Abstract
Background
Reverse shoulder arthroplasty (RSA) is offered to young patients with a failed previous arthroplasty or a cuff-deficient shoulder, but the overall results are still uncertain. We conducted a systematic review of the literature to report the midterm outcomes and complications of RSA in patients younger than 65 years.
Methods
A search of the MEDLINE and Cochrane electronic databases identified clinical studies reporting the results, at a minimum 2-year follow-up, of patients younger than 65 years treated with an RSA. The methodologic quality was assessed with the Methodological Index for Non-Randomized Studies score by 2 independent reviewers. Complications, reoperations, range of motion, functional scores, and radiologic outcomes were analyzed.
Results
Eight articles were included, with a total of 417 patients. The mean age at surgery was 56 years (range, 21-65 years). RSA was used as a primary arthroplasty in 79% of cases and revision of a failed arthroplasty in 21%. In primary cases, the indications were cuff tear arthropathy and/or massive irreparable cuff tear in 72% of cases. The overall complication rate was 17% (range, 7%-38%), with the most common complications being instability (5%) and infection (4%). The reintervention rate was 10% at 4 years, with implant revision in 7% of cases. The mean weighted American Shoulder and Elbow Surgeons score, active forward elevation, and external rotation were 64 points, 121°, and 29°, respectively.
Conclusions
RSA provides reliable clinical improvements in patients younger than 65 years with a cuff-deficient shoulder or failed arthroplasty. The complication and revision rates are comparable to those in older patients.
Keywords: Reverse shoulder arthroplasty, systematic review, young population, functional outcomes, complications, revision arthroplasty
Reverse shoulder arthroplasty (RSA) was initially designed for the treatment of cuff tear arthropathy (CTA)12 but was progressively used to treat different etiologies.4 Although initially implanted in elderly patients with cuff-deficient shoulders, RSA is now commonly used for revision of previously failed shoulder arthroplasty in younger patients, as well as in young patients with nonfunctional shoulders after irreparable cuff tears or fracture sequelae.3, 14, 23, 24 However, the outcomes of these implants in this younger, more active and more demanding population are still uncertain. In recent years, some authors have reported the results of RSA in this specific population, and we were interested in pooling these data to answer the following questions: (1) What are the indications to perform an RSA in patients younger than 65 years? (2) What are the overall complication and revision rates? (3) What are the overall functional outcomes in this specific patient population? Therefore, we conducted a systematic review of the literature to assess midterm functional outcomes and complications of RSA in younger patients.
Methods
We followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines,20 and our review protocol was registered in the PROSPERO database5 (registration no. CRD42018116351), an international register of systematic review protocols, and can be accessed at http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018116351.
PICOT (population, intervention, control, outcomes, time) statement
The PICOT (population, intervention, control, outcomes, time) statement was defined as follows: population, patients younger than 65 years; intervention, RSA; control, none; outcomes, complication rate, revision rate, range of motion, and functional scores; and time, at least 2 years of follow-up
Search strategy
An electronic search of the MEDLINE and Cochrane databases between 1986 and May 2019 was performed on May 31, 2019, using a combination of the keywords “reverse shoulder arthroplasty,” “reverse,” and “arthroplasty or replacement” and one of the following terms: “young,” “younger,” “65,” “60,” “55,” or “50.” We analyzed the titles and abstracts of the studies, and when the abstract indicated a clinical study including patients younger than 65 years who were treated with an RSA, then the study was selected for subsequent analysis. The references of the included studies were screened for eligibility.
Study eligibility
The inclusion criteria were clinical series in the English or French language; studies reporting clinical results with at least 2 years of follow-up; and studies including only patients younger than 65 years at the time of surgery who were treated with RSA for any indication, whether primary or revision RSA. The exclusion criteria were as follows: case reports and reviews of the literature or biomechanical studies; clinical follow-up of less than 2 years; clinical outcomes not reported at the final follow-up; results combined with different types of arthroplasties; and results mixed with those of patients older than 65 years at the time of surgery.
