Abstract
Background:
While bariatric surgery is an effective treatment for obesity, utilization of bariatric procedures in older adults remains low. Previous work reported higher morbidity in older patients undergoing bariatric surgery. However, the generalizability of this data to contemporary septuagenarians is unclear.
Objectives:
We sought to evaluate differences in 30-day outcomes, 1-year weight loss, and comorbidity remission after bariatric surgery among three age groups: < 45 years old (y.o.), 45–69 y.o., and ≥ 70 y.o.
Setting:
Statewide quality improvement collaborative.
Methods:
Using a large quality improvement collaborative, we identified patients undergoing sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB) between 2006 – 2018. Patients were categorized into three age cohorts: <45 y.o., 45–69 y.o., and ≥ 70 y.o. We used multivariable logistic regression models to evaluate the association between age cohorts and 30-day outcomes, 1-year weight loss, and comorbidity remission.
Results:
We identified 641 septuagenarians who underwent SG (68.5%) or RYGB (31.5%). Compared to 45–69 y.o., septuagenarians had higher rates of hemorrhage (5.1% vs 3.1%; p=0.045) following RYGB and higher rates of leak/perforation (0.9% vs 0.3%; p=0.044) following SG. Compared to younger patients, septuagenarians lost less of their excess weight, losing 64.8% following RYGB and 53.8% following SG. Remission rates for diabetes and obstructive sleep were similar for ≥70 y.o, and 45–69 y.o.
Conclusions:
Bariatric surgery in septuagenarians results in substantial weight loss and comorbidity remission with an acceptable safety profile. Surgeons with self-imposed age limits should consider broadening their selection criteria to include patients ≥70 y.o.
Keywords: Bariatric Surgery, Health Policy, Outcomes, Elderly, Older Adult, Sleeve Gastrectomy, Roux-en-Y Gastric Bypass
INTRODUCTION
Bariatric surgery is the most effective treatment for obesity.1–4 While older adults are equally affected by obesity compared to younger patients, the utilization of bariatric procedures in older adults remains low.4,5 Recent work demonstrated a similar safety profile and effectiveness of bariatric surgery in older adults compared to younger patients; however older adult often was defined as patients age 55 and older.6–8 The generalizability to all older patients remains unclear. As life expectancy increases in the US and the prevalence of obesity in the overall population continues to rise, understanding the current safety and effectiveness of bariatric surgery in patients 70 years and older is particular salient.
Prior studies showed that bariatric surgery in this population resulted in significantly increased morbidity and mortality.9–11 However, many of these studies evaluated patients after open Roux-en-Y gastric bypass and may not be applicable to the current patients undergoing minimally invasive procedures and sleeve gastrectomy. It is possible that bariatric surgery in patients greater than 70 years old is contraindicated due to increased morbidity or poor clinical outcomes. On the other hand, with the increasing use of less invasive procedures, bariatric surgery may be safe and effective and in this population. Given the paucity of data on patients older than 70, it remains difficult to assess and counsel septuagenarians on the potential risks and benefits of bariatric surgery.
In this context, we used clinical registry data from a statewide quality improvement collaborative to assess differences in perioperative and 1-year outcomes for patients age <45 years old, 45–69 years old, and 70 years of age and older undergoing bariatric surgery.
METHODS
Data Source and Population
This study utilized data from the Michigan Bariatric Surgery Collaborative (MBSC), a statewide clinical registry that includes information from >95% of patients undergoing bariatric surgery in the state of Michigan. The MBSC, described in detail in previous work, is a consortium which includes 42 hospitals and employs trained data abstractors that perform extensive chart review regarding patients’ demographics, comorbidities, perioperative care and process details, and postoperative outcomes for multiple bariatric operations.1,12 Patients are surveyed preoperatively and annually after surgery to assess information that includes weight loss, medication use and health-related quality of life. Use of the secondary, deidentified data were deemed exempt by the institutional review board of the University of Michigan.
We identified all patients age ≥ 18 years old in the MBSC registry who underwent primary sleeve gastrectomy (SG) or Roux-en-Y gastric bypass (RYGB) from June 13, 2006 and April 4, 2018. Patients undergoing revision surgery were excluded from the analysis.
