149.9) than at the waist (62.2 ± 32.0; p < 0.01). There was no difference in the measured SE at the wrist (91.7 ± 4.7), waist (92.6 ± 5.6), or WASO (34.5 ± 18.3 and 31.8 ± 24.4 at the wrist and waist, respectively). Measurements were strongly correlated (Table 3; MAC for the ZCM, r = 0.769; MAC for the PIM, r = 0.706; SE, r = 0.813; and WASO, r = 0.569) in the LBP group.
Table 2.
Sleep Analysis of Healthy Volunteers.
| Wrist | Waist | P value | Correlation coefficient | |
|---|---|---|---|---|
| MAC for the ZCM | 19.0±7.5 | 14.3±6.4 | 0.097 | 0.681 |
| MAC for the PIM | 319.4±149.9 | 71.2±34.7 | P<0.01 | 0.762 |
| Sleep efficiency | 90.7±5.2 | 93.2±5.4 | 0.141 | 0.541 |
| WASO | 35.2±17.2 | 27.9±18.1 | 0.150 | 0.567 |
MAC, mean active count; ZCM, zero-crossing mode; PIM, proportional-integrating mode; WASO, wake after sleep onset
Table 3.
Sleep Analysis of the Patients with Low Back Pain.
| Wrist | Waist | P value | Correlation coefficient | |
|---|---|---|---|---|
| MAC for the ZCM | 16.8±5.9 | 14.5±6.8 | 0.241 | 0.769 |
| MAC for the PIM | 273.2±149.9 | 62.2±32.0 | P<0.01 | 0.706 |
| Sleep efficiency | 91.7±4.7 | 92.6±5.6 | 0.296 | 0.813 |
| WASO | 34.5±18.3 | 31.8±24.4 | 0.358 | 0.569 |
MAC, mean active count; ZCM, zero-crossing mode; PIM, proportional-integrating mode; WASO, wake after sleep onset
Discussion
In the present study, we evaluated the relationship between movement measures recorded using a wearable accelerometer at the wrist and waist in healthy volunteers and patients with LBP. During waking hours, both ZCM and PIM were significantly greater in magnitude at the wrist than waist, although these two measurements were strongly correlated. Furthermore, the MAC ratio of the PIM of the waist to the wrist and the number of waist movements relative to wrist movements were both significantly lower in the LBP group. By contrast, during sleep, there was no difference between the ZCM and the PIM, with a strong correlation between wrist and waist measurements for all measured variables. This was similar for both groups.
Previous studies have reported an association between activity level and pain. Liszka-Hackzell and Martin14) identified a significant correlation between the intensity of acute LBP and activity level, whereas Wilson and Palermo15) reported a significantly lower activity level among patients with chronic pain compared with healthy controls. In our study, the amount of activity measured at the waist was lower than that measured at the wrist, and waist movements relative to wrist movements were significantly lower in the LBP group, which might be indicative of a possible decrease in trunk movement among patients with LBP; this might, in part, result from pain-related avoidance of general physical activity and muscular overactivity16,17).
In Table 4, we summarize findings from previous studies that have compared accelerometer-based measurements of movement recorded from different locations of the body. Rowlands et al.18) reported a correlation coefficient of 0.83 between measures obtained at the wrist and hip. Among healthy participants, Kamada et al.19) and Dieu et al.8) reported a correlation coefficient of 0.73 between measurements obtained at the wrists and lower limbs, with a coefficient of 0.88 between the wrists and the trunk. In our study, we reported a correlation coefficient of 0.96 for the ZCM measured at the wrist and waist, with a correlation coefficient of 0.91 of the PIM (Table 4). Therefore, regardless of the presence or absence of pain, measurements of movement at the wrist and waist do correlate with one another, both in magnitude and amount. Based on these findings, we speculate that movement, overall, is lower among patients with LBP. The MAC of the ZCM and PIM were correlated during sleep, albeit to a lower extent than during daytime hours. Among patients with Parkinson disease with pain, movement during sleep was reported to be decreased20). Therefore, it seems likely that trunk movements (measured at the waist) are decreased among patients with LBP, with the pain having little effect on upper limb movements.
Table 4.
Correlations of Mean Activity according to the Measurement Location.
| n | Subjects | Device | Wearing site | Correlation coefficient | |
|---|---|---|---|---|---|
| Kamada, M | 94 | Healthy volunteer | GT3X | wrist-lower limbs | 0.73 |
| Rowlands, A.V | 58 | Children | GT3X, GENEActiv | wrist-hip | 0.83 |
| Dieu | 40 | Healthy volunteer | GT3X | waist-wrist | 0.88 |
| Current study | 20 | Low back pain | Micro motion logger | waist-wrist | 0.91 |
In our data set, the measurement error for daytime movement measurement using the actigraph system was low for both the wrist and waist, despite our participants having LBP. Therefore, it appears that using wristwatch-type wearable accelerometers to measure movement and evaluate sleep, a method widely used in other patient populations, is also effective for patients with LBP. Measuring activities of daily living with wearable accelerometers may be a novel and objective method for evaluating LBP treatment in the future, as the measurements from this type of accelerometer appear to have high clinical value.
The current study has some limitations. First, several LBP diagnoses were included, which might have increased the variability of our results. Second, the number of participants was relatively small. Future studies with larger sample sizes are necessary.
