Abstract
Background
Most academic medical institutions lack a structured program that provides residents with an in-depth research training. The objectives of this paper are to describe a comprehensive residency research program at a university hospital, and to assess the pre- post-self-assessment of research capabilities of resident for the evaluation of the program.
Methods
The residency research program (RRP) was implemented in 2011 as an essential component of the residency program at the American University of Beirut Medical Center. Categorical residents are required to carry out a research project and go through all the steps of the research process from identifying a topic to writing a manuscript. As for evaluating the program, data were collected from residents who graduated between 2014 and 2016 using a questionnaire, which included the overall evaluation of the program, self-assessment on research-related tasks pre- and post- joining the program, as well as general recommendations. The mean scores on the five-point Likert scale were transformed into percentages (0–100%). The average was calculated and the difference in the means was reported.
Results
Overall, 103 residents from the different clinical departments were included in this study. Residents’ self-assessment showed a 19.3% improvement in research-related tasks before and after completion of the RRP (P < 0.0001). Most of the residents have either published or are in the process of publishing their projects (34 and 55.3%, respectively). Time management was the most reported challenge. Generally, the program was evaluated positively.
Conclusion
The RRP is a unique, well-structured program, encompassing residents from various clinical departments, which enhances residents’ research capabilities.
Keywords: Residency research program, University hospital, Academic career, Residents, Structured program
Background
Research is a systematic investigation founded on observation, experimentation and evaluation designed to develop or contribute valid and reliable knowledge [1]. Medical research in particular, whether basic, clinical or epidemiological has enriched and supported the development of the scientific literature worldwide [2]. Early exposure to research experience in undergraduate college and medical students was considered an important opportunity to foster one’s academic medical career [3, 4].
Nonetheless, early exposure to research experience during the residency period is equally beneficial. Actually, research was found to be important in guiding treatment decision and enhanced the residents’ ability to care for patients [5, 6]. Indeed, the number of residents’ scholarly publications was found in a study to be significantly associated with residents’ clinical performance [7]. Investing substantial time and efforts in research allows the practicing resident to keep up with the constantly evolving field of medicine, to comprehend new discoveries and to translate them into patient care [8]. Moreover, getting involved in research prepares residents to become lifelong self-learners and develop their appreciation for research advancement in general [5]. This was confirmed by a longitudinal study of an integrated research residency training curriculum which was found successful in promoting the entry of residents into primary research careers [9]. Furthermore, this period is thought to be a critical juncture for residents who are on their way to start their individual academic path [10]. In addition, residents’ research attitude was found to influence their career expectation and increased their interest in pursuing fellowship training opportunities in their specialty of interest [11].
Acknowledging the aforementioned benefits, several academic institutions have established clinical research as part of their residency-training curriculum. The effectiveness of such programs has been published in a variety of settings and research in this domain has been increasingly discussed [5–9, 12]. However, to our knowledge, existing research residency programs worldwide, did not encompass all the clinical departments and where confined to only a single department within an institution [9, 13]. Moreover, we did not find articles describing a structured research program targeting residents during their training.
The two objectives of this paper are first to describe a comprehensive Residency Research Program (RRP), implemented at a university hospital, and second to perform a pre- and post- self assessment of research capabilities of the residents taking part of the program for the overall evaluation of the program.
Methods
Residency research program description
This section covers the first objective of the paper, which is the description of the RRP:
RRP
The RRP is a program that was established in 2011 in the department of Internal Medicine at the American University of Beirut (AUBMC), Lebanon, then expanded in 2012 to become an essential requirement of the residency program at all departments of the Faculty of Medicine. Categorical residents are required to carry out a research project throughout their residency program.
Eligibility and duration
The RRP is designed to accommodate residents with or without any previous research background. No pre-requisites are needed to be involved in the program. Residents are required to have a serious commitment to fulfill the program requirements. The duration of the RRP is three years, although some specific residency programs might extend beyond that duration (e.g. surgery). Moreover, the program accommodates residents who submit their work prior to the deadlines.
RRP process
Following are the different steps of the RRP process.
The questionnaires
Two questionnaires, the “resident’s questionnaire” and the “advisor’s questionnaire” need to be filled at the initiation of the process to gather information about both the residents and the advisors. The “resident’s questionnaire” includes information about the resident, their research background, as well as personal assessment of their research skills and knowledge in which the residents had to fill. Similarly, the “advisor’s questionnaire” includes the advisor’s information, research field, interests and ongoing research project filled by the advisor.