Assessment of study quality
Two reviewers (M.C. and L.L.C.) independently assessed the methodologic quality of all included studies with the Methodological Index for Non-Randomized Studies (MINORS),30 which is a validated instrument designed to assess the methodologic quality of nonrandomized surgical studies. Eight methodologic items are evaluated from 0 to 2, leading to a maximum total score of 16 for noncomparative studies. For comparative studies, 4 additional items are studied, with a maximum overall score of 24. Any discrepancies between reviewers were resolved by consensus.
Outcomes
For each article, we collected the number of patients, sex distribution, etiologies, operative details, complications, reoperations, revisions, clinical outcomes at last follow-up (active forward elevation [AFE], external rotation, and internal rotation), and whenever possible, functional scores (American Shoulder and Elbow Surgeons [ASES] score,25 Subjective Shoulder Value [SSV],11 and Constant score6) and radiologic outcomes (scapular notching and loosening). Postoperative complications were collected and divided into major and minor complications. A major complication was defined as any complication leading to a new surgical procedure (infection, humeral or glenoid loosening, periprosthetic fracture requiring open reduction–internal fixation, open reduction for dislocation, and hematoma requiring evacuation), and a minor complication was defined as any complication not requiring a surgical procedure (acromial fracture, temporary nerve palsy, nonrecurrent dislocation managed with closed reduction, or heterotopic ossification complicated by stiffness).
Data collection
Data were extracted independently by 2 authors (M.C. and L.L.C.) using a purpose-built form combining the MINORS score, the main results for the previously defined outcomes, the possible biases of the study, and the relevant clinical conclusions. For comparative studies that provided complete data for RSA in patients younger than 65 years, we extracted these particular data and included them in the analysis.
Results
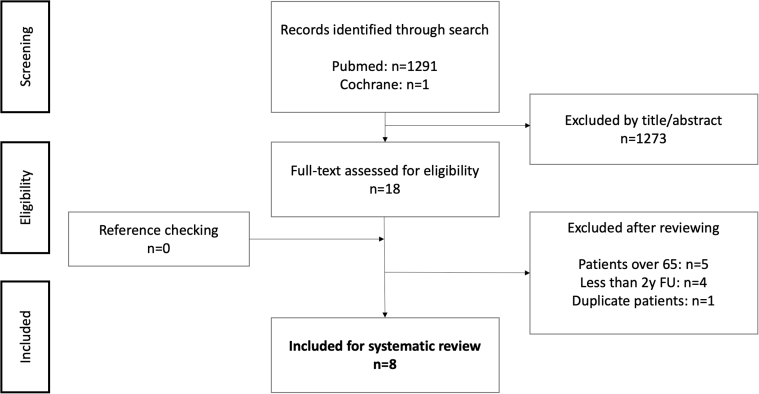
Figure 1 presents the flowchart of the literature search. Eight articles (detailed in Table I) were included in the analysis, with a total of 417 patients (median, 36; minimum, 32; maximum, 67). Two studies compared primary and revision RSA2, 22 and provided complete data for each group, which were therefore analyzed separately in this systematic review. Two studies examined partly duplicate patients with different follow-up periods and ages at inclusion.7, 8 In this case, we kept the study with the largest effective (Ek et al7) and excluded the other series whose follow-up duration was above the median of the other studies (140 months for Ernstbrunner et al8 vs. 50 for all other studies) to decrease heterogeneity.
Figure 1.
Flowchart of included studies. FU, follow-up.
Table I.
