Abstract
Background
The number of total shoulder arthroplasties (TSAs) performed is increasing annually, with a continued effort to improve outcomes using new techniques and materials. In anatomic TSAs, the main options for glenoid fixation currently involve keeled or pegged components. The aim of this review was to determine which fixation option provides optimal long-term functional outcomes with decreased rates of revision surgery and radiolucency.
Methods
The MEDLINE, Embase, PubMed, and Cochrane databases were searched from 2007 to July 10, 2017, for all articles that examined TSAs using either pegged or keeled glenoid fixations. All studies were screened in duplicate for eligibility. Two separate analyses were completed examining noncomparative and comparative studies independently.
Results
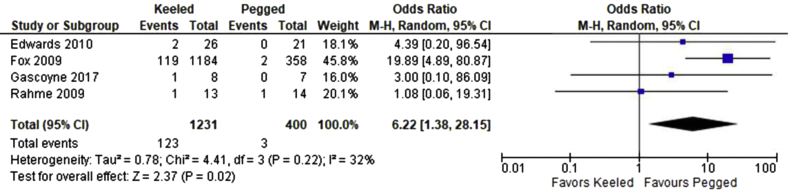
A total of 7 comparative studies and 25 noncomparative studies were included in the final analysis. Included in the analysis were 4 randomized (level I) studies, 1 level II study, 8 level III studies, and 19 level IV studies. Meta-analysis of the comparative studies demonstrated a higher rate of revision surgery with keeled fixations compared with pegged fixations (odds ratio, 6.22; 95% confidence interval [CI], 1.38-28.1; P = .02). No significant difference was found with respect to functional outcomes, such as the American Shoulder and Elbow Surgeons score (mean difference, 9.54; 95% CI, –8.25 to 27.34; P = .29) and Constant score (mean difference, 5.31; 95% CI, –12.28 to 22.89; P = .55), as well as radiolucency rates (odds ratio, 1.89; 95% CI, 0.56−6.39; P = .30).
Conclusion
Pegged glenoid fixation may result in a decreased risk of revision TSAs, but no significant differences in patient-reported outcomes have been identified to date.
Keywords: Glenoid fixation, keeled glenoid component, pegged glenoid component, total shoulder arthroplasty, total shoulder replacement, TSA
The use of anatomic total shoulder arthroplasty (TSA) for the treatment of primary osteoarthritis, rheumatoid arthritis, and other glenohumeral pathologies reduces pain, improves movement, and increases power.6, 17 The prevalence of shoulder osteoarthritis in the United States has been demonstrated to be as high as 32.8%.10 The rate of TSAs completed between 1993 and 2007 increased by 10.6% annually,13 and most recently, the American Academy of Orthopaedic Surgeons reported that approximately 53,000 TSAs are completed each year.1 Over time, radiolucency can develop between the bone-cement interface of the TSA glenoid component, with a reported prevalence of 15% to 84%.8 Although controversial, radiolucent lines at the glenoid bone-cement interface on plain radiographs may be an indicator of glenoid component loosening and potentially an early sign of impending component failure.35 There is some suggestion that the development of focal radiolucency may be associated with component migration and poor clinical function, leading ultimately to failure and the need for revision surgery.12, 26, 39, 54 The reported rate of revision for TSA ranges from 15.6% to 32% in the literature after approximately 3.5 years of follow-up.4, 34, 55
Surgical techniques and total shoulder components have evolved in an effort to continue to improve long-term outcomes. A quickly evolving area is glenoid component design and fixation.41 The 2 main options with respect to glenoid components are keeled and pegged designs. The keeled fixation was first introduced in 1973 as part of Neer’s original glenoid component design.37 The keeled design has undergone many variations but ultimately resembles a tapered “fin,” with a rectangular geometry.32 The pegged design is more recent and encompasses a variable number of pegs of varying lengths. Biomechanical studies have suggested that pegged fixation withstands high shear forces and may result in a decreased rate of loosening compared with keeled glenoid components.3, 24, 32 In addition, basic science, retrospective, and prospective studies have suggested that keeled designs have a propensity to develop more radiolucency over time than pegged designs.21, 33, 48, 52 Although the literature suggests that using pegged glenoid components may result in decreased radiolucency over time, it is unclear whether this relation directly correlates with superior long-term clinical outcomes.22
The aim of this systematic review was to compare both the clinical and radiographic outcomes of pegged vs. keeled glenoid components in anatomic TSA. We hypothesized that pegged components would demonstrate a lower rate of development of focal radiolucency, as well as superior long-term functional outcomes and lower rates of revision surgery.
Methods
Search strategy
A comprehensive search of the MEDLINE, Embase, PubMed, and Cochrane databases from 2007 to 2017 was performed for articles on TSA. The search was run on July 10, 2017, in duplicate by 2 independent reviewers (A.W. and C.G.). The search terms included “arthroplasty, replacement, shoulder,” “equipment failure analysis,” “osteoarthritis,” “joint instability,” “range of motion, articular,” “shoulder,” “glenoid cavity,” and “prosthesis failure,” and the keywords “Peg*” and “Keel*” were used in all searches. Medical Subject Headings (MeSH) and Emtree terms were used in various combinations to increase search sensitivity. The search strategy is provided in Supplementary Material.
Study screening
All titles, abstracts, and full texts were screened by 2 independent reviewers (A.W. and C.G.). Any disagreements at the title and abstract stages were included in the next stage of screening, and disagreements at the final stage were discussed and resolved by the 2 reviewers.
Study eligibility
The inclusion criteria for this review were as follows: (1) human studies evaluating the efficacy of TSA with either pegged or keeled glenoid components; (2) studies examining the components independently, as well as comparative studies; (3) randomized controlled trials (RCTs), cohort studies, or retrospective studies; (4) studies with a minimum of 6 months’ follow-up postoperatively; and (5) studies examining adult populations (aged > 18 years).
Studies using a radiostereometric analysis were included in the review, but only functional outcomes were analyzed. The exclusion criteria were (1) systematic reviews and case reports; (2) studies that used cadaveric specimens, animal specimens, or hybrid glenoid component designs; and (3) studies that examined only revision TSAs.
Assessment of study quality
The quality of the individual studies was assessed by both reviewers. The Methodological Index for Non-randomized Studies (MINORS) criteria were used for observational studies.46 The MINORS tool evaluates 8 domains comprising the aim, appropriateness of the sample, study design, outcome measures, bias, follow-up, data completeness, and power of a study. There are an additional 4 domains for comparative studies. The tool assesses the methodologic quality of studies with higher scores indicating higher-quality studies. A maximum score of 16 for noncomparative studies and 24 for comparative studies can be achieved. The Cochrane Risk of Bias Tool was used for all RCTs. The tool assesses potential selection bias, reporting bias, performance bias, detection bias, attrition bias, and other sources of bias. A score of either high, low, or unclear bias is given for each domain. Any discrepancies were resolved by consensus between 2 independent assessors (A.W. and C.G.) and the senior author (M.K.).