Resident / advisor matching
The matching process involves mutual agreement of the resident and advisor to work on a specific research project. This matching is done either through self-matching or through the RRP departmental committee. During self-matching, resident identifies the advisor for the specific research question in mind based on similar interests and personal communication. For residents who fail to identify a potential match, the RRP departmental committee carries out the matching based on mutual interest and agreement.
Research topic
The research topic could be resident-initiated, where the residents identify the research topic, or faculty-initiated in which the faculty member is the one who provides a project for the resident to work on, which is mainly appropriate to residents who do not have a specific research question in mind.
Letter of intent
The resident prepares a letter of intent, which includes information on the resident and the advisor, and a brief description about the project (such as title, objectives, methodology and significance). This letter is submitted and evaluated by the RRP departmental committee.
Research proposal
In this step, the resident writes the full proposal, which includes information about the title, starting date, duration of the project, type of project, abstract, objectives, background and significance, research design and methods (including study area, study subjects, study design, sample size, sampling technique, data collection methods, data management and analysis plan), and references. The proposal is submitted to the RRP departmental committee for approval. Moreover, the proposal is submitted to the Institutional Review Board (IRB) at AUB to get the ethical approval.
Conducting the research project
After getting the approval on the proposal from both the RRP and the IRB, the resident starts working either on the already existing data (if applicable) or carrying out the data collection and performing data analysis, results interpretation and comparison to literature.
Progress presentations
Residents provide an update on the status of their projects, as well as any challenges, by delivering two progress presentations in the presence of members of the departmental committee who provide feedback to the residents.
Final report
A final report in the form of a manuscript needs is prepared by the resident, and it includes the following sections: the residents’ and advisors’ information, title, abstract, introduction/background, methodology, results, discussion, conclusion/ recommendations, references, tables and graphs. The report is evaluated by the RRP departmental committee.
Final presentation
The resident delivers a final presentation during an RRP research day (see related section). The following parts are presented: title, introduction, objective(s), methods, results, discussion, conclusion, references. The final presentations are evaluated by jury members from different departments.
RRP key players
The success of the RRP depends on four key players: the resident, the advisor, the RRP departmental committees, and the RRP committee.
Resident
The resident has the major responsibility to carry out the research project in a satisfactory manner. The resident is highly encouraged to submit the prepared report for publications in peer-reviewed journals, as well as to present their research in national and international conferences.
Advisor
Any faculty member at the AUBMC could be eligible to be an advisor to one or more residents at any given time. The major responsibility of the advisor is to guide and supervise the resident in the research process. The advisor has to ensure that the resident is carrying out the RRP in a satisfactory manner, through holding regular meetings.
RRP departmental committees
The RRP departmental committee includes faculty members who have research expertise in different fields in their respective department. These committees are responsible for carrying out the matching process, evaluating the residents’ work (letter of intent, full proposal, progress presentations, and final report).
RRP committee
The RRP committee includes representatives from all the clinical departments, and are responsible for ensuring the efficient flow of the RRP. Members of the committee meet on regular basis to oversee the progress of the program, as well as to address different arising issues.
RRP website, educational sessions and portal
A website for the RRP has been developed which includes program information and guide (http://www.aub.edu.lb/fm/medicalresearch/ClinicalandTranslationalResearch/FRRP/Pages/FRRPHome.aspx). Specific forms have been developed and posted online for each of the different steps of the research process, such as the questionnaires, letter of intent, proposal, final report, and presentation templates assessment sheets. These documents were inspired from international guidelines for manuscript writing with the specific structure and word count included in these forms. As for the assessment sheets, it included ratings about the scientific value of the project, as well as the technical and presentation skills of the resident. Moreover, a series of educational sessions on different research topics were recorded and posted online for the residents, which is continuously updated. Residents were continuously encouraged to either attend these sessions or refer to them online. Finally, an online portal has been established, whereby residents can login, create their RRP profile, then fill and submit all the needed documents online.