Details of studies included in systematic review
| Year | Design | Level of evidence | No. of patients | Male patients, % | Follow-up, mo | Mean age at RSA, yr | Maximum age at RSA, yr | Primary RSA, % | |
|---|---|---|---|---|---|---|---|---|---|
| Authors | |||||||||
| Black et al2: P | 2014 | Case control | III | 33 | 27 | 55 | 59 | 65 | 100 |
| Black et al: R | 2014 | Case control | III | 32 | 22 | 56 | 59 | 65 | 0 |
| Ek et al7 | 2013 | Retrospective case series | IV | 40 | 55 | 93 | 60 | 64 | 100 |
| Leathers et al16 | 2018 | Retrospective cohort | IV | 32 | 34 | 41 | 57 | 65 | 81 |
| Matthews et al18 | 2019 | Retrospective cohort | IV | 43 | 43 | 48 | 60 | 65 | 100 |
| Muh et al21 | 2013 | Retrospective cohort | IV | 67 | 43 | 37 | 52 | 60 | 87 |
| Otto et al22: P | 2017 | Retrospective case series | IV | 32 | 59 | 60 | 49 | 54 | 100 |
| Otto et al: R | 2017 | Retrospective case series | IV | 35 | 40 | 65 | 46 | 54 | 0 |
| Samuelsen et al28 | 2017 | Retrospective case series | IV | 67 | 40 | 36 | 60 | 65 | 100 |
| Sershon et al29 | 2014 | Retrospective case series | IV | 36 | 33 | 34 | 54 | 60 | 86 |
| Total | 2016 | IV (7 of 8) | 417 | 40 | 50 | 56 | 65 | 79 | |
| Minimum | 2013 | — | 32 | 22 | 34 | 46 | 54 | 0 | |
| Maximum | 2018 | — | 67 | 59 | 93 | 60 | 65 | 100 |
RSA, reverse shoulder arthroplasty; P, primary RSA only; R, revision RSA only.
Two studies provided separate outcomes for primary and revision RSA and were detailed separately.
Quality assessment
All included studies were published between 2013 and 2019 in English and were single-center retrospective studies, except for 1 multicenter retrospective study (3 centers).21 Four studies were comparative, those of Black et al,2 Leathers et al,16 Matthews et al,18 and Otto et al,22 and had respective MINORS scores of 17, 12, 12, and 13, respectively. Four studies were noncomparative, those of Ek et al,7 Muh et al,21 Samuelsen et al,28 and Sershon et al,29 with the following MINORS scores: 10, 7, 10, and 10, respectively (detailed in Supplementary Table S1).
Indications for RSA
RSA was used as a primary arthroplasty in 330 patients (79%) and revision of a previous arthroplasty in 87 cases (21%). In primary cases, the indication was CTA or a massive irreparable cuff tear (MICT) in 238 patients (72%), primary osteoarthritis (OA) in 35 (11%), fracture sequelae in 16 (5%), rheumatoid arthritis in 13 (4%), acute fracture in 9, instability arthropathy in 6, and other etiologies in 13. In 2 articles, the CTA and MICT etiologies were combined,2, 28 but in the 6 other articles, the ratio was 75 MICT cases to 79 CTA cases.
Demographic characteristics of study participants and follow-up
Among the 417 cases, 250 were female patients (weighted mean, 60%; range, 41%-78%), with a mean age at surgery of 56 years (range, 21-65 years). The mean follow-up duration was 50 months (range, 34-93 months), and the studies reported that between 0% and 39% of patients were lost to follow-up before 2 years (Table I). Two included studies reported outcomes with a mean follow-up period greater than 5 years.7, 22
Preoperative clinical examination
The authors reported preoperative AFE and active external rotation (AER) in 7 of 8 studies, preoperative ASES scores in 5 of 8, and preoperative active internal rotation and preoperative SSVs in 3 of 8. Preoperatively, the weighted mean AFE, AER, active internal rotation, ASES score, and SSV were 62° (range, 50°-79°), 18° (range, 10°-27°), 3 of 10 points (range, 2-4 points), 33 points (range, 24-40 points), and 22% (range, 19%-24%), respectively.
Surgical technique
The surgical approach was reported in 6 articles2, 7, 18, 21, 22, 29 and was deltopectoral in 309 of 313 cases (99%). Implants were reported in all but 1 article and were different for all studies: Anatomical Shoulder Inverse (Zimmer, Warsaw, IN, USA),2 Delta III (DePuy, Raynham, MA, USA),7, 18 Zimmer Trabecular Metal (Zimmer),16 Aequalis (Tornier, Edina, MN, USA),18, 21 Equinoxe (Exactech, Gainesville, FL, USA),18 Reverse Shoulder Prosthesis (DJO, Vista, CA, USA),18, 22 and Biomet Comprehensive (Biomet, Warsaw, IN, USA).28 In 14 cases (3%), a latissimus dorsi transfer was associated with RSA,2, 7 and a humeral allograft was required for 4 revision RSAs in 1 series.22
Postoperative complications and revisions
Postoperative complications were reported in all articles. The overall complication rate was 16.5% (range, 2%-38%), comprising 11% major (range, 0%-30%) and 6% minor complications, with the most common being instability (5.0%) and infection (3.6%). Other complications included temporary nerve palsy (6 of 417 patients), aseptic glenoid loosening (5 of 417), acromial fracture (5 of 417), scapular spine fracture (4 of 417), periprosthetic humeral fracture (4 of 417), hematoma (3 of 417), and aseptic humeral loosening (2 of 417).
