Abstract
Poor diet has been identified as a major cause of chronic disease. In this study we estimated the 2018 economic burden of chronic disease attributable to not complying with Canadian food recommendations. We retrieved the chronic disease risk estimates for intakes of both protective (fruit, vegetables, milk, whole grains, nuts and seeds) and harmful foods (sugar-sweetened beverages, processed meat, red meat) from the Global Burden of Disease Study, and food intakes from the 2015 Canadian Community Health Survey 24-hour dietary recalls (n = 19,797). Population attributable fractions (PAFs) were calculated for all food–chronic disease combinations, and mathematically adjusted to estimate the 2018 annual direct (hospital, physician, drug) and indirect (human capital approach) economic burden for each disease. Not meeting the eight food recommendations was estimated to be responsible for CAD$15.8 billion/year in direct (CAD$5.9 billion) and indirect (CAD$9.9 billion) costs. The economic burden of Canadians under-consuming healthful foods exceeded the burden of overconsumption of harmful foods (CAD$12.5 billion vs. CAD$3.3 billion). Our findings suggest poor diet represents a substantial economic burden in Canada. Interventions may be more effective if they are wide in focus and promote decreased consumption of harmful foods alongside increased consumption of healthful foods, with emphasis on whole grains and nuts and seeds.
Keywords: health economics, health care costs, food consumption, dietary assessment, national survey, Canada, CCHS
1. Introduction
Noncommunicable chronic diseases such as cancers, cardiovascular disease, and type 2 diabetes, remain the leading cause of death in Canada [1]. The direct (i.e., hospitalization, physician, and drug costs) and indirect (i.e., lost productivity, morbidity, and premature mortality) health care costs associated with chronic disease amount to billions of dollars each year according to the Economic Burden of Illness (EBIC) study [2]. Extensive research has identified poor diet quality as a major, though modifiable, cause of chronic disease [3]. In Canada, poor diet represents a substantial contributor to the burden of chronic disease, with only smoking ranking higher [4]. Given the important role of poor diet in chronic disease, the current economic burden in terms of direct and indirect costs of unhealthy eating in Canada needs to be characterized in order to identify the potential economic benefits of health promotion strategies targeting Canadians’ diets.
Various approaches have been utilized to measure the burden of chronic disease due to suboptimal diet. Recently, the Global Burden of Disease Diet Collaborators released a systematic analysis of the health effects of dietary risks in 195 countries [5]. They reported that 11 million deaths from noncommunicable diseases in 2017 were attributable to dietary factors, with low intake of whole grains, vegetables, and fruit and high intake of sodium as the leading dietary risk factors for deaths globally [5].The most common approach to estimating the economic burden of unhealthy eating is to quantify the impact of a single dietary factor, such as inadequate consumption of vegetables and fruit [6,7], dairy [8,9], meat [10], and fiber [11], and overconsumption of sugar-sweetened beverages [12,13]. However, these approaches do not capture the full picture and underestimate the overall economic burden of unhealthy eating.
Fewer studies have estimated the overall economic burden of poor diet quality or unhealthy eating. The existing studies vary as to whether they consider specific dietary intakes, and use an incidence-based (estimate of the lifetime costs of a condition from onset until recovery or death) or prevalence-based approach (estimate costs of a condition in a set period of time (e.g., one year), regardless of onset) to estimate the economic burden. A study of five European countries (France, Italy, Germany, Spain, UK) used an incidence-based approach to calculate the economic burden of unhealthy diets on type 2 diabetes, projecting a total burden of €883 million (equivalent to CAD$1.2 billion) for the year 2020 [14]. In 2006, Scarborough et al. used a prevalence-based approach to estimate the economic burden of ill health (cardiovascular disease, cancer, type 2 diabetes, and dental caries) due to diet and other known risk factors, finding poor diet to be responsible for £5.8 billion per year in the U.K. (equivalent to CAD$9.5 billion) [15]. Using a prevalence-based approach for coronary heart disease, cancer, stroke, and diabetes, a study in the United States estimated an economic burden of USD$70.9 billion (equivalent to CAD$93 billion) attributed to poor eating patterns in 1995 [16]. In terms of Canadian estimates, Health Canada used a similar approach to estimate the direct and indirect costs of unhealthy eating in 1998 to be CAD$6.6 billion [17]. More recently, Nshimyumukiza et al. used a prevalence-based approach and the healthy eating index to determine the economic burden of eating a low-quality diet in 2004 and 2015 in Canada, finding a slight decrease in overall economic burden (CAD$13.21 to $13.08 billion), but an increase in burden in the elderly [18].
The World Health Organization (WHO) has identified Mediterranean and Nordic-style diets as evidence-based diets for the prevention and control of noncommunicable chronic diseases [19]. The Mediterranean diet is rich in vegetables, fruit, nuts, cereals, and olive oil and favors consumption of fish and poultry over red meat and processed meats. The Nordic diet is similar, with emphasis on vegetables, berries, whole grains, pulses, fatty fish, and rapeseed oil. As of 2018, the WHO reported 15 countries in the European region have policies or programs recommending adherence to these diets [19]. In the Canadian context, Health Canada has established food recommendations to help the public consume a balanced diet by promoting consumption of healthful foods such as fruit, vegetables, nuts and seeds, whole grains, and milk, while limiting intake of harmful foods such as red meat, processed meat, and sugar-sweetened beverages. However, these guidelines are not widely met in Canada [20]. Studying adherence to established recommendations yields direction to the work of both policy makers and practitioners. For the year 2014, we estimated the economic burden of chronic disease (cardiovascular disease, cancer, type 2 diabetes, chronic kidney disease) due to not meeting recommendations for healthful and harmful foods to be $13.8 billion using data from the 2004 Canadian Community Health Survey (CCHS) [21]. To our knowledge, outside of our previous study, no others have quantified the economic burden of chronic disease due to not meeting established food recommendations. Since the CCHS data were collected in 2004, there has been a shift in public perception of what constitutes an acceptable diet and more up to date dietary survey data are available from the 2015 CCHS. To support ongoing evaluation of existing nation-wide food policies and implementation of future dietary programs and interventions, a more recent estimation is needed. In this study we estimate the 2018 economic burden of chronic disease due to not complying with food recommendations in Canada using 2015 CCHS data.
2. Materials and Methods
We defined the economic burden of chronic disease for 2018 as that which could be potentially circumvented if all Canadians complied entirely with food recommendations. This analysis pertains to the difference in the number of servings of fruit, vegetables, whole grains, nuts and seeds, milk, red meat, processed meat, and sugar-sweetened beverages Canadians are recommended to consume, and what they actually consumed using representative, population-based data from 2015. The present analysis follows our previous approach that used 2004 dietary data to estimate the economic burden of unhealthy eating in Canada in 2014 [21] Our estimations involved a prevalence-based, bottom-up approach, which estimated the economic burden of chronic diseases attributable to foods for specific age and sex groups (for a set period of time, one year). The steps in this approach included: (1) selection of foods for inclusion and retrieval of dose–response relative risks (RRs); (2) analysis of diet history data; (3) calculation of PAFs; and (4) estimation of attributable direct and indirect health care costs. The four steps are outlined below. Full analytic details can be found in our previous analysis [21].
2.1. Food Selection
We selected foods for inclusion that were identified by the 2017 Global Burden of Disease Study (GBD) as having convincing or probable evidence against one or more chronic diseases, and for which recommendations are in effect [3]. We included the following eight foods: fruit (not including juice), whole grains, nonstarchy vegetables, fluid milk, nuts and seeds, processed meat, red meat, and sugar-sweetened beverages (SSB). The 2017 GBD also included legumes, however we did not include them in the analysis as Canadian recommendations for their consumption were not in effect at the time of the survey in 2015. We retrieved dose–response relative risks for each of the food–chronic diseases combinations from the 2017 GBD (with the exception of SSB, which were retrieved from the 2013 GBD [22] as the RR values in 2017 did not correspond to the conventional 226.8 g serving). Table 1 presents all included food–chronic disease combinations. All RRs used are presented in Table S1.
Table 1.