RRP outcome: RRP research day
In recognition to the efforts carried out by the residents, advisors, RRP committee and RRP departmental committee members, an RRP research day is scheduled yearly before the residents’ graduation. During this activity, residents present their work either as poster or oral presentations in front of an audience from the medical field. A jury from different departments evaluate the residents’ work and prizes are awarded to the best presentations.
Evaluation of the program
To evaluate the program, questionnaires are filled out by the residents during the research day. The content of the questionnaire will be discussed in the following section.
Residency research program evaluation
The following section covers the second objective of this paper, which is the evaluation of the RRP.
Data collection and measures
Since the program’s establishment, three groups of graduates have successfully completed the RRP process, graduates of years 2014, 2015, and 2016, thus have joined the program in 2011, 2012 and 2013, respectively. Two sources of data were used to obtain an overall evaluation of the program both obtained by giving a self-filling questionnaire to the residents. The first source was the data collected from the residents through their “resident’s questionnaire” filled up upon joining the program (pre-), which included the following: 1- demographic information, 2- residents’ research background before enrolling in the RRP, 3- residents’ self-assessment of their research skills and knowledge before joining the RRP (results presented in Table 2). The second source of data was a similar questionnaire, upon completion of the program (post-), and included the following: 1- demographic information, 2- level of agreement regarding problems faced during the RRP process (results presented in Table 3), 3- advisors’ evaluation, and 4- overall satisfaction and recommendations. Answers to the above questions were mainly based on a 5-point Likert scale.
Table 2.
Residents’ self-assessment of research related tasks before and after completing the RRP, as well as the difference in their assessment
| Variables | Pre Mean ± SD |
Post Mean ± SD |
Diff (Post-Pre) Mean ± SD |
P-value |
|---|---|---|---|---|
| Total score 1-Literature Review | 66.4 ± 19.5 | 80.5 ± 15.5 | 14.1 ± 12.6 | < 0.0001 |
| Literature review | 65.4 ± 21.5 | 78.4 ± 17.6 | 13.3 ± 16.1 | < 0.0001 |
| Using PubMed | 65.1 ± 20.8 | 80.0 ± 16.9 | 14.9 ± 14.8 | < 0.0001 |
| Reading articles | 70.4 ± 19.9 | 83.3 ± 15.7 | 12.9 ± 14.5 | < 0.0001 |
| Summarizing articles | 65.4 ± 23.2 | 80.2 ± 17.7 | 14.7 ± 16.9 | < 0.0001 |
| Total score 2-Writing the Proposal | 48.0 ± 20.5 | 71.1 ± 15.8 | 23.1 ± 17.7 | < 0.0001 |
| Defining research objectives | 57.8 ± 23.8 | 76.8 ± 17.1 | 19.0 ± 18.6 | < 0.0001 |
| Constructing questionnaire | 49.5 ± 22.9 | 69.3 ± 17.9 | 19.8 ± 18.6 | < 0.0001 |
| Writing proposal | 45.7 ± 24.9 | 72.2 ± 17.4 | 26.5 ± 22.0 | < 0.0001 |
| Applying to IRB | 68.5 ± 21.0 | 52.6 ± 21.9 | 29.3 ± 22.0 | < 0.0001 |
| Total score 3-Data management and analyses | 52.6 ± 21.9 | 72.8 ± 16.1 | 20.2 ± 17.7 | < 0.0001 |
| Data collection | 59.4 ± 26.3 | 79.4 ± 17.9 | 20.0 ± 20.0 | < 0.0001 |
| Data entry | 54.9 ± 27.1 | 77.7 ± 18.3 | 22.7 ± 23.2 | < 0.0001 |
| Data analyses | 45.4 ± 23.5 | 66.3 ± 20.6 | 21.0 ± 21.1 | < 0.0001 |
| Data summarization | 52.3 ± 24.5 | 71.7 ± 18.6 | 19.4 ± 21.6 | < 0.0001 |
| Tables graphs | 52.1 ± 23.4 | 72.1 ± 17.8 | 20.0 ± 20.6 | < 0.0001 |
| Total score 4-Writing | 52.8 ± 21.9 | 72.2 ± 17.7 | 19.4 ± 17.1 | < 0.0001 |
| Writing introduction | 57.4 ± 25.2 | 77.0 ± 17.2 | 19.6 ± 20.2 | < 0.0001 |
| Writing methods | 52.6 ± 25.1 | 74.4 ± 18.7 | 21.8 ± 19.9 | < 0.0001 |
| Writing results | 53.4 ± 24.1 | 74.4 ± 18.2 | 21.0 ± 19.2 | < 0.0001 |
| Writing discussion | 53.3 ± 23.5 | 71.5 ± 18.2 | 18.2 ± 17.9 | < 0.0001 |
| References | 57.4 ± 26.3 | 76.2 ± 18.6 | 18.8 ± 21.4 | < 0.0001 |
| Submission publication | 39.4 ± 24.1 | 59.8 ± 25.6 | 20.4 ± 23.3 | < 0.0001 |
| Study presentation | 60.4 ± 25.6 | 78.8 ± 18.6 | 18.4 ± 21.8 | < 0.0001 |
| Total score | 54.5 ± 19.5 | 73.8 ± 15.0 | 19.3 ± 14.1 | < 0.0001 |
IRB Institutional Review Board, SD standard deviation; RRP Residency Research Program
Table 3.