Humeral and/or glenoid revisions were required in 7.2% of patients (range, 0%-23%), and reoperations without revision of glenoid or humeral implants (change of polyethylene liner for instability, debridement for infection, or open reduction–internal fixation) were performed in 5.3% (range, 0%-28%), with an overall reintervention rate of 10.3% (range, 0%-28%). Two studies with mean follow-up periods of 7.8 years7 and 3 years28 included 5-year survival without revision: 98% and 91%, respectively. The complication and reintervention rates are detailed in Table II.
Table II.
Detailed complication and reintervention rates
| Year | N | FU, mo | Complication, % | Revision, % | Reoperation, % | |
|---|---|---|---|---|---|---|
| Authors | ||||||
| Black et al2: primary | 2014 | 33 | 55 | 18 | 6 | 3 |
| Black et al: revision | 2014 | 32 | 56 | 28 | 3 | 9 |
| Ek et al7 | 2013 | 40 | 93 | 38 | 23 | 28 |
| Leathers et al16 | 2018 | 32 | 41 | 9 | 0 | 0 |
| Matthews et al18 | 2019 | 43 | 50 | 2 | 0 | 0 |
| Muh et al21 | 2013 | 67 | 37 | 13 | 7 | 4 |
| Otto et al22: primary | 2017 | 32 | 60 | 19 | 13 | 3 |
| Otto et al: revision | 2017 | 35 | 65 | 26 | 9 | 3 |
| Samuelsen et al28 | 2017 | 67 | 36 | 7 | 3 | 1 |
| Sershon et al29 | 2014 | 36 | 34 | 17 | 11 | 3 |
| Weighted mean | 2016 | 417 | 50 | 16.5 | 7.2 | 5.3 |
| Minimum mean | 2013 | 32 | 34 | 2 | 0 | 0 |
| Maximum mean | 2019 | 67 | 93 | 38 | 23 | 28 |
FU, follow-up duration.
Two studies compared outcomes of primary and revision RSA2, 22 and did not find any significant differences in complication rates (28% vs. 18% and 26% vs. 19%), revision rates (3% vs. 6% and 9% vs. 13%), or reintervention rates (13% vs. 9% and 11% vs. 16%).
Clinical outcomes
AFE and external rotation with the arm at the side (AER1) at final follow-up were reported in all studies; ASES score, 6 studies; internal rotation, 3 studies; SSV, 2 studies; and adjusted Constant score, 2 studies. All studies showed improvement in AFE with a weighted mean AFE of 121° at final assessment. Preoperative and final AER1 values were compared in 6 studies, of which 3 found significantly improved range of motion,21, 28, 29 with an overall weighted mean AER1 of 29° at last follow-up. Clinical outcomes are detailed in Table III.
Table III.