Foods and chronic diseases included in estimation of the economic burden of unhealthy eating in Canada.
| Food | Chronic Disease | Food Recommendation | Serving Size | CNF/CFG Group Subgroup and Tiers Included for Analysis |
|---|---|---|---|---|
| Fruit | Cancer: Mouth; Larynx; Esophagus; Trachea, Lung, and Bronchus Cardiovascular Disease: Ischemic Heart Disease; Ischemic Stroke; Hemorrhagic Stroke Diabetes |
Female and Male † ≤14 years: 2 servings/day 15+ years: 3 servings/day |
80 g | Vegetables and Fruit
|
| Vegetables | Cardiovascular Disease: Ischemic Heart Disease; Ischemic Stroke; Hemorrhagic Stroke | Female † ≤14 years: 3 servings/day 15+ years: 4 servings/day Male † ≤14 years: 3 servings/day15–54 years: 5 servings/day 55+ years: 4 servings/day |
80 g | Vegetables and Fruit (note all corn and potatoes were removed from relevant categories):
|
| Whole Grains | Cardiovascular Disease: Ischemic Heart Disease; Ischemic Stroke; Hemorrhagic Stroke Diabetes |
Female †† ≤14 years: 2.5 servings/day 15+ years: 3 servings/day Male †† ≤14 years: 2.5 servings/day 15–54 years: 4 servings/day 55+ years: 3.5 servings/day |
35 g | Grain Products
|
| Nuts and Seeds | Cardiovascular Disease: Ischemic Heart Disease Diabetes |
30 g (~1 Canada Food Guide serving)/d* | 30 g | Meat and Alternatives
|
| Milk | Cancer: Colorectal | 2 cups/day †† | 1 cup (~257.8 g) | Milk and Alternatives (all soy beverages removed)
|
| Red Meat | Cancer: Colorectal Diabetes |
No more than 3 × 85 g servings/week (rounded this to <0.5 servings/day) ** | 75 g | Meat and Alternatives (all offal and meat not meeting the International Agency for Research on Cancer criteria for red meat were excluded):
|
| Processed Meat | Cancer: Colorectal Cardiovascular Disease: Ischemic Heart Disease Diabetes |
Only for special occasions (assumed 0.05 servings/day servings/day) ** Assumed those who usually consumed <0.25 servings/day had no elevated risk of disease |
75 g | Meat and Alternatives
|
| Sugar-Sweetened Beverages | Cancer: Esophagus; Thyroid; Liver; Pancreas; Colorectal; Breast (post-menopausal); Ovary, Uterus; Kidney; Leukemia Cardiovascular Disease: Ischemic Heart Disease; Ischemic Stroke; Hemorrhagic Stroke Diabetes Chronic Kidney Disease |
5 g g/day *** Assumed those who usually consumed <56.7 g/day had no elevated risk of disease. |
226.8 g | Beverages sweetened with sugar with ≥50 kcal/226.8 g were included from the following categories
|
CNF: Canadian Nutrient File, CFG: Canada’s Food Guide. † Based on recommendations from Canada’s Food Guide and the 2017 GBD; †† based on Canada’s Food Guide recommendations; * based on 2016 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult; ** based on Canadian Cancer Society recommendations; *** based on GBD 2013 recommendations.
2.2. Food Consumption Data Analysis
We extracted data on Canadians’ food consumption from the CCHS Cycle 2.2 (Nutrition) 2015, a cross-sectional national survey conducted by Statistics Canada in 2015. Respondents (n = 20,487) completed a 24-hour dietary recall, and of those respondents, 7623 (37%) completed a second recall. Details on sampling and data collection methodology are available elsewhere [23]. We excluded respondents that were <2 years of age, records where only breast milk or no foods were recorded, and records marked as invalid. In total, we included 24-hour dietary recall records from 19,797 respondents.
Established recommendations from the Canadian government outline a dietary pattern for Canadians to help meet nutrient requirements and prevent chronic diseases. In 2019, a new Canadian food guide was released, however Eating Well with Canada’s Food Guide (CFG 2007) was used in the present analysis, as it was in effect at the time of the survey [24]. Specific recommendations for four food groups (grain products, milk and alternatives, vegetables and fruits, meat and alternatives) and other dietary factors (water, fats, and oils) are outlined for each age and sex group. As all foods in our analysis (with the exception of SSB) are part of CFG food groups, we defined the consumption of these foods in CFG serving sizes.
To calculate the number of CFG servings from the 24-hour dietary recalls, we used the Canada Food Guide file, which categorizes all included foods according to Health Canada’s Canadian Nutrient File (CNF/CFG) tool [25,26]. The tool classifies foods into the four CFG groups and further subgroups. Within those subgroups, foods are tiered based on quantities of sodium, fat, and sugar. Foods in Tiers 1–3 count towards CFG servings, and foods in Tier 4 (higher in sugars, fat, and sodium) are generally not counted [26].
Table 1, column 1, presents the food groups included in our analyses. We included all foods belonging to each of the CFG groups, with a few exceptions. We excluded potatoes, corn, and fortified soy beverages from the relevant subgroups [27]. For red meat, only meat from the muscle of mammals (pork, beef, veal, lamb) that met the International Agency for Research on Cancer’s red meat definition were included [28]. For healthful foods, only those in Tiers 1–3 were included. For harmful foods, we included foods in Tier 1–4 [26]. Beverages in the CNF/CFG beverage subgroup with ≥50 kcal/226.8 g were included and considered as SSBs [27]. We assumed one serving of SSB was equal to 226.8 g (Table 1).
We assumed that complying with food recommendations was associated with the lowest disease risk. As CFG does not contain separate fruit and vegetable recommendations (only a combined recommendation), we estimated these using the GBD 2015 Theoretical Minimum Risk Exposure (TMRE). Vegetable and fruit servings were multiplied by ~0.63 and ~0.37 for vegetables and fruit, respectively [22]. As CFG age categories do not coincide with those in the EBIC economic cost calculations, we assumed the following: for individuals in the ≤14 years EBIC age category we used CFG recommendations for children 4–8 years, as this was the nearest to the middle of the EBIC category; for adult age groups, we used the CFG recommendation that applied to the majority of each EBIC age and sex group. As CFG does not have specific recommendations for consumption of processed meat, red meat, or nuts and seeds, we used established recommendations from other reliable Canadian organizations. For processed meat and red meat, Canadian Cancer Society recommendations were used (processed meat: only for special occasions, assumed <0.05 servings/day based on 2015 GBD TMRE; red meat: ≤385 g cooked servings/week) [29]. For nuts and seeds, the recommendation of 30 g/day (~1 CFG serving of nuts and seeds) from the 2016 Canadian Cardiovascular Society Guidelines [30] was used. For SSB, a recommendation of 5g/day was used, based on the 2015 GBD TMRE. Recommendations are summarized in Table 1.
We used the National Cancer Institute (NCI) method to estimate the usual intake distributions for each age and sex group [31]. Details on the method can be found elsewhere [31]. Similar to our previous study and others [21,32,33,34], we stratified the sample into children (≤14 years) and adults (≥15 years). However, because of a smaller sample size in 2015 CCHS compared to 2004, we were unable to run sex-stratified adult models, and instead used dummy variables. We used the model for food consumed non-episodically (i.e., consumed by almost everyone) for all foods except vegetables and milk, where a model for foods consumed episodically (i.e., not consumed daily by everyone) was used. For nuts and seeds models, only one-day intakes were used as few respondents consumed this food.
Using the NCI method, we estimated the number of servings of each food consumed by each EBIC age and sex group. Information on the proportion of the population consuming half CFG serving increments for all foods were obtained, with the exception of SSBs, where full serving increments were obtained. For foods with recommended intake near zero, we assumed consumption below the following cut-points was not associated with elevated risk: 56.7 g/day of SSB, 0.25 serving/day of processed meat, as accurate estimates below these cut-points could not be calculated.
2.3. Population Attributable Fraction Calculations
Similar to our previous approach, we calculated population attributable fractions (PAF) using dose–response RRs and food consumption data. PAFs estimate the fraction of disease cases that would be prevented if the exposure were to be eliminated from the population (i.e., if everyone complied with food recommendations) [35]. The standard PAF equation is: P(RR-1)/(P(RR-1) + 1), where P is the risk factor prevalence and RR is the relative risk of disease. However, as the extent to which each recommendation is met influences the disease risk, we used the method described by Krueger et al. to account for multiple risk exposure levels [35]. Further explanation of the equation can be found in our previous analysis [21].
Similar to our previous analysis, we calculated separate PAFs for each food and chronic disease combination by sex for each of the following age groups: ≤14 years, 15–34 years, 35–54 years, 55–64 years, 65–74 years, and ≥75 years. PAF values were then combined for each chronic disease. To avoid double counting, we used the following approach suggested by Krueger: combined PAF = 1-((1-PAF1)(1-PAF2)…(1-PAFn)) [35]. This approach assumes the risk factors are independent and the joint effects of the risk factors are multiplicative. This is the same approach we used previously and has been used to combine dietary risk factors previously [3,36,37].
2.4. Estimation of Direct Health Care and Indirect Costs
Direct health care costs for each age and sex group, including hospital, physician, and drug costs, associated with each chronic disease were retrieved from the 2008 EBIC [2]. Costs were then multiplied by 2018 National Health Expenditure Trends (i.e., costs in 2018 Canadians dollars ($) [38] to estimate more current direct health care costs. We used the modified human capital approach as outlined by Krueger et al. to estimate indirect health care costs (including those associated with mortality, long-term disability, and short-term disability) [35]. In short, using the 1998 EBIC [39], a ratio of total indirect health care to direct costs was calculated for each disease [21]. The calculated ratios were then multiplied by the 2018 direct costs to obtain indirect costs for each chronic disease by age and sex group. The direct and indirect costs were then multiplied by the relevant PAF to determine the costs attributable to unhealthy eating. To determine the economic burden attributable to individual foods, a disintegration step was applied [35,40]. All costs are reported in 2018 Canadian dollars ($).
Similar to Krueger et al. [41], a sensitivity analysis was conducted to estimate the upper and lower bounds of our cost estimates. To do this, we recalculated the PAFs using the 95% confidence intervals for all included relative risks. We conducted a second sensitivity analysis excluding the relationships between SSBs and cancers (leukemia, thyroid, liver, pancreatic, breast, ovarian, uterine, and kidney), as unlike the 2013 GBD [42], the 2017 GBD [3] did not provide the respective relative risks (see discussion section).
3. Results
Food recommendation adherence in the Canadian population is summarized by age and sex groups in Table 2. Healthful food recommendations met least often include (range of percent adherence in brackets): nuts and seeds (0.5–6.3%), whole grains (1.3–5.3%), and vegetables (0.8–7.2%). In comparison, more Canadians complied with recommendations for fruit (5.4–25.1%) and milk (2.1–21.1%). On average, Canadians were more likely to meet recommendations for harmful foods, adhering to recommendations for processed meat (18.8–40.5%), sugar-sweetened beverages (18.4–36.2%), and red meat (21.7–86.5%). Additional information on the Canadian population’s consumption of specific numbers of food servings can be found in Table S2.
Table 2.
Food recommendation adherence percentages of 2015 Canadian population stratified by age and sex.
| Canadian Population in 2018 (‘000) † | Healthful Foods (% Consuming at or Above Recommendation) |
Harmful Foods (% Consuming at or Below Recommendation) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Nuts and Seeds | Whole Grains | Fruit | Vegetables | Milk | Processed Meat †† | Sugar-Sweetened Beverages * | Red Meat | ||
| Females | |||||||||
| ≤14 years | 2780.6 | 1.1 | 4.8 | 19.0 | 15.9 | 27.6 | 49.3 | 15.8 | 70.1 |
| 15–34 years | 4703.0 | 1.5 | 1.6 | 5.8 | 5.8 | 9.7 | 67.0 | 24.6 | 59.2 |
| 35–54 years | 4989.7 | 3.1 | 1.6 | 8.7 | 13.4 | 6.0 | 70.6 | 48.7 | 44.2 |
| 55–64 years | 2378.0 | 4.3 | 2.4 | 8.9 | 15.7 | 4.7 | 78.4 | 57.7 | 42.0 |
| 65–74 years | 1629.2 | 1.9 | 1.5 | 9.0 | 13.1 | 5.5 | 73.2 | 61.7 | 48.0 |
| 75+ years | 1434.6 | 1.5 | 2.2 | 8.1 | 6.7 | 6.9 | 84.0 | 66.7 | 49.8 |
| Males | |||||||||
| ≤14 years | 2928.0 | 0.8 | 9.1 | 15.7 | 12.2 | 37.8 | 34.4 | 12.5 | 54.8 |
| 15–34 years | 4825.4 | 2.5 | 1.3 | 5.2 | 7.0 | 16.8 | 22.4 | 9.9 | 22.4 |
| 35–54 years | 5002.8 | 3.5 | 1.8 | 9.9 | 9.4 | 6.7 | 28.3 | 29.3 | 17.1 |
| 55–64 years | 2347.5 | 3.5 | 3.5 | 12.6 | 26.1 | 5.8 | 26.2 | 42.5 | 22.1 |
| 65–74 years | 1516.3 | 3.0 | 3.1 | 11.6 | 21.3 | 7.1 | 38.1 | 54.4 | 27.9 |
| 75+ years | 1005.1 | 2.8 | 2.8 | 9.4 | 17.4 | 11.8 | 51.2 | 68.9 | 36.3 |
† Statistics Canada 2018 [43], †† ≤0.25 servings/day; * <56.7 g/day.
Table 3 presents the combined PAF values for each disease. The combined PAF values were generally larger for males than females. The combined PAF values for diabetes and cardiovascular diseases (range: 14.5–94.4%) were generally higher than for chronic kidney disease and cancers (range: 0.1–24.9%). Additionally, combined PAF values for diabetes and cardiovascular diseases were generally larger for ages under 54 compared to 55 and over.
Table 3.
Combined population attributable fractions for foods with established food recommendations presented by age, sex, and chronic disease.
| Females | Males | Foods Included in Calculations | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤14 years | 15–34 years | 35–54 years | 55–64 years | 65–74 years | 75+ years | ≤14 years | 15–34 years | 35–54 years | 55–64 years | 65–74 years | 75+ years | ||
| Cancer | |||||||||||||
| Mouth | 2.3 | 5.8 | 5.5 | 5.2 | 5.3 | 5.4 | 2.4 | 6.1 | 5.7 | 5.5 | 5.6 | 5.6 | F |
| Larynx | 2.3 | 5.8 | 5.5 | 5.2 | 5.3 | 5.4 | 2.4 | 6.1 | 5.7 | 5.5 | 5.6 | 5.6 | F |
| Thyroid | 0.3 | 0.3 | 0.2 | 0.2 | 0.1 | 0.1 | 0.5 | 0.5 | 0.5 | 0.4 | 0.3 | 0.2 | SSB |
| Trachea, Lung, and Bronchus | 4.2 | 10.1 | 9.6 | 9.1 | 9.3 | 9.5 | 4.3 | 10.6 | 10.0 | 9.6 | 9.7 | 9.9 | F |
| Esophagus | 8.5 | 19.3 | 18.3 | 17.5 | 17.8 | 17.9 | 8.9 | 20.5 | 19.3 | 18.5 | 18.6 | 18.7 | F, SSB |
| Liver | 0.3 | 0.4 | 0.2 | 0.2 | 0.2 | 0.1 | 0.7 | 0.8 | 0.5 | 0.5 | 0.4 | 0.3 | SSB |
| Pancreas | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.2 | 0.2 | 0.2 | 0.1 | 0.1 | 0.1 | SSB |
| Colorectal | 15.4 | 18.5 | 19.4 | 19.8 | 19.0 | 18.5 | 16.9 | 23.5 | 23.9 | 24.9 | 23.2 | 22.6 | M, RM, PM, SSB |
| Kidney | 0.5 | 0.6 | 0.4 | 0.3 | 0.3 | 0.2 | 0.6 | 0.7 | 0.5 | 0.4 | 0.3 | 0.2 | SSB |
| Leukemia | 0.3 | 0.3 | 0.2 | 0.2 | 0.1 | 0.1 | 0.2 | 0.2 | 0.2 | 0.2 | 0.1 | 0.1 | SSB |
| Post-Menopausal Breast | 0.1 | 0.1 | 0.1 | SSB | |||||||||
| Ovary | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | SSB | ||||||
| Uterus | 1.0 | 1.0 | 0.7 | 0.6 | 0.5 | 0.3 | SSB | ||||||
| Cardiovascular Diseases | |||||||||||||
| Ischemic Heart Disease | 86.2 | 86.8 | 64.1 | 54.1 | 47.2 | 41.7 | 88.3 | 93.0 | 73.9 | 60.5 | 53.1 | 46.6 | F, V, WG, NS, PM, SSB |
| Ischemic Stroke | 76.4 | 89.9 | 61.9 | 47.3 | 34.0 | 14.5 | 76.5 | 94.4 | 70.5 | 50.5 | 36.2 | 15.5 | F, V, WG, SSB |
| Hemorrhagic Stroke | 62.9 | 79.5 | 56.4 | 46.8 | 37.0 | 17.1 | 63.2 | 86.3 | 64.8 | 49.9 | 39.3 | 18.3 | F, V, WG, SSB |
| Diabetes | 64.1 | 70.4 | 54.8 | 45.9 | 37.3 | 23.6 | 71.5 | 83.2 | 68.4 | 57.9 | 47.5 | 30.6 | F, WG, NS, RM, PM, SSB |
| Chronic Kidney Disease | 1.2 | 1.2 | 0.8 | 0.7 | 0.5 | 0.2 | 1.4 | 1.6 | 1.1 | 1.0 | 0.7 | 0.3 | SSB |
F = fruit; V = vegetables; M = milk; WG = whole grains; NS = nuts and seeds; RM = red meat; PM = processed meat; SSB = sugar-sweetened beverages.
We estimated not meeting food recommendations for five healthful and three harmful foods to be responsible for a total economic burden of $15.8 billion (Table 4). Of this total, direct health care costs amounted to $5.9 billion and indirect costs constituted $9.9 billion of the burden. Table 4 is stratified by sex, and further separated by direct and indirect health care costs. The total economic burden of not meeting recommendations for each food is presented and further stratified by the diseases contributing to the burden. The summed total costs for each food are presented on the right of Table 4, with the total direct and indirect costs for males and females at the bottom of the table. Not complying with food recommendations accounted for approximately 3.93% of all hospital, physician, and drug costs in 2018. Men had over twice the costs of women, with $4.1 billion and $1.8 billion direct costs, and $6.8 billion and $3.1 billion indirect health care costs, respectively. Out of the economic burden attributable to poor diet, 58% of estimated health care costs were attributable to ischemic heart disease ($3.4 billion in direct health care costs, $5.7 billion indirect costs). Type 2 diabetes and colon/rectal cancer were also substantial contributors with $4.1 billion and $1.2 billion total direct and indirect costs, respectively. Fewer of the estimated costs were attributable to other cancers ($520 million), chronic kidney disease ($5.3 million), and stroke ($904 million). Using the 95% confidence intervals from the relative risks in our PAF calculations, we performed a sensitivity analysis and obtained the low and high estimates of the total economic burden cost to be $7.9 billion and $21.2 billion, respectively. The low to high estimate intervals for the direct and indirect costs were $3.0–7.8 billion and $4.9–13.5 billion, respectively.
Table 4.
Economic burden in Canada in 2018 of the eight foods that have established recommendations.
| 2018 Costs ($CAN) | |||||||
|---|---|---|---|---|---|---|---|
| Females | Males | Females and Males | |||||
| Direct Costs | Indirect Costs | Direct Costs | Indirect Costs | Direct Costs | Indirect Costs | Total Direct Health and Indirect Costs | |
| Whole Grains | 479,696,161 | 732,962,516 | 1,013,846,354 | 1,592,873,190 | 1,493,542,514 | 2,325,835,706 | 3,819,378,221 |
| Ischemic Heart Disease | 231,644,786 | 404,966,223 | 608,802,593 | 1,064,321,328 | 840,447,379 | 1,469,287,550 | 2,309,734,929 |
| Ischemic Stroke | 28,258,369 | 49,401,867 | 41,805,494 | 73,085,232 | 70,063,862 | 122,487,098 | 192,550,961 |
| Hemorrhagic Stroke | 22,328,761 | 39,035,604 | 27,651,485 | 48,340,901 | 49,980,247 | 87,376,505 | 137,356,752 |
| Diabetes | 197,464,245 | 239,558,823 | 335,586,782 | 407,125,730 | 533,051,027 | 646,684,553 | 1,179,735,579 |
| Nuts and Seeds | 498,432,254 | 782,751,451 | 954,697,875 | 1,546,309,433 | 1,453,130,129 | 2,329,060,883 | 3,782,191,012 |
| Ischemic Heart Disease | 332,804,780 | 581,816,223 | 725,346,710 | 1,268,066,174 | 1,058,151,490 | 1,849,882,397 | 2,908,033,887 |
| Diabetes | 165,627,474 | 200,935,227 | 229,351,164 | 278,243,259 | 394,978,638 | 479,178,486 | 874,157,125 |
| Fruit | 326,305,644 | 596,430,274 | 576,656,369 | 1,049,843,530 | 902,962,012 | 1,646,273,804 | 2,549,235,816 |
| Mouth Cancer | 1,728,793 | 8,442,531 | 3,812,495 | 18,618,252 | 5,541,288 | 27,060,783 | 32,602,071 |
| Laryngeal Cancer | 476,108 | 2,325,065 | 2,075,830 | 10,137,280 | 2,551,938 | 12,462,345 | 15,014,283 |
| Esophageal Cancer | 2,936,399 | 14,339,852 | 9,816,589 | 47,939,145 | 12,752,988 | 62,278,997 | 75,031,985 |
| Tracheal, Bronchial and Lung Cancer | 21,104,161 | 103,061,806 | 23,602,668 | 115,263,226 | 44,706,829 | 218,325,032 | 263,031,861 |
| Ischemic Heart Disease | 137,370,373 | 240,153,738 | 317,238,513 | 554,602,952 | 454,608,886 | 794,756,690 | 1,249,365,576 |
| Ischemic Stroke | 32,067,357 | 56,060,819 | 40,893,335 | 71,490,577 | 72,960,692 | 127,551,396 | 200,512,088 |
| Hemorrhagic Stroke | 25,378,191 | 44,366,681 | 26,858,418 | 46,954,444 | 52,236,609 | 91,321,125 | 143,557,734 |
| Diabetes | 105,244,262 | 127,679,781 | 152,358,521 | 184,837,656 | 257,602,783 | 312,517,437 | 570,120,219 |
| Processed Meat | 146,720,962 | 240,898,174 | 693,784,426 | 1,158,558,074 | 840,505,388 | 1,399,456,248 | 2,239,961,636 |
| Colon and Rectal Cancer | 7,435,911 | 36,313,146 | 27,537,031 | 134,476,619 | 34,972,943 | 170,789,766 | 205,762,708 |
| Ischemic Heart Disease | 66,551,012 | 116,345,861 | 403,342,304 | 705,131,386 | 469,893,316 | 821,477,247 | 1,291,370,563 |
| Diabetes | 72,734,038 | 88,239,168 | 262,905,091 | 318,950,068 | 335,639,129 | 407,189,236 | 742,828,365 |
| Vegetables | 190,257,302 | 332,611,764 | 436,385,955 | 762,898,984 | 626,643,257 | 1,095,510,748 | 1,722,154,005 |
| Ischemic Heart Disease | 166,710,242 | 291,446,305 | 405,516,582 | 708,932,505 | 572,226,824 | 1,000,378,809 | 1,572,605,633 |
| Ischemic Stroke | 13,301,355 | 23,253,704 | 17,991,402 | 31,452,942 | 31,292,757 | 54,706,647 | 85,999,403 |
| Hemorrhagic Stroke | 10,245,706 | 17,911,755 | 12,877,971 | 22,513,537 | 23,123,677 | 40,425,292 | 63,548,969 |
| Sugar-Sweetened Beverages | 109,485,809 | 140,609,158 | 255,443,721 | 324,647,983 | 364,929,531 | 465,257,142 | 830,186,672 |
| Esophageal Cancer | 49,594 | 242,189 | 270,047 | 1,318,772 | 319,641 | 1,560,961 | 1,880,602 |
| Thyroid Cancer | 76,400 | 373,097 | 54,084 | 264,117 | 130,484 | 637,214 | 767,698 |
| Liver Cancer | 9898 | 48,336 | 80,200 | 391,655 | 90,098 | 439,991 | 530,089 |
| Pancreatic Cancer | 43,910 | 214,434 | 59,525 | 290,688 | 103,435 | 505,122 | 608,556 |
| Colorectal Cancer | 170,942 | 834,793 | 1,018,775 | 4,975,168 | 1,189,717 | 5,809,961 | 6,999,677 |
| Breast Cancer | 347,638 | 1,697,684 | 347,638 | 1,697,684 | 2,045,322 | ||
| Ovarian Cancer | 25,635 | 125,189 | 25,635 | 125,189 | 150,824 | ||
| Uterine Cancer | 380,325 | 1,857,312 | 380,325 | 1,857,312 | 2,237,637 | ||
| Kidney Cancer | 290,291 | 1,417,629 | 192,135 | 938,286 | 482,425 | 2,355,915 | 2,838,340 |
| Leukemia | 196,821 | 961,173 | 179,011 | 874,199 | 375,833 | 1,835,372 | 2,211,205 |
| Ischemic Heart Disease | 4,228,109 | 7,391,669 | 15,693,878 | 27,436,363 | 19,921,987 | 34,828,032 | 54,750,019 |
| Ischemic Stroke | 463,246 | 809,857 | 966,438 | 1,689,547 | 1,429,684 | 2,499,404 | 3,929,088 |
| Hemorrhagic Stroke | 697,652 | 1,219,649 | 1,089,408 | 1,904,525 | 1,787,059 | 3,124,174 | 4,911,233 |
| Diabetes | 101,401,444 | 123,017,768 | 234,020,470 | 283,907,948 | 335,421,915 | 406,925,716 | 742,347,631 |
| Chronic Kidney Disease | 1,103,904 | 398,379 | 1,819,751 | 656,715 | 2,923,655 | 1,055,094 | 3,978,750 |
| Milk | 50,108,728 | 244,705,113 | 63,055,698 | 307,931,418 | 113,164,426 | 552,636,531 | 665,800,957 |
| Colon and Rectal Cancer | 50,108,728 | 244,705,113 | 63,055,698 | 307,931,418 | 113,164,426 | 552,636,531 | 665,800,957 |
| Red Meat | 17,465,576 | 32,182,526 | 63,406,702 | 117,840,630 | 80,872,278 | 150,023,157 | 230,895,435 |
| Colon and Rectal Cancer | 2,995,312 | 14,627,554 | 11,148,157 | 54,441,833 | 14,143,469 | 69,069,386 | 83,212,855 |
| Diabetes | 14,470,264 | 17,554,973 | 52,258,546 | 63,398,798 | 66,728,810 | 80,953,770 | 147,682,580 |
| TOTAL COSTS | 1,818,472,435 | 3,103,150,976 | 4,057,277,100 | 6,860,903,243 | 5,875,749,535 | 9,964,054,219 | 15,839,803,754 |
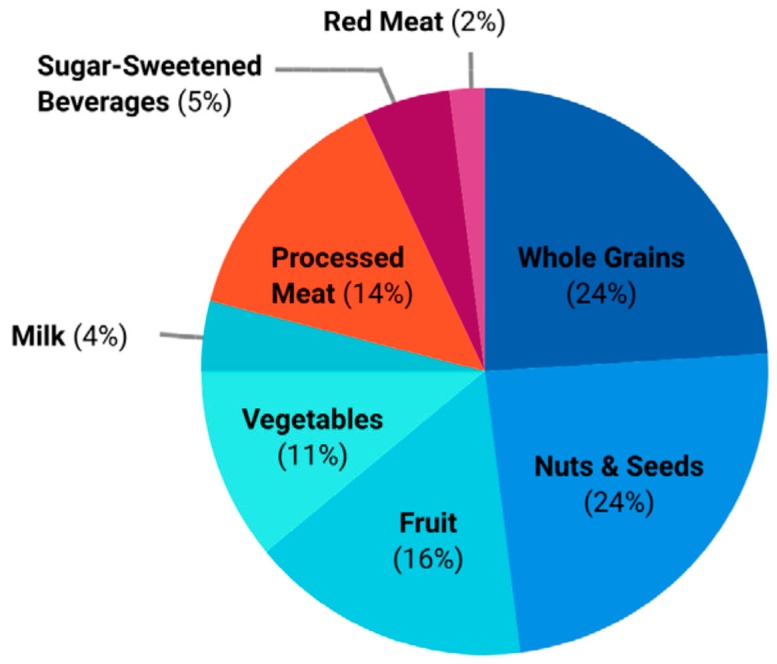
The estimated economic burden of Canadians not consuming adequate amounts of recommended healthful foods (fruit, vegetables, nuts and seeds, whole grains, milk) greatly exceeded the economic burden of overconsumption of harmful foods (processed meat, red meat, SSBs) ($12.5 billion vs. $3.3 billion) (Table 4). Inadequate consumption of whole grains and nuts and seeds accounted for almost half of the economic burden attributable poor diet, with each accounting for over $1.4 billion and $2.3 billion in direct and indirect health care costs, respectively. Inadequate consumption of fruit and excess consumption of processed meat were each responsible for an estimated 14–16% of direct and indirect health care costs. Inadequate consumption of vegetables and excess consumption of SSBs were each, respectively, responsible for an estimated 10% and 4–6% of direct and indirect health care costs. Red meat and milk and were responsible for the lowest estimated economic burden at <5% (Table 4). The proportion of the economic burden attributable to each food is summarized in Figure 1.
Figure 1.
Proportion of CAD$15.8 billion economic burden attributable to not meeting established food recommendations.
Table 5 presents the estimated direct and indirect economic burden attributable to poor diet by age and sex groups. Men were responsible for 66.9% of the economic burden ($10.6 billion) and men in age groups 35–54 and 55–64 were responsible for the largest proportion of the economic burden at 25.7% and 27.2%, respectively. Among women, those aged 65–74 and 75 and over were responsible for the largest proportion of the economic burden at 25.2% and 29.8%, respectively. Overall, men aged 55–64 alone were responsible for the largest proportion of the total burden at 18.2% (Table 5).
Table 5.
Economic burden in Canada in 2018 by age and sex groups.
| 2018 Costs ($CAN) | Percent of Costs | ||||
|---|---|---|---|---|---|
| Direct Costs | Indirect Costs | Total Direct and Indirect Costs | Costs within Sex Group | Total Costs | |
| Females | 1,936,570,565 | 3,302,166,717 | 5,238,737,282 | 100.0% | 33.1% |
| ≤14 years | 12,040,403 | 15,666,224 | 27,706,627 | 0.5% | 0.2% |
| 15–34 years | 76,513,918 | 100,906,919 | 177,420,837 | 3.4% | 1.1% |
| 35–54 years | 386,859,501 | 595,385,456 | 982,244,957 | 18.7% | 6.2% |
| 55–64 years | 440,519,124 | 728,965,831 | 1,169,484,955 | 22.3% | 7.4% |
| 65–74 years | 480,354,720 | 840,813,557 | 1,321,168,277 | 25.2% | 8.3% |
| 75+ years | 540,282,899 | 1,020,428,729 | 1,560,711,628 | 29.8% | 9.9% |
| Males | 3,939,178,970 | 6,661,887,503 | 10,601,066,473 | 100.0% | 66.9% |
| ≤14 years | 24,667,689.36 | 31,113,645.39 | 55,781,335 | 0.5% | 0.4% |
| 15–34 years | 87,878,603 | 118,808,699 | 206,687,302 | 1.9% | 1.3% |
| 35–54 years | 1,076,934,563 | 1,651,501,848 | 2,728,436,411 | 25.7% | 17.2% |
| 55–64 years | 1,074,108,771 | 1,808,010,348 | 2,882,119,119 | 27.2% | 18.2% |
| 65–74 years | 972,731,815 | 1,717,252,172 | 2,689,983,987 | 25.4% | 17.0% |
| 75+ years | 702,857,528 | 1,335,200,790 | 2,038,058,318 | 19.2% | 12.9% |
| All years | 3,939,178,970 | 6,661,887,503 | 10,601,066,473 | 100.0% | 66.9% |
4. Discussion
We estimated that a total of $15.8 billion in direct and indirect health care costs could potentially be avoided if Canadians fully complied with established food recommendations. Our sensitivity analysis revealed this economic burden could be as low as $7.9 billion or high as $21.2 billion. Out of the eight foods considered, inadequate consumption of whole grains and nuts and seeds were the largest contributors, together accounting for over half of the burden.
Our estimates reinforce diet as one of the larger contributors to the economic burden of chronic disease, alongside excess bodyweight, tobacco smoking, and physical inactivity. In 2012, the economic burden for each of these latter risk factors were estimated to be $23.5 billion, $19.5 billion, and $10.6 billion, respectively [41]. These estimates also used PAFs and similar cost estimation methods, however they took a broader approach to costs and included those of other health care expenditures, other health professionals, and health research, in addition to the hospital care, physician, and drug costs for each disease. If we had included all the costs considered by Kruger et al. in our present study, our estimate could be 30% to 50% higher ($20.5–23.7 billion) [41]. Nevertheless, our estimate of $15.8 billion positions unhealthy diet after the burden of smoking and higher than the burden of physical inactivity. The upper end of our sensitivity analysis ($21.2 billion) would position the burden of unhealthy eating just after that of excess weight and even more costly than the economic burden of smoking.
Putting the estimates for the economic burden of poor diets in Canada in perspective, the most recent estimate before ours was conducted over 20 years ago and revealed the costs to be $6.6 billion in 1998. Our previous estimate of $13.8 billion using 2004 data and our current estimate of $15.8 billion using 2015 data and 2018 costs, depict the economic burden of chronic disease attributable to poor diet as steadily increasing. On the contrary, in Nshimyumukiza et al.’s [18] analysis of the economic burden of poor diet quality in terms of the Healthy Eating Index, the temporal changes in Canadians’ diets from 2004 to 2015 were found to improve, translating to a $133 million decrease in economic burden ($13.21 billion vs. $13.08 billion). This study noted that the economic burden decreased among males, but increased among females ($333 million) and among those over 65 years ($200 million). In the present study, the proportion of men’s costs compared to women’s costs showed marginal improvements when compared to our previous estimates (66.9% vs. 67.3%). However, men aged 55–64 remained the most burdensome, accounting for 18.2% of the total economic burden. The elderly (men and women over the age of 65 combined) were responsible for 48% of the total costs in the present analysis, a slight increase from our previous analysis, where they were responsible for 46% of the burden. In general, the proportion of costs between age and sex groups remained substantially similar over time.
The $3 billion (22%) increase from our estimate in 2014 to the present estimate appears dramatic. When we eliminate inflation and the general increase in health care costs over the last four years by using the 2014 National Health Expenditure Trends in the present models [38], the economic burden is estimated to be $13.89 billion, an increase of only $90 million from our previous estimate. Additionally, discrepancies between the 2004 and 2015 CCHS data have come to light, with a 250 kcal lower energy intake across the entire 2015 sample compared to 2004 [44]. This lower energy intake was consistent across all categories of respondents for many foods, including SSBs, meat, milk, and cereal grains. However, energy intake was higher for nuts [44]. As our analysis depends on both consuming enough of certain foods while limiting others, the effect of underreporting (on all foods except nuts) has bidirectional effects on our estimate and complicates comparisons between studies. The same issues in comparison between the 2004 and 2015 CCHS may exist in Nshimyumukiza et al.’s analysis, and it is not known if a 250 kcal decrease in 2015 influenced the apparent improvement in diet quality. However, the assessment of diet quality in terms of the HEI score may have circumvented inaccuracies in the 2015 CCHS estimation of quantity. Comparison issues aside, this study also found the majority of Canadians have a poor-quality diet that results in an attributable high economic burden, and that there is little evidence of substantial change between 2004 and 2015.
We revealed that the highest proportion of the economic burden resulted from inadequate intake of nuts and seeds, whole grains, and fruit. These proportions appeared similar to those based on the 2004 CCHS data [20]. In contrast, in the present analysis using the 2015 data (vs. using the 2004 data), vegetables (10.9% vs. 8.5%) and SSBs (6.3% vs. 5.2%) had higher proportions of attributable burden, while costs due to red meat consumption decreased slightly (1.5% vs. 2.9%). The total costs of processed meat and milk remained proportionally similar. Concordant with Nshimyumukiza et al.’s temporal analysis of diet quality in Canada, our analysis reveals little evidence of substantial change in Canadians’ diets [18].
It is possible that inadequate consumption of whole grains and the associated increase in economic burden could be due to the rise of gluten-free and low-carbohydrate diets in the past decade [45,46]. Gluten is a protein found in a variety of grains, including wheat, rye, and barley. Some individuals have an intolerance to gluten and individuals with Celiac disease have an autoimmune reaction and can experience severe side effects if they consume the protein. In Canada, approximately 1% of the population has Celiac disease and an additional 1–6% report gluten sensitivity, however the true prevalence is difficult to establish as non-Celiac gluten sensitivity is often self-diagnosed [45,47]. An estimated 25% of American consumers reported consuming gluten-free food in 2015, and it is likely Canadian consumption of gluten free food was similar [48]. It is still possible to meet whole grain recommendations by consuming non-gluten whole grains such as buckwheat, millet, and quinoa, however those individuals on low carbohydrate diets are unlikely to consume these carbohydrate-containing items. Thus, the popularity of gluten-free and low-carbohydrate diets in Canada is likely responsible for the, on average, lower consumption of whole grains and for an increase in economic burden.
The present analysis used the 2017 GBD dietary- and disease-relative risks for all food–disease combinations except for SSBs. The 2013 GBD dietary risks were used instead for SSBs, as the 2017 risks are no longer presented in standard serving units (226.8 g/day). To reflect that unlike the 2013 GBD, the 2017 report does not present risks for SSBs and cancers, a sensitivity analysis was conducted to estimate the cost when the cost of these cancers are not included. We found these cancers only account for 4% ($39.5 million) of the total economic burden of excess consumption of SSBs ($996 million).
Our study suggests that investment in promotion of healthy eating has the potential of substantial savings in direct and indirect health care costs. The present analysis provides information on economic benefits of what is to gain if Canadians were to eat according to established recommendations, and gives direction and guidance to health promotion. We revealed which specific food group yielded the biggest economic burden; these food groups, whole grains, nuts and seeds, and fruit, should receive priority. We also revealed that 79.2% of the economic burden is caused by underconsumption of healthful foods and 20.8% by overconsumption of harmful foods, suggesting that promotion of healthful foods, rather than restricting or taxing harmful foods, has the bigger potential to reduce the risk for chronic disease and associated economic burden. We further identified those age and sex groups wherein improving their diets could yield the greatest improvement in chronic disease prevention and reduction in economic burden. Whereas it is clear that investments in effective health promotion may result in enormous cost savings, it is not the only sector that needs attention [6]. Strategizing food production is essential to ensure the availability of healthy foods [6]. The latter issue is not uncomplicated in light of the demands for agricultural lands to ensure sustainable food production to meet the Western food recommendations [49].
There are several strengths in the present study. We used 24-hour dietary recalls from a large representative sample of the Canadian population. Only those foods identified by the GBD to cause chronic disease were included. We considered multiple dietary components, however our estimation was limited by not including the costs associated with over- and underconsumption of nutrients (e.g., fiber, sodium, fat). Established limitations of dietary research apply to the present study: assessment of dietary intake relies on self-report, which is susceptible to error (e.g., over-reporting of healthy foods and under-reporting of unhealthy foods), and reporting of food frequency does not directly translate into absolute consumption. In addition, we assumed the costs by disease and the ratio of indirect to direct costs did not change over time. However, this assumption has been made in other similar studies [6,7,40,50]. Our results do not estimate the lifetime costs of not complying with established food recommendations, a limitation of all prevalence-based studies. The use of an incidence-based approach would have allowed for the estimate of lifetime costs. However, given that many of the chronic diseases included have a long duration, and would require a long follow-up, the prevalence-based approach was appropriate. Lastly, our characterization of the economic burden may represent an underestimation, as we limited our direct cost estimation to hospital, physician, and drug costs and did not include costs related to other health care expenditures and health professionals, which have been included in some previous Canadian studies [7,41].
5. Conclusions
The economic burden due to unhealthy eating has remained very high over the last 11 years, despite the health promotion efforts to improve diet quality. Relatively small dietary changes at the population level can amount to substantial cost savings. Policy and decision makers are encouraged to develop more effective targeted nutritional programs to limit consumption of harmful foods, and in particular, promote consumption of healthful foods such as whole grains and nuts and seeds.
Acknowledgments
We would like to extend great thanks to Jessica R.L. Lieffers for her contributions to the conceptualization and methodology of the present study, and to Irene Wong (University of Alberta Research Data Centre Analyst) for her assistance in accessing the Canadian Community Health Survey Data.
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6643/11/10/2529/s1, Table S1: Relative risks from Global Burden of Disease 2013 and 2017, used in analyses; Table S2: Percentages of the 2015 Canadian population by age, sex, and level of food intake.
Author Contributions
Conceptualization, J.P.E., O.K.L., A.O., and P.J.V.; methodology, J.P.E., O.K.L., A.O., and P.J.V.; software, O.K.L.; validation, O.K.L. and J.P.E.; formal analysis, O.K.L.; investigation, O.K.L.; resources, P.J.V. and A.O.; data curation, O.K.L.; writing—original draft preparation, O.K.L.; writing—review and editing, J.P.E., A.O. and P.J.V.; visualization, O.K.L.; supervision, A.O. and P.J.V.; funding acquisition, P.J.V. and A.O.
Funding
This research was funded by the Collaborative Research and Innovative Opportunities (CRIO) Team program from Alberta Innovates (AI), grant number 201300671 to P.J.V. and A.O. All interpretations and opinions in the present study are those of the authors. Although the research and analysis are based on data from Statistics Canada, the opinions expressed do not represent the views of Statistics Canada or the Canadian Research Data Centre Network (CRDCN).
Conflicts of Interest
The authors have declared that no conflict of interest exist.
References
- 1.Statistics Canada Leading Causes of Death, Total Population, by Age Group. [(accessed on 28 June 2019)]; Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310039401.
- 2.Public Health Agency of Canada . Government of Canada; Ottawa, ON, Canada: 2014. [(accessed on 10 May 2018)]. Economic Burden of Illness in Canada, 2005–2008; pp. 1–111. Available online: http://www.phac-aspc.gc.ca/publicat/ebic-femc98/pdf/ebic1998.pdf. [Google Scholar]
- 3.Stanaway J.D., Afshin A., Gakidou E., Lim S.S., Abate D., Hassen Abate K., Abbafati C., Abbasi N., Abbastabar H., Abd-Allah F., et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. [(accessed on 17 May 2019)];Lancet. 2018 392 doi: 10.1016/S0140-6736(18)32225-6. Available online: www.thelancet.com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.IHME Country Profile: Canada. Top 10 Risks Contributing to DALYS in 2016 and Percent Change, 2005–2016, All Ages. [(accessed on 5 July 2019)]; Available online: http://www.healthdata.org/canada.
- 5.Afshin A., Sur P.J., Fay K.A., Cornaby L., Ferrara G., Salama J.S., Mullany E.C., Abate K.H., Abbafati C., Abebe Z., et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. [(accessed on 20 April 2019)];Lancet. 2019 393:1958–1972. doi: 10.1016/S0140-6736(19)30041-8. Available online: https://linkinghub.elsevier.com/retrieve/pii/S0140673619300418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ekwaru J.P., Ohinmaa A., Loehr S., Setayeshgar S., Thanh N.X., Veugelers P.J. The economic burden of inadequate consumption of vegetables and fruit in Canada. [(accessed on 15 May 2018)];Public Health Nutr. 2016 20:1–9. doi: 10.1017/S1368980016002846. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5426323/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krueger H., Koot J., Andres E. The economic benefits of fruit and vegetable consumption in Canada. [(accessed on 5 July 2019)];Can. J. Public Health. 2017 108:e152–e161. doi: 10.17269/CJPH.108.5721. Available online: http://www.ncbi.nlm.nih.gov/pubmed/28621651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doidge J.C., Segal L., Gospodarevskaya E. Attributable Risk Analysis Reveals Potential Healthcare Savings from Increased Consumption of Dairy Products. [(accessed on 5 July 2019)];J. Nutr. 2012 142:1772–1780. doi: 10.3945/jn.111.154161. Available online: https://academic.oup.com/jn/article/142/9/1772/4630973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCarron D., Heaney R.P. Estimated healthcare savings associated with adequate dairy food intake. [(accessed on 5 July 2019)];Am. J. Hypertens. 2004 17:88–97. doi: 10.1016/j.amjhyper.2003.08.008. Available online: https://academic.oup.com/ajh/article-lookup/doi/10.1016/j.amjhyper.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 10.Barnard N.D., Nicholson A., Howard J.L. The Medical Costs Attributable to Meat Consumption. [(accessed on 5 July 2019)];Prev. Med. 1995 24:646–655. doi: 10.1006/pmed.1995.1100. Available online: https://www.sciencedirect.com/science/article/pii/S0091743585711000?via%3Dihub. [DOI] [PubMed] [Google Scholar]
- 11.Abdullah M.M.H., Gyles C.L., Marinangeli C.P.F., Carlberg J.G., Jones P.J.H. Cost-of-illness analysis reveals potential healthcare savings with reductions in type 2 diabetes and cardiovascular disease following recommended intakes of dietary fiber in Canada. [(accessed on 5 July 2019)];Front. Pharmacol. 2015 6:167. doi: 10.3389/fphar.2015.00167. Available online: http://journal.frontiersin.org/Article/10.3389/fphar.2015.00167/abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meier T., Deumelandt P., Christen O., Stangl G.I., Riedel K., Langer M. Global Burden of Sugar-Related Dental Diseases in 168 Countries and Corresponding Health Care Costs. [(accessed on 5 July 2019)];J. Dent. Res. 2017 96:845–854. doi: 10.1177/0022034517708315. Available online: http://journals.sagepub.com/doi/10.1177/0022034517708315. [DOI] [PubMed] [Google Scholar]
- 13.Jones A.C., Veerman J.L., Hammond D. The Health and Economic Impact of a Tax on Sugary Drinks in Canada. University Waterloo; Waterloo, ON, Canada: 2017. [(accessed on 15 May 2018)]. pp. 1–77. Available online: https://www.diabetes.ca/getattachment/Newsroom/Latest-News/Will-a-sugary-drinks-levy-benefit-Canadians/The-Health-and-Economic-Impact-of-a-Sugary-Drinks-Tax.pdf.aspx. [Google Scholar]
- 14.Candari C.J., World Health Organization. Cylus J., Nolte E., European Observatory on Health Systems and Policies . Assessing the Economic Costs of Unhealthy Diets and Low Physical Activity an Evidence Review and Proposed Framework. World Health Organization; Geneva, Switzerland: 2017. [PubMed] [Google Scholar]
- 15.Scarborough P., Bhatnagar P., Wickramasinghe K.K., Allender S., Foster C., Rayner M. The economic burden of ill health due to diet, physical inactivity, smoking, alcohol and obesity in the UK: An update to 2006-07 NHS costs. [(accessed on 5 July 2019)];J. Public Health (Bangk.) 2011 33:527–535. doi: 10.1093/pubmed/fdr033. Available online: https://academic.oup.com/jpubhealth/article-lookup/doi/10.1093/pubmed/fdr033. [DOI] [PubMed] [Google Scholar]
- 16.Frazao E. High Costs of Poor Eating Patterns in the United States. [(accessed on 8 July 2019)];Agric. Inf. Bull. 1999 :494. Available online: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.467.3556&rep=rep1&type=pdf. [Google Scholar]
- 17.Health Canada Food and Nutrition Surveillance in Canada: An Environmental Scan. [(accessed on 16 October 2019)];2000 Available online: https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/food-nutrition-surveillance-canada-environmental-scan-health-canada-2000.html.
- 18.Nshimyumukiza L., Lieffers J.R.L., Ekwaru J.P., Ohinmaa A., Veugelers P.J. Temporal changes in diet quality and the associated economic burden in Canada. [(accessed on 22 November 2018)];PLoS ONE. 2018 13:e0206877. doi: 10.1371/journal.pone.0206877. doi: 10.1371/journal.pone.0206877. Available online: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Renzella J., Townsend N., Jewell J., Breda J., Roberts N., Rayner M., Wickramasinghe K. What National and Subnational Interventions and Policies Based on Mediterranean and Nordic Diets are Recommended or Implemented in the WHO European Region, and Is There Evidence of Effectiveness in Reducing Noncommunicable Diseases? WHO Regional Office for Europe; Copenhagen, Danmark: 2018. Health Evidence Network Synthesis Report. [PubMed] [Google Scholar]
- 20.Garriguet D. Canadians’ eating habits. Health Rep. 2007;18:17–32. [PubMed] [Google Scholar]
- 21.Lieffers J.R.L., Ekwaru J.P., Ohinmaa A., Veugelers P.J. The economic burden of not meeting food recommendations in Canada: The cost of doing nothing. [(accessed on 28 August 2018)];PLoS ONE. 2018 13:e0196333. doi: 10.1371/journal.pone.0196333. doi: 10.1371/journal.pone.0196333. Available online: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forouzanfar M.H., Afshin A., Alexander L.T., Anderson H.R., Bhutta Z.A., Biryukov S., Brauer M., Burnett R., Cercy K., Charlson F.J., et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. [(accessed on 5 July 2019)];Lancet. 2016 388:1659–1724. doi: 10.1016/S0140-6736(16)31679-8. Available online: https://www.sciencedirect.com/science/article/pii/S0140673616316798?via%3Dihub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Health Canada Reference Guide to Understanding and Using the Data 2015 Canadian Community Health Survey-Nutrition. [(accessed on 9 July 2019)];2017 Available online: https://www.canada.ca/content/dam/hc-sc/documents/services/food-nutrition/food-nutrition-surveillance/ReferenceGuide2015CCHS-Nutr_Eng_Final_06192017.pdf.
- 24.Health Canada Eating Well with Canada’s Food Guide. [(accessed on 6 June 2019)];2007 Available online: https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/fn-an/alt_formats/hpfb-dgpsa/pdf/food-guide-aliment/print_eatwell_bienmang-eng.pdf.
- 25.Elvidge Munene L.A., Dumais L., Esslinger K., Jones-Mclean E., Mansfield E., Verreault M.-F., Villeneuve M., Miller D. A surveillance tool to assess diets according to Eating Well with Canada’s Food Guide. [(accessed on 15 May 2018)];Health Rep. 2015 26:12–20. Available online: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed16&NEWS=N&AN=611137297. [PubMed] [Google Scholar]
- 26.Health Canada The Development and Use of a Surveillance Tool: The Classification of Foods in the Canadian Nutrient File according to Eating Well with Canada’s Food Guide. [(accessed on 16 July 2019)];:25. Available online: http://publications.gc.ca/site/eng/9.698720/publication.html.
- 27.Micha R., Kalantarian S., Wirojratana P., Byers T., Danaei G., Elmadfa I., Ding E., Giovannucci E., Powles J., Smith-Warner S., et al. Estimating the global and regional burden of suboptimal nutrition on chronic disease: Methods and inputs to the analysis. [(accessed on 26 September 2019)];Eur. J. Clin. Nutr. 2012 66:119–129. doi: 10.1038/ejcn.2011.147. Available online: http://www.nature.com/articles/ejcn2011147. [DOI] [PubMed] [Google Scholar]
- 28.International Agency for Research on Cancer IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. [(accessed on 16 July 2019)]; Available online: https://monographs.iarc.fr/
- 29.Canadian Cancer Society Red and Processed Meat. [(accessed on 2 May 2019)]; Available online: http://www.cancer.ca/en/prevention- and-screening/live-well/nutrition-and-fitness/eating-well/red-and-processed-meat/?region=on.
- 30.Anderson T.J., Grégoire J., Pearson G.J., Barry A.R., Couture P., Dawes M., Francis G.A., Genest J., Grover S., Gupta M., et al. 2016 Canadian Cardiovascular Society Guidelines for the Management of Dyslipidemia for the Prevention of Cardiovascular Disease in the Adult. [(accessed on 16 July 2019)];Can. J. Cardiol. 2016 32:1263–1282. doi: 10.1016/j.cjca.2016.07.510. Available online: https://www.sciencedirect.com/science/article/pii/S0828282×16307322?via%3Dihub. [DOI] [PubMed] [Google Scholar]
- 31.Tooze J.A., Midthune D., Dodd K.W., Freedman L.S., Krebs-Smith S.M., Subar A.F., Guenther P.M., Carroll R.J., Kipnis V. A New Statistical Method for Estimating the Usual Intake of Episodically Consumed Foods with Application to Their Distribution. [(accessed on 16 July 2019)];J. Am. Diet. Assoc. 2006 106:1575–1587. doi: 10.1016/j.jada.2006.07.003. Available online: https://www.sciencedirect.com/science/article/pii/S0002822306016907?via%3Dihub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kirkpatrick S.I., Dodd K.W., Parsons R., Ng C., Garriguet D., Tarasuk V. Household Food Insecurity Is a Stronger Marker of Adequacy of Nutrient Intakes among Canadian Compared to American Youth and Adults. [(accessed on 16 July 2019)];J. Nutr. 2015 145:1596–1603. doi: 10.3945/jn.114.208579. Available online: https://academic.oup.com/jn/article/145/7/1596/4589978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kirkpatrick S.I., Dodd K.W., Reedy J., Krebs-Smith S.M. Income and Race/Ethnicity Are Associated with Adherence to Food-Based Dietary Guidance among US Adults and Children. [(accessed on 16 July 2019)];J. Acad. Nutr. Diet. 2012 112:624–635.e6. doi: 10.1016/j.jand.2011.11.012. Available online: https://www.sciencedirect.com/science/article/pii/S2212267211019435?via%3Dihub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krebs-Smith S.M., Guenther P.M., Subar A.F., Kirkpatrick S.I., Dodd K.W. Americans Do Not Meet Federal Dietary Recommendations. [(accessed on 16 July 2019)];J. Nutr. 2010 140:1832–1838. doi: 10.3945/jn.110.124826. Available online: https://academic.oup.com/jn/article/140/10/1832/4600316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krueger H., Williams D., Ready E., Trenaman L., Turner D. Improved estimation of the health and economic burden of chronic disease risk factors in Manitoba. [(accessed on 10 May 2018)];Chronic Dis. Inj. Can. 2013 33:236–246. Available online: http://www.ncbi.nlm.nih.gov/pubmed/23987220. [PubMed] [Google Scholar]
- 36.Whiteman D.C., Webb P.M., Green A.C., Neale R.E., Fritschi L., Bain C.J., Parkin D.M., Wilson L.F., Olsen C.M., Nagle C.M., et al. Cancers in Australia in 2010 attributable to modifiable factors: Introduction and overview. [(accessed on 9 July 2019)];Aust. N. Z. J. Public Health. 2015 39:403–407. doi: 10.1111/1753-6405.12468. Available online: http://doi.wiley.com/10.1111/1753-6405.12468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Azevedo ESilva G., de Moura L., Curado M.P., Gomes Fda S., Otero U., Rezende L.F., de Daumas R.P., Guimarães R.M., Meira K.C., Leite Ida C., et al. The Fraction of Cancer Attributable to Ways of Life, Infections, Occupation, and Environmental Agents in Brazil in 2020. [(accessed on 9 July 2019)];PLoS ONE. 2016 11:e0148761. doi: 10.1371/journal.pone.0148761. Available online: http://www.ncbi.nlm.nih.gov/pubmed/26863517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Canadian Institute for Health Information National Health Expenditure Trends, 1975 to 2018. [(accessed on 16 July 2019)]; Available online: https://www.cihi.ca/en/health-spending/2018/national-health-expenditure-trends.
- 39.Health Canada Economic Burden of Illness in Canada, 1998. [(accessed on 16 July 2019)];2002 Available online: http://publications.gc.ca/collections/Collection/H21-136-1998E.pdf.
- 40.Krueger H., Andres E.N., Koot J.M., Reilly B.D. The economic burden of cancers attributable to tobacco smoking, excess weight, alcohol use, and physical inactivity in Canada. [(accessed on 26 September 2018)];Curr. Oncol. 2016 23:241–249. doi: 10.3747/co.23.2952. Available online: http://www.ncbi.nlm.nih.gov/pubmed/27536174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Krueger H., Turner D., Krueger J., Ready A.E. The economic benefits of risk factor reduction in Canada: Tobacco smoking, excess weight and physical inactivity. [(accessed on 8 July 2019)];Can. J. Public Health. 2014 105:e69–e78. doi: 10.17269/cjph.105.4084. Available online: http://www.ncbi.nlm.nih.gov/pubmed/24735700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Forouzanfar M.H., Alexander L., Anderson H.R., Bachman V.F., Biryukov S., Brauer M., Burnett R., Casey D., Coates M.M., Cohen A., et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. [(accessed on 9 July 2019)];Lancet. 2015 386:2287–2323. doi: 10.1016/S0140-6736(15)00128-2. Available online: http://www.ncbi.nlm.nih.gov/pubmed/26364544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Statistics Canada Table 2 Population by Age Group and Sex, Canada. [(accessed on 10 April 2019)];2014 Available online: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1710000501.
- 44.Garriguet D. Accounting for misreporting when comparing energy intake across time in Canada. [(accessed on 12 April 2019)];Health Rep. 2018 29:3–12. Available online: http://www.ncbi.nlm.nih.gov/pubmed/29852052. [PubMed] [Google Scholar]
- 45.Fedorak R.N., Switzer C.M., Bridges R.J. Canadian Digestive Health Foundation Public Impact Series 4: Celiac disease in Canada. Incidence, prevalence, and direct and indirect economic impact. [(accessed on 17 July 2019)];Can. J. Gastroenterol. 2012 26:350–352. doi: 10.1155/2012/384787. Available online: http://www.ncbi.nlm.nih.gov/pubmed/22720277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Topper A. Non-Celiacs Drive Gluten-Free Market Growth. [(accessed on 18 July 2019)];2014 Available online: https://www.mintel.com/blog/food-market-news/gluten-free-consumption-trends.
- 47.Canadian Celiac Association Non-Celiac Gluten Sensitivity: How to Diagnose and Differentiate It from Celiac Disease. [(accessed on 17 July 2019)]; Available online: https://www.celiac.ca/gluten-related-disorders/non-celiac-gluten-sensitivity/
- 48.Rubio-Tapia A., Ludvigsson J.F., Brantner T.L., Murray J.A., Everhart J.E. The Prevalence of Celiac Disease in the United States. [(accessed on 18 July 2019)];Am. J. Gastroenterol. 2012 107:1538–1544. doi: 10.1038/ajg.2012.219. Available online: http://insights.ovid.com/crossref?an=00000434-201210000-00017. [DOI] [PubMed] [Google Scholar]
- 49.Rizvi S., Pagnutti C., Fraser E., Bauch C.T., Anand M. Global land use implications of dietary trends. PLoS ONE. 2018;13:e0200781. doi: 10.1371/journal.pone.0200781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Krueger H., Krueger J., Koot J. Variation across Canada in the economic burden attributable to excess weight, tobacco smoking and physical inactivity. [(accessed on 26 September 2018)];Can. J. Public Health. 2015 106:171–177. doi: 10.17269/cjph.106.4994. Available online: http://journal.cpha.ca/index.php/cjph/article/view/4994/3123. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.