Distribution of problems faced by residents during the RRP, stratified by the different phases of the research project
| Problems faced by residents during the RRP | N = 103 Mean ± SD |
|---|---|
| Total score 1-Time issues | 57.2 ± 24.5 |
| Time management | 59.6 ± 26.5 |
| Time frame for the project | 55.1 ± 25.2 |
| Total score 2-Data processing | 50.4 ± 18.8 |
| Data analyses | 53.9 ± 23.4 |
| Data collection | 51.7 ± 24.3 |
| Data summarization | 49.5 ± 20.7 |
| F Data entry | 46.9 ± 21.9 |
| Total score 3-Logistics | 50.1 ± 17.1 |
| Topic Identification | 53.2 ± 23.7 |
| Proposal Writing | 49.5 ± 20.9 |
| Report writing | 47.9 ± 18.9 |
| Total score 4-Other | 45.3 ± 16.1 |
| Getting approval from IRB | 51.1 ± 24.1 |
| Lack of knowledge | 48.4 ± 22.4 |
| Identifying a supervisor | 44.6 ± 22.4 |
| Supervisor relationship | 37.5 ± 18.4 |
| Total Score | 49.7 ± 16.4 |
RRP Residency Research Program
Statistical analyses
The IBM’s Statistical Package for the Social Sciences (SPSS) version 22.0 (IBM, Inc., Chicago, IL) was used for data management and analyses. The mean scores on the 5-point Likert scale were transformed into percentages with a score of 0 corresponding to 0% and a score of 5 corresponding to 100%. Difference between the self-assessment scores in the pre- and post- RRP were also calculated. Data were summarized as numbers and percent for categorical variables and mean and standard deviation for continuous ones. The association between the pre- and post- RRP was assessed by the Chi square test for categorical variables, and Student’s t-test for continuous ones. Statistical significance was indicated at the 0.05% level.
Results
Residents’ characteristics
Table 1 summarizes the characteristics of the residents completing the RRP requirements. Although all residents at the AUBMC were eligible in this study, 103 out of 122 residents (84.4%) from the different departments were included in this analyses, mainly: Internal Medicine, Pediatrics, Family Medicine, Emergency Medicine, Anesthesiology, Neurology, Pathology and Lab Medicine, Obstetrics and Gynecology, Ophthalmology, Dermatology, Diagnostic Radiology and Radiation Oncology. Those who are excluded from the analyses were residents with incomplete information at the time of the analyses. The largest number of residents was from the department of Internal Medicine (30.1%), followed by Pediatrics (17.5%) and Family Medicine (11.7%). Moreover, 74.5% had some theoretical background in research, thus previously attended courses on research, statistics, research database experience or evidence base medicine. As for the residents’ previous research experience, 61.2% have been involved prior to their enrollment in the RRP in some stages of the research process, out of whom 14.3% were previously engaged in more advanced stages such as statistical analysis and writing the manuscript.
Table 1.
