Abstract
Introduction
The prevalence of patients with osteoporosis continues to increase in aging societies, including Japan. The first choice for managing osteoporotic vertebral compression fracture (OVF) is conservative treatment. Failure in conservative treatment for OVF may lead to non-union or vertebral collapse, resulting in neurological deficit and subsequently requiring surgical intervention. This multicenter nationwide study in Japan was conducted to comprehensively understand the outcomes of surgical treatments for OVF non-union.
Methods
This multicenter, retrospective study included 403 patients (89 males, 314 females, mean age 73.8 ± 7.8 years, mean follow-up 3.9 ± 1.7 years) with neurological deficit due to vertebral collapse or non-union after OVF at T10-L5 who underwent fusion surgery with a minimum 1-year follow-up. Radiological and clinical outcomes at baseline and at the final follow-up (FU) were evaluated.
Results
OVF was present at a thoracolumbar junction such as T12 (124 patients) and L1 (117 patients). A majority of OVF occurred after a minor trauma, such as falling down (55.3%) or lifting objects (8.4%). Short segment fusion, including affected vertebra, was conducted (mean 4.0 ± 2.0 vertebrae) with 256.8 minutes of surgery and 676.1 g of blood loss. A posterior approach was employed in 86.6% of the patients, followed by a combined anterior and posterior (8.7%), and an anterior (4.7%) approach. Perioperative complications and implant failures were observed in 18.1% and 41.2%, respectively. VAS scores of low back pain (74.7 to 30.8 mm) and leg pain (56.8 to 20.7 mm) improved significantly at FU. Preoperatively, 52.6% of the patients were unable to walk and the rate of non-ambulatory patients decreased to 7.5% at FU.
Conclusions
This study demonstrated that substantial improvement in activity of daily living (ADL) was achieved by fusion surgery. Although there was a considerable rate of complications, fusion surgery is beneficial for elderly OVF patients with non-union.
Keywords: Vertebral compression fracture, Osteoporosis, Multicenter study
Introduction
The prevalence of patients with osteoporosis continues to increase as societies skew toward an older demographic, which is particularly acute in aging societies including Japan. Osteoporosis prevalence has been estimated to be as high as 38% in women and 4% in men aged 50 years and above1). According to the 2015 Guidelines for Prevention and Treatment of Osteoporosis published by the Japan Osteoporosis Society, 12.8 million patients are estimated to have osteoporosis in Japan which accounts for more than 10% of the population.
These patients are at risk of developing vertebral compression fracture after a minor trauma. An estimated 1.4 million new osteoporotic fractures at the vertebrae occurred in the year 20002). Most patients can be managed conservatively, such as through bed rest, medication, or a spinal brace. Lee et al. reported a 95% success rate with conservative treatment in patients who showed favorable results after the initial three weeks of treatment3). However, failure during appropriate conservative treatment of osteoporotic compression fracture may result in a severe deterioration of activity of daily living (ADL), with neurological deficits or progression of kyphosis, requiring surgical intervention. Since the first surgical case for paraplegia due to osteoporotic vertebral compression fracture (OVF) was reported by Kempinsky et al.4), many studies have reported various surgical techniques and outcomes for this condition, such as anterior decompression and fusion, posterolateral fusion, posterior spinal shortening, posterior fixation with vertebroplasty, and combined anterior and posterior fixation5-8). Many of these studies are case series at a single institution, or cohort studies from a few institutions; studies with a large sample size are limited. There is one systematic review that included 596 patients from 29 publications comparing three different surgical methods: anterior decompression and reconstruction, posterior surgery, and posteroanterior surgery9). However, inclusion criteria may vary among the studies, so it is difficult to perform statistical analysis comparing each surgical procedure, or on various radiological parameters, as the data from each individual patient was not available in this systematic review.
In this study, we performed a nationwide, multicenter, retrospective study of patients that underwent fusion surgery for osteoporotic vertebral collapse to comprehensively understand and gain an overview of patient demographics, surgical methods, and outcomes.