Outcome Measures
The primary outcome for this study was 30-day postoperative complication rates, as determined from patient medical records via direct, clinical chart abstraction. Severe complications included intraabdominal abscess formation (requiring drainage/reoperation), bowel obstruction/hernia (requiring operation), anastomotic leak, bleeding (transfusion >4 units), respiratory failure (requiring intubation for at least 2 days or tracheostomy), renal failure (requiring in-hospital dialysis or long-term dialysis), wound infection/dehiscence, VTE, myocardial infarction/cardiac arrest, and death.
Secondary outcomes included postoperative healthcare resource utilization (Emergency Department (ED) visits, hospital readmissions, and reoperation) within 30 days of the index operation. Percent total body weight loss (%TBWL) and percent excess body weight loss (%EBWL) at 1 year after the primary operation were also captured through chart abstraction. Additionally, we evaluated comorbidity remission, defined as treatment discontinuation at 1-year after surgery. Patients were queried on each survey whether they currently used insulin, oral diabetes medications, high blood pressure medications, cholesterol-lowering drugs, or treatment for sleep apnea (CPAP, BiPAP, or other). A list of common medications for each category was included in the patient survey. Comorbidity treatment discontinuation was defined as a patient who reported use of a medication/treatment class on the preoperative MBSC survey and denied use on the 1-year postoperative survey.
Study Variables
Age at the time of primary operation was collected for all patients. All included patients undergoing primary RYBG or SG were assigned to one of three age categories, (i) <45 years of age, (ii) 45–69 years of age, or (iii) ≥ 70 years of age. The age groups were selected based off of prior studies and previously polled data from practicing surgeons in the MBSC and SAGES Foregut Surgical Collaboration Facebook group in which surgeons most commonly reported 70 years of age as the upper limit for offering bariatric surgery.13
Data regarding demographic information (such as gender, race, and body mass index (BMI)) and health comorbid conditions (such as diabetes, hypertension, coronary artery disease, cerebrovascular disease and serious lung disease) were collected for all patients.
Statistical Analysis
Pearson χ2 test and one-way ANOVA test were used to compare baseline characteristics across age categories. We then utilized Pearson χ2 tests to assess whether there was an association between unadjusted complications and the assigned age-cohort for RYGB and SG separately. For risk adjustment, we performed a stepwise regression to evaluate the covariate-adjusted association between assigned age-cohort and the primary study outcomes for each operation separately. Adjustment covariates included gender, race, preoperative BMI, insurance payer, cardiovascular disease (hypertension, peripheral vascular disease, or other cardiovascular disease), diabetes (type 1, type 2, insulin-dependent, or other), lung disease, liver disease, musculoskeletal disorder, psychological disorder (depression, anxiety, bipolar, or other), GERD, kidney failure, sleep apnea, urinary incontinence, venous thromboembolism, the total number of comorbidities, and the operative technique (open versus minimally invasive). Statistically significant factors in univariate analysis were included as risk-adjusted variables.
We included the risk-adjusted variables and assigned age category variable in a multivariable logistic regression model as predictor variables and with complications, postoperative resource utilization, and comorbidity treatment (yes vs no) as the outcomes of interest. %EBWL and %TBWL 1-year after surgery were compared using a one-way ANOVA test. Two-sided p values less than 0.05 were considered statistically significant. All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, North Carolina).
RESULTS
We identified 62,561 patients, age 18–81 years, undergoing primary RYGB or SG during the study period. Of these patients, 37,099 (59%) underwent SG and 25,462 (41%) underwent RYGB. This cohort included 30,243 patients that were less than 45 years of age, 31,677 patients age 45 to 69 years old, and 641 patients age 70 years or older (Table 1).
Table 1.