Residents’ Characteristics classified by year of graduation, department and previous theoretical background
|
N = 103 N (%) |
|
|---|---|
| Year of graduation | |
| 2014 | 14 (13.6) |
| 2015 | 42 (40.8) |
| 2016 | 47 (45.6) |
| Department | |
| Internal Medicine | 31 (30.1) |
| Pediatrics | 18 (17.5) |
| Family Medicine | 12 (11.7) |
| Emergency Medicine | 11 (10.7) |
| Anesthesiology | 5 (4.9) |
| Neurology | 5 (4.9) |
| Pathology and Lab Medicine | 5 (4.9) |
| Obstetrics & Gynecology | 4 (3.9) |
| Ophthalmology | 4 (3.9) |
| Dermatology | 4 (3.9) |
| Diagnostic Radiology | 3 (2.9) |
| Radiation Oncology | 1 (1.0) |
| Theoretical Background | |
| Any theoretical background | 76 (74.5) |
| Research courses | 32 (31.4) |
| Statistic courses | 69 (67.6) |
| Research databases | 20 (19.8) |
| Evidence based medicine | 44 (43.6) |
| Others | 7 (6.8) |
| Involvement in research before RRP | 63 (61.2) |
| Involved in advanced stages (statistical analysis, manuscript write-up) | 9 (14.3) |
RRP Residency Research Program
Residents’ assessment
Table 2 summarizes residents’ self-assessment according to four different categories pre- and post- completing the RRP. In “Literature Review” category, using PubMed was found to be the variable that had mostly improved with a mean difference of 14.9% (SD = 14.8). In the second category “Writing the Proposal”, applying to the IRB was the variable that has shown the most significant improvement with a mean difference of 29.3% (SD = 22.0) followed by writing the proposal with a mean difference of 26.5% (SD = 22). As for the third category “Data Management and Analyses”, data entry was the variable that has significantly improved with a mean difference of 22.7% (SD = 23.2), followed by data analysis with a mean difference of 21% (SD = 21.1). Finally in the fourth category “Writing”, writing the methods has shown a significant improvement among participants with a mean difference of 21.8% (SD = 19.9). Combining all four categories together, a significant improvement was noted in the various variables with a total mean difference of 19.3% (SD = 14.1). The residents’ self-assessment post completion of the RRP was significant for each individual category and for all categories.
Residents’ publications after enrollment in the RRP
As for the publication rate after RRP completion, results are reported in Fig. 1. More specifically, 34% have published their RRP studies, 55.3% are in the process (writing or submitting the manuscript for publication), whereas, 10.7% have decided not to submit their work to journals for publication due to various reasons (e.g. the results were not conclusive, missing data …).
Fig. 1.
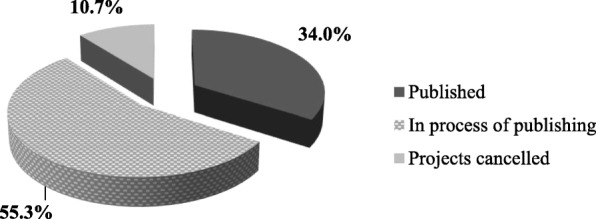
Residents’ publications’ distribution after enrollment in the RRP (n = 36)
Problems faced by the residents during the RRP
Table 3 provides data regarding problems faced by residents during the RRP at various levels, such as time issues, data processing, logistics and many others. Time management was noted to be a significant barrier for residents where 59.6% (SD = 26.5) of the residents reported time management issues. Moreover, 53.9% (SD = 23.4) had some problems in the data analysis. Similarly, 53.2% (SD = 23.7) of the residents had difficulties identifying a topic for their research project and 51.1% (SD = 24.1) had some delays in getting IRB approval for their research project.
Residents’ evaluation and feedback
The overall program evaluation score by the residents’ was found to be 73.0% (SD = 12.6) (Table 4). On a 5-point Likert scale, the highest evaluation criteria were that “residents will carry out research in the future” with a score of 78.8 (SD = 15.0). Out of the several recommendations, 89.2% of residents’ recommended “more teaching in data analyses”, 83.2% recommended “more teaching in paper writing”, and 73.5% recommended “allocated a dedicated time for RRP”. Moreover, residents’ feedback on RRP advisors yielded a total average score of 90.8% (SD = 16.0), where the mean scores ranged between 88.4% for “allocated enough time” to 91.8% for “being helpful during the process” (Table 5).
Table 4.
Residents’ evaluation and recommendation of the program
| RRP Evaluation and recommendations | N = 103 |
|---|---|
| Evaluation | Mean ± SD |
| I will carry out research in the future | 78.8 ± 15.0 |
| The FRRP is an important component of the curriculum | 77.1 ± 20.1 |
| I have the expertise to initiate a research project | 76.3 ± 16.3 |
| The FRRP was not a waste of my time | 73.2 ± 22.5 |
| I have the expertise to finalize a research project | 72.8 ± 17.7 |
| I have the expertise to present in national and international conferences | 72.8 ± 19.6 |
| The FRRP enhanced my interest in research | 71.3 ± 22.0 |
| The time allocated for the FRRP could not have been utilized for better purposes | 70.1 ± 23.1 |
| I have the expertise to publish in medical journals | 65.3 ± 21.6 |
| Total Score | 73.0 ± 12.6 |
| Recommendations | N (%) |
| More teaching in data analysis is required | 91 (89.2) |
| More teaching in paper writing is required | 84 (83.2) |
| A dedicated time needs to be given when joining the RRP | 75 (73.5) |
| More time needs to be given to do the RRP project | 62 (60.8) |
| Supervisors needs to be more aware and committed to the projects | 54 (52.9) |
| RRP kept as it is | 43 (42.6) |
| RRP made an optional part of the curriculum | 39 (38.6) |
| RRP cancelled from the curriculum | 9 (8.9) |
RRP: Residency Research Program
Table 5.
Residents’ feedback on RRP advisors
| Residents’ feedback on RRP advisors | N = 103 Mean ± SD |
|---|---|
| Was helpful during the process | 91.8 ± 16.4 |
| Reviewed documents promptly | 91.5 ± 16.5 |
| Had adequate research expertise | 91.5 ± 16.6 |
| Provided important advice | 91.3 ± 16.3 |
| Supported me | 91.3 ± 16.5 |
| Provided constructive feedback | 90.7 ± 17.5 |
| Was easy to be reached | 89.7 ± 17.9 |
| Allocated enough time | 88.4 ± 18.5 |
| Total Score | 90.8 ± 16.0 |
RRP Residency Research Program
Discussion
This paper provides a comprehensive description of a research program targeting categorical medical residents (RRP) at the AUBMC, as well as a pre- and post- self-assessment of the program. The RRP is one of the essential components of the residency curriculum at the Faculty of Medicine. This program enabled residents to develop a deeper understanding of the scientific and evidence based medicine (EBM) which is beyond what is offered in the core curriculum as shown by previous similar research [14]. Residents positively evaluated the RRP and showed a significant improvement in several research areas.
The RRP is a well-structured program, which follows an organized process starting with topic selection to manuscript finalization. The program is unique as it is the only residency research program, to our knowledge, to encompass residents from the various clinical departments, while previous research has only focused on single departments at a time [9, 13]. Moreover, our program establishes a structured timetable for residents, as it was lacking in similar programs described in the literature [15, 16]. As lacking in most other similar programs, an important aspect in the RRP is the development of educational sessions covering basic to advanced topics in research methodology [17, 18]. Resident’s research background and experience was collected at the beginning of the program, which was not addressed in other similar programs [13, 16, 19]. This led to tailoring these educational sessions for the residents which were posted on the university website to be accessed by the residents. This step was beneficial for them in conducting their projects as this was lacking in other research programs implemented in other institutions.
The RRP has subjectively assessed the residents’ knowledge and experience in research pre- and post- the completion of the program. More specifically, residents enhanced their knowledge and expertise pertaining to the different steps of the research process. The program enabled the residents to publish their articles in peer-reviewed journals, as well as to present in international conferences. This finding is in line with previous literature as it has been found that a dedicated research program during residency is indeed linked to a greater number of publications by residents [20]. Residents, throughout the process have also improved their communication skills while preparing their oral presentations as was outlined in previous similar studies [21]. In addition, residents were given the chance to get connected with advisors from various backgrounds with different specialty and subspecialty areas. Indeed having a well-structured relation between the advisor and the resident is crucial for the success of the any residency research program [16]. Indeed, the RRP was considered a great start for residents who wish to pursue a research career, along to their clinical practice, as previously reported [3, 4].
An additional aspect of the uniqueness of this program is the inclusion of residents’ self-assessment, as well as an overall evaluation of the program. Moreover, residents offered recommendations for future improvement. In fact, continuous evaluation of any newly established program, whether in medicine or any other discipline, leads to its rapid growth and its improvement [22]. Such an evaluation has not been reported in papers describing similar programs, except for a single paper only reporting the number of publications and residents’ enrollment in a postdoctoral research fellowship [9].
