Abstract
Purpose
Define incidence of severe ocular trauma in orbital fracture patients and determine if ocular signs and symptoms are useful predictors of severe ocular injuries.
Methods
Retrospective chart review on all patients with orbital fractures between April 1, 2013, and December 31, 2014. Patients were included if they had radiographic evidence of acute fracture of at least one orbital wall and were evaluated by the Ophthalmology service. Demographics, concurrent injury data, and symptoms and signs of ocular trauma were collected. Concurrent ocular injuries were grouped by severity. Predictive signs or symptoms for severe ocular trauma were identified by stepwise logistic regression analysis. The threshold point for predictive signs and symptoms was detected by a receiver operating characteristic (ROC).
Results
512 patients were included. The most common mechanisms of injury were assault (39%), fall (25%), and motor vehicle accident (21%). The incidence of any concurrent ocular trauma was 75% (383/512), with 14% (70/512) being severe. Four signs and symptoms were predictors of severity: blurred vision (P<0.0001), pain with eye movements (P<0.0001), visual acuity worse than 20/40 in the ipsilateral eye (P<0.001), and restricted motility (P<0.001). The presence of 2 or more of these signs or symptoms was predictive of severe ocular trauma with high sensitivity (91%) and specificity (86%).
Conclusions
In cooperative patients with acute orbital wall fractures, the presence of 2 or more signs or symptoms is predictive of severe ocular trauma and necessitates the need for urgent ophthalmic consultation.
Precis
Severe ocular injury associated with orbital wall fracture is more likely in patients with 2 or more ophthalmic signs or symptoms.
Failure to recognize concomitant ocular injury in orbital fracture patients is a feared consequence of inadequate evaluation in the emergency room setting. The reported incidence of ocular injury ranges from 9–93%, with severe injuries, including vision-threatening diagnoses such as open globe injuries, hyphema, retinal detachment, and orbital compartment syndrome from retrobulbar hemorrhage, reported to be 10–29% of all ocular injuries.1–4
Several studies have previously evaluated ways to recognize ocular injury in maxillofacial trauma patients. Al-Qurainy et al found that impaired visual acuity, blowout orbital fractures, diplopia, and amnesia were the best predictors of severe ocular injury.5, 6 From that review, a 7-item questionnaire was created, which could then be used to indicate the urgency for ophthalmologic evaluation. Unfortunately, the use of this questionnaire has not translated well into clinical practice. In other studies, visual acuity and presence of a relative afferent pupillary defect were found to be strong predictors for ocular injury.7, 8
In the United States, the use of computed tomography (CT) scans in the emergency room setting has quadrupled from 1996 to 2007.9 With the increased number of CT scans, it is expected that the number of orbital fractures detected would increase, with 102,999 diagnosed with orbital fracture in 2007.9 A reflexive, emergent ophthalmology consultation on every orbital fracture potentially places tremendous burden on the healthcare system and will likely yield many normal exams. However, without the identification of predictive signs and symptoms of severe ocular injury, the optimal timing for an ophthalmologic consult is difficult to define. By reviewing data on orbital fracture patients at a level 1 trauma center, our aim is to identify predictors of severe ocular injury in the setting of orbital fractures requiring urgent ophthalmologic consultation.
Methods
A retrospective chart review was performed on all patients presenting with an orbital fracture to the Memorial Hermann Hospital—Texas Medical Center Emergency Department, a level 1 trauma center, between April 1, 2013, and December 31, 2014. Institutional Review Board approval was obtained from The University of Texas Health Science Center Committee for the Protection of Human Subjects and Memorial Hermann Hospital. Informed consent was waived as deemed by the Institutional Review Board. All research adhered to the tenets of the Declaration of Helsinki and was HIPAA compliant.
Patients of all ages were included if they had an acute fracture of at least one orbital wall, as demonstrated on CT scan, and were evaluated by the Ophthalmology service. Patients were excluded for incomplete medical records or inability to cooperate with the ophthalmic exam.
The charts were reviewed for demographic data (age, race, and sex), injury characteristics (date of injury, date of emergency room presentation, date of ophthalmic consultation, mechanism of injury, location of fracture, and concurrent ocular injuries), and mental status. From the Ophthalmology consultation reports, the presence of signs and symptoms of ocular injury were recorded. Reviewed symptoms included blurred vision, pain with eye movements, double vision (binocular diplopia), photophobia, flashes of light, floaters, scotoma, nausea, vomiting, syncope, and tearing. Reviewed signs included near visual acuity (measured by a Rosenbaum pocket vision screener), extraocular movement exam, ocular alignment, and heart rate. Decreased vision was defined as near vision of 20/40 or worse. The concurrent ocular injuries were categorized by level of severity (mild, moderate, or severe; Table 1). If multiple ocular injuries were recorded, the patient’s injuries were categorized by the most severe level. A χ2 test was performed to compare demographics and injury characteristics among severity levels.
Table 1.
Severity of Ocular Injuries
|
Mild ophthalmic injury - Eyelid edema/ecchymosis - Orbital emphysema - Periorbital edema/ecchymosis - Subconjunctival hemorrhage/chemosis |
|
Moderate ophthalmic injury - Conjunctival laceration - Corneal abrasion - Eyelid laceration - Macular edema - Nasolacrimal damage - Traumatic iridocyclitis - Traumatic mydriasis |
|
Severe ophthalmic injury - Angle recession - Hyphema - Muscle entrapment - Open globe injury - Optic nerve injury - Retinal detachment - Retrobulbar hemorrhage - Vitreous hemorrhage |
Predictive signs and symptoms for severe ocular injury were identified by stepwise logistic regression analysis. The number of predictive signs and symptoms for each patient was calculated by summing the significant signs and symptoms identified in the stepwise regression analysis. To determine and verify the optimal number of predictive signs and symptoms that can discriminate between severe and non-severe ocular trauma, we randomly divided the data into training (2/3 of samples) and testing sets (1/3 of samples). The optimal number was determined by logistic regression analysis with Youden optimal threshold criteria.10
The training set was further divided into 3 random subsets. Each training subset was then used to compute the area under receiver operating characteristic curve (AUROC) and Youden optimal threshold. This training procedure was repeated 500 times, and the optimal threshold was determined by the mean of 1500 replicates (=500 × 3 subsets). In addition, mean AUROC, 95% confidence limits, and means of corresponding sensitivity and specificity were calculated.
Then, the recommended Youden optimal thresholds obtained from the training set were applied to the testing data set, and sensitivity, specificity, and kappa were calculated to validate the thresholds. The accuracy statistics were further evaluated with a bootstrapping procedure. The same number of patients in the testing set were randomly selected with replacement from the testing set, and accuracy statistics were calculated using the recommended Youden optimal thresholds. The procedure was repeated 500 times, and the mean, minimum, and maximum of accuracy statistics were calculated to assess the accuracy in classifying a patient with either severe or non-severe ocular injury.
All statistical analyses were performed using SAS for Window 9.4 (SAS Inc., Cary, NC) and R 3.0.3 with optimal.cutoffs() in optimal.cutoffs package. A P value less than 0.05 was considered statistically significant. The AUROC criteria were 0.5 – 0.6 failed; 0.61 to 0.70 poor; 0.71 to 0.80 fair; 0.81 to 0.90 good, and 0.91 – 1.0 excellent. It should be noted that this is statistical classification terminology, which may not reflect clinical terminology.
Results
Of the 592 charts reviewed, 512 patients were included in the study, and 80 were excluded due to an inability to cooperate with the examination. Of the charts included, 484 patients (95%) were evaluated within 1 day of their presentation to the Emergency Room (range 0 to 6 days). The average age was 44 years (range 8 to 94 years), and 74% of the patients were male. Assault was the most common cause of the orbital fracture (39%), followed by falls (25%), and motor vehicle collision (21%) (Table 2).
Table 2.
Demographics and Injury Characteristics
| Variable | All (N=512) |
Severity | ||||
|---|---|---|---|---|---|---|
| None (N=129) |
Mild (N=225) |
Moderate (N=87) |
Severe (N=71) |
P [P*] |
||
| Demographics | ||||||
| Age (years, SD) [Range] | 44.1 (±19.8) [8.0 – 94.0] |
48.1 (±20.2) [8 – 93] |
43.1 (±19.1) [14.3 – 91.2] |
40.8 (±17.6) [17.2 – 85.1] |
44.1 (±22.6) [9.5 – 94] |
0.042 [1.0] |
| Sex (Males, %) | 378 (74%) | 90 (70%) | 166 (74%) | 67 (77%) | 55 (77%) | 0.56 [0.45] |
| Race (%)* | 0.10 [0.24] |
|||||
| White | 242 (48%) | 71 (57%) | 97 (44%) | 36 (42%) | 38 (54%) | |
| Black | 127 (25%) | 24 (19%) | 64 (29%) | 27 (31%) | 12 (17%) | |
| Other (including Hispanics) | 133 (26%) | 30 (24%) | 60 (27%) | 23 (27%) | (20 (29%) | |
| Injury Characteristics | ||||||
| Mechanism of Injury (%) | 0.008 [0.039] |
|||||
| Assault | 201 (39%) | 40 (31%) | 99 (44%) | 38 (44%) | 24 (34%) | |
| Fall | 129 (25%) | 47 (36%) | 52 (23%) | 18 (21%) | 12 (17%) | |
| Motor Vehicle Collision | 106 (21%) | 23 (18%) | 43 (19%) | 23 (26%) | 17 (24%) | |
| Sports-related | 13 (3%) | 3 (2%) | 3 (1%) | 3 (3%) | 4 (6%) | |
| Others | 63 (12%) | 16 (12%) | 28 (12%) | 5 (6%) | 14 (20%) | |
| Injury to Presentation in ED (days, SD) [Range] | 0.5 (±0.7) [0 – 3] |
0.3 (±0.5) [0 – 3] |
0.4 (±0.6) [0 – 3] |
0.8 (±0.9) [0 – 3] |
1.2 (±0.7) [0 – 3] |
0.79 [0.94] |
| Fracture Location | ||||||
| Floor (%) | 0.17 [0.19] |
|||||
| Bilateral | 25 (5%) | 7 (5%) | 15 (7%) | 2 (2%) | 1 (1%) | |
| Left | 198 (39%) | 53 (41%) | 91 (40%) | 29 (33%) | 25 935%) | |
| Right | 155 (30%) | 31 (24%) | 62 (28%) | 34 (39%) | 28 (39%) | |
| Medial Wall (%) | 0.18 [0.92] |
|||||
| Bilateral | 21 (4%) | 5 (4%) | 10 (4%) | 3 (3%) | 3 (4%) | |
| Left | 108 (21%) | 24 (19%) | 45 (20%) | 23 (26%) | 16 (23%) | |
| Right | 97 (19%) | 21 (16%) | 36 (16%) | 25 (29%) | 15 (21%) | |
| Lateral Wall (%) | 0.25 [0.72] |
|||||
| Bilateral | 5 (1%) | 0 (0%) | 5 (2%) | 0 (0%) | 0 (0%) | |
| Left | 40 (8%) | 9 (7%) | 20 (9%) | 4 (5%) | 7 (10%) | |
| Right | 40 (8%) | 6 (5%) | 20 (9%) | 8 (9%) | 6 (8%) | |
| Roof (%) | 0.70 [0.97] |
|||||
| Bilateral | 10 (2%) | 4 (3%) | 5 (2%) | 0 (0%) | 1 (1%) | |
| Left | 26 (5%) | 9 (7%) | 11 (5%) | 3 (3%) | 3 (4%) | |
| Right | 28 (5%) | 4 (3%) | 15 (7%) | 5 (6%) | 4 (6%) | |
Missing10 data points
[P*]: Compare between severe and non-severe patients (including none, mild and moderate ocular injury
SD=standard deviation; ED=emergency department
A total of 383 patients (75%) had a concurrent ocular injury, with 71 patients (14%) having a severe ocular injury. Age (P = 0.042) and mechanism of injury (P = 0.008) were significantly different among severity of ocular injury. The average age of moderate ocular injury patients was younger than those patients without concurrent ocular injury. Patients injured with fall were less likely to have a severe ocular injury (Table 2). The location of fractures did not correlate with severity levels (P > 0.15).
Signs and Symptoms
The average number of reported symptoms on presentation was 0.5 (± 0.7; range 0 to 3), with 294 patients (57%) reporting no ocular symptoms. However, in the cohort of patients with severe injuries, only 8 out of 71 (11%) reported no ocular symptoms. Of the 5 symptoms studied, floaters and flashes of light were only observed in 2 of 512 patients (<0.5%), and photophobia was seen in 13 patients (3%). The most frequently observed symptoms were blurry vision (n=158, 31%), followed by pain with eye movements (n=69, 13%). These 2 symptoms were also seen frequently in injured patients classified as severe (P=0.01, Table 3).
Table 3.
Distributions of Symptoms and Signs
| Variable | All (N=512) |
Severity | ||
|---|---|---|---|---|
| Non-Severe (N=354) |
Severe (N=71) |
P | ||
| Symptoms | ||||
| Blurry Vision (%) | 158 (31%) | 105 (24%) | 53 (75%) | <0.001 |
| Binocular Diplopia (%) | 41 (8%) | 32 (7%) | 9 (13%) | 0.15 |
| Photophobia (%) | 13 (3%) | 12 (3%) | 1 (1%) | 1.0 |
| Floaters/Flashes (%) | 2 (<1%) | 1 (0%) | 1 (1%) | 0.26 |
| Pain with EOM (%) | 69 (13%) | 47 (11%) | 22 (31%) | <0.001 |
| Number of Symptoms (mean, SD) [Range] |
0.5 (±0.7) [0 – 3] |
0.4 (±0.7) [0 – 3] |
1.2 (±0.) [0 −3] |
<0.001 |
| Signs | ||||
| Ipsilateral Vision (%) | 143 (28%) | 88 (20%) | 55(77%) | <0.001 |
| Limited EOM (%) | 177 (35%) | 131 (30%) | 46 (65%) | <0.001 |
| Number of Signs (mean, ±SD) [Range] |
0.6 (±0.7) [0 – 2] |
0.5 (±0.6) [0 – 2] |
1.4 (±0.6) [0 – 2] |
<0.001 |
EOM = extraocular motility; SD=standard deviation
Two hundred and sixty-two patients had no abnormal signs (neither ipsilateral decreased vision nor limited extraocular motility [EOM]). However, in patients with severe ocular injuries, only 3 out of 71 (6%) exhibited no abnormal signs. The incidence of each sign was significantly higher (2 to 3 times higher) in patients with severe injuries (Table 3).
The 4 significant predictors for severe injury identified by stepwise regression analysis were decreased vision (odds ratio [OR] = 7.2, 95% confidence interval [CI] = 3.6 – 14.1, P<0.001), blurry vision (OR = 4.0, 95% CI = 2.1 – 7.8, P<0.001), limited EOM (OR= 2.6, 95% CI = 1.4 – 4.9, P=0.002), and pain with eye movement (OR = 2.7, 95% CI = 1.3 – 5.7, P=0.008). These 4 signs and symptoms were used to compute number of predictive signs and symptoms for each patient. Average number of predictive signs and symptoms was 1.07 (±1.10; range 0 to 4) with 0.84 (±0.95) for non-severe and 2.48 (±0.92) for severe injured, respectively (P<0.001).
Determination of Optimal Threshold
Of 342 patients randomly selected to form the training set, 49 (14%) had ocular injuries classified as severe, which was a similar incidence to the full data set. Figure 1 demonstrates that the number of predictive signs and symptoms were able to discriminate severe and non-severe injury with AUROC=0.87 (good) using one of the subsets of data (n=114) from the training set. In this particular example, the sensitivity and specificity were 0.94 and 0.75, respectively, with the optimal threshold of 2 predictive signs and symptoms. This procedure was repeated 1500 times (=500 × 3), and the results are summarized in Table 4. The mean AUROC was 0.86, which was good (0.81 – 0.9), with the optimal threshold of presenting 2 predictive signs and symptoms. At the optimal threshold, the mean sensitivity was 0.88 (±0.07) with a specificity of 0.80 (±0.07).
Figure 1.
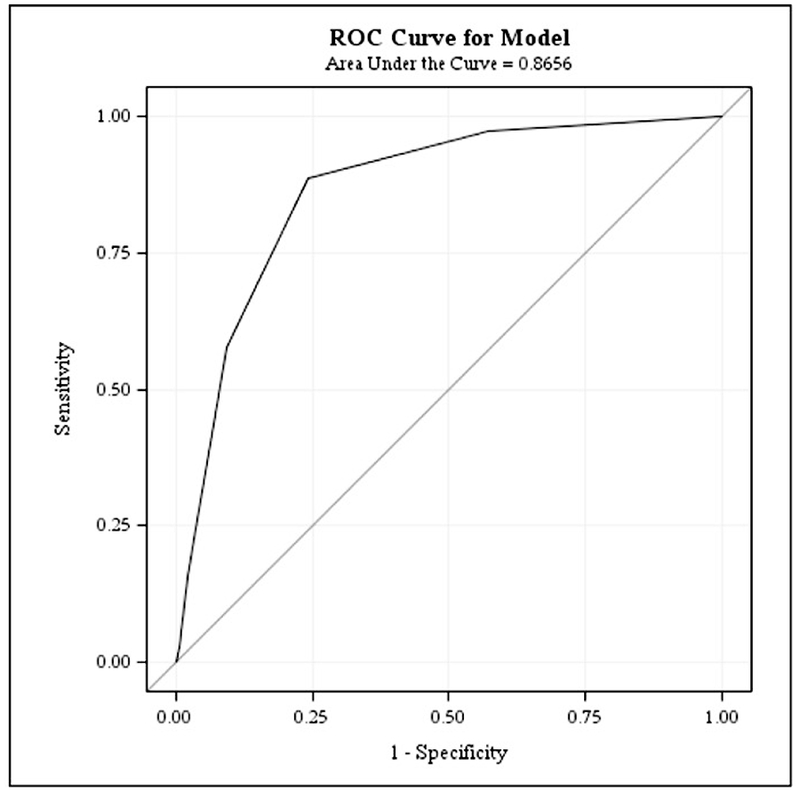
Receiver Operating Characteristic Curve (ROC) demonstrating the number of predictive signs and symptoms that were able to discriminate severe and non-severe injury with AUROC=0.87.
Table 4.
Accuracy Statistics from Training Set
| Statistics | Mean (±SD) | 95% Confidence Interval |
|---|---|---|
| AUROC | 0.86 (±0.04) | 0.79 – 0.94 |
| Optimal Threshold | 2.00 (±0.04) | 1.91 – 2.09 |
| Sensitivity at Optimal Threshold | 0.88 (±0.07) | 0.74 – 1.00 |
| Specificity at Optimal Threshold | 0.80 (±0.03) | 0.74 – 0.87 |
AUROC = area under receiving operating characteristic curve
Thresholds Validation
Of 170 patients in the testing set, 22 patients (13%) had severe injuries. The sensitivity and specificity of 2 predictive signs and symptoms for detection of severe eye injuries were 0.91 and 0.81, respectively. Mean sensitivity and specificity were 0.91 (±0.06) and 0.86 (±0.03) respectively, using 500 bootstrapping procedures.
Discussion
All patient with orbital fractures and suspected severe ocular injury should have a comprehensive ophthalmologic examination on initial presentation, as early detection of ocular injury may change management of orbital fractures and in some circumstances possibly preserve vision. However, when an ophthalmology service is not available, appropriate triage systems for ocular injuries in the setting of facial trauma should be in place for emergency room physicians and facial trauma surgeons. Unfortunately, there is currently no standardization for screening criteria for ocular trauma in orbital fractures. In this study, we propose criteria to predict severe ocular injury warranting urgent ophthalmology consultation.
Maxillofacial fractures with concomitant ocular and periocular injuries have been well documented in the literature.1, 2, 5, 6, 11–16 These injuries range from minor injuries (e.g., subconjunctival hemorrhage or chemosis), with minimal and reversible visual impairment, to severe injuries (e.g., retinal detachment, lens subluxation, or globe rupture), with devastating and irreversible visual consequences. Traditionally, ophthalmologists have reported a higher incidence of ocular injuries in facial trauma compared to non-ophthalmologists.1, 2, 5, 6, 11–16 Some injuries may appear minimal but mask severe ocular dysfunction, and subtle signs and symptoms of eye injury may be missed by non-ophthalmologists.
The relationship between the anatomic location of orbital fractures and ocular injury has been well studied.7, 8, 17–20 In a study of orbital roof fractures, Fulcer and Sullivan reported 8 out of 22 patients with orbital roof fractures had ocular injuries, and most of the injuries (5 of 8) were severe and associated with vision loss.18 Conversely, studies by Andrews et al and Chow et al found that the pattern and location of the orbital fractures did not correlate with the severity of ocular injury.7, 8 Similarly, in our study we found no correlation between the severity of ocular injury and location of the fracture. Interestingly, Andrews et al also analyzed the depth of orbital fractures, and they reported that fractures involving the posterior 1/3 of the orbit had a strong association with ocular injury, presumably due to the higher energy required to generate a posterior orbital fracture.7 Depth of orbital fracture was not assessed in our study.
Emergency room physicians and maxillofacial trauma surgeons typically rely on patient symptoms to determine whether an ophthalmologic evaluation is necessary. However, there is a paucity of data on the correlation between subjective visual complaints and severity of ocular injury. In a case series by Mellema et al, the presence of ophthalmic symptoms, including blurry vision, pain, photophobia, diplopia, nausea, floaters, photopsias, scotomata, dizziness, tearing, and pressure sensation, reported at initial presentation is a very sensitive predictor of severe ocular injury. Blurry vision was not assessed independently from other visual symptoms. Interestingly, their results showed no statistical correlation between visual acuity and severity of injury.21 In another case review by Chow et al, subjective visual acuity changes were found to be a key predictor of occult major ocular injury.8 In our study, blurry vision was reported in 75% of patients with severe ocular injuries, as compared to in 24% of patients with non-severe injuries. This finding matches that reported elsewhere in the literature.7, 8 It is important to note that a quarter of the patients with severe ocular injuries did not report blurry vision on initial presentation, signifying that these injuries may manifest with other ocular findings.
Previous studies have suggested that decreased visual acuity is an important predictor of ocular injuries. Decreased visual acuity associated with ocular injury ranges from 4 to 22% of facial fracture patients.3, 5, 6, 14, 22, 23 A systematic review by Kim et al reported that decreased visual acuity was associated with 7.5% of blowout fractures and 8.3% of non-blowout fractures.24 Among the studies that reported quantitative data on visual acuity, a case review series by Mellema et al showed 53% of patients with severe ocular injuries had visual acuities 20/40 or worse, as compared to 11% of patients with non-severe injuries.21 In a retrospective review by Petro et al, decreased visual acuity was found in 14 of 26 (53.8%) patients with concurrent facial fractures and ocular injuries.4 Al-Qurainy et al reported that decreased visual acuity alone had an 80% sensitivity in detecting severe concomitant ocular injuries in patients with midface fractures.5, 6 In our study, the incidence of decreased visual acuity was 77% in patients with severe ocular injuries, which is twice as high as in the group of patients with non-severe injuries. Compared to other studies, the incidence of decreased visual acuity reported in our study is significantly higher. This discrepancy likely results from earlier assessment of visual acuity from the time of presentation. Furthermore, the incidence of decreased visual acuity (77%) was consistent with the subjective complaints of blurred vision (75%) within the same population group. Therefore, it is important for physicians who manage facial trauma to be familiar with visual acuity testing.
Visual acuity alone is an unreliable predictor of severe ocular injuries for several reasons. First, patients with pre-existing low vision, hyperopia, or presbyopia may perform poorly on evaluation with near cards. In trauma-related injuries, cooperation with visual acuity testing may be limited due to agitation, intoxication, pain, or intracranial injuries. Alternatively, severe ocular injuries may coincide with good visual acuity but have other symptoms (e.g., diplopia, floaters, photophobia, or photopsias), which are frequently undiscovered by non-ophthalmologists. To further complicate the reliance of visual acuity as a predictor of severe ocular injuries, transiently decreased visual acuity may also occur with mild to moderate ocular conditions, such as corneal abrasion, traumatic iridocyclitis, or traumatic mydriasis. These injuries could cause an early decrease in visual acuity and may be managed by experienced non-ophthalmologist practitioners in the emergency room setting with a low risk of permanent visual loss.
Data on pain with ocular movement associated with major ocular injuries are inconsistent. In one study on pediatric orbital fractures, 95.6% of patients with extraocular muscle incarceration had pain with eye movement.25 In a different study, only one out of 75 patients with ocular injuries associated with orbital fractures reported pain with globe movement.8 In our study, 31% of patients with severe ocular injuries reported movement-induced pain. The incidence of muscle entrapment was 2.5% in our study. However, muscle entrapment was found in 69% of patients with movement-induced pain. Our findings are consistent with those of previous studies, demonstrating pain with eye movement is predictive of muscle entrapment. However, we are unable to definitively conclude whether pain with eye movement is an independent predictor of severe ocular injury, as close to one-third of patients with this subjective complaint did not have muscle entrapment.
Extraocular motility limitation is an important exam finding associated with facial trauma, and the incidence ranges from 9.8 to 84%.15, 16, 25–27 Deficit of EOM may indicate muscular contusion/injury, muscle entrapment, neurologic injury, or intraorbital hemorrhage/contusion. Numerous studies have reported EOM restriction as a sign of muscle entrapment.15, 16, 25–27 Lane et al reported that 43% of pediatric orbital floor fractures were not associated with grossly visible signs, resulting in “white-eyed blowout fractures” that were often uncovered with careful extraocular motility examinations.26 The incidence of EOM limitation reported in our study is consistent with previous reports in the literature. Among the patients with severe ocular injuries, 65% had EOM limitations. However, muscle entrapment only accounted for 18% of this subgroup of patients with EOM limitations, suggesting that orbital edema, compartment syndrome with retrobulbar hemorrhage, and/or muscle contusion are rather prevalent in the setting severe ocular injuries. The incidence of EOM limitation was twice as high in patients with severe ocular injuries compared to those with non-severe ocular injuries. Our study is the first to demonstrate that EOM limitation is significantly increased in patients with severe ocular injuries, which provides evidence for using EOM limitation as a screening indicator for concurrent severe ocular trauma.
Unlike previous studies evaluating subjective and objective parameters independently, our study proposes a method to predict severe ocular trauma in orbital fracture patients. Based on our data, we have determined that among the 7 signs and symptoms evaluated, the combination of 2 or more of the 4 parameters blurry vision, eye-movement-induced pain, decreased visual acuity, or EOM restriction has a 91% sensitivity and 86% specificity in identifying severe ocular injuries.
There are several limitations to this study. First, this is a retrospective study. Baseline ophthalmologic evaluations were not available for patients included in this study. In addition, our study excluded patients who were incapable of cooperating with our examination; therefore, these predictors will not apply to this population. Finally, this study does not track the long-term visual outcomes of these patients. A prospective study will be needed to evaluate our criteria and confirm our findings.
The goal of this study was to establish a simple guideline for non-ophthalmologist physicians to determine the need for an urgent ophthalmology consultation for facial fracture patients on initial presentation. Our multifactorial screening tool may be better at identifying severe ocular injuries as compared to guidelines in the literature. In cooperative patients with acute orbital wall fractures, the presence of 2 or more of the 4 signs/symptoms of blurry vision, pain with eye movements, decreased visual acuity, or EOM restriction has a relatively high sensitivity and specificity for detecting concurrent severe eye injuries.
Financial Support:
Supported in part by National Eye Institute Vision Core Grant P30EY028102 and the Hermann Eye Fund
Footnotes
Previous Meeting Presentation: Presented at the 2017 Annual Meeting of the Association for Research in Vision and Ophthalmology on May 11, 2017, in Baltimore, MD.
Disclosures: None
References
- 1.Cook T Ocular and periocular injuries from orbital fractures. J Am Coll Surg 2002;195:831–4. [DOI] [PubMed] [Google Scholar]
- 2.Holt GR and Holt JE Incidence of eye injuries in facial fractures: an analysis of 727 cases. Otolaryngol Head Neck Surg 1983;91:276–9. [DOI] [PubMed] [Google Scholar]
- 3.Kreidl KO, Kim DY and Mansour SE Prevalence of significant intraocular sequelae in blunt orbital trauma. Am J Emerg Med 2003;21:525–8. [DOI] [PubMed] [Google Scholar]
- 4.Petro J, Tooze FM, Bales CR and Baker G Ocular injuries associated with periorbital fractures. J Trauma 1979;19:730–3. [DOI] [PubMed] [Google Scholar]
- 5.al-Qurainy IA, Dutton GN, Ilankovan V, et al. Midfacial fractures and the eye: the development of a system for detecting patients at risk of eye injury--a prospective evaluation. Br J Oral Maxillofac Surg 1991;29:368–9. [DOI] [PubMed] [Google Scholar]
- 6.al-Qurainy IA, Stassen LF, Dutton GN, et al. The characteristics of midfacial fractures and the association with ocular injury: a prospective study. Br J Oral Maxillofac Surg 1991;29:291–301. [DOI] [PubMed] [Google Scholar]
- 7.Andrews BT, Jackson AS, Nazir N, et al. Orbit fractures: Identifying patient factors indicating high risk for ocular and periocular injury. Laryngoscope 2016;126 Suppl 4:S5–11. [DOI] [PubMed] [Google Scholar]
- 8.Chow J, Parthasarathi K, Mehanna P and Whist E Primary Assessment of the Patient With Orbital Fractures Should Include Pupillary Response and Visual Acuity Changes to Detect Occult Major Ocular Injuries. J Oral Maxillofac Surg 2018;76:2370–75. [DOI] [PubMed] [Google Scholar]
- 9.Yadav K, Cowan E, Wall S and Gennis P Orbital fracture clinical decision rule development: burden of disease and use of a mandatory electronic survey instrument. Acad Emerg Med 2011;18:313–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freeman E and Moisen G A comparison of the performance of threshold criteria for binary classification in terms of predicted prevalence and kappa. Ecological Modeling 2008;217:48–58. [Google Scholar]
- 11.Amrith S, Saw SM, Lim TC and Lee TK Ophthalmic involvement in cranio-facial trauma. J Craniomaxillofac Surg 2000;28:140–7. [DOI] [PubMed] [Google Scholar]
- 12.Ashar A, Kovacs A, Khan S and Hakim J Blindness associated with midfacial fractures. J Oral Maxillofac Surg 1998;56:1146–50; discussion 51. [DOI] [PubMed] [Google Scholar]
- 13.Gossman MD, Roberts DM and Barr CC Ophthalmic aspects of orbital injury. A comprehensive diagnostic and management approach. Clin Plast Surg 1992;19:71–85. [PubMed] [Google Scholar]
- 14.Jayamanne DG and Igillie RF Orbital blow-out fractures: long-term visual outcome of associated ocular injuries. J Accid Emerg Med 1995;12:273–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jayamanne DG and Gillie RF Do patients with facial trauma to the orbito-zygomatic region also sustain significant ocular injuries? J R Coll Surg Edinb 1996;41:200–3. [PubMed] [Google Scholar]
- 16.Miller GR and Tenzel RR Ocular complications of midfacial fractures. Plast Reconstr Surg 1967;39:37–42. [DOI] [PubMed] [Google Scholar]
- 17.Crumley RL, Leibsohn J, Krause CJ and Burton TC Fractures of the orbital floor. Laryngoscope 1977;87:934–47. [DOI] [PubMed] [Google Scholar]
- 18.Fulcher TP and Sullivan TJ Orbital roof fractures: management of ophthalmic complications. Ophthalmic Plast Reconstr Surg 2003;19:359–63. [DOI] [PubMed] [Google Scholar]
- 19.He D, Blomquist PH and Ellis E 3rd. Association between ocular injuries and internal orbital fractures. J Oral Maxillofac Surg 2007;65:713–20. [DOI] [PubMed] [Google Scholar]
- 20.Shere JL, Boole JR, Holtel MR and Amoroso PJ An analysis of 3599 midfacial and 1141 orbital blowout fractures among 4426 United States Army Soldiers, 1980–2000. Otolaryngol Head Neck Surg 2004;130:164–70. [DOI] [PubMed] [Google Scholar]
- 21.Mellema PA, Dewan MA, Lee MS, et al. Incidence of ocular injury in visually asymptomatic orbital fractures. Ophthalmic Plast Reconstr Surg 2009;25:306–8. [DOI] [PubMed] [Google Scholar]
- 22.Barry C, Coyle M, Idrees Z, et al. Ocular findings in patients with orbitozygomatic complex fractures: a retrospective study. J Oral Maxillofac Surg 2008;66:888–92. [DOI] [PubMed] [Google Scholar]
- 23.Riaz N, Chatha AA, Warraich RA, et al. Ophthalmic injuries in orbito-zygomatic fractures. J Coll Physicians Surg Pak 2014;24:649–52. [PubMed] [Google Scholar]
- 24.Kim YS, Kim JH and Hwang K The Frequency of Decreased Visual Acuity in Orbital Fractures. J Craniofac Surg 2015;26:1581–3. [DOI] [PubMed] [Google Scholar]
- 25.Yoo YJ, Yang HK, Kim N and Hwang JM Pediatric orbital wall fractures: Prognostic factors of diplopia and ocular motility limitation. PLoS One 2017;12:e0184945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lane K, Penne RB and Bilyk JR Evaluation and management of pediatric orbital fractures in a primary care setting. Orbit 2007;26:183–91. [DOI] [PubMed] [Google Scholar]
- 27.Roh JH, Jung JW and Chi M A clinical analysis of bilateral orbital fracture. J Craniofac Surg 2014;25:388–92. [DOI] [PubMed] [Google Scholar]