Materials and Methods
Study design
This study was a retrospective, multicenter study conducted through the Japan Association of Spine Surgeons with Ambition (JASA), which consists of 52 university hospitals all over Japan. Inclusion criteria were patients who had neurological deficits due to vertebral collapse or non-union after OVF at T10-L5 and underwent fusion surgery with a minimum 1-year follow-up. Patients with back pain due to kyphotic deformity without any neurological deficit or patients who underwent BKP alone were excluded from this study. A datasheet was sent to each site, and spine surgeons were asked to fill in the datasheet to include the information noted below. A total 403 patients (89 males, 314 females, mean age 73.8 ± 7.8 years, mean follow-up 3.9 ± 1.7 years) from 28 university hospitals and affiliated hospitals were included in this study. Most of the patients (394 patients) were followed longer than two years.
Information included in the datasheet
The datasheet included information about patient background such as age, gender, comorbidities, type of traumatic event, medication for osteoporosis, existence and cause of secondary osteoporosis, and amount of steroid intake. Information about surgery, such as method of fixation, upper (UIV) and lower instrumented vertebra (LIV), estimated blood loss, and surgical time were collected. Information about perioperative complications within six weeks after the surgery and need for revision surgery were also collected. Radiological findings, such as mechanical failure, newly developed fracture after the surgery, and pseudoarthrosis were evaluated. Mechanical failures were defined as a failure related to the implant within the fused vertebra, such as loosening or back out of a pedicle screw, hook dislodgement, rod fracture, dislodgement or subsidence cage, and fracture at UIV or LIV. The local kyphosis angle (LKA) was defined as the angle between the upper endplate of a proximal adjacent vertebra and lower endplate of a distal adjacent vertebra of an affected vertebra and was measured preoperatively, early after the surgery, and at the final follow-up. Pseudoarthrosis was defined as one of following at the final follow-up: instability with flexion/extension radiographs, presence of clear zone around the bone graft, or rod fracture.
Clinical outcomes were evaluated preoperatively and at the final follow-up with Visual Analogue Scale (VAS) score of low back pain and leg pain, and Japanese Orthopaedic Association (JOA) score. For JOA score, only scores for subjective symptoms (9 points), clinical signs (6 points), and urinary bladder function (−6 points) were included; a full score was 15 points. For activities of daily living, patients were classified into the original six categories focused on gait ability, such as: (1) bedridden, (2) wheelchair, (3) walking while holding on to wall or creep, (4) walking with walker, bilateral canes, or 1 cane with support from others, (5) walking with unilateral cane without any support, and (6) walking freely.
Statistical analysis
Paired Student's t-test was used to compare the LKA, JOA score, and VAS scores between preoperative and at the final follow-up. All data were presented as mean ± standard deviation. Statistical analyses were performed using SPSS ver. 21 (IBM Inc.). For all statistical analyses, a p value < 0.05 was considered statistically significant.
Results
Patient demographics
Table 1 shows the demographic data for all patients. In a majority of the patients, vertebral fractures were associated with minor trauma such as falling down, lifting objects, or sneezing, and 23.6% of the patients recognized no traumatic event indicating that bone fragility may underlie this injury. Nearly one-third of patients (30.8%) had primary causes that induce osteoporosis, such as steroid intake. A majority of the patients (67.5%) had at least one comorbidity and 6.9% had more than three comorbidities.
Table 1.
Patient Demographic Data.
| Variables | |
|---|---|
| Type of traumatic event | |
| Fall down | 55.3% |
| Lifting of object | 8.4% |
| Other (sneeze, farm work, etc.) | 1.0% |
| No trauma | 23.6% |
| Undetermined | 11.7% |
| Secondary osteoporosis | 30.8% |
| Steroid intake | |
| 0 mg | 87.3% |
| <5 mg | 4.7% |
| 5-10 mg | 6.7% |
| 10-20 mg | 0.7% |
| >20 mg | 0.5% |
| History of smoking | 13.4% |
| Number of comorbidities | |
| none | 32.5% |
| 1 | 38.0% |
| 2 | 22.6% |
| >3 | 6.9% |
Table 2 shows the rate of osteoporosis treatment and type of medication used. Although a majority of the patients in this study were elderly females, the rate of osteoporosis treatment was limited to 40.1% at the time of vertebral fracture (Table 2). This rate significantly increased to 75.3% after surgery. Bisphosphonates were the most frequently used medication before the fracture; however, a marked increase of teriparatide use was observed after surgery.
Table 2.
Medication for Osteoporosis.
| Preoperatively | Postoperatively | |
|---|---|---|
| Number of the patients with medication | 159 (40.1%) | 299 (75.3%) |
| Types of medication used (including duplicates) | ||
| Bisphosphonates | 100 | 147 |
| Vitamin D analogs | 27 | 30 |
| Teriparatide | 23 | 118 |
| SERM | 7 | 6 |
| Vitamin K2 | 4 | 2 |
| Calcium compounds | 2 | 1 |
| Calcitonin | 1 | 2 |
| Denosumab | 0 | 5 |
| Total | 164 | 311 |
Fig. 1 shows the distribution of the primary affected vertebra. A thoracolumbar junction, such as T12 and L1, was the most frequent level of the fracture; however, 18.9% had a fracture at the mid to lower lumbar spine (L3 to L5).
Figure 1.
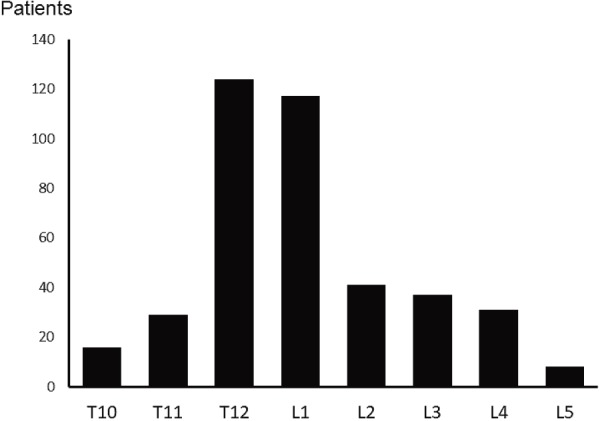
Distribution of primary affected vertebra.
T12 and L1 are the most frequently affected vertebrae.
The degree of osteoporosis was evaluated with dual-energy X-ray absorptiometry (DEXA) in 220 patients (69 patients in lumbar spine and 151 patients in femoral neck). The mean bone mineral density was 0.724 ± 0.14 g/cm2 in the lumbar spine, 0.604 ± 0.17 g/cm2 in the femoral neck, and the mean YAM (young adult mean) value was 71.6 ± 5.9%.
Surgical information and radiological results
Table 3 reveals that a posterior approach is the current mainstream method for the treatment of this pathology followed by a combined anterior and posterior approach and anterior-only approach. Among patients who had a posterior approach, 44.5% had vertebroplasty combined with posterior fusion and 33.5% had 3-column osteotomy. A mean 4.0 ± 2.0 vertebrae were fused with moderate surgical invasion such as 256.8 ± 115.0 minutes of surgery and 676.3 ± 1166.9 g of blood loss. Perioperative complication was observed in 18.1% of the patients, including delirium (23 patients), dural tear (5 patients), deep wound infection (4 patients), superficial infection (4 patients), hematoma (4 patients), pneumonia (3 patients), and deep vein thrombosis (3 patients).
Table 3.
Information Related to Surgery.
| Variables | |
|---|---|
| Surgical approach | |
| Posterior only | 349 (86.6%) |
| Anterior only | 19 (4.7%) |
| Combined anterior and posterior | 35 (8.7%) |
| Surgical time (minutes) | 256.8±115.0 |
| Blood loss (g) | 676.1±1166.9 |
| Number of fused segments | 4.0±2.0 |
| Complication within 6 weeks | 18.1% |
| Mechanical failure | 41.2% |
| Pseudoarthrosis | 6.2%* |
*Among 385 patients who were able to judge the bone union.
Mechanical failure was observed in 41.2% of the patients. Loosening of pedicle screws was the most common mechanical failure (99 patients), followed by back out of pedicle screws (38 patients) and fracture of UIV (23 patients). A majority of the patients accomplished bone union at the final follow-up with a pseudoarthrosis rate of 6.2%.
Fig. 2 shows the change of LKA. Preoperative LKA was 22.0 ± 16.9° and corrected to 5.2 ± 13.1°. LKA at the final follow-up was 12.0 ± 15.2° with a mean correction loss of 6.7 ± 8.8°.