Patient baseline characteristics by age
| < 45 years old | 45 – 69 years old | ≥70 years old | P value | |
|---|---|---|---|---|
| Patients, No. | 30,243 | 31,677 | 641 | |
| Age, mean (SD), years | 35.9 (11.6) | 54.7 (6.4) | 72.4 (2.0) | <0.001 |
| Age, median (IQRa), years | 36.9 (31.7–41.0) | 54.1 (49.3–59.4) | 71.9 (70.8–73.5) | <0.001 |
| Procedure Type (%) | ||||
| Roux-en-Y Gastric Bypass | 39.7 | 41.9 | 31.5 | <0.001 |
| Sleeve Gastrectomy | 60.3 | 58.1 | 68.5 | <0.001 |
| Male (%) | 18.4 | 24.3 | 34.0 | <0.001 |
| Starting BMIb (%) | ||||
| <40 | 11.1 | 17.2 | 24.0 | <0.001 |
| 40–49 | 49.0 | 50.3 | 52.7 | 0.002 |
| 50–59 | 29.6 | 25.1 | 20.8 | <0.001 |
| ≥60 | 10.3 | 7.4 | 2.5 | <0.001 |
| Mean (SD) | 49.0 (8.7) | 47.3 (8.1) | 45.1 (6.8) | <0.001 |
| Race/ethnicity (%) | ||||
| White, Non-Hispanic | 71.5 | 80.2 | 91.7 | <0.001 |
| Black, Non-Hispanic | 18.4 | 13.0 | 2.8 | <0.001 |
| Other or Multiracial | 10.0 | 6.9 | 5.5 | <0.001 |
| Comorbidities (%) | ||||
| Diabetes | 23.4 | 44.2 | 57.7 | <0.001 |
| Hypertension | 34.9 | 69.9 | 88.8 | <0.001 |
| Hyperlipidemia | 34.2 | 62.4 | 81.1 | <0.001 |
| Obstructive Sleep Apnea | 38.4 | 55.8 | 61.0 | <0.001 |
| CVDc | 36.5 | 72.1 | 91.3 | <0.001 |
| CADd | 1.7 | 9.6 | 25.4 | <0.001 |
| Serious Lung Disease | 24.7 | 28.4 | 31.5 | <0.001 |
| Anticoagulation Use | 0.1 | 0.1 | 0.3 | 0.005 |
| Total Comorbidities, No. (SD) | 3.8 (2.0) | 5.3 (2.0) | 6.1 (1.7) | <0.001 |
IQR; Inter-Quartile Range (25%−75%),
BMI; Body Mass Index (kg/m2),
CVD; cardiovascular disease,
CAD; coronary artery disease
Patient Characteristics
Table 1 presents baseline characteristics of patients stratified by their age. Compared to the two younger cohorts, patients ≥70 years old were more likely to be male (34.0% vs 24.3% vs 18.4%) and white (91.7% vs 80.2% vs 71.5%) and more likely to have individual comorbidities and a greater total number of comorbidities (6.1 vs 5.3 vs 3.8). Patients 70 years and older were more likely to have a lower BMI at the time of the operation (45.1 vs 47.3 vs 49.0), with 77% having a baseline BMI less than 50. Septuagenarians were also more likely to undergo sleeve gastrectomy (68.5%). Patients in each of the three age cohort were equally as likely to be operated on by a “high-volume surgeon” (surgeon in the top quartile of case volume).
Postoperative Complications
Risk-adjusted 30-day postoperative complications are shown in Table 2. With regard to RYGB, patients <45 years old had a decreased rate of leak/perforation (0.6% vs 1.8%; p=0.017) and hemorrhage (0.6% vs 3.1%; p=0.015) and an increased rate of obstruction (3.0% vs 2.0%; p=0.001) compared to those aged 45–69. Conversely, septuagenarians had a significantly higher rate of any complication (14.6% vs 10.7%; p=0.046) and specifically hemorrhage (5.1% vs 3.1%; p=0.045) compared to patients 45–69. However, there was no significant difference in severe complications or mortality for patients ≥70 undergoing RYGB compared to those 45–69 years of age.
Table 2.