Conclusion
We identified a strong correlation between movement data, measured with the actigraph system at the wrist and waist, during both daytime activities and sleep in patients with LBP. This is the first known study to measure the correlation between wrist and waist movement data in this patient population, and our findings correspond to those of previous studies. Thus, based on our results, a wearable accelerometer worn on the wrist can sufficiently and reliably measure the amount of movement of patients with LBP, simplifying data capture for clinical and research purposes and improving patient quality of life.
Disclaimer: Sumihisa Orita is one of the Editors of Spine Surgery and Related Research and on the journal's Editorial Committee. He was not involved in the editorial evaluation or decision to accept this article for publication at all.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: The present study was supported by the project research funded by the Japanese Orthopaedic Association (#2016-1).
Author Contributions: MI, SuO, MiS, KI, KF, YS, HirK, KA, HidK, MN, TU, ST, MasasS, MasahS, KE, and SeO, designed the study and analyzed and/or interpreted the data. MI wrote the article and SuO, MiS, KI, YE, YA and SeO provided critical comments on the draft of the manuscript. All authors read and approved the final version of the manuscript.
Acknowledgement
We gratefully acknowledge the work of past and present members of our laboratory.
References
- 1.Hallal PC, Anderson LB, Bull FC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247-57. [DOI] [PubMed] [Google Scholar]
- 2.Westerterp KR. Assessment of physical activity: a critical appraisal. Eur J Appl Physiol. 2009;105(6):823-8. [DOI] [PubMed] [Google Scholar]
- 3.Westerterp KR. Physical activity assessment with accelerometers. Int J Obes. 1999;23(S3):S45-9. [DOI] [PubMed] [Google Scholar]
- 4.Hjorth MF, Chaput JP, Damsgaard CT, et al. Measure of sleep and physical activity by a single accelerometer: can a waist-worn actigraph adequately measure sleep in children? Sleep Biol Rhythms. 2012;10(4):328-35. [Google Scholar]
- 5.Lloret SP, Rossi M, Cardinali DP, et al. Actigraphic evaluation of motor fluctuations in patients with Parkinson's disease. Int J Neurosci. 2010;120(2):137-43. [DOI] [PubMed] [Google Scholar]
- 6.Zhang, JH, MacFarlane DJ, Sobko T. Feasibility of a chest-worn accelerometer for physical activity measurement. J Sci Med Sport. 2016;19(12):1015-9. [DOI] [PubMed] [Google Scholar]
- 7.Tudor-Locke C, Barreira TV, Schuna JM. Comparison of step outputs for waist and wrist accelerometer attachment sites. Med Sci Sports Exerc. 2015;47(4):839-42. [DOI] [PubMed] [Google Scholar]
- 8.Dieu O, Mikulovic J, Fardy PS, et al. Physical activity using wrist-worn accelerometers: comparison of dominant and non-dominant wrist. Clin Physiol Funct Imaging. 2017;37(5):525-9. [DOI] [PubMed] [Google Scholar]
- 9.Rosenberger ME, Haskell WL, Albinali F, et al. Estimating activity and sedentary behavior from an accelerometer on the hip or wrist. Med Sci Sports Exerc. 2013;45(5):964-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gironda RJ, Lloyd J, Clark ME, et al. Preliminary evaluation of reliability and criterion validity of Actiwatch-Score. J Rehabil Res Dev. 2007;44(2):223-30. [DOI] [PubMed] [Google Scholar]
- 11.Girardin JL, Kripke DF, Cole RJ, et al. Sleep detection with an accelerometer actigraph: comparisons with polysomnography. Physiol Behav. 2001;72(1-2):21-8. [DOI] [PubMed] [Google Scholar]
- 12.Moran DS, Heled Y, Gonzalez RR. Metabolic rate monitoring and energy expenditure prediction using a novel actigraphy method. Med Sci Monit. 2004;10(11):MT117-20. [PubMed] [Google Scholar]
- 13.Blackwell T, Redline S, Ancoli-Israel S, et al. Comparison of sleep parameters from actigraphy and polysomnography in older women: the SOF study. Sleep. 2008;31(2):283-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liszka-Hackzell JJ, Martin DP. An analysis of the relationship between activity and pain in chronic and acute low back pain. Anesth Analg. 2004;99(2):477-81. [DOI] [PubMed] [Google Scholar]
- 15.Wilson AC, Palermo TM. Physical activity and function in adolescents with chronic pain: a controlled study using actigraphy. J Pain. 2012;13(2):121-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317-32. [DOI] [PubMed] [Google Scholar]
- 17.Pedler A, Kamper SJ, Maujean A, et al. Investigating the fear avoidance model in people with whiplash: The association between fear of movement and in vivo activity. Clin J Pain. 2017;34(2):130-7. [DOI] [PubMed] [Google Scholar]
- 18.Rowlands A, Rennie K, Koraski R, et al. Children's physical activity assessed with wrist- and hip-worn accelerometers. Med Sci Sports Exerc. 2014;46:2308-16. [DOI] [PubMed] [Google Scholar]
- 19.Kamada M, Shiroma EJ, Harris B, et al. Comparison of physical activity assessed using hip- and wrist-worn accelerometers. Gait Posture. 2016;44:23-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stack EL, Ashburn AM. Impaired bed mobility and disordered sleep in Parkinson's disease. Mov Disord. 2006;21(9):1340-2. [DOI] [PubMed] [Google Scholar]