Data abstraction
Data were extracted into a piloted electronic database (Microsoft Excel; Microsoft, Redmond, CA, USA) independently by both reviewers. Data were extracted on the number of participants, mean follow-up time, incidence of radiolucency, rate of revision, Constant score, and American Shoulder and Elbow Surgeons (ASES) shoulder score. Demographic data on the year published, study design, population, inclusion criteria, and exclusion criteria were also extracted.
The primary outcomes were shoulder pain and function as delineated by clinical outcome scores (ASES and Constant scores). Secondary outcomes included rate of revision surgery and reported rate of radiolucency of glenoid components.
Statistical analysis
Comparative and noncomparative studies were analyzed as separate data sets. This was done to avoid bias, as significant heterogeneity was present among the noncomparative studies. Noncomparative studies were evaluated via a qualitative analysis. The categorical data (revision rate and radiolucency) were evaluated via the pooled rate. Continuous data (ASES and Constant scores) were evaluated via the mean and standard deviation of the reported mean. Categorical and continuous data were evaluated via the mean and standard deviation at 3 different ranges of follow-up: short (<1 year), moderate (1-5 years), and long (>5 years). The radiolucency rate was expressed as a percentage as a function of the different follow-up ranges. Both keeled and pegged data were aggregated to evaluate the impact of follow-up time on the various outcome measures. Follow-up time was evaluated to examine the effect of time following implantation in all patients with anatomic shoulder arthroplasties, irrespective of component type. Comparative studies were included in the quantitative synthesis. For comparative studies, the data were reviewed for statistical heterogeneity using the I2 statistic. Meta-analysis was performed for use of a random-effects model. For each included study, mean differences (MDs) and 95% confidence intervals (CIs) were calculated for continuous outcomes whereas odds ratios (ORs) and 95% CIs were calculated for dichotomous outcomes. When variance data were not available, imputation was used with variance data from the studies that were not able to be pooled. We performed sensitivity analysis to confirm that imputed standard deviations did not change the final conclusions of the meta-analysis. Similarly, as for the noncomparative studies, the mean follow-up time for the comparative studies was subdivided into 3 categories—short (<1 year), moderate (1-5 years), and long (>5 years)—and evaluated for categorical data and continuous data via the mean and standard deviation. All analyses were completed using Review Manager software, version 5.3 (The Cochrane Collaboration, London, UK).
Results
Included studies
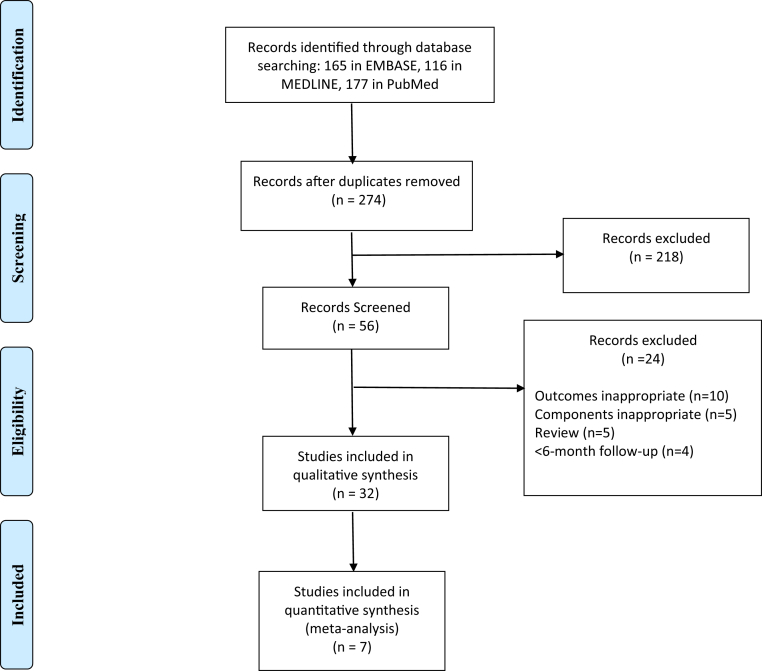
The search yielded a total of 458 articles from the PubMed, Embase, and MEDLINE databases. Following duplicate removal and title and abstract screening, 56 articles underwent a full review. Thirty-two articles were included in the qualitative analysis, comprising both comparative and noncomparative studies. Among these articles, 7 comparative studies were included in the meta-analysis. The inter-rater reliability for the raters was found to be κ = 0.847 (P < .001), with a 95% CI of 0.759 to 0.935, indicating almost complete agreement with respect to study eligibility. A PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) diagram detailing the flow of the review is shown in Figure 1.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) flow diagram.
Of the studies, 17 were completed in North America; 14, Europe; and 1, Australia. A total of 25 studies were noncomparative. Of these studies, 9 examined keeled glenoid fixations9, 12, 15, 19, 23, 31, 50, 51, 54 and 16 examined pegged glenoid fixations5, 7, 14, 25, 26, 27, 28, 29, 35, 36, 38, 39, 42, 45, 49, 53 (Table I). Among these studies, 10 reported ASES scores, 16 reported Constant scores, 19 reported radiolucency rates, and 19 reported revision rates.
Table I.