30-day risk-adjusted perioperative complications and healthcare resource utilization by age
| < 45 years old | 45 – 69 years old | ≥70 years old | ||||
|---|---|---|---|---|---|---|
| Rate (%) |
OR | Rate (%) |
OR | Rate (%) |
OR | |
| Roux-en-Y Gastric Bypass | ||||||
| Patients, No. | 12014 | 13267 | 202 | |||
| MISa Technique | 100 | 100 | 100 | |||
| Any Complication | 11.2 | 1.06 (0.97, 1.16) | 10.7 | Ref. | 14.6 | 1.46* (1.01, 2.11) |
| Severe Complication | 3.0 | 0.88 (0.75, 1.03) | 3.4 | Ref. | 4.6 | 1.42 (0.78, 2.57) |
| Leak or Perforation | 0.6 | 0.66* (0.47, 0.93) | 0.8 | Ref. | 1.8 | 2.49 (0.90, 6.89) |
| Hemorrhage | 2.6 | 0.81* (0.69, 0.96) | 3.1 | Ref. | 5.1 | 1.77* (1.01, 3.08) |
| VTEb | 0.4 | 0.73 (0.47, 1.13) | 0.5 | Ref. | 0.7 | 1.69 (0.40, 7.10) |
| Infection | 3.4 | 1.05 (0.90, 1.22) | 3.3 | Ref. | 2.5 | 0.76 (0.34, 1.74) |
| Obstruction | 3.0 | 1.35* (1.12, 1.61) | 2.0 | Ref. | 1.9 | 0.88 (0.32, 2.39) |
| Mortality | 0.09 | 0.49 (0.22, 1.13) | 0.16 | Ref. | 0.31 | 2.16 (0.28, 16.54) |
| ED Visitd | 10.6 | 1.34* (1.22, 1.48) | 8.5 | Ref. | 9.7 | 1.11 (0.71, 1.75) |
| Readmission | 5.8 | 1.21* (1.07, 1.36) | 5.0 | Ref. | 5.3 | 1.03 (0.58, 1.82) |
| Reoperation | 2.3 | 1.00 (0.83, 1.20) | 2.3 | Ref. | 3.0 | 1.33 (0.62, 2.85) |
| Sleeve Gastrectomy | ||||||
| Patients, No. | 18229 | 18410 | 439 | |||
| MISa Technique, % | 99.9 | 99.8 | 99.5 | |||
| Any Complication | 5.5 | 1.09 (0.98, 1.20) | 5.2 | Ref. | 7.4 | 1.47* (1.06, 2.04) |
| Severe Complication | 1.6 | 1.11 (0.93, 1.33) | 1.5 | Ref. | 2.7 | 1.83* (1.09, 3.07) |
| Leak or Perforation | 0.4 | 1.26 (0.85, 1.86) | 0.3 | Ref. | 0.9 | 2.86* (1.01, 8.07) |
| Hemorrhage | 0.9 | 0.65* (0.52, 0.82) | 1.3 | Ref. | 1.9 | 1.53 (0.88, 2.67) |
| VTEb | 0.4 | 0.96 (0.67, 1.36) | 0.4 | Ref. | 0.6 | 1.53 (0.47, 4.91) |
| Infection | 1.2 | 1.15 (0.93, 1.43) | 1.0 | Ref. | 1.8 | 1.81 (0.92, 3.59) |
| Obstruction | 0.5 | 1.41 (0.98, 2.01) | 0.4 | Ref. | 0.2 | 0.53 (0.07, 3.84) |
| Mortality | 0.02 | 0.22* (0.06, 0.77) | 0.09 | Ref. | 0.00 | 0.00 |
| ED Visitc | 8.7 | 1.46* (1.34, 1.60) | 6.5 | Ref. | 7.8 | 1.15 (0.81, 1.62) |
| Readmission | 3.8 | 1.34* (1.18, 1.52) | 3.0 | Ref. | 4.6 | 1.54* (1.03, 2.31) |
| Reoperation | 0.9 | 1.23 (0.96, 1.58) | 0.8 | Ref. | 2.0 | 2.74* (1.50, 5.03) |
p <0.05 compared with risk-adjusted complication rate of patients age 45–69 years old,
MIS; minimally invasive,
VTE; venous thromboembolism,
ED; emergency department
As for SG, patients <45 years old had a decreased rate of hemorrhage (0.9% vs 1.3%; p<0.001) and mortality (0.02% vs 0.09%; p=0.019) compared to those 45–69 years of age. (Table 2) On the other hand, patients ≥70 years old had an increased rate of any complication (7.4% vs 5.2%; p=0.021), severe complications (2.7% vs 1.5%; p=0.021), and specifically leak/perforation (0.9% vs 0.3%; p=0.044) compared to patients 45–69 years old, as well as higher rates of these complications compared to patients less than 45 years of age. As with RYGB, mortality was not significantly higher in patients 70 years and older (45–69 years: 0.09% vs ≥70 years: 0.00%; p=0.999). (Figure 1a–b)
Figure 1.
Risk-adjusted 30-day complication rate by age.
(a) Roux-en-Y gastric bypass
(b) sleeve gastrectomy.
*p<0.05 compared with risk-adjusted complication rate of 45–69-year old.
Postoperative Healthcare Resource Utilization
Septuagenarians who underwent RYGB did not have higher rates of postoperative ED visits (9.7% vs 8.5; p=0.650), readmission (5.3% vs 5.0%; p=0.923), or reoperation (3.0% vs 2.3%; p=0.471) compared to patients age 45–69 years. (Table 2) Patients age 70 and older who received a SG were more likely to be readmitted to the hospital (4.6% vs 3.0%; p=0.035) and undergo a reoperation (2.1% vs 0.8%; p=00.001) than patients age 45–69. The youngest patients (age <45 years old) had higher rates of ED visits and readmission for both RYGB and SG compared to patients age 45–69 years old.
Among all patients who underwent bariatric surgery, 54% had complete 1-year postoperative data (<45 years of age: 50.0%, 45–69 years of age: 57.6%, 70 years of age and older: 61.0%) and were included in analyses regarding weight loss and comorbidity remission.
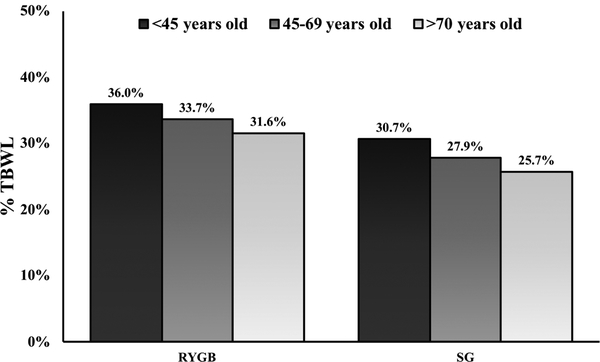
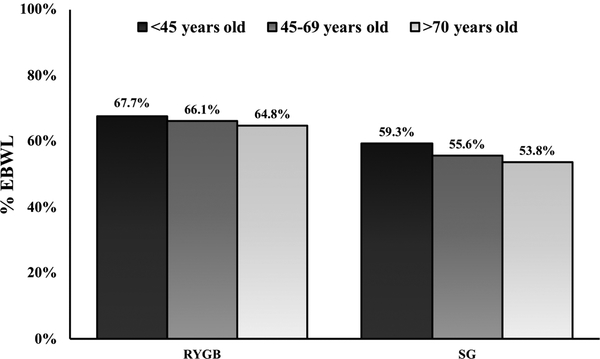
Weight Loss
Elderly patients had lower 1-year weight loss than the younger cohorts for both RYGB and SG (Figure 2). For the <45-year old, 45–69 year old, and ≥70 year old patients total weight loss after RYGB was 36.0%, 33.7% and 31.6%, (p<0.001) and excess body weight loss was 67.7%, 66.1%, and 64.8%, (p<0.001). (Figure 2a) Following SG, total weight loss was 30.7%, 27.9%, and 25.7%, (p<0.001) and excess body weight loss was 59.3%, 55.6%, and 53.8%, (p<0.001). (Figure 2b)
Figure 2.
Mean weight loss 1-year after Roux-en-Y gastric bypass (RYGB) or sleeve gastrectomy (SG) by age.
(a) % total body weight loss (%TBWL)
(b) % excess body weight loss (%EBWL).
Comorbidity Remission
Patients less than age 45 had higher rates of remission for all comorbidities compared to those 45–69 years old. (Table 3) For both RYGB and SG, patients 70 years and older had similar rates of remission for diabetes (oral medications: RYGB 90.9% vs 80.1%, p=0.632; SG 74.1% vs 76.9%, p=0.232), obstructive sleep apnea (RYGB 51.6% vs 62.4%, p=0.083; SG 48.6% vs 51.8%, p=0.369), and hyperlipidemia (RGYB 63.3% vs 67.8%, p=0.164; SG 42.4% vs 52.0%, p=0.053) when compared to the 45–69 year old cohort. However, remission of hypertension was lower after both RYGB (45.7% vs 53.6%; p=0.023) and SG (43.4% vs 50.4%; p=0.022) for the older population.
Table 3.
1-year postoperative comorbidity remission by age
| < 45 years old | 45 – 69 years old | ≥70 years old | ||||
|---|---|---|---|---|---|---|
| Rate (%) |
ORa | Rate (%) |
OR | Rate (%) |
OR | |
| Roux-en-Y Gastric Bypass | ||||||
| Diabetes: Oral medications (N= 3149) |
85.3 | 1.63* (1.28, 2.07) | 80.1 | Ref. | 90.9 | 1.20 (0.56, 2.57) |
| Diabetes: Insulin (N=1590) |
75.0 | 1.25 (0.93, 1.69) | 71.6 | Ref. | 67.0 | 0.76 (0.38, 1.53) |
| Obstructive Sleep Apnea (N=3523) |
72.9 | 1.90* (1.59, 2.26) | 62.4 | Ref. | 51.6 | 0.59 (0.32, 1.07) |
| Hyperlipidemia (N=3627) |
77.3 | 2.04* (1.64, 2.53) | 67.8 | Ref. | 63.3 | 0.68 (0.40, 1.17) |
| Hypertension (N=5490) |
68.9 | 2.23* (1.94, 2.56) | 53.6 | Ref. | 45.7 | 0.59* (0.37, 0.93) |
| Sleeve Gastrectomy | ||||||
| Diabetes (oral medications) (N=3868) |
82.0 | 1.62* (1.32, 1.99) | 76.9 | Ref. | 74.1 | 0.75 (0.47, 1.20) |
| Diabetes (insulin) (N=1480) |
67.2 | 1.40* (1.04, 1.88) | 61.9 | Ref. | 67.9 | 0.84 (0.46, 1.53) |
| Obstructive Sleep Apnea (N=5467) |
63.4 | 1.86* (1.63, 2.12) | 51.8 | Ref. | 48.6 | 0.83 (0.55, 1.24) |
| Hyperlipidemia (N=4639) |
63.2 | 1.89* (1.61, 2.23) | 52.0 | Ref. | 42.4 | 0.68 (0.46, 1.01) |
| Hypertension (N=8106) |
64.3 | 2.03* (1.82, 2.27) | 50.4 | Ref. | 43.4 | 0.69* (0.50, 0.95) |
p <0.05 compared with risk-adjusted complication rate of patients age 45–69 years old,
OR; odds ratio
DISCUSSION
This study of patients 70 years of age and older undergoing bariatric surgery has two key findings. First, we found that patients age ≥70 have higher rates of overall complications following RYGB and SG and higher rates of severe complications and readmission following SG when compared to younger patients. While statistically significant, the absolute rates were still low with no significant increased risk of mortality in septuagenarians. This implies that while age ≥ 70 years is associated with a higher risk of morbidity and resource utilization, it is not clinically prohibitive in this population as the serious complication rate remains <5% and there is no difference in mortality compared to younger patients. Second, we found that despite modestly lower weight loss in elderly patients, they achieved similar rates of remission for diabetes, obstructive sleep apnea, and hyperlipidemia compared to patients age 45–69 years old. The overall substantial weight loss and comorbidity remission, combined with an acceptable safety profile, highlights the potential effectiveness of bariatric surgery in patients 70 years and older.
Advanced age was initially viewed as a relative contraindication to bariatric surgery with concerns of increased morbidity and mortality.9–11,14 In more recent years the safety profile of bariatric surgery in “elderly” patients has been more promising. However, the definition of advanced age used varies substantially across studies, ranging from >55 years to >75 years old.6–8,15–20 A number of studies specifically evaluated patients ≥70 years of age and reported no difference in postoperative complications.19,21–23 However, these findings are limited by cohorts of less than 50 patients and calls into question the power to detect differences in operative outcomes between septuagenarians and younger patients. Our study is the largest analysis of septuagenarians undergoing bariatric surgery and shows that patients ≥70 years old undergoing RYGB and SG do have significantly higher rates of complications compared to younger patients. However, the absolute differences in morbidity are modest and there was no significant difference in mortality, suggesting that advanced age alone should not be considered a contraindication to surgery.
We found that weight loss was modestly lower in septuagenarian following RGYB and SG compared to their younger counterparts. This finding echoes results of previous studies which reported lower weight loss in older adults.8,13,18,20,24,25. For example, Sugerman et al demonstrated that patients >60 years old lost 57% of EBWL compared to 65% in younger patients (p<0.01) and a more recent analysis of the Ontario Bariatric Registry replicated this finding.18,25 While septuagenarians lost less weight than younger patients, it is worthwhile to note that bariatric surgery remains the most effective treatment of obesity in this population and comparative weight loss across age groups may not be the optimal measure of procedural value.
While weight loss remains a key focus of bariatric surgery, these procedures offer other substantial health benefits for patients, including comorbidity remission, improved pain, and increased physical function.18,26 In our analysis septuagenarians achieved similar rates of treatment discontinuation for diabetes, obstructive sleep apnea, and hyperlipidemia compared to patients age 45–69 years old. The current literature on comorbidity remission is comparable to our findings with older adults consistently described as having similar or only slightly decreased rates of comorbidity remission compared to their younger counterparts.18,24 Given substantial weight loss and comorbidity remission in patients 70 years and older, our study suggests that bariatric surgery in this population is effective.
This study has several limitations. First, we only included patients from a single state, and the results may not be fully generalizable to patients in other states or countries. However, the study population in our analysis reflects those of other studies, and the demographics are similar to the general population undergoing bariatric surgery in the United States. Second, we evaluated 30-day postoperative complications and thus were not able to evaluate the impact of age on late complications such as stricture or marginal ulcer. Nonetheless, the risk of early postoperative complications often drives decisions of surgical candidacy. Third, we used treatment discontinuation to define comorbidity remission as opposed to more objective criteria, such as hemoglobin A1c level to evaluate diabetes, and this may have affected the accuracy of our results. Finally, patients over 70 years of age accounted for a very small percentage of those undergoing bariatric surgery in our registry and we were unable to account for mortality beyond 30-day, potentially leading to issues of selection bias. However, this study is the largest population-based study to evaluate outcomes in this patient group.
Despite these limitations, our findings demonstrate that bariatric surgery in patients ≥70 years old results in substantial weight loss and comorbidity remission and has an acceptable safety profile, with a serious complication rate of <5% and mortality rate similar to younger patients. As a result of this work, bariatric surgery programs and surgeons with self-imposed age limits should consider broadening their patient selection criteria to include patients ≥70 years old after careful evaluation to ensure their appropriateness for surgery. Identifying which elderly patients will benefit from surgical intervention will be critical, and providers may find utility in evaluating patients physiologic age through measures of mobility, frailty, and potential longevity, as opposed to using chronologic age as a threshold. Notably, all septuagenarians deemed as appropriate surgical candidates should still be counseled that, despite favorable outcomes, they have an increased likelihood of experiencing a complication with either RYGB or SG. Ultimately, given the well documented benefits and safety of bariatric surgery, further attention to advocacy and expanding adoption of this beneficial treatment should be pursued, with inclusion of elderly patients in these efforts.
Highlights.
Septuagenarians experience more postoperative complications; however, serious complications are <5%.
Septuagenarians lose 60% of their excess body weight after bariatric surgery.
Septuagenarians have similar rates of postoperative diabetes remission compared to patients 45–69-year-old.
Bariatric surgeons should not exclude patients ≥70 years old based on age alone.
Conflicts of Interest and Sources of Funding Research Support:
Margaret E Smith is supported by funding from the National Institute of Health Obesity Surgery Scientist Training Grant (T32-DK-108740). Dr. Daniel Bacal has no disclosures or conflicts of interest. Dr. Oliver Varban, Dr. Jonathan Finks, Dr. Arthur Carlin, and Dr. Amir Ghaferi obtain salary support from Blue Cross Blue Shield for participating in quality improvement initiates and the Executive Committee of the Michigan Bariatric Surgery Collaborative.
Conflicts of Interest: Dr. Oliver Varban, Dr. Jonathan Finks, Dr. Arthur Carlin, and Dr. Amir Ghaferi obtain salary support from Blue Cross Blue Shield for participating in quality improvement initiates and the Executive Committee of the Michigan Bariatric Surgery Collaborative. Dr. Margaret Smith, Mr. Aaron Bonham, and Dr. Daniel Bacal have nothing to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Birkmeyer NJ, Dimick JB, Share D, et al. Hospital complication rates with bariatric surgery in Michigan. Jama. 2010;304(4):435–442. [DOI] [PubMed] [Google Scholar]
- 2.Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg. 2014;149(3):275–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Courcoulas AP, Yanovski SZ, Bonds D, et al. Long-term outcomes of bariatric surgery: a National Institutes of Health symposium. JAMA Surg. 2014;149(12):1323–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS data brief. 2015(219):1–8. [PubMed] [Google Scholar]
- 5.Habermann EB, Durham SB, Dorman R, Jarosek S, Virnig BA. Trends in bariatric surgery in Medicare beneficiaries: Data Points # 17 In: Data Points Publication Series. Rockville (MD): Agency for Healthcare Research and Quality (US); 2011. [PubMed] [Google Scholar]
- 6.Dorman RB, Abraham AA, Al-Refaie WB, Parsons HM, Ikramuddin S, Habermann EB. Bariatric surgery outcomes in the elderly: an ACS NSQIP study. J Gastrointest Surg. 2012;16(1):35–44. [DOI] [PubMed] [Google Scholar]
- 7.Gebhart A, Young MT, Nguyen NT. Bariatric surgery in the elderly: 2009–2013. Surg Obes Relat Dis. 2015;11(2):393–398. [DOI] [PubMed] [Google Scholar]
- 8.Lynch J, Belgaumkar A. Bariatric surgery is effective and safe in patients over 55: a systematic review and meta-analysis. Obes Surg. 2012;22(9):1507–1516. [DOI] [PubMed] [Google Scholar]
- 9.Livingston EH, Huerta S, Arthur D, Lee S, De Shields S, Heber D. Male gender is a predictor of morbidity and age a predictor of mortality for patients undergoing gastric bypass surgery. Ann Surg. 2002;236(5):576–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pajecki D, Santo MA, Joaquim HD, et al. Bariatric Surgery in the elderly: results of a mean follow-up of five years. Arq Bras Cir Dig.. 2015;28 Suppl 1:15–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scozzari G, Passera R, Benvenga R, Toppino M, Morino M. Age as a long-term prognostic factor in bariatric surgery. Ann Surg. 2012;256(5):724–728; discussion 728–729. [DOI] [PubMed] [Google Scholar]
- 12.Scally CP, Varban OA, Carlin AM, Birkmeyer JD, Dimick JB. Video ratings of surgical skill and late outcomes of bariatric surgery. JAMA Surg. 2016;151(6):e160428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Contreras JE, Santander C, Court I, Bravo J. Correlation between age and weight loss after bariatric surgery. Obes Surg. 2013;23(8):1286–1289. [DOI] [PubMed] [Google Scholar]
- 14.Sosa JL, Pombo H, Pallavicini H, Ruiz-Rodriguez M. Laparoscopic gastric bypass beyond age 60. Obes Surg. 2004;14(10):1398–1401. [DOI] [PubMed] [Google Scholar]
- 15.Chow A, Switzer NJ, Gill RS, et al. Roux-en-Y gastric bypass in the elderly: a systematic review. Obes Surg. 2016;26(3):626–630. [DOI] [PubMed] [Google Scholar]
- 16.Flum DR, Belle SH, King WC, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361(5):445–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giordano S, Victorzon M. Bariatric surgery in elderly patients: a systematic review. Clin Interv Aging. 2015;10:1627–1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaplan U, Penner S, Farrokhyar F, et al. Bariatric surgery in the elderlyi is associated with similar surgical risks and significant long-term health benefits. Obes Surg. 2018;28(8):2165–2170. [DOI] [PubMed] [Google Scholar]
- 19.Nor Hanipah Z, Punchai S, Karas LA, et al. The Outcome of Bariatric Surgery in Patients Aged 75 years and Older. Obes Surg. 2017. [DOI] [PubMed] [Google Scholar]
- 20.Thereaux J, Poitou C, Barsamian C, Oppert JM, Czernichow S, Bouillot JL. Midterm outcomes of gastric bypass for elderly (aged >/= 60 yr) patients: a comparative study. Surg Obes Relat Dis. 2015;11(4):836–841. [DOI] [PubMed] [Google Scholar]
- 21.Loy JJ, Youn HA, Schwack B, Kurian MS, Fielding GA, Ren-Fielding CJ. Safety and efficacy of laparoscopic adjustable gastric banding in patients aged seventy and older. Surg Obes Relat Dis. 2014;10(2):284–289. [DOI] [PubMed] [Google Scholar]
- 22.Ramirez A, Roy M, Hidalgo JE, Szomstein S, Rosenthal RJ. Outcomes of bariatric surgery in patients >70 years old. Surg Obes Relat Dis. 2012;8(4):458–462. [DOI] [PubMed] [Google Scholar]
- 23.Zaveri H, Surve A, Cottam D, et al. A comparison of outcomes of bariatric surgery in patient greater than 70 with 18 month of follow up. SpringerPlus. 2016;5(1):1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.St Peter SD, Craft RO, Tiede JL, Swain JM. Impact of advanced age on weight loss and health benefits after laparoscopic gastric bypass. Arch Surg. 2005;140(2):165–168. [DOI] [PubMed] [Google Scholar]
- 25.Sugerman HJ, DeMaria EJ, Kellum JM, Sugerman EL, Meador JG, Wolfe LG. Effects of bariatric surgery in older patients. Ann Surg. 2004;240(2):243–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.King WC, Chen JY, Belle SH, et al. Change in Pain and Physical Function Following Bariatric Surgery for Severe Obesity. JAMA. 2016;315(13):1362–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]