Figure 2.
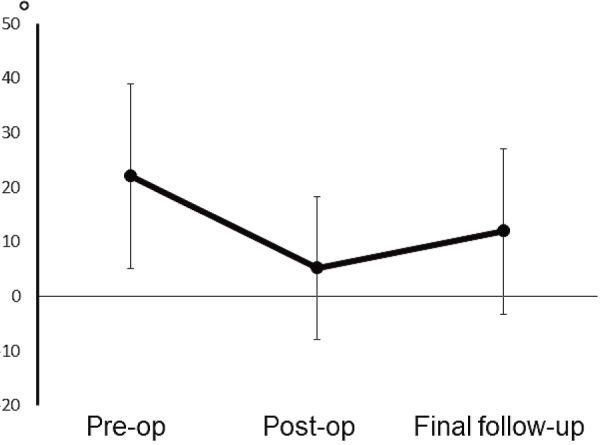
Change of local kyphosis angle.
The local kyphosis angle was defined as the angle between the upper endplate of a proximal adjacent vertebra and the lower endplate of a distal adjacent vertebra of affected vertebra.
Clinical outcomes
Fig. 3 shows that both VAS scores of LBP and leg pain significantly improved after surgery. Also, JOA score was significantly improved (by approximately 5 points) at the final follow-up. Evaluation of ADL revealed that 52.4% of patients were unable to walk before surgery (bedridden or wheelchair), which decreased to 7.5% at the final follow-up (Table 4). More than 65% of patients were able to walk without any support (walking with 1 cane without support or freely) at the final follow-up.
Figure 3.
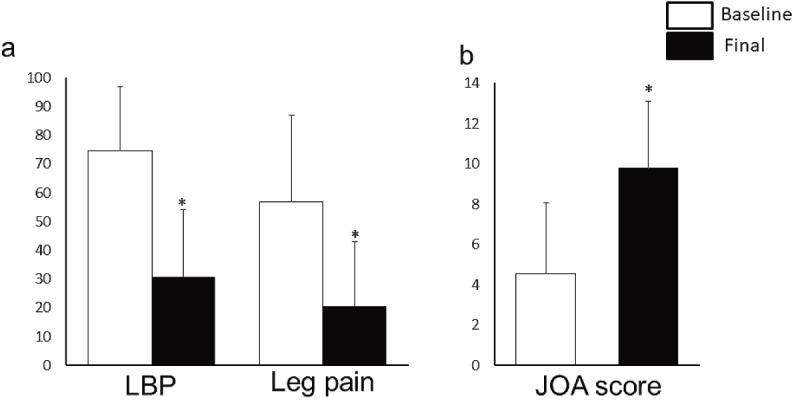
Clinical outcomes.
a. VAS scores of low back pain (LBP) and leg pain.
b. JOA score with a full score being 15 points.
*p<0.05 with Student’s t-test.
Table 4.
ADL Classification.
| Baseline (%) | Follow-up (%) | |
|---|---|---|
| 1. Bedridden | 12.9 | 0.5 |
| 2. Wheelchair | 39.5 | 7.0 |
| 3. Walking while holding on to wall, creeping | 15.1 | 6.3 |
| 4. Walking with walker, 2 canes, 1 cane with support | 14.1 | 19.8 |
| 5. Walking with 1 cane without support | 13.4 | 31.8 |
| 6. Walking freely | 5.0 | 34.6 |
Discussion
The thoracolumbar/lumbar spine is one of the most common sites for fracture due to osteoporosis. An osteoporotic vertebral compression fracture (OVF) may affect activities of daily living. Olenski et al. reported that, among low BMD postmenopausal women, vertebral fracture was shown to be associated with decreased HRQOL score10). Additionally, OVF has been shown to be related to a higher mortality rate at a 10-year follow-up11). Therefore, appropriate management of OVF is important in aging societies where the number of osteoporosis patients will likely continue to increase.
There are many previous studies evaluating various surgical methods for OVF non-union. Kanayama et al. evaluated surgical outcomes after anterior spinal reconstruction with instrumentation in 31 OVF patients with neurological compromise and reported the advantages of this method, such as safety and reliability of decompression, with a success rate of 80%5). Akata et al. investigated the results of posterior spinal fusion without decompression for thoracolumbar OVF with neurological deficits and reported that substantial improvements of back pain and neurological symptoms were obtained8). Matsuyama et al. demonstrated the efficacy of posterior spinal fusion, combined with vertebroplasty using calcium phosphate cement, in five OVF patients7). Saita et al. were the first to report the surgical technique of posterior spinal shortening osteotomy, which was intended to reduce the force that may dislodge implants by correcting the kyphosis6). The efficacy of this method was confirmed in 13 OVF patients with paraparesis in a subsequent study12).
In addition to these case-series of certain surgical methods, there are several comparison studies of several surgical methods. Kashii et al. reviewed 88 OVF patients with neurological deficits who underwent surgery at four facilities with three different methods: anterior decompression and reconstruction, posterior shortening osteotomy, and posterior fusion combined with vertebroplasty13). An equivalent improvement of neurological deficits and ADL function were achieved with every surgical method and posterior fusion combined with vertebroplasty was shown to have the least surgical invasion. Another comparative study was reported by Nakashima et al. who included 93 patients from six hospitals14). They compared patients who underwent combined anterior and posterior surgery and posterior fusion with vertebroplasty and revealed that stability of the fixation was superior in combined anterior and posterior surgery.
A majority of these studies focusing on surgical outcomes for OVF with neurological deficits were reported from Japan, a country with the most advanced aging society in the world. There are several studies from other countries such as China, France or Korea; however, the number of patients in their samples were small and studies with a large number of patients is limited15-17). There is one previous, large-scale, systematic review that included 596 OVF patients with delayed neurological deficit from 29 publications9). In this review, posterior surgery was conducted in 60.6% of patients followed by anterior decompression and reconstruction in 36.6%. Although 21 out of 29 publications were from Japan, the proportion for anterior surgery in this review (36.6%) was largely different from our study (4.7%). One of the reasons for this discrepancy might be due to the difference in period of publication. Many studies used in this review were published in the 1990s to 2000s, whereas our patients had surgery recently. The other discrepancies between this review and our study were the rates of complication and implant failure. These rates were reported to be 12.2% for complication and 15.8% for implant failure, which were lower compared to our study (complication 18.1% and mechanical failure 41.2%). A possible explanation for these differences might be due to definitions for complication and implant failure varies among the studies included in this review which may underestimate these rates.
In this study, we intended to comprehensively understand current trends and outcomes for the surgical treatment of OVF with neurological deficit, and did not aim to compare certain surgical methods or to reveal the risk factors for complications or mechanical failures. Toward this purpose, we designed a multicenter study that included 41 facilities throughout Japan, where the number of OVF patients who require surgical treatment is rapidly expanding. Our study revealed that subjects of the surgical treatment were elderly patients who had OVF with minor or no trauma, which suggests underlying bone fragility in these patients. Short segment posterior fusion at the affected level is the current mainstream approach in surgical treatment with an acceptable surgical invasion of 256.8 minutes of surgery, 676.3 g of blood loss and 18.1% for perioperative complications. Clinical outcomes assessed with JOA score and VAS score significantly improved after surgery, and a majority of the patients were able to walk postoperatively, suggesting that spinal fusion surgery is effective for quality of life improvement even for the elderly patients.
There are several limitations in this study. This was a multicenter retrospective study, and the indication for fusion surgery or choices of surgical procedures were not standardized and were dependent on the surgeons in charge of the treatment at each facility. Secondary, as clinical outcomes or complications were obtained from chart review, the accuracy of the information might be inferior compared to a prospective study.
In conclusion, we comprehensively conducted an overview of the current surgical treatment for OVF with neurological deficit and found the relevance of the spinal fusion surgery. We also elucidated the high rate of mechanical failure. Future studies are required to assess how to prevent such failures related to implants and to improve overall outcomes.
Disclaimer: Sumihisa Orita is one of the Editors of Spine Surgery and Related Research and on the journal's Editorial Committee. He was not involved in the editorial evaluation or decision to accept this article for publication at all.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Author Contributions: Naobumi Hosogane analyzed and wrote the manuscript, and all other authors participated in acquisition or analysis of data, drafting the work. All authors have read, reviewed and approved the article.
References
- 1.Wade SW, Strader C, Fitzpatrick LA, et al. Estimating prevalence of osteoporosis: examples from industrialized countries. Arch Osteoporos. 2014;9(1):182. [DOI] [PubMed] [Google Scholar]
- 2.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726-33. [DOI] [PubMed] [Google Scholar]
- 3.Lee HM, Park SY, Lee SH, et al. Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCFs): conservative treatment versus balloon kyphoplasty. Spine J. 2012;12(11):998-1005. [DOI] [PubMed] [Google Scholar]
- 4.Kempinsky WH, Morgan PP, Boniface WR. Osteoporotic kyphosis with paraplegia. Neurology. 1958;8(3):181-6. [DOI] [PubMed] [Google Scholar]
- 5.Kanayama M, Ishida T, Hashimoto T, et al. Role of major spine surgery using Kaneda anterior instrumentation for osteoporotic vertebral collapse. J Spinal Disord Tech. 2010;23(1):53-6. [DOI] [PubMed] [Google Scholar]
- 6.Saita K, Hoshino Y, Kikkawa I, et al. Posterior spinal shortening for paraplegia after vertebral collapse caused by osteoporosis. Spine (Phila Pa 1976). 2000;25(21):2832-5. [DOI] [PubMed] [Google Scholar]
- 7.Matsuyama Y, Goto M, Yoshihara H, et al. Vertebral reconstruction with biodegradable calcium phosphate cement in the treatment of osteoporotic vertebral compression fracture using instrumentation. J Spinal Disord Tech. 2004;17(4):291-6. [DOI] [PubMed] [Google Scholar]
- 8.Ataka H, Tanno T, Yamazaki M. Posterior instrumented fusion without neural decompression for incomplete neurological deficits following vertebral collapse in the osteoporotic thoracolumbar spine. Eur Spine J. 2009;18(1):69-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sheng X, Ren S. Surgical techniques for osteoporotic vertebral collapse with delayed neurological deficits: a systematic review. Int J Surg. 2016;33:42-8. [DOI] [PubMed] [Google Scholar]
- 10.Oleksik A, Lips P, Dawson A, et al. Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res. 2000;15(7):1384-92. [DOI] [PubMed] [Google Scholar]
- 11.Ikeda Y, Sudo A, Yamada T, et al. Mortality after vertebral fractures in a Japanese population. J Orthop Surg (Hong Kong). 2010;18(2):148-52. [DOI] [PubMed] [Google Scholar]
- 12.Saita K, Hoshino Y, Higashi T, et al. Posterior spinal shortening for paraparesis following vertebral collapse due to osteoporosis. Spinal Cord. 2008;46(1):16-20. [DOI] [PubMed] [Google Scholar]
- 13.Kashii M, Yamazaki R, Yamashita T, et al. Surgical treatment for osteoporotic vertebral collapse with neurological deficits: retrospective comparative study of three procedures--anterior surgery versus posterior spinal shorting osteotomy versus posterior spinal fusion using vertebroplasty. Eur Spine J. 2013;22(7):1633-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakashima H, Imagama S, Yukawa Y, et al. Comparative study of 2 surgical procedures for osteoporotic delayed vertebral collapse: anterior and posterior combined surgery versus posterior spinal fusion with vertebroplasty. Spine (Phila Pa 1976). 2015;40(2):E120-6. [DOI] [PubMed] [Google Scholar]
- 15.Blondel B, Fuentes S, Metellus P, et al. Severe thoracolumbar osteoporotic burst fractures: treatment combining open kyphoplasty and short-segment fixation. Orthop Traumatol Surg Res. 2009;95(5):359-64. [DOI] [PubMed] [Google Scholar]
- 16.Wang F, Wang D, Tan B, et al. Comparative study of modified posterior operation to treat Kummell's disease. Medicine (Baltimore). 2015;94(39):e1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park SJ, Kim HS, Lee SK, et al. Bone cement-augmented percutaneous short segment fixation: an effective treatment for Kummell's disease? J Korean Neurosurg Soc. 2015;58(1):54-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