Summary of demographic characteristics of noncomparative studies∗
| Authors | Population: primary OA vs. various† | Component | No. of participants | Total no. of shoulders with radiolucency at final follow-up | ASES score | Constant score | Revision rate |
|---|---|---|---|---|---|---|---|
| Arnold et al,5 2011 | Primary | Pegged | 35 | 11 | 81.3 | 0 | |
| Bell and Coghlan,7 2014 | Primary | Pegged | 50 | 8 | 92.58 | 86 | 0.020 |
| Budge et al,9 2013 | Various | Keeled | 19 | 1 | 70.5 | 0.158 | |
| Collin et al,12 2011 | Primary | Keeled | 56 | 20 | 63 | 0.054 | |
| De Wilde et al,14 2013 | Various | Pegged | 34 | 4 | 72 | ||
| Denard et al,15 2013 | Primary | Keeled | 50 | 22 | 73.4 | 0.34 | |
| Fox et al,19 2013 | Various | Keeled | 151 | 102 | 0.046 | ||
| Gazielly and Scarlat,23 2015 | Primary | Keeled | 39 | 6 | 73 | 0.026 | |
| Greiner et al,25 2013 | Various | Pegged | 90 | 24 | 84.2 | 0.075 | |
| Groh,26 2010 | Various | Pegged | 83 | 0 | 0 | ||
| Gulotta et al,27 2015 | Primary | Pegged | 40 | 80.1 | 0.05 | ||
| Ho et al,28 2013 | Primary | Pegged | 66 | 29 | |||
| Hsu et al,29 2014 | Unspecified | Pegged | 50 | 89.85 | 0.04 | ||
| Kooistra et al,31 2017 | Primary | Keeled | 29 | 84 | 0 | ||
| McLendon et al,35 2017 | Various | Pegged | 287 | 227 | 0.091 | ||
| Merolla et al,36 2016 | Primary | Pegged | 40 | 2 | 93.4 | 69.8 | 0 |
| Nuttall et al,39 2012 | Primary | Pegged | 11 | 6 | 85 | 63 | |
| Nuttall et al,38 2017 | Primary | Pegged | 11 | 74.7 | 61.4 | ||
| Press et al,42 2014 | Various | Pegged: perforated | 18 | 91 | 77.4 | ||
| Pegged: unperforated | 34 | 82.6 | 75.6 | ||||
| Service et al,45 2017 | Various | Pegged | 71 | 20 | 0.042 | ||
| Vidil et al,49 2013 | Various | Pegged | 27 | 3 | 74.5 | 0 | |
| Walch et al,51 2011 | Primary | Keeled | 302 | 57 | 67.6 | 0.026 | |
| Walch et al,50 2012 | Primary | Keeled | 518 | 166 | |||
| Wirth et al,53 2012 | Various | Pegged | 44 | 84.5 | 0.023 | ||
| Young et al,54 2011 | Primary | Keeled | 217 | 99 | 57.6 | 0.168 |
OA, osteoarthritis; ASES, American Shoulder and Elbow Surgeons.
All values are presented at latest follow-up; number of participants are based on participants included in the radiolucency analysis.
Various includes inflammatory arthritis, post-traumatic arthritis, osteonecrosis, rheumatoid arthritis, and other.
A total of 7 studies compared keeled vs. pegged glenoid fixations. Table II shows the details. Among these studies, 2 reported ASES scores, 2 reported Constant scores, 4 reported radiolucency rates, and 4 reported revision rates.
Table II.
Summary of demographic characteristics of comparative studies∗
| Authors | Population: primary OA vs. various† | Component | No. of participants | Total no. of shoulders with radiolucency at final follow-up | ASES score | Constant score | Revision rate |
|---|---|---|---|---|---|---|---|
| Edwards et al,16 2010 | Primary | Keeled | 24 | 19 | 0.077 | ||
| Pegged | 21 | 5 | 0 | ||||
| Fox et al,18 2009 | Various | Keeled | 1184 | 0.101 | |||
| Pegged | 358 | 0.006 | |||||
| Gascoyne et al,22 2017 | Unspecified | Keeled | 8 | 73.5 | 0.125 | ||
| Pegged | 7 | 96.4 | 0 | ||||
| Nuttall et al,40 2007 | Primary | Keeled | 10 | 84 | 65 | ||
| Pegged | 10 | 78 | 62 | ||||
| Rahme et al,43 2009 | Primary | Keeled | 12 | 9 | 70 | 0.077 | |
| Pegged | 14 | 8 | 70 | 0.071 | |||
| Roche et al,44 2017 | Unspecified | Keeled | 54 | 16 | 82.9 | 69.3 | |
| Pegged | 111 | 46 | 83 | 68.9 | |||
| Throckmorton et al,47 2010 | Primary | Keeled | 50 | 39 | |||
| Pegged | 50 | 37 |
OA, osteoarthritis; ASES, American Shoulder and Elbow Surgeons.
All values are presented at latest follow-up; number of participants are based on participants included in the radiolucency analysis.
Various includes inflammatory arthritis, post-traumatic arthritis, osteonecrosis, rheumatoid arthritis, and other.
Quality assessment and risk of bias
A total of 28 nonrandomized and 4 randomized (level I) studies were included in this review. Of the nonrandomized studies, 1 was level II, 8 were level III, and 19 were level IV. The mean MINORS score was 11.62 ± 0.90 for noncomparative studies and 18.71 ± 1.83 for comparative studies, which indicated a fair quality of evidence for all studies (Table III). All RCTs were at high risk of bias owing to incomplete data. Of the 4 RCTs, 3 did well in maintaining a low risk of bias with respect to randomization, participant allocation, and other sources of bias (Table IV).
Table III.
Methodologic index for nonrandomized controlled trials
| Authors | Clearly stated aim | Inclusion of consecutive patients | Prospective collection of data | Endpoints appropriate for aim | Unbiased assessment of endpoints | Appropriate follow-up period | Loss to follow-up rate <5% | Prospective calculation of study size | Adequate control group | Contemporary groups | Baseline equivalence of groups | Adequate statistical analysis | Total score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Arnold et al,5 2011 | 2 | 1 | 2 | 2 | 2 | 2 | 0 | 0 | 11 | ||||
| Bell and Coghlan,7 2014 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 0 | 12 | ||||
| Budge et al,9 2013 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 0 | 12 | ||||
| Collin et al,12 2011 | 0 | 2 | 2 | 2 | 1 | 2 | 1 | 0 | 2 | 2 | 2 | 2 | 18 |
| De Wilde et al,14 2013 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | 12 | ||||
| Denard et al,15 2013 | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 0 | 11 | ||||
| Fox et al,18 2009 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 21 |
| Fox et al,19 2013 | 2 | 2 | 1 | 2 | 1 | 2 | 1 | 0 | 11 | ||||
| Gazielly and Scarlat,23 2015 | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 0 | 11 | ||||
| Greiner et al,25 2013 | 0 | 2 | 2 | 2 | 1 | 2 | 1 | 0 | 10 | ||||
| Groh,26 2010 | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 0 | 11 | ||||
| Gulotta et al,27 2015 | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 21 |
| Ho et al,28 2013 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 0 | 13 | ||||
| Hsu et al,29 2014 | 2 | 1 | 1 | 2 | 2 | 2 | 2 | 0 | 12 | ||||
| Kooistra et al,31 2017 | 0 | 2 | 1 | 2 | 1 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 17 |
| McLendon et al,35 2017 | 2 | 1 | 1 | 2 | 1 | 2 | 2 | 0 | 11 | ||||
| Merolla et al,36 2016 | 2 | 2 | 1 | 2 | 1 | 2 | 1 | 0 | 11 | ||||
| Nuttall et al,39 2012 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | 13 | ||||
| Nuttall et al,38 2017 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | 13 | ||||
| Press et al,42 2014 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 0 | 2 | 2 | 1 | 2 | 20 |
| Roche et al,44 2017 | 1 | 1 | 2 | 2 | 0 | 2 | 1 | 0 | 2 | 2 | 1 | 2 | 16 |
| Service et al,45 2017 | 1 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | 12 | ||||
| Throckmorton et al,47 2010 | 2 | 1 | 1 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 18 |
| Vidil et al,49 2013 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | 12 | ||||
| Walch et al,51 2011 | 2 | 2 | 1 | 2 | 1 | 2 | 1 | 0 | 11 | ||||
| Walch et al,50 2012 | 2 | 2 | 1 | 2 | 2 | 2 | 1 | 1 | 13 | ||||
| Wirth et al,53 2012 | 2 | 2 | 1 | 2 | 2 | 2 | 1 | 0 | 12 | ||||
| Young et al,54 2011 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 0 | 10 |
Table IV.
Cochrane risk-of-bias assessment of randomized controlled trials
| Authors | Random sequence generation | Allocation concealment | Selective reporting | Other sources of bias | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data |
|---|---|---|---|---|---|---|---|
| Edwards et al,16 2010 | Low | Low | Low | Low | Unclear | Unclear | High |
| Gascoyne et al,22 2017 | Low | Low | Low | Low | Low | Low | High |
| Nuttall et al,40 2007 | Unclear | Unclear | Low | High | Unclear | Unclear | High |
| Rahme et al,43 2009 | Low | Low | Low | Low | Unclear | Low | High |
Clinical outcomes
The clinical outcomes consisted of the ASES and Constant scores. These scores provide a surrogate of the overall functional outcome of the TSA. The qualitative analysis of the noncomparative studies yielded a mean Constant score of 69.77 ± 9.22 among the keeled fixation studies vs. a mean of 74.52 ± 8.26 for the pegged fixation studies. With respect to mean follow-up time, no studies had a short follow-up, whereas the moderate follow-up studies demonstrated a mean Constant score of 69.10 ± 8.34 and the long follow-up studies had a mean Constant score of 66.92 ± 27.98 for both keeled and pegged components combined. Only 1 keeled fixation study reported the mean ASES score, which was found to be 70.5,9 whereas the mean ASES score for the pegged fixation studies was 85.97 ± 6.28. With respect to mean follow-up time, no studies had a short follow-up; the moderate follow-up studies demonstrated a mean ASES score of 83.82 ± 7.89; and there was only 1 long follow-up study, with a mean ASES score of 89.85.29
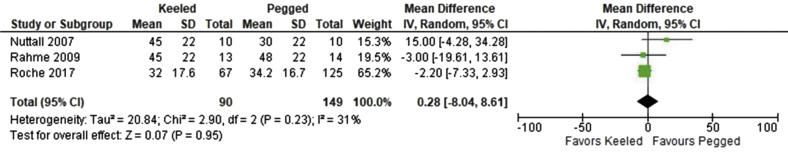
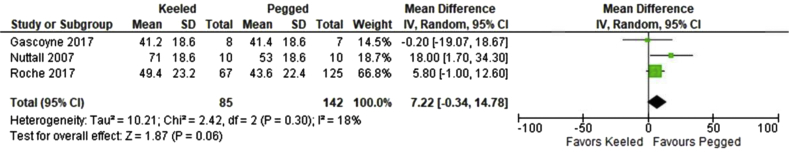
Of the 7 comparative studies, 3 reported Constant scores.43, 44, 40 This included 90 patients with keeled components and 149 patients with pegged components. There was no significant difference between the 2 groups (MD, 0.28; 95% CI, –8.04 to 8.61; P = .95) (Fig. 2). With respect to follow-up, there were no short follow-up studies, whereas the mean for moderate follow-up studies was 66.75 ± 3.95 and the mean for long follow-up studies was 69.1 ± 0.28 for both keeled and pegged components combined. In addition, 3 of the 7 studies reported ASES scores.22, 40, 44 This included 85 patients with keeled components and 142 with pegged components. There was no significant difference between the 2 groups (MD, 7.22; 95% CI, –0.34 to 14.78; P = .06) (Fig. 3). When we examined the follow-up time for ASES scores, there were no short follow-up studies, whereas moderate follow-up studies demonstrated a mean of 82.98 ± 9.93 and long follow-up studies demonstrated a mean of 82.95 ± 0.07 for both keeled and pegged components combined.
Figure 2.
Forest plot of American Shoulder and Elbow Surgeons score with pegged and keeled glenoid components. SD, standard deviation; CI, confidence interval; IV, inverse variance.
Figure 3.
Forest plot of radiolucency line rates at latest follow-up with pegged and keeled glenoid components. SD, standard deviation; CI, confidence interval; IV, inverse variance.
Radiolucency
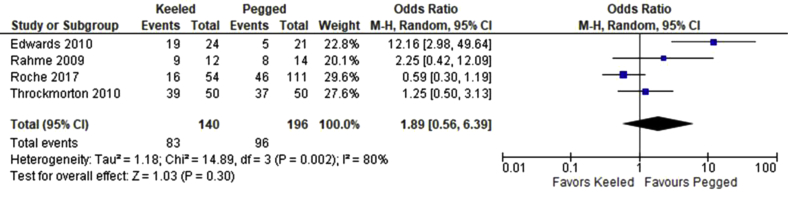
Qualitative analysis of the noncomparative studies demonstrated that the pooled rate of radiolucency at final follow-up for the keeled fixation studies was 34.99% (473 of 1352) whereas the pooled rate for pegged fixation studies was 42% (334 of 794). As a function of follow-up time, there were no short follow-up studies that reported radiolucency, whereas the moderate follow-up studies demonstrated a rate of radiolucency development of 20.5% (108 of 526) at final follow-up and the long follow-up studies demonstrated a rate of 43% (699 of 1620) for both keeled and pegged components combined. Of the 7 comparative studies, 4 reported rates of radiolucency at final follow-up.16, 43, 44, 47 There were a total of 140 patients with keeled components and 196 with pegged components. No significant difference was found between the 2 groups (OR, 1.89; 95% CI, 0.56-6.39; P = .30) (Fig. 4). Statistical heterogeneity was found among the studies (I2 = 80%, P = .002). With respect to follow-up time in the comparative studies, there were no short follow-up studies, whereas the moderate follow-up studies demonstrated a rate of 68% of shoulders (117 of 171) with radiolucency at final follow-up and the long follow-studies showed a rate of 38% (62 of 165) at final follow-up for both keeled and pegged components combined.
Figure 4.
Forest plot of Constant score with pegged and keeled glenoid components. CI, confidence interval; M-H, Mantel-Haenszel.
Revision surgery
Qualitative analysis of the noncomparative studies demonstrated that the pooled rate of revisions for the keeled fixation studies was 8.76% (133 of 1518) and the pooled rate for the pegged fixation studies was 5.22% (46 of 880). When we examined the mean revision rate as a function of follow-up time, there were no studies with a short follow-up, whereas the mean revision rate for moderate follow-up studies was 3% ± 5% and that for long follow-up studies was 10% ± 11% for both keeled and pegged components combined. Regarding the comparative studies, 4 reported revision rates.16, 18, 22, 43 This included a total of 1231 patients with keeled components and 400 patients with pegged components. A significant difference was found between the 2 groups (OR, 6.22; 95% CI, 1.38-28.1; P = .02), with the pegged group (3 of 400, 0.75%) having fewer revisions than the keeled group (123 of 1231, 10%) (Fig. 5). Statistical heterogeneity was not found among the studies (I2 = 32%, P = .22). As a function of follow-up time, there were no short follow-up studies among the comparative studies; the mean revision rate among moderate follow-up studies was 5% ± 5%; and there was only 1 long follow-up study, with a revision rate of 10%.18 All of the results including ASES scores, Constant scores, radiolucency rates, and revision rates are summarized for comparative and noncomparative studies in Tables V and VI, respectively.
Figure 5.
Forest plot of revision rates after total shoulder arthroplasty with keeled and pegged glenoid components. CI, confidence interval; M-H, Mantel-Haenszel.
Table V.
Summary of results for comparative studies for various follow-up periods
| Follow-up period | ASES score | Constant score | Revision rate, % | Radiolucency total rate, % |
|---|---|---|---|---|
| Short (<6 mo) | 0 | 0 | 0 | 0 |
| Moderate (6 mo to 5 yr) | 82.98 ± 9.93 | 66.75 ± 3.95 | 5 ± 5 | 68 |
| Long (>5 yr) | 82.95 ± 0.07 | 69.10 ± 0.28 | 10∗ | 38 |
ASES, American Shoulder and Elbow Surgeons.
Only 1 study within follow-up period.
Table VI.
Summary of results for noncomparative studies for various follow-up periods
| Follow-up period | ASES score | Constant score | Revision rate, % | Radiolucency total rate, % |
|---|---|---|---|---|
| Short (<6 mo) | 0 | 0 | 0 | 0 |
| Moderate (6 mo to 5 yr) | 83.82 ± 7.89 | 69.10 ± 8.34 | 3 ± 5 | 20.5 |
| Long (>5 yr) | 89.85∗ | 66.92 ± 27.98 | 10 ± 11 | 43 |
ASES, American Shoulder and Elbow Surgeons.
Only 1 study within follow-up period.
Discussion
This systematic review evaluates reported outcomes with respect to pegged vs. keeled glenoid components in TSA. It is interesting to note that no significant difference was found between pegged and keeled components regarding functional outcomes (Constant and ASES scores) in higher-quality comparative studies. We found a non–statistically significant trend with respect to Constant and ASES scores in noncomparative studies, suggesting improved functional outcomes with pegged fixation. Because of the high heterogeneity among the noncomparative studies, no formal statistical analysis could be completed owing to the increased risk of bias. Given that most comparative data are derived from small studies of fair-quality evidence, the trend toward pegged fixation in the noncomparative studies suggests the need for a large trial to provide high-quality evidence to definitively determine which component provides improved patient outcomes with a decreased risk of complications and risk of revision surgery.
We found the rate of revisions to be lower with pegged fixation in comparison with keeled fixation (OR, 6.22; 95% CI, 1.38-28.1; P = .02). However, no difference in radiolucency data was found between pegged and keeled fixations, suggesting that glenoid loosening may not be directly correlated with the underlying indication for revision surgery in those cases. Although the absence of radiolucency postoperatively is often used as an indicator of success, the clinical relevance of radiolucent lines following TSA is controversial in the literature.8, 33 Although it was initially suggested that radiolucency correlates directly with glenoid component loosening, recent data have demonstrated that this may not be a causative correlation. A review by Bohsali et al8 examining complications of TSA identified that 80% of patients developed radiolucent lines yet only 7% ultimately required revision surgery. In addition, Lazarus et al33 examined the prevalence of radiolucency in 328 patients undergoing TSA. They identified a high prevalence of radiolucent lines around glenoid components and found that only 20 of the 328 glenoids (6%) demonstrated no radiolucencies. Although radiolucency may be a potential surrogate for glenoid component loosening, a number of other factors are likely at play when considering the need for revision of TSA.11 This review supports the current trend suggesting radiolucent lines may not be directly correlated to glenoid loosening, and other causes should be evaluated when considering revision in the setting of a painful shoulder following TSA.
The lower revision rate with pegged fixation in comparison to keeled fixation may be influenced by a number of factors. A biomechanical study by Anglin et al3 identified that pegged components offered greater resistance to off-center loads than keeled components. In addition, less subchondral bone resection is required with pegged components, and the placement of the pegs in stronger peripheral bone may offer a biomechanical advantage.2 Furthermore, keeled fixations are generally cemented whereas newer pegged designs using hybrid fixation offer potential for partial bony ingrowth, which may strengthen fixation.
Another important variable to consider is the length of time each study followed up its participants postoperatively. A formal statistical analysis was not completed examining the effect of follow-up time on radiolucency and revision rates because of the variability with which the variance around the follow-up time was reported in the studies. Therefore, concrete conclusions cannot be drawn. However, there was a trend for studies with longer follow-up periods to show increased total numbers of shoulders that developed radiolucencies and to show increased revision rates. This may have contributed to the significant difference seen between keeled and pegged components with respect to the revision rate in comparative studies, as the majority of the keeled shoulders came from a long-term follow-up study.18 However, further studies examining follow-up in comparative studies of the 2 glenoid fixations are necessary. Conversely, among functional measures such as the ASES and Constant scores, the same trend was not seen. This may support the contention that the development of radiolucency in the glenoid component may not be a good surrogate for patient satisfaction.
The finding in this systematic review of no difference in radiolucency rates between glenoid components opposes the current literature, which suggests keeled glenoid components are more likely to develop radiolucent lines.30 Khazzam et al30 completed a systematic review comparing 107 pegged and 96 keeled components and found that the presence of radiolucent lines was more common in keeled glenoid components with a risk difference of –0.32 (P < .05; 95% CI, –0.62 to –0.03) favoring pegged components. The results in our review may differ owing to the inclusion of the comparative study by Roche et al,44 which was the only study to demonstrate a higher rate of radiolucent lines in patients with pegged components (41.4%) than in patients with keeled components (29.6%). Sensitivity analysis excluding the study of Roche et al confirmed our findings to be robust (OR, 3.07; 95% CI, 0.74-12.81; P = .12). It is interesting to note that there was no significant difference between the ASES and Constant scores in the study by Roche et al, further reinforcing the notion that radiolucent lines may not be a strong indicator of functional outcomes.
The study by Khazzam et al,30 as with many other studies on this topic, primarily evaluated outcomes with respect to radiolucent lines and glenoid failure. Our systematic review took an approach in which functional outcomes were analyzed as they pertain to keeled and pegged fixations while also including analyses of both comparative and noncomparative studies. This review focused primarily on functional outcomes as these are often more valuable and clinically important to patients. Other strengths of this study include a rigorous methodology and inclusion criteria when systematically including studies in the review. We had 2 independent reviewers examine all the studies, and they demonstrated strong agreement as reflected by the high κ score.
A limitation to our analysis of the functional outcomes is that comparative studies did not report standard deviations; therefore, variances were generated using data that were not able to be pooled, which could have impacted the accuracy of the comparison.20 In addition, only 2 comparative studies reported the ASES and Constant scores. When this information is taken into consideration with the means found in the noncomparative studies, no strong conclusion can be drawn and it seems that there is a paucity of high-quality evidence examining functional outcomes with each glenoid component after TSA. Another limitation of our study is the heterogeneity found among the studies in the radiolucency rate analysis. This may have been a result of variable follow-up times in the studies, ranging from a mean of 24 months to 73.9 months. In addition, some studies included only patients with primary osteoarthritis whereas others included patients with other indications for TSA. Another limitation is the lack of information surrounding the indications for revision in the studies. Finally, variations in the keeled and pegged glenoid fixation models may have contributed to increased heterogeneity. Although the inclusion of noncomparative studies expanded our search and encompassed all available data, these studies could not be included in the final meta-analysis to avoid a biased statistical analysis.
Larger high-quality randomized trials are needed when comparing pegged and keeled glenoid components, particularly with respect to functional outcomes. Only a small percentage of the available literature on the topic is composed of level I studies, as seen in this review. In addition, given that radiolucency rates did not correlate well with revision rates, perhaps other factors should be the focus of future research to determine how to prevent failure and improve outcomes.
Conclusion
The rate of revision for pegged glenoid implants in TSA is significantly lower than that for keeled implants, but the data to date suggest no differences in functional outcomes with either component. However, this may not necessarily be attributable to glenoid component loosening and the formation of radiolucent lines on plain radiographs. The number of comparative studies examining functional outcomes is scarce, and there is a need for high-level studies to incorporate functional outcomes such as the ASES and Constant scores in the future.
Disclaimer
Asheesh Bedi is a paid consultant for Arthrex. All the other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Appendix A: Search strategies for Medline and PubMed
Database: OVID Medline Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to Present
Search Strategy:
1 exp Arthroplasty, Replacement, Shoulder/
2 shoulder arthroplasty.mp.
3 exp Prosthesis Failure/
4 exp Osteoarthritis/
5 exp Joint Instability/ or exp "Range of Motion, Articular"/
6 exp Shoulder Joint/ or exp Glenoid Cavity/
7 1 or 2 or 3 or 4 or 5 or 6
8 peg*.mp.
9 keel*.mp.
10 8 or 9
11 7 and 10
12 limit 11 to yr="2007 -Current"
Database: Embase <1996 to 2017 July 05>
Search Strategy:
1 exp shoulder arthroplasty/
2 shoulder arthroplasty.mp.
3 exp prosthesis failure/
4 exp osteoarthritis/
5 exp joint instability/
6 exp "range of motion"/
7 exp shoulder/
8 exp glenoid cavity/
9 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8
10 peg*.mp.
11 keel*.mp.
12 10 or 11
13 9 and 12
14 limit 13 to yr="2007 -Current"
References
- 1.American Academy of Orthopaedic Surgeons . 2011. Shoulder joint replacement. OrthoInfo.https://orthoinfo.aaos.org/en/treatment/shoulder-joint-replacement [Google Scholar]
- 2.Anglin C., Tolhurst P., Wyss U.P., Pichora D.R. Glenoid cancellous bone strength and modulus. J Biomech. 1999;32:1091–1097. doi: 10.1016/s0021-9290(99)00087-1. [DOI] [PubMed] [Google Scholar]
- 3.Anglin C., Wyss U.P., Nyffeler R.W., Gerber C. Loosening performance of cemented glenoid prosthesis design pairs. Clin Biomech. 2001;16:144–150. doi: 10.1016/s0268-0033(00)00078-4. [DOI] [PubMed] [Google Scholar]
- 4.Antoni M., Barthoulot M., Kempf J.F., Clavert P. Revisions of total shoulder arthroplasty: clinical results and complications of various modalities. Orthop Traumatol. 2016;102:297–303. doi: 10.1016/j.otsr.2016.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Arnold R.M., High R.R., Grosshans K.T., Walker C.W., Fehringer E.V. Bone presence between the central peg's radial fins of a partially cemented pegged all poly glenoid components suggest few radiolucencies. J Shoulder Elbow Surg. 2011;20:315–321. doi: 10.1016/j.jse.2010.05.025. [DOI] [PubMed] [Google Scholar]
- 6.Barrett W.P., Franklin J.L., Jackins S.E., Wyss C.R., Matsen 3rd., F.A. Total shoulder arthroplasty. J Bone Joint Surg Am. 1987;69:865–872. [PubMed] [Google Scholar]
- 7.Bell S.N., Coghlan J.A. Short stem shoulder replacement. Int J Shoulder Surg. 2014;8:72–75. doi: 10.4103/0973-6042.140113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bohsali K.I., Wirth M.A., Rockwood Jr., C.A. Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88:2279–2292. doi: 10.2106/JBJS.F.00125. [DOI] [PubMed] [Google Scholar]
- 9.Budge M.D., Nolan E.M., Heisey M.H., Baker K., Wiater J.M. Results of total shoulder arthroplasty with a monoblock porous tantalum glenoid component: a prospective minimum 2-year follow-up study. J Shoulder Elbow Surg. 2013;22:535–541. doi: 10.1016/j.jse.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 10.Chillemi C., Franceschini V. Shoulder osteoarthritis. Arthritis. 2013;2013:370231. doi: 10.1155/2013/370231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cofield R.H., Edgerton B.C. Total shoulder arthroplasty: complications and revision surgery. Instr Course Lect. 1990;39:449–462. [PubMed] [Google Scholar]
- 12.Collin P., Tay A.K.L., Melis B., Boileau P., Walch G. A ten-year radiologic comparison of two-all polyethylene glenoid component designs: a prospective trial. J Shoulder Elbow Surg. 2011;20:1217–1223. doi: 10.1016/j.jse.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 13.Day J.S., Lau E., Ong K.L., Williams G.R., Ramsey M.L., Kurtz S.M. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010;19:1115–1120. doi: 10.1016/j.jse.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 14.De Wilde L., Dayerizadeh N., De Neve F., Basamania C., Van Tongel A. Fully uncemented glenoid component in total shoulder arthroplasty. J Shoulder Elbow Surg. 2013;33:e1–e7. doi: 10.1016/j.jse.2013.01.036. [DOI] [PubMed] [Google Scholar]
- 15.Denard P.J., Raiss P., Sowa B., Walch G. Mid- to long-term follow-up of total shoulder arthroplasty using a keeled glenoid in young adults with primary glenohumeral arthritis. J shoulder Elbow Surg. 2013;22:894–900. doi: 10.1016/j.jse.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 16.Edwards T.B., Labriola J.E., Stanley R.J., O’Connor D.P., Elkousy H.A., Gartsman G.M. Radiographic comparison of pegged and keeled glenoid components using modern cementing techniques: a prospective randomized study. J Shoulder Elbow Surg. 2010;19:251–257. doi: 10.1016/j.jse.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 17.Fehringer E.V., Kopjar B., Boorman R.S., Churchill R.S., Smith K.L., Matsen F.A., 3rd Characterizing the functional improvement after total shoulder arthroplasty for osteoarthritis. J Bone Joint Surg Am. 2002;84-A:1349–1353. doi: 10.2106/00004623-200208000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Fox T.J., Cil A., Sperling J.W., Sanchez-Sotelo J., Schleck C.D., Cofield R.H. Survival of the glenoid component in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:859–863. doi: 10.1016/j.jse.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 19.Fox T.J., Foruria A.M., Klika B.J., Sperling J.W., Schleck C.D., Cofield R.H. Radiographic survival I total shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:1221–1227. doi: 10.1016/j.jse.2012.12.034. [DOI] [PubMed] [Google Scholar]
- 20.Furukawa T.A., Barbui C., Cipriani A., Brambilla P., Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. J Clin Epidemiol. 2006;59:7–10. doi: 10.1016/j.jclinepi.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 21.Gartsman G.M., Elkousy H.A., Warnock K.M., Edwards B., O’Connor D.P. Radiographic comparison of pegged and keeled glenoid components. J Shoulder Elbow Surg. 2005;14:252–257. doi: 10.1016/j.jse.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Gascoyne T.C., McRae S.M.B., Parashin S.L., Leiter J.R.S., Petrak M.J., Bohm E.R. Radiostereometric analysis of keeled versus pegged glenoid components in total shoulder arthroplasty: a randomized feasibility study. Can J Surg. 2017;60:273–279. doi: 10.1503/cjs.001817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gazielly D.F., Scarlat M.M. Long-term survival of the glenoid components in total shoulder replacement for arthritis. Int Orthop. 2015;39:285–289. doi: 10.1007/s00264-014-2637-y. [DOI] [PubMed] [Google Scholar]
- 24.Giori N.J., Beaupré G.S., Carter D.R. The influence of fixation peg design on the shear stability of prosthetic implants. J Orthop Res. 1990;8:892–898. doi: 10.1002/jor.1100080615. [DOI] [PubMed] [Google Scholar]
- 25.Greiner S., Berth A., Kääb M., Irlenbusch U. Glenoid morphology affects the incidence of radiolucent lines around cemented pegged polyethylene glenoid components. Arch Orthop Trauma Surg. 2013;133:1331–1339. doi: 10.1007/s00402-013-1813-7. [DOI] [PubMed] [Google Scholar]
- 26.Groh G.I. Survival and radiographic analysis of a glenoid component with a cementless fluted central peg. J Shoulder Elbow Surg. 2010;19:1265–1268. doi: 10.1016/j.jse.2010.03.012. [DOI] [PubMed] [Google Scholar]
- 27.Gulotta L.V., Chambers K.L., Warren R.F., Dines D.M., Craig E.V. No differences in early results of a hybrid glenoid compared with a pegged implant. Clin Orthop Relat Res. 2015;473:3918–3924. doi: 10.1007/s11999-015-4558-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ho C.J., Sabesam V.J., Iannotti J.P. Glenoid component retroversion is associated with osteolysis. J Bone Joint Surg Am. 2013;95:e82. doi: 10.2106/JBJS.L.00336. [DOI] [PubMed] [Google Scholar]
- 29.Hsu J.E., Namdari S., Baron M., Kuntz A.F., Abboud J.A., Huffman R. Glenoid perforation with pegged components during shoulder total shoulder arthroplasty. Orthopedics. 2014;37:587–591. doi: 10.3928/01477447-20140528-61. [DOI] [PubMed] [Google Scholar]
- 30.Khazzam M., Argo M., Landrum M., Box H. Comparison of pegged and keeled glenoid components for total shoulder arthroplasty: a systematic review. J Shoulder Elbow Arthroplasty. 2017;1:1–7. [Google Scholar]
- 31.Kooistra B.W., Willems W.J., Lemmens E., Hartel B.P., van den Bekerom M.P.J., van Deurzen D.F.P. Comparative study of total shoulder arthroplasty versus total shoulder surface replacement for glenohumeral osteoarthritis with minimum 2-year follow-up. J Shoulder Elbow Surg. 2017;26:430–436. doi: 10.1016/j.jse.2016.07.029. [DOI] [PubMed] [Google Scholar]
- 32.Lacroix D., Murphy L.A., Prendergast P.J. Three-dimensional finite analysis of glenoid replacement prostheses: a comparison of keeled and pegged anchorage systems. J Biomech Eng. 2000;122:430–436. doi: 10.1115/1.1286318. [DOI] [PubMed] [Google Scholar]
- 33.Lazarus M.D., Jensen K.L., Southworth C., Matsen 3rd., F.A. The radiographic evaluation of keeled and pegged glenoid component insertion. J Bone Joint Surg Am. 2002;84:1174–1182. doi: 10.2106/00004623-200207000-00013. [DOI] [PubMed] [Google Scholar]
- 34.Levy J.C., Virani N., Pupello D., Frankle M. Use of reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Joint Surg Br. 2007;89-B:189–195. doi: 10.1302/0301-620X.89B2.18161. [DOI] [PubMed] [Google Scholar]
- 35.McLendon P.B., Schoch B.S., Sperling J.W., Sánchez-Sotelo J., Schleck C.D., Cofield R.H. Survival of the pegged glenoid component in shoulder arthroplasty: part II. J Shoulder Elbow Surg. 2017;26:1469–1476. doi: 10.1016/j.jse.2016.12.068. [DOI] [PubMed] [Google Scholar]
- 36.Merolla G., Chin P., Sasyniuk T.M., Paladini P., Porcellini G. Total shoulder arthroplasty with a second-generation tantalum trabecular metal-backed glenoid component. Bone Joint J. 2016;98:75–80. doi: 10.1302/0301-620X.98B1.36620. [DOI] [PubMed] [Google Scholar]
- 37.Neer C.S., II . Glenohumeral arthroplasty. In: Neer C.S. II, editor. Shoulder reconstruction. WB Saunders; Philadelphia: 1990. p. 143. [Google Scholar]
- 38.Nuttall D., Birch A., Haines J.F., Watts A.C., Trail I.A. Early migration of a partially cemented fluted glenoid component inserted using a cannulated preparation system. Bone Joint J. 2017;99:674–679. doi: 10.1302/0301-620X.99B5.BJJ-2016-0745.R1. [DOI] [PubMed] [Google Scholar]
- 39.Nuttall D., Haines J.F., Trail I.A. The early migration of partially cemented fluted pegged glenoid component using radiostereometric analysis. J Shoulder Elbow Surg. 2012;21:1191–1196. doi: 10.1016/j.jse.2011.07.028. [DOI] [PubMed] [Google Scholar]
- 40.Nuttall D., Haines J.F., Trail I.I. A study of the micromovement of pegged and keeled glenoid components compared using radiostereometric glenoid components compared using radiosterometric analysis. J Shoulder Elbow Surg. 2007;16:65–70. doi: 10.1016/j.jse.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 41.Pinkas D., Wiater B., Wiater J.M. The glenoid component in anatomic shoulder arthroplasty. J Am Acad Orthop Surg. 2015;23:317–326. doi: 10.5435/JAAOS-D-13-00208. [DOI] [PubMed] [Google Scholar]
- 42.Press C.M., O'Connor D.P., Elkousy H.A., Gartsman G.M., Edwards B. Glenoid perforation does not affect the short-term outcomes of pegged all-polyethylene implants in total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1203–1207. doi: 10.1016/j.jse.2013.11.024. [DOI] [PubMed] [Google Scholar]
- 43.Rahme H., Mattsson P., Wikbald L., Nowak J., Larsson S. Stability of cemented in-line pegged glenoid compared with keeled glenoid components in total shoulder arthroplasty. J Bone Joint Surg Am. 2009;91:1965–1972. doi: 10.2106/JBJS.H.00938. [DOI] [PubMed] [Google Scholar]
- 44.Roche C, Flurin PH, Grey S, Wright T, Zuckerman J. Comparison of midterm aTSA clinical outcomes with keeled and pegged glenoids of equivalent radial mismatch. Paper presented at: 2017 Annual Meeting of Orthopaedic Research Society. March 19-22, 2017; San Diego, CA.
- 45.Service B.C., Hsu J.E., Somerson J.S., Russ S.M., Masten F.A., III Does postoperative glenoid retroversion affect the 2-year clinical and radiographic outcomes for total shoulder arthroplasty? Clin Orthop Relat Res. 2017;475:2726–2739. doi: 10.1007/s11999-017-5433-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 47.Throckmorton T.W., Zarkadas P.C., Sperling J.W., Cofield R.H. Pegged versus keeled glenoid components in total shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19:726–733. doi: 10.1016/j.jse.2009.10.018. [DOI] [PubMed] [Google Scholar]
- 48.Trail I.A., Nuttall D. The results of shoulder arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Br. 2002;84:1121–1125. doi: 10.1302/0301-620x.84b8.12695. [DOI] [PubMed] [Google Scholar]
- 49.Vidil A., Valenti P.H., Guichoux F., Barthas J.H. CT scan evaluation of glenoid component fixation: a prospective study of 27 minimally cemented shoulder arthroplasties. Eur J Orthop Surg Traumatol. 2013;23:521–525. doi: 10.1007/s00590-012-1126-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Walch G., Young A.A., Boileau P., Loew M., Gazielly D., Molé D. Patterns of loosening of polyethylene keeled glenoid components after shoulder arthroplasty for primary osteoarthritis. J Bone Joint Surg Am. 2012;94:145–150. doi: 10.2106/JBJS.J.00699. [DOI] [PubMed] [Google Scholar]
- 51.Walch G., Young A.A., Melis B., Gazielly D., Loew M., Boileau P. Results of a convex-back cemented keeled glenoid component in primary osteoarthritis: multicenter study with a follow-up greater than 5 years. J Shoulder Elbow Surg. 2011;20:385–394. doi: 10.1016/j.jse.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 52.Wirth M.A., Korvick D.L., Basamania C.J., Toro F., Aufdemorte T.B., Rockwood Jr., C.A. Radiologic, mechanical, and histologic evaluation of 2 glenoid prosthesis designs in a canine model. J Shoulder Elbow Surg. 2001;10:140. doi: 10.1067/mse.2001.112021. [DOI] [PubMed] [Google Scholar]
- 53.Wirth M.A., Loredo R., Garcia G., Rockwood C.A., Southworth C., Iannotti J.P. Total shoulder arthroplasty with an all-polyethylene pegged bone-ingrowth glenoid component. J Bone Joint Surg Am. 2012;94:260–267. doi: 10.2106/JBJS.J.01400. [DOI] [PubMed] [Google Scholar]
- 54.Young A., Walch G., Boileau P., Favard L., Gohlke F., Loew M. A multicentre study of the long-term results of using flat-back polyethylene glenoid component in shoulder replacement for primary osteoarthritis. J Bone Joint Surg Br. 2011;93:210–216. doi: 10.1302/0301-620X.93B2.25086. [DOI] [PubMed] [Google Scholar]
- 55.Zumstein M.A., Pinedo M., Old J., Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20:146–157. doi: 10.1016/j.jse.2010.08.001. [DOI] [PubMed] [Google Scholar]