The RRP was equally beneficial to the advisors who got support from the residents in their ongoing research projects or any new research within the advisors’ research interests. Indeed, research as a requirement during residency was found to enhance collaborative resident and faculty publication productivity [19]. As for the institutional level, this program has increased the number of ongoing research projects and publications in the various clinical departments and has allowed cross-departmental collaboration. More specifically, several topics were tackled through collaboration between different clinical departments. Finally, the RRP has established a research culture among the members of the AUBMC community.
Like any other residency research program implemented in an institution, the RRP has faced several challenges at different levels, such as financial, administrative, and time-related issues. Financial barriers were among the challenges of our program, more specially the limited financial support allocated for residents’ research projects, which could be addressed by encouraging residents to apply for internal and external funding, as well as to secure institutional budget allocated for residents’ research. Moreover, the advisor did not explicitly assess the research skills of the residents, which should be tackled in future implementation of this program. Another challenge was the administrative issues that needed to be worked out to ensure a proper structure and flow of the program. Moreover, facing some delays at different stages of the research process, one of which was securing the IRB approval, as most of these projects were new projects was another challenge. Another main challenge was pertaining to time-related issues, mainly the commitment to the RRP deadlines from the committee members, advisors and residents. Unfortunately, as reported previously [15], residents have complained about the lack of protected time in their schedule for undergoing research and found some difficulties managing their clinical work and practice with the research deadlines required by the RRP. For the purpose of overcoming these challenges, time tables were developed taking into consideration the expected delays at early stages. Another strategy to overcome time-related issues was to send e-mails to remind residents, advisors and committee members of the RRP deadlines, to schedule meetings with representatives to discuss the residents’ progress, schedule progress presentations with residents to discuss challenges and ways to overcome them and to offer assistance in the different stages of their research projects. Another approach to deal with this challenge is to introduce workshops on time management skills offered to residents with the aim to reach a well-balanced clinical/research time allocation. Finally, although the RRP is a well-structured and positively evaluated program, replicating it in other institutions whether in Lebanon or in the surrounding countries might be faced with some difficulties depending on the institution’s mission and regulations.
Conclusion
The RRP is a mandatory research program that provides residents at AUBMC with the opportunity to conduct research in different areas under the supervision of advisors in different specialties. This program has created a unique research culture allowing residents to foster their academic medical career, thus becoming better clinicians and researchers. The RRP is a unique, well-structured program, encompassing residents from various clinical departments, as well as collecting feedback and evaluation on regular basis. Based on continuous evaluation, we anticipate more changes to be implemented with the hope to reach a program with even higher standards. We envision expanding it in the subsequent years to include clinical fellows at AUBMC and probably to expand and collaborate with other academic medical schools at the national and international levels. Future papers describing similar programs will have an added contribution to enhancing residents’ involvement in research.
Acknowledgements
Not applicable.
Abbreviations
- AUBMC
American University of Beirut Medical Center
- EBM
Evidence based medicine
- IRB
Institutional Review Board
- RRP
Residency Research Program
Authors’ contributions
All authors participated in the design and interpretation of the residency research program. SKha was responsible for designing the evaluation questionnaires and completed the data collection. HT and ZA provided statistical advice on study design and analysed the data. FT undertook the literature review and drafted the manuscript. HT, SZ, AT and SKho contributed substantially to its revision. HT, AT and SKho took responsibility for the paper as a whole. All authors read and approved the final manuscript.
Funding
No funding was received for this project.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The RRP is part of the residency education program at the AUBMC, and thus, this research paper falls under the quality improvement for the program. Accordingly, IRB approval was not required for conducting this work. Moreover, upon joining the program, the residents consent to have their data used for quality improvement and research purposes, which is included in their signed enrollment.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hani Tamim and Salah Zeineldine contributed equally to this work.
Contributor Information
Hani Tamim, Email: htamim@aub.edu.lb.
Salah Zeineldine, Email: sz01@aub.edu.lb.
Faysal Tabbara, Email: ft19@aub.edu.lb.
Samia Khoury, Email: sk88@aub.edu.lb.
Zeina Akiