Abstract
Individuals with substance use disorders (SUDs) often face discrimination. A recent study found that people in the general population hold significantly more negative views toward persons with drug addiction than those with other mental illnesses (Barry et al. in Psychiatric Services, 65(10), 1269–1272, 2014). It is possible that these negative attitudes stem from the historical view of addiction as a moral shortcoming or lack of willpower. Behavior analysts’ approach to behavior is guided by the underlying philosophy of behaviorism, which proposes that behavior is determined by genetic and environmental factors, as opposed to the free will of an individual. Because behavior analysts view behavior as determined and do not assign responsibility to an individual for his or her behavior, one would hypothesize that behavior analysts would not view individuals with SUDs more negatively than those with other mental disorders. This study surveyed 288 behavior analysts regarding their views on SUDs and mental disorders. Results showed that behavior analysts have significantly more negative attitudes toward people with SUDs than toward people with other mental disorders. Respondents reported a greater desire for social distance and greater acceptability of discrimination for people with SUDs than for people with mental disorders. They also reported less potential for recovery and lower support for policies to improve equity in insurance coverage and were less supportive of using government funding to improve treatment, housing, and job support for people with SUDs.
Keywords: Substance use disorder, Drug addiction, Mental illness, Behavior analyst, Attitudes, Stigma, Discrimination, Behaviorism
Only 13% of people who need treatment for a substance use disorder (SUD) receive it (SAMHSA, 2018). Efforts are being made to increase access to effective treatment, and it has been suggested that behavior analysts may be particularly well suited to working with patients with SUDs given their training in the analyses and treatment of problem behavior (Normand & Kohn, 2013). Behavior analysis has made, and continues to make, important contributions to the area of SUDs with efficacious treatments, such as contingency management, the community-reinforcement approach, and the therapeutic workplace (e.g., Higgins, Budney, et al., 1994; Higgins, Delaney, et al., 1991; Higgins, Sigmon, et al., 2003; Silverman, 2004; Silverman, DeFulio, & Sigurdsson, 2012). There are also signs that behavior analysts’ systematic contact with this population is increasing. For example, the Association for Behavior Analysis International not only has an entire program area identifier for behavioral pharmacology but also, in November 2018, held a full conference dedicated to substance use and addiction. Also, as part of their strategic plan to support the growth of workforces in underrepresented applied behavior analysis (ABA) practice areas, the Behavior Analyst Certification Board (BACB) has recently convened a work group and created an action plan to increase the number of behavior analysts working with SUDs.
Individuals with SUDs often face stigma and discrimination. The stigmatization and discrimination of individuals with SUDs have been shown to have detrimental effects on their physical and mental health, as well as serve as an important barrier to seeking and continuing treatment for SUDs (Ahern, Stuber, & Galea, 2007; Anstice, Strike, & Brands, 2009; Brener, von Hippel, von Hippel, Resnick, & Treloar, 2010; Kerridge et al., 2017; Link, Struening, Rahav, Phelan, & Nuttbrock, 1997; Radcliffe & Stevens, 2008). A recent study found that people in the general population hold significantly more negative views toward persons with drug addiction than those with other mental illnesses (Barry, McGinty, Pescosolido, & Goldman, 2014). Specifically, results of this study showed that people were more willing to accept discriminatory practices, were more doubtful about the effectiveness of treatments, and were more likely to oppose public policies directed at helping people with drug addiction than those with mental illness.
Health care professionals, who are crucial to facilitating access to treatment for patients with SUDs, are not immune to these prejudices. Research has shown that health care professionals often have negative views and attitudes toward patients with SUDs, which can have a negative impact on the care these patients receive (Deans & Soar, 2005; Ford, 2011; Gilchrist et al., 2011; Howard & Chung, 2000; Van Boekel, Brouwers, Van Weeghel, & Garretsen, 2013a, 2014). It is possible that these negative attitudes stem from the historical view of addiction as a moral shortcoming or lack of willpower. Research has shown that negative attitudes toward individuals with SUDs are associated with perceived controllability, responsibility, and blame for their disorder (Corrigan, Kuwabara, & O’Shaughnessy, 2009; Corrigan, Markowitz, Watson, Rowan, & Kubiak, 2003; Schomerus et al., 2011; Van Boekel, Brouwers, Van Weeghel, & Garretsen, 2013b, 2014; Weiner, Perry, & Magnusson, 1988).
Behavior analysts’ treatment approach is guided by the underlying philosophy of behaviorism, which proposes that all behavior, including problem behavior, is a result of genetic and environmental factors, as opposed to the free will of an individual. Because behavior analysts recognize that behavior is determined and reject the notion of free will, they do not assign responsibility to an individual for his or her behavior. According to Skinner (1953), we are likely to drop the notion of responsibility once we recognize that the variables responsible for operant behavior are just as inexorable as those responsible for reflex responses. For example, Skinner (1953) wrote that we have every reason to agree with the alcoholic who insists he cannot help drinking. As a result, one would hypothesize that behavior analysts would not view individuals with SUDs more negatively than those with other mental disorders. To our knowledge, no research to date has examined behavior analysts’ views on this subject. Therefore, the purpose of this study is to compare behavior analysts’ attitudes about individuals with SUDs with their attitudes about those with other mental disorders.
Method
Participants
We recruited participants through the BACB e-mail list. Invitations to participate in this study were sent via e-mail to Board Certified Behavior Analyst (BCBA) and Board Certified Behavior Analyst–Doctoral (BCBA-D) certificants in the United States. We did not restrict recruitment based on any other variables, such as primary emphasis of work, primary area of work, or primary age group of certificants’ clients. The survey was distributed on September 11, 2018, and we received all responses that same day. Participants were compensated with a $15 electronic gift card for completing the survey. The University of Vermont Institutional Review Board reviewed the protocol and declared it exempt from further review.
Measures
We administered the online survey electronically using Qualtrics www.qualtrics.com. Participants were asked to complete the same survey items developed by Barry et al. (2014), which consisted of 11 items assessing their attitudes on drug addiction, and the same 11 items assessing their attitudes on mental illness (Table 1). Though the terms SUD and mental disorders would have been preferred, we retained the terms drug addiction and mental illness to be consistent with the terminology used by Barry et al. The first two questions related to stigma and were designed to measure desire for social distance from people with drug addiction and mental illness. The next three statements related to the acceptability of discrimination. The next two statements related to the effectiveness of treatment. The final four statements gauged support for policy issues regarding insurance parity and government spending on treatment, housing, and job support.
Table 1.
Survey items
| 1. | Would you be willing to have a person with drug addiction marry into your family? |
| 2. | Would you be willing to have a person with drug addiction start working closely with you on a job? |
| 3. | Discrimination against people with drug addiction is a serious problem. |
| 4.* | Employers should be allowed to deny employment to persons with drug addiction. |
| 5.* | Landlords should be able to deny housing to a person with drug addiction. |
| 6. | The treatment options for persons with drug addiction are effective at controlling symptoms. |
| 7. | Most people with drug addiction can, with treatment, get well and return to productive lives. |
| 8. | Do you favor or oppose requiring insurance companies to offer benefits for the treatment of drug addiction? |
| 9. | Do you favor or oppose increasing government spending on the treatment of drug addiction? |
| 10. | Do you favor or oppose increasing government spending on programs to subsidize housing costs for people with drug addiction? |
| 11. | Do you favor or oppose increasing government spending on programs that help people with drug addiction find jobs and provide on-the-job support as needed? |
To assess views on mental illness, the previous statements were presented with the words mental illness replacing drug addiction
*Higher values indicate a more positive attitude for all items except Items 4 and 5, in which higher values indicate a more negative attitude
Participants responded to each item by moving a slider left or right on a visual analogue scale (VAS) ranging from 0 to 100; 0 indicated definitely unwilling, strongly disagree, or strongly oppose, and 100 indicated definitely willing, strongly agree, or strongly favor, depending on the item. Higher scores indicated a more positive attitude for all items with the exception of Items 4 and 5, in which it was the opposite. To minimize concerns about priming, the order of items relating to drug addiction and mental illness were counterbalanced across respondents such that approximately half of the participants (N = 155) responded to items about drug addiction first and the other half (N = 133) responded to items about mental illness first. Participants also provided information regarding their sociodemographic characteristics.
Data Analysis
Mixed model analyses of variance corresponding to a crossover design (Jones & Kenward, 2015) were used to compare participants’ VAS responses relating to individuals with drug addiction and mental illness and to test for order effects for each of the 11 items. Additional analyses of variance (ANOVA) were performed to examine associations between participant responses and their sociodemographic and professional characteristics. Pairwise comparisons were based on Fisher’s Least Significant Difference (LSD) procedure. For some characteristics (e.g., age and years of work experience), adjacent categories were collapsed to allow for reasonable sample sizes within each category. Characteristics examined were age (18–34 years vs. ≥35 years), sex (male vs. female), race/ethnicity (White vs. non-White), political affiliation (Democrat vs. Republican vs. Independent), highest degree obtained (master’s vs. doctorate), certification (BCBA vs. BCBA-D), years of training and work experience (≤5 years vs. 6–10 years vs. ≥11 years), self-identification as a behavior analyst (yes vs. no), and adherence to a behavioral philosophy (yes vs. no). The outcome measure for examining sociodemographic characteristics was the difference in participants’ response to each question as it related to mental illness and SUD (i.e., VASDiff = VASMental Illness − VASDrug Addiction). Effect sizes (ES) were computed based on Cohen’s d, where two conditions or groups are being compared, and Cohen’s f, for more than two groups (Cohen, 1988). All statistical analyses were performed using SAS Statistical Software Version 9.4 (SAS Institute, Cary, NC). Statistical significance was determined based on α = .05.
Results
A total of 288 participants completed the survey. Table 2 shows the sociodemographic characteristics of the sample. About half of the participants were 18–34 years old (52%), with the majority being female (83%), White (77%), and approximately half self-identifying as Democrats (48%). For the majority of participants, the highest degree obtained was a master’s (82%), and they were predominantly BCBA certificants (87%). About half of the participants had 11 or more years of training and work experience (44%). Most participants identified as behavior analysts (92%) and adhered to a behavioral philosophy (68%), but only half endorsed radical behaviorism as their personal philosophy (44%). Additionally, the majority of participants were clinicians (74%), reported that their primary area of practice was autism (91%), and had a disciplinary background in ABA (99%); only 1% reported a primary area of practice and disciplinary background in substance abuse or addiction (data not shown).
Table 2.
Sociodemographic characteristics of sample (N=288)
| Characteristic | n (%) |
|---|---|
| Personal characteristics | |
| Age (years) | |
| 18–34 | 151 (52%) |
| 35 or older | 137 (48%) |
| Sex | |
| Male | 44 (15%) |
| Female | 239 (83%) |
| Prefer not to answer | 5 (2%) |
| Race/ethnicity | |
| Asian or Pacific Islander | 18 (6%) |
| Black or African American | 4 (1%) |
| Hispanic or Latino/a | 23 (8%) |
| White | 221 (77%) |
| Other/Prefer not to answer | 20 (7%) |
| Political affiliation | |
| Democrat | 137 (48%) |
| Republican | 36 (13%) |
| Independent | 60 (21%) |
| Don’t know/Prefer not to answer | 40 (14%) |
| Professional characteristics | |
| Highest degree obtained | |
| Master’s degree | 235 (82%) |
| Doctoral degree | 53 (18%) |
| Certification | |
| BCBA | 250 (87%) |
| BCBA-D | 38 (13%) |
| Years of training and work experience (years) | |
| ≤5 | 61 (21%%) |
| 6–10 | 101 (35%) |
| ≥11 | 126 (44%) |
| Identify as a behavior analyst | |
| Yes | 265 (92%) |
| No | 18 (6%) |
| Don’t know | 5 (2%) |
| Adhere to a behavioral philosophy | |
| Yes | 197 (68%) |
| No | 47 (16%) |
| Don’t know | 44 (15%) |
| Personal philosophy | |
| Radical behaviorism | 126 (44%) |
| Functional contextualism | 33 (11%) |
| Interbehaviorism | 7 (2%) |
| Methodological behaviorism | 26 (9%) |
| Not behaviorism | 2 (1%) |
| Not sure | 79 (27%) |
| Other | 15 (5%) |
Comparison of Attitudes
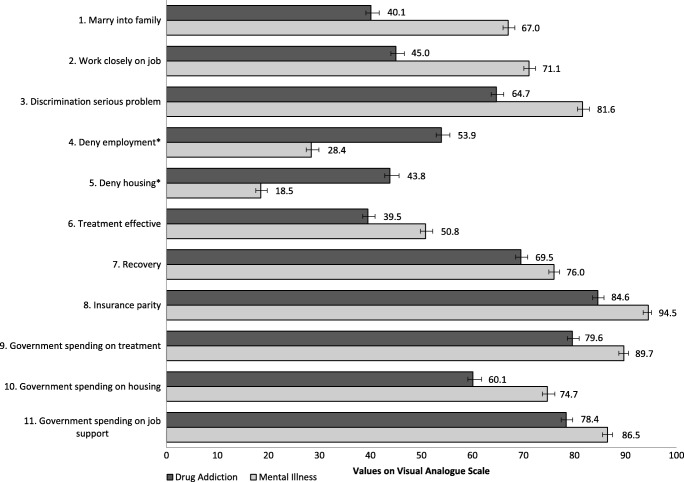
Across all items on the survey, participants responded significantly more negatively to items pertaining to those with drug addiction relative to those with mental illness (Fig. 1).
Fig. 1.
Mean values per survey item. Participants responded by moving a slider left or right on a visual analogue scale (VAS) with a range of 0 to 100; 0 indicated either definitely unwilling, strongly disagree, or strongly oppose, whereas 100 indicated definitely willing, strongly agree, or strongly favor, depending on the item. Higher values indicate a more positive attitude for all items except those that are asterisked (Items 4 and 5), in which higher values indicate a more negative attitude. Error bars represent Standard error. For all items, participants responded significantly more negatively to items pertaining to those with drug addiction relative to those with mental illness (p < .001). For the first two items, mean responses were dependent on the order of presentation (ps < .05). For Item 1, means were 44.8 versus 71.0 when mental illness was presented first and 36.4 versus 63.6 when drug addiction was presented first. For Item 2, corresponding means were 47.8 versus 75.0 when mental illness was presented first and 42.5 versus 67.4 when drug addiction was presented first
Stigma
Results indicated higher levels of desire for social distance from those with drug addiction than from those with mental illness. Participants were less willing to have a person with drug addiction marry into their family than someone with mental illness, ES = 1.07, F(286) = 299.3, p < .001 (Fig. 1, Item 1). They were also less willing to have a person with drug addiction work closely with them on a job compared to someone with mental illness, ES = 1.04, F(1,286) = 302.7, p < .001 (Fig. 1, Item 2). For these first two items, mean responses were dependent on presentation order, with greater willingness for both types when mental illness items were presented prior to drug abuse items (see Fig. 1’s caption for more details).
Acceptability of Discrimination
On average, respondents agreed that discrimination against people with both drug addiction and mental illness is a serious problem (mean score on Item 3 = 73.2); however, they more strongly agreed that discrimination was problematic for those with mental illness than for those with drug addiction, ES = 0.77, F(1,286) = 136.9, p < .001 (Fig. 1, Item 3). They also disagreed more strongly that employers should be allowed to deny employment and that landlords should be able to deny housing to those with mental illness than to those with drug addiction, ESs = 0.94 and 0.95, Fs(1,286) = 622.5 and 222.0, respectively, ps < .001 (Fig. 1, Items 4 and 5).
Effectiveness of Treatment
Participants responded significantly more positively to statements regarding treatment effectiveness and recovery for mental illness than for drug addiction. They more strongly agreed that treatment options for people with mental illness are effective in controlling symptoms and that people with mental illness can get well and return to productive lives relative to people with drug addiction, ESs = 0.47 and 0.31, Fs(1,286) = 53.3 and 25.0, respectively, ps < .001 (Fig. 1, Items 6 and 7).
Policy
Participants reported high levels of support for public policies directed at helping both groups of people (mean score on Items 8–11 = 81.0), but they more strongly supported policies directed at helping those with mental illness than policies supporting those with drug addiction. Participants showed significantly more support for policies requiring insurance companies to offer benefits for treatment for those with mental illness than for those with drug addiction, and were more supportive of increasing government spending on treatment for mental illness than for drug addiction, ESs = 0.60 and 0.52, Fs(1, 286) = 81.0 and 94.1, respectively, ps < .001 (Fig. 1, Items 8 and 9). Participants also more strongly favored increasing government spending on programs to subsidize housing costs for people with mental illness than for people with drug addiction, and more strongly favored increasing government spending on programs that help people with mental illness find jobs and provide on-the-job support than for people with drug addiction, ESs = 0.54 and 0.42, Fs(1,286) = 144.0 and 60.8, respectively, ps < .001 (Fig. 1, Items 10 and 11).
Correlates of Divergent Attitudes on Mental Illness and Drug Addiction
Tables 3 and 4 display participant characteristics that were significantly associated with disparity in VAS responses to drug addiction and mental illness (i.e., divergent responses or attitudes) for specific items discussed subsequently.
Table 3.
Associations between divergent attitudes and sociodemographic characteristics
| Characteristic | Item | Category | Drug addiction | Mental illness | Mean difference | p value |
|---|---|---|---|---|---|---|
| Age | 1 | 18–34 | 38.9 ± 2.2 | 69.0 ± 1.7 | 30.1 ± 2.1 | .028 |
| 35 or greater | 41.5 ± 2.4 | 64.8 ± 2.1 | 23.3 ± 2.2 | |||
| 2 | 18–34 | 42.4 ± 2.3 | 72.6 ± 1.7 | 30.2 ± 2.2 | .004 | |
| 35 or greater | 47.8 ± 2.4 | 69.4 ± 1.9 | 21.6 ± 1.9 | |||
| Sex | 1 | Male | 44.9 ± 4.5 | 63.4 ± 3.7 | 18.5 ± 3.3 | .013 |
| Female | 39.1 ± 1.8 | 68.0 ± 1.4 | 28.9 ± 1.7 | |||
| 2 | Male | 53.6 ± 3.9 | 72.0 ± 3.0 | 18.5 ± 3.5 | .022 | |
| Female | 43.3 ± 1.9 | 71.2 ± 1.4 | 28.0 ± 1.7 | |||
| 9 | Male | 84.0 ± 3.0 | 88.8 ± 2.4 | 4.8 ± 2.0 | .027 | |
| Female | 78.9 ± 1.5 | 90.2 ± 1.0 | 11.3 ± 1.2 | |||
| Certification | 3 | BCBA | 63.9 ± 1.5 | 82.0 ± 1.2 | 18.1 ± 1.6 | .039 |
| BCBA-D | 70.0 ± 4.0 | 78.9 ± 3.9 | 8.9 ± 4.5 | |||
| Behavioral philosophy | 6 | Yes | 40.0 ± 1.8 | 49.3 ± 1.7 | 9.3 ± 1.8 | .003 |
| No | 36.3 ± 3.1 | 58.1 ± 3.3 | 21.7 ± 4.0 |
Higher values under “Drug Addiction” and “Mental Illness” indicate a more positive attitude. Mean difference computed as Mental Illness − Drug Addiction
Table 4.
Associations between divergent attitudes and political affiliation
| Item | Political affiliation | Drug addiction | Mental illness | Mean difference+ | p value# |
|---|---|---|---|---|---|
| 4* | Democrat | 48.7 + 2.4 | 26.3 + 2.0 | 22.3 + 2.5a | |
| Republican | 75.0 + 3.6 | 37.7 + 5.4 | 37.4 + 7.2b | .033 | |
| Independent | 53.9 + 3.7 | 25.6 + 3.1 | 28.3 + 3.7ab | ||
| 5* | Democrat | 37.1 + 2.4 | 15.2 + 1.6 | 21.9 + 2.2a | |
| Republican | 70.2 + 4.8 | 30.9 + 4.8 | 39.3 + 6.8b | .005 | |
| Independent | 47.0 + 4.1 | 16.2 + 2.5 | 30.8 + 4.0ab | ||
| 6 | Democrat | 35.7 + 1.9 | 52.0 + 1.9 | 16.4 + 2.1a | |
| Republican | 46.5 + 3.8 | 53.4 + 4.2 | 6.9 + 4.5b | .029 | |
| Independent | 42.7 + 3.6 | 50.6 + 2.9 | 7.9 + 3.0b | ||
| 8 | Democrat | 88.5 + 16.8 | 95.5 + 0.8 | 7.0 + 1.3a | |
| Republican | 68.5 + 4.7 | 89.7 + 2.6 | 21.2 + 5.0b | <.001 | |
| Independent | 86.2 + 2.1 | 95.9 + 1.0 | 9.7 + 2.0a | ||
| 9 | Democrat | 84.9 + 1.7 | 93.2 + 1.0 | 8.3 + 1.3a | |
| Republican | 61.4 + 3.9 | 78.9 + 3.6 | 17.5 + 4.2b | .016 | |
| Independent | 78.0 + 2.8 | 89.7 + 2.1 | 11.7 + 1.9ab | ||
| 11 | Democrat | 82.8 + 1.6 | 89.1 + 1.4 | 6.3 + 1.2a | |
| Republican | 62.4 + 3.8 | 79.3 + 3.0 | 16.8 + 4.2b | .004 | |
| Independent | 78.3 + 2.6 | 85.4 + 2.1 | 7.1 + 2.1a |
Age
Participants between the ages of 18–34 years had greater discrepancies between mental illness and drug addiction for Items 1 and 2 related to stigma than participants ≥35 years. Participants in the 18- to 34-years group indicated greater desire for social distance from those with drug addiction and lower levels for the same for those with mental illness than participants ≥35 years, ESs = 0.26 and 0.34, Fs(1, 283) = 4.8 and 8.3, respectively, ps ≤ .029 (Table 3).
Sex
Sex was significantly associated with discrepant answers for Items 1, 2, and 9. For all three, females answered more discrepantly than males and rated those with drug addiction more negatively than males, ESs = 0.43, 0.39 and 0.36, Fs(1, 278) = 6.1, 5.3, and 4.9, respectively, ps ≤ .027 (Table 3).
Certification and Behavioral Philosophy
Certification was only significantly associated with Item 3. Specifically, BCBAs less strongly agreed that discrimination against those with drug addiction is a serious problem and more strongly agreed that discrimination against people with mental illness is a serious problem than BCBA-Ds did, ES = 0.34, F(1, 286) = 4.3, p = .039 (Table 3). Behavioral philosophy was only significantly associated with Item 6. Respondents who did not adhere to a behavioral philosophy disagreed more strongly that treatment options for people with drug addiction are effective at controlling symptoms and agreed more strongly that treatment options for people with mental illness are effective at controlling symptoms when compared to respondents who adhered to a behavioral philosophy, ES = 0.48, F(1, 242) = 8.9, p = .003 (Table 3).
Political Affiliation
Table 4 displays political affiliation characteristics that were significantly associated with disparity in VAS responses to drug addiction and mental illness for specific items. Political affiliation was significantly associated with divergent responses for a majority of the survey items. Republicans had significantly more divergent responses from Democrats and Independents for Items 8 and 11, ESs = 0.19 and 0.22, Fs(2,230) = 8.5 and 5.6, respectively, ps ≤ .004, and from Democrats alone for Items 4, 5, and 9, ESs = 0.17, 0.21, and 0.18, Fs(2,230) = 3.5, 5.4, and 5.2, respectively, ps ≤ .033. These items were related to the acceptability of discrimination and policy issues. Republicans rated each of these items more negatively for both drug addiction and mental illness compared to Democrats and Independents. Democrats had more divergent responses for Item 6, ES = 0.17 F(2,230) = 3.6, p = .04. They less strongly agreed compared to Republicans and Independents that treatment options for persons with drug addiction and mental illness are effective at controlling symptoms.
Discussion
This study showed that behavior analysts have significantly more negative attitudes toward people with drug addiction than toward people with mental illness. Behavior analysts reported a greater desire for social distance and greater acceptability of discrimination for people with drug addiction than for people with mental illness. They also reported less potential for recovery and lower support for policies to improve equity in insurance coverage and government funding to improve treatment, housing, and job support for people with drug addiction.
These results are generally consistent with views endorsed by the general population (Barry et al., 2014), which is interesting given the deterministic tenet of behaviorism. Previous research suggests that negative attitudes toward people with SUDs are associated with the view that addiction is blameworthy and the result of a lack of willpower (Corrigan, Kuwabara, & O’Shaughnessy, 2009; Corrigan, Markowitz, et al., 2003; Schomerus et al., 2011; Weiner et al., 1988). Because behavior analysts supposedly reject the notion that decisions happen freely, and instead believe that behavior is determined by heredity and environmental factors, we expected to find less divergent attitudes toward people with drug addiction and mental illness.
One possible explanation for these results is that behavior analysts are not all behaviorists in their philosophical views. In fact, only 68% of participants stated that they adhered to a behavioral philosophy. It is also possible that, even among those participants who endorsed a behavioral philosophy, some were not well versed in the philosophical tenets of behaviorism despite having met the requisites to be certified by the BACB. For example, 9% of participants endorsed methodological behaviorism as their personal philosophy. This is rather suspect considering that it is a somewhat outdated version of behaviorism that ignores or denies the relevance of private events, such as thinking and feeling (Baum, 2005; Bergmann, 1956; Moore, 1980; Skinner, 1974; Watson, 1913). Therefore, it is possible that behavior analysts who self-identified as behaviorists still subscribed to the lay view of addiction that remains pervasive in the general population. The possibility that some behavior analysts might not have a full understanding of the philosophical tenets of behaviorism may explain why self-identifying as a behaviorist was not a significant characteristic associated with nondivergent responses for more than one survey item.
Political affiliation was the only demographic characteristic that was associated with divergent responding for the majority of the items in the survey. Barry et al. (2014) also found some differences in responding as a function of political affiliation. In the current study, Republicans had more divergent responding, rating drug abuse significantly more negatively than mental illness, than Democrats on five items related to the acceptability of discrimination and policy issues. Democrats had more divergent responding, also rating drug abuse more negatively than mental illness, than Republicans for one item related to treatment effectiveness. Conservative ideology tends to emphasize self-reliance and personal responsibility (Skitka & Tetlock, 1992, 1993). Some studies have found that conservative attitudes are associated with a greater belief in free will and that conservatives are more likely to hold people responsible for their moral wrongdoing (Carey & Paulhus, 2013; Clark et al., 2017). It is possible that political affiliation was a predictor of divergent responding due to the association between conservative attitudes and a belief in free will.
Health care professionals who specialize in addiction services tend to have more positive attitudes toward individuals with SUDs than do health care professionals who specialize in other areas (Van Boekel et al., 2014). Though there are effective behavior-analytic treatments for SUDs, only 1% of our sample endorsed “substance abuse and/or addiction” as their primary area of practice or research. Behavior analysts working with individuals with SUDs are probably less likely to pursue or maintain certification through the BACB because it is not widely recognized in this area of practice. Therefore, they were less likely to be in our participant pool. It is possible that our results would differ if we had sampled a greater number of respondents working with individuals with SUDs.
In interpreting our results, it is important to note that from a behavior-analytic perspective, attitudes are simply verbal behavior. As with any verbal behavior, attitudes are shaped and maintained by the practices of a verbal community (Guerin, 1994). Thus, it is possible that behavior analysts’ attitudes toward individuals with SUDs and mental disorders have not been strongly shaped by a behavior-analytic community and instead are more robustly controlled by verbal communities outside the field of behavior analysis (e.g., those better defined by political affiliation). This might explain why the divergent attitudes found in our results do not align with a behavior-analytic worldview. Stigma and discrimination are critically important issues, and yet they are often unaddressed or largely ignored in the field of behavior analysis. Results from this study indicate that behavior analysts may benefit from training that addresses these issues, possibly through coursework, continuing education, or other opportunities.
There are several limitations to this study that should be noted. First, respondents were not selected at random; instead, we used a convenience sample that may have been subject to response bias. Second, we were not specific about the nature of either disorder or the severity. For example, people may have responded differently if the drug addiction items specified cigarette smoking and the mental illness items specified schizophrenia. Third, although the differences in responses to all items were statistically significant, we do not have a method for determining whether the magnitude of these differences is socially significant. For example, it is possible that the mean scores on Item 8, 84.6 and 94.5, do not indicate a meaningful difference in support for requiring that insurance companies offer benefits for treatment. Finally, we used the terms drug addiction and mental illness to be consistent with Barry et al. (2014); however, these are stigmatizing terms, and terminology such as SUD and mental disorder would have been less stigmatizing and more accurate.
In conclusion, participants responded significantly more negatively toward individuals with drug addiction than they did toward those with mental illness for all survey items, including items relating to stigma, acceptability of discrimination, effectiveness of treatment, and policy. Results from this study suggest that although philosophical underpinnings, including radical behaviorism and determinism, are part of the foundational knowledge that should be mastered prior to entering practice (BACB, 2012, 2017), many BCBAs and BCBA-Ds do not adhere to a behavioral philosophy. These results also suggest that behavior analysts may benefit from trainings addressing stigma and discrimination with respect to individuals with SUDs.
Author Note
We would like to thank Dr. Matthew Price for his assistance with Qualtrics.
This work was partially supported by grants from the National Institute on Drug Abuse (R01DA036670, R01DA047867, and T32DA07242).
Compliance with Ethical Standards
Conflict of Interest
Catalina N. Rey declares that she has no conflict of interest. Allison N. Kurti declares that she has no conflict of interest. Gary J. Badger declares that he has no conflict of interest. Alex H. Cohen declares that he has no conflict of interest. Sarah H. Heil declares that she has no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Ahern J, Stuber J, Galea S. Stigma, discrimination and the health of illicit drug users. Drug and Alcohol Dependence. 2007;88:188–196. doi: 10.1016/j.drugalcdep.2006.10.014. [DOI] [PubMed] [Google Scholar]
- Anstice S, Strike CJ, Brands B. Supervised methadone consumption: Client issues and stigma. Substance Use and Misuse. 2009;44(6):794–808. doi: 10.1080/10826080802483936. [DOI] [PubMed] [Google Scholar]
- Barry CL, McGinty EE, Pescosolido B, Goldman HH. Stigma, discrimination, treatment effectiveness and policy support: Comparing public views about drug addiction with mental illness. Psychiatric Services. 2014;65(10):1269–1272. doi: 10.1176/appi.ps.201400140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum WM. Understanding behaviorism: behavior, culture, and evolution. 2. Malden, MA: Blackwell Publishing; 2005. [Google Scholar]
- Behavior Analyst Certification Board. (2012). BCBA/BCaBA Task List (4th ed.) [White paper]. Retrieved from https://www.bacb.com/wp-content/uploads/2017/09/160101-BCBA-BCaBA-task-list-fourth-edition-english.pdf.
- Behavior Analyst Certification Board. (2017). BCBA/BCaBA Task List (5th ed.) [White paper]. Retrieved from https://www.bacb.com/wp-content/uploads/2017/09/170113-BCBA-BCaBA-task-list-5th-ed-.pdf.
- Bergmann G. The contribution of John B. Watson. Psychological Review. 1956;63:265–276. doi: 10.1037/h0049200. [DOI] [PubMed] [Google Scholar]
- Brener L, von Hippel W, von Hippel C, Resnick I, Treloar C. Perceptions of discriminatory treatment by staff as predictors of drug treatment completion: Utility of a mixed methods approach. Drug and Alcohol Review. 2010;29:491–497. doi: 10.1111/j.1465-3362.2010.00173.x. [DOI] [PubMed] [Google Scholar]
- Carey JM, Paulhus DL. Worldview implications of believing in free will and/or determinism: Politics, morality, and punitiveness. Journal of Personality. 2013;81(2):130–141. doi: 10.1111/j.1467-6494.2012.00799.x. [DOI] [PubMed] [Google Scholar]
- Clark, C. J., Everett, J. A., Luguri, J. B., Earp, B. D., Ditto, P. H., & Shariff, A. (2017). Political differences in free will belief are driven by differences in moralization. SSRN Electronic Journal.10.2139/ssrn.3011597. [DOI] [PubMed]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Corrigan P, Markowitz FE, Watson A, Rowan D, Kubiak MA. An attribution model of public discrimination towards persons with mental illness. Journal of Health and Social Behavior. 2003;44:162–179. doi: 10.2307/1519806. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Kuwabara SA, O’Shaughnessy J. The public stigma of mental illness and drug addiction: Findings from a stratified random sample. Journal of Social Work. 2009;9:139–147. doi: 10.1177/1468017308101818. [DOI] [Google Scholar]
- Deans C, Soar R. Caring for clients with dual diagnosis in rural communities in Australia: The experience of mental health professionals. Journal of Psychiatric and Mental Health Nursing. 2005;12:268–274. doi: 10.1111/j.1365-2850.2005.00830.x. [DOI] [PubMed] [Google Scholar]
- Ford R. Interpersonal challenges as a constraint on care: The experience of nurses’ care of patients who use illicit drugs. Contemporary Nurse. 2011;37:241–252. doi: 10.5172/conu.2011.37.2.241. [DOI] [PubMed] [Google Scholar]
- Gilchrist G, Moskalewicz J, Slezakova S, Okruhlica L, Torrens M, Vajd R, Baldacchino A. Staff regard towards working with substance users: A European multi-centre study. Addiction. 2011;106(6):1114–1125. doi: 10.1111/j.1360-0443.2011.03407.x. [DOI] [PubMed] [Google Scholar]
- Guerin B. Attitudes and beliefs as verbal behavior. The Behavior Analyst. 1994;17:155–163. doi: 10.1007/BF03392661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Foerg FE, Donham R, Badger G. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Archives of General Psychiatry. 1994;51:568–576. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Delaney DD, Budney AJ, Bickel WK, Hughes JR, Foerg F, Fenwick JW. A behavioral approach to achieving initial cocaine abstinence. The American Journal of Psychiatry. 1991;148(9):1218–1224. doi: 10.1176/ajp.148.9.1218. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Sigmon SC, Wong CJ, Heil SH, Badger GJ, Donham R, et al. Community reinforcement therapy for cocaine-dependent outpatients. Archives of General Psychiatry. 2003;60(10):1043–1052. doi: 10.1001/archpsyc.60.9.1043. [DOI] [PubMed] [Google Scholar]
- Howard MO, Chung SS. Nurses’ attitudes towards substance misusers I: Surveys. Substance Use & Misuse. 2000;35(3):347–365. doi: 10.3109/10826080009147701. [DOI] [PubMed] [Google Scholar]
- Jones B, Kenward MG. Design and analysis of crossover trials. Boca Raton, FL: CRC Press; 2015. [Google Scholar]
- Kerridge Bradley T., Mauro Pia M., Chou S. Patricia, Saha Tulshi D., Pickering Roger P., Fan Amy Z., Grant Bridget F., Hasin Deborah S. Predictors of treatment utilization and barriers to treatment utilization among individuals with lifetime cannabis use disorder in the United States. Drug and Alcohol Dependence. 2017;181:223–228. doi: 10.1016/j.drugalcdep.2017.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: Evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. Journal of Health and Social Behavior. 1997;38(2):177–190. doi: 10.2307/2955424. [DOI] [PubMed] [Google Scholar]
- Moore J. On behaviorism and private events. Psychological Record. 1980;30:459–475. doi: 10.1007/BF03394698. [DOI] [Google Scholar]
- Normand Matthew P., Kohn Carolynn S. Don’t wag the dog: Extending the reach of applied behavior analysis. The Behavior Analyst. 2013;36(1):109–122. doi: 10.1007/BF03392294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radcliffe P, Stevens A. Are drug treatment services only for “thieving junkie scumbags”? Drug users and the management of stigmatised identities. Social Science & Medicine. 2008;67(7):1065–1073. doi: 10.1016/j.socscimed.2008.06.004. [DOI] [PubMed] [Google Scholar]
- Schomerus G, Lucht M, Holzinger A, Matschinger H, Carta MG, Angermeyer MC. The stigma of alcohol dependence compared with other mental disorders: A review of population studies. Alcohol and Alcoholism. 2011;46:105–112. doi: 10.1093/alcalc/agq089. [DOI] [PubMed] [Google Scholar]
- Silverman K. Exploring the limits and utility of operant conditioning in the treatment of drug addiction. The Behavior Analyst. 2004;27(2):209. doi: 10.1007/BF033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, DeFulio A, Sigurdsson SO. Maintenance of reinforcement to address the chronic nature of drug addiction. Preventive Medicine. 2012;55(Suppl):S46–S53. doi: 10.1016/j.ypmed.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner BF. Science and human behavior. New York, NY: Macmillan; 1953. [Google Scholar]
- Skinner BF. About behaviorism. New York, NY: Alfred A. Knopf; 1974. [Google Scholar]
- Skitka LJ, Tetlock PE. Allocating scarce resources: A contingency model of distributive justice. Journal of Experimental Social Psychology. 1992;28(6):491–522. doi: 10.1016/0022-1031(92)90043-J. [DOI] [Google Scholar]
- Skitka LJ, Tetlock PE. Providing public assistance: Cognitive and motivational processes underlying liberal and conservative policy preferences. Journal of Personality and Social Psychology. 1993;65(6):1205–1223. doi: 10.1037/0022-3514.65.6.1205. [DOI] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2018). SAMHSA’s annual mental health, substance use data provide roadmap for future action [White paper]. Retrieved from https://www.hhs.gov/about/news/2018/09/14/samhsa-annual-mental-health-substance-use-data-provide-roadmap-for-future-action.html.
- Van Boekel LC, Brouwers EPM, Van Weeghel J, Garretsen HFL. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug and Alcohol Dependence. 2013;131:23–35. doi: 10.1016/j.drugalcdep.2013.02.018. [DOI] [PubMed] [Google Scholar]
- Van Boekel LC, Brouwers EPM, Van Weeghel J, Garretsen HFL. Public opinion on imposing restrictions to people with an alcohol- or drug addiction: A cross-sectional survey. Social Psychiatry and Psychiatric Epidemiology. 2013;48(12):2007–2016. doi: 10.1007/s00127-013-0704-0. [DOI] [PubMed] [Google Scholar]
- Van Boekel LC, Brouwers EPM, Van Weeghel J, Garretsen HFL. Healthcare professional’s regard towards working with patients with substance use disorders: Comparison of primary care, general psychiatry and specialist addiction services. Drug and Alcohol Dependence. 2014;134:92–98. doi: 10.1016/j.drugalcdep.2013.09.012. [DOI] [PubMed] [Google Scholar]
- Watson JB. Psychology as the behaviorist views it. Psychological Review. 1913;20:158–177. doi: 10.1037/h0074428. [DOI] [Google Scholar]
- Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology. 1988;55:738–748. doi: 10.1037/0022-3514.55.5.738. [DOI] [PubMed] [Google Scholar]