Detailed clinical outcomes
| Year | N | FU, mo | AFE, ° |
AER1, ° |
AIR1 (of 10) |
ASES score |
Adjusted CS at last FU, % | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preop | Last FU | Preop | Last FU | Preop | Last FU | Preop | Last FU | |||||
| Authors | ||||||||||||
| Black et al2: primary | 2014 | 33 | 55 | — | 112 | — | 35 | — | — | — | — | — |
| Black et al: revision | 2014 | 32 | 56 | — | 115 | — | 31 | — | — | — | — | — |
| Ek et al7 | 2013 | 40 | 93 | 72 | 115 | 27 | 22 | — | — | — | — | 73 |
| Leathers et al16 | 2018 | 32 | 41 | 67 | 133 | 24 | 40 | 4 | 5 | 36 | 72 | — |
| Matthews et al18 | 2019 | 43 | 50 | 79 | 123 | 16 | 25 | 4 | 6 | 32 | 71 | |
| Muh et al21 | 2013 | 67 | 37 | 55 | 134 | 10 | 20 | — | — | 40 | 72 | — |
| Otto et al22: primary | 2017 | 32 | 60 | 65 | 113 | 11 | 30 | 2 | 6 | 28 | 59 | — |
| Otto et al: revision | 2017 | 35 | 65 | 50 | 86 | 13 | 16 | 2 | 4 | 23 | 41 | — |
| Samuelsen et al28 | 2017 | 67 | 36 | 58 | 132 | 20 | 39 | — | — | — | 62 | — |
| Sershon et al29 | 2014 | 36 | 34 | 75 | 121 | 23 | 30 | — | — | 31 | 66 | 54 |
| Weighted mean | 2016 | 417 | 50 | 121 | 29 | 5.3 | 64 | 64 | ||||
| Minimum mean | 2013 | 32 | 34 | 86 | 16 | 4 | 41 | 54 | ||||
| Maximum mean | 2019 | 67 | 93 | 134 | 40 | 6 | 72 | 64 | ||||
FU, follow-up duration; AFE, active forward elevation; AER1, active external rotation with arm at side; AIR1, active internal rotation; ASES, American Shoulder and Elbow Surgeons; CS, Constant score; Preop, preoperative.
After the exclusion of 67 revision cases from 2 studies,2, 22 the weighted mean AFE and AER1 were 125° and 30°, respectively. Black et al2 did not find any differences in range of motion or ASES scores between primary and revision surgery cases but found a significant difference in the SSV (60% for revision vs. 76% for primary, P = .015). Otto et al22 did not find any significant differences in patient satisfaction or improvement between preoperative and postoperative functional scores.
Radiologic outcomes
Scapular notching was reported in 6 studies (285 patients) and was found in 30% of cases (range, 9%-48%), with grade 3 or 4 notching in 6% (range, 0%-20%). One group of authors reported a significant difference in the adjusted Constant score at 7.8 years of follow-up between patients with and without scapular notching (66% vs. 86%, P = .02).7 Other studies did not report any association between notching and clinical outcomes. Humeral loosening was reported in 2 cases (1%), and glenoid loosening was reported in 7 (2%).
Discussion
In 2013, several authors started to report their results of RSA in patients younger than 65 years, with a growing body of literature since 2017, which motivated our systematic review. RSA was performed in younger patients mainly for MICTs with or without glenohumeral arthritis and as a solution for revision arthroplasty, consisting of 80% of all indications. Fracture sequelae were found in only 14 patients, but this may be under-represented in this systematic review, as the results of these patients are reported in series mixing younger and older patients. In a systematic review of the literature on RSA for fracture sequelae by Holton et al,15 the mean age at surgery was 69.7 years, and 8 of 9 studies included patients younger than 65 years at the time of surgery. Primary OA was the indication in only 6%, as expected in this young population with competent rotator cuffs. No authors detailed the reason to use an RSA for primary OA, but the common indications likely include concomitant cuff tears and severe humeral head static subluxation with or without glenoid erosion (type B2, B3, or C glenoid).17, 19, 31
Postoperative complications were found in 17% of patients, leading to a new surgical procedure in 10% of all patients at a mean follow-up of 4.2 years. These results are comparable to those found by Zumstein et al33 in their systematic review of RSA (N = 782; mean age, 68 years), with a 21% complication rate and 13% reintervention rate at a mean of 3.5 years of follow-up, dominated by instability and infection, similarly to our systematic review. Moreover, 2 included studies compared outcomes of patients younger than 65 years and those older than 70 years (results of older patients were not included in our analysis) and did not find any significant differences in the complication or revision rates.16, 18 These results need to be further confirmed with appropriately designed long-term studies. The loosening rate was found to be low at midterm follow-up (1.6%), but long-term follow-up can be concerning in these patients with an increased life expectancy. A recent study showed that the 10-year revision-free survival rate of RSA was 92% in patients younger than 60 years and that clinical outcomes did not significantly deteriorate beyond 10 years.8 Anatomic total shoulder arthroplasty (TSA) in the same population leads to revision-free survival rates of 98% to 100% at 5 years, which is superior to what we found with RSA, but the survival rate decreases to 62% to 92% at 10 years.26 Therefore, further studies are required to confirm the encouraging long-term results of RSA found by Ernstbrunner et al.8
Midterm clinical outcomes were shown to be successful as they restored forward elevation above the horizontal (weighted mean, 121°) and allowed AER (weighted mean, 29°) in these patients with poor preoperative range of motion (AFE, 62°; AER, 18°). However, these results may not lead to complete satisfaction of these younger patients' expectations. In a study of the Danish Shoulder Arthroplasty Registry, Ammitzboell et al1 found that the 1-year median Western Ontario Osteoarthritis of the Shoulder index (quality-of-life questionnaire) after RSA was 79 in patients older than 65 years but was only 54 in younger patients. Matthews et al18 reported that younger patients had a comparable range of motion at final follow-up to that in older patients, but the ASES score and Short Form health survey score (Short Form 12, another quality-of-life questionnaire) were lower in younger patients. Leathers et al16 showed better range of motion and improvement in range of motion in younger patients, whereas the ASES score was not different from that in older patients at final review. Furthermore, Friedman et al10 analyzed an international database of 660 RSA patients with a mean age of 72 years. They found that each 1-year increase was associated with an improved ASES score by 0.19 points (P = .006) but with decreased forward flexion by 0.39° (P = .001) per year. These results tend to support the idea that younger patients expect higher functional levels and experience less satisfaction as reflected in patient-reported outcomes.
The range of motion obtained with RSA seems lower than what is reported with anatomic TSA in young patients. Roberson et al,26 in a systematic review of 154 patients younger than 65 years who were treated with TSA, reported 130° of abduction and 39° of external rotation at a mean of 9.4 years of follow-up, which are better results than those in our systematic review. However, the etiologies were different for these anatomic TSAs, dominated by primary OA and rheumatoid arthritis, and TSA could not be a viable solution in patients without competent rotator cuffs regardless of the age of the patients.4, 9
We were not able to highlight any differences in the outcomes of primary and revision RSA in this review including 2 studies comparing these populations. However, higher complication and revision rates have been demonstrated in older patients by at least 3 studies that compared primary and revision RSA and reported significantly higher rates of postoperative complications (19% to 69%) after revision RSA.13, 27, 32
Our study was limited by the retrospective design of all the included studies with inherent selection bias, as well as by the exclusion of studies including patients younger than 65 years but whose results were mixed with those of older patients and could not be isolated for meta-analysis. In the same way, we could not directly compare outcomes between etiologies, as the studies did not present these results separately for each indication. We tried to compare primary and revision RSA by removing 67 revision cases from 2 studies.2, 22 Nevertheless, this was limited by 22 revision cases in 3 studies,16, 21, 29 whose results were mixed with those of primary cases. One study reported a 39% loss-to-follow-up rate but was included in this systematic review because it analyzed the highest number of patients within the 8 included studies,28 although this may bias our results. Finally, the short follow-up duration of these studies does not allow conclusions on long-term outcomes, which is essential in this young and active population. However, to our knowledge, this is the first attempt to summarize the results of RSA in young patients to present an up-to-date summary of this topic.
Conclusion
RSA is mostly used in young patients for MICTs with or without glenohumeral arthritis, as well as revision of failed arthroplasties with poor preoperative shoulder function. The complication (17%) and reintervention (12%) rates at mean follow-up of 4 years are comparable to those of older patients. AFE and external rotation were restored in most patients, although the functional results were modest. Therefore, RSA can be a viable option in young patients with a cuff-deficient shoulder or failed arthroplasty, when nonoperative treatment has failed, with reliable clinical improvements and midterm complication rates comparable to those of older patients.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jses.2019.06.003.
Supplementary data
References
- 1.Ammitzboell M., Baram A., Brorson S., Olsen B.S., Rasmussen J.V. Poor patient-reported outcome after shoulder replacement in young patients with cuff-tear arthropathy: a matched-pair analysis from the Danish Shoulder Arthroplasty Registry. Acta Orthop. 2019;90:119–122. doi: 10.1080/17453674.2018.1563855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Black E.M., Roberts S.M., Siegel E., Yannopoulos P., Higgins L.D., Warner J.J.P. Reverse shoulder arthroplasty as salvage for failed prior arthroplasty in patients 65 years of age or younger. J Shoulder Elbow Surg. 2014;23:1036–1042. doi: 10.1016/j.jse.2014.02.019. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P., Trojani C., Chuinard C., Lehuec J.-C., Walch G. Proximal humerus fracture sequelae: impact of a new radiographic classification on arthroplasty. Clin Orthop Relat Res. 2006;442:121–130. doi: 10.1097/01.blo.0000195679.87258.6e. [DOI] [PubMed] [Google Scholar]
- 4.Boileau P., Watkinson D.J., Hatzidakis A.M., Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14:S147–S161. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 5.Booth A., Clarke M., Dooley G., Ghersi D., Moher D., Petticrew M. The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst Rev. 2012;1:2. doi: 10.1186/2046-4053-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Constant C.R., Murley A.H. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160–164. [PubMed] [Google Scholar]
- 7.Ek E.T.H., Neukom L., Catanzaro S., Gerber C. Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elbow Surg. 2013;22:1199–1208. doi: 10.1016/j.jse.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 8.Ernstbrunner L., Andronic O., Grubhofer F., Camenzind R.S., Wieser K., Gerber C. Long-term results of reverse total shoulder arthroplasty for rotator cuff dysfunction: a systematic review of longitudinal outcomes. J Shoulder Elbow Surg. 2019;28:774–781. doi: 10.1016/j.jse.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Franklin J.L., Barrett W.P., Jackins S.E., Matsen F.A., 3rd Glenoid loosening in total shoulder arthroplasty. Association with rotator cuff deficiency. J Arthroplasty. 1988;3:39–46. doi: 10.1016/s0883-5403(88)80051-2. [DOI] [PubMed] [Google Scholar]
- 10.Friedman R.J., Cheung E.V., Flurin P.-H., Wright T., Simovitch R.W., Bolch C. Are age and patient gender associated with different rates and magnitudes of clinical improvement after reverse shoulder arthroplasty? Clin Orthop Relat Res. 2018;476:1264–1273. doi: 10.1007/s11999.0000000000000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gerber C., Fuchs B., Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505–515. doi: 10.2106/00004623-200004000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Grammont P., Trouilloud P., Laffay J., Deries X. Study and development of a new shoulder prosthesis. Rhumatologie. 1987;39:17–22. [in French] [Google Scholar]
- 13.Groh G.I., Groh G.M. Complications rates, reoperation rates, and the learning curve in reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:388–394. doi: 10.1016/j.jse.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Hattrup S.J., Waldrop R., Sanchez-Sotelo J. Reverse total shoulder arthroplasty for posttraumatic sequelae. J Orthop Trauma. 2016;30:e41–e47. doi: 10.1097/BOT.0000000000000416. [DOI] [PubMed] [Google Scholar]
- 15.Holton J., Yousri T., Arealis G., Levy O. The role of reverse shoulder arthroplasty in management of proximal humerus fractures with fracture sequelae: a systematic review of the literature. Orthop Rev Pavia. 2017;9:6977. doi: 10.4081/or.2017.6977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leathers M.P., Ialenti M.N., Feeley B.T., Zhang A.L., Ma C.B. Do younger patients have better results after reverse total shoulder arthroplasty? J Shoulder Elbow Surg. 2018;27(Suppl):S24–S28. doi: 10.1016/j.jse.2017.11.014. [DOI] [PubMed] [Google Scholar]
- 17.Magosch P., Habermeyer P., Lichtenberg S., Tauber M., Gohlke F., Mauch F. Ergebnisse des deutschen Schulter- und Ellenbogenprothesenregisters (SEPR) [Results from the German shoulder- and elbow arthroplasty register (SEPR): anatomic or reverse shoulder arthroplasty in B2-glenoids?] Orthopade. 2017;46:1063–1072. doi: 10.1007/s00132-017-3485-4. [in German] [DOI] [PubMed] [Google Scholar]
- 18.Matthews C.J., Wright T.W., Farmer K.W., Struk A.M., Vasilopoulos T., King J.J. Outcomes of primary reverse total shoulder arthroplasty in patients younger than 65 years old. J Hand Surg. 2019;44:104–111. doi: 10.1016/j.jhsa.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 19.Mizuno N., Denard P.J., Raiss P., Walch G. Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Joint Surg Am. 2013;95:1297–1304. doi: 10.2106/JBJS.L.00820. [DOI] [PubMed] [Google Scholar]
- 20.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 21.Muh S.J., Streit J.J., Wanner J.P., Lenarz C.J., Shishani Y., Rowland D.Y. Early follow-up of reverse total shoulder arthroplasty in patients sixty years of age or younger. J Bone Joint Surg Am. 2013;95:1877–1883. doi: 10.2106/JBJS.L.10005. [DOI] [PubMed] [Google Scholar]
- 22.Otto R.J., Clark R.E., Frankle M.A. Reverse shoulder arthroplasty in patients younger than 55 years: 2- to 12-year follow-up. J Shoulder Elbow Surg. 2017;26:792–797. doi: 10.1016/j.jse.2016.09.051. [DOI] [PubMed] [Google Scholar]
- 23.Raiss P., Edwards T.B., Collin P., Bruckner T., Zeifang F., Loew M. Reverse shoulder arthroplasty for malunions of the proximal part of the humerus (type-4 fracture sequelae) J Bone Joint Surg Am. 2016;98:893–899. doi: 10.2106/JBJS.15.00506. [DOI] [PubMed] [Google Scholar]
- 24.Raiss P., Edwards T.B., da Silva M.R., Bruckner T., Loew M., Walch G. Reverse shoulder arthroplasty for the treatment of nonunions of the surgical neck of the proximal part of the humerus (type-3 fracture sequelae) J Bone Joint Surg Am. 2014;96:2070–2076. doi: 10.2106/JBJS.N.00405. [DOI] [PubMed] [Google Scholar]
- 25.Richards R.R., An K.-N., Bigliani L.U., Friedman R.J., Gartsman G.M., Gristina A.G. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 26.Roberson T.A., Bentley J.C., Griscom J.T., Kissenberth M.J., Tolan S.J., Hawkins R.J. Outcomes of total shoulder arthroplasty in patients younger than 65 years: a systematic review. J Shoulder Elbow Surg. 2017;26:1298–1306. doi: 10.1016/j.jse.2016.12.069. [DOI] [PubMed] [Google Scholar]
- 27.Saltzman B.M., Chalmers P.N., Gupta A.K., Romeo A.A., Nicholson G.P. Complication rates comparing primary with revision reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1647–1654. doi: 10.1016/j.jse.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 28.Samuelsen B.T., Wagner E.R., Houdek M.T., Elhassan B.T., Sánchez-Sotelo J., Cofield R. Primary reverse shoulder arthroplasty in patients aged 65 years or younger. J Shoulder Elbow Surg. 2017;26:e13–e17. doi: 10.1016/j.jse.2016.05.026. [DOI] [PubMed] [Google Scholar]
- 29.Sershon R.A., Van Thiel G.S., Lin E.C., McGill K.C., Cole B.J., Verma N.N. Clinical outcomes of reverse total shoulder arthroplasty in patients aged younger than 60 years. J Shoulder Elbow Surg. 2014;23:395–400. doi: 10.1016/j.jse.2013.07.047. [DOI] [PubMed] [Google Scholar]
- 30.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 31.Walch G., Moraga C., Young A., Castellanos-Rosas J. Results of anatomic nonconstrained prosthesis in primary osteoarthritis with biconcave glenoid. J Shoulder Elbow Surg. 2012;21:1526–1533. doi: 10.1016/j.jse.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 32.Wall B. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89:1476. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 33.Zumstein M.A., Pinedo M., Old J., Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20:146–157. doi: 10.1016/j.jse.2010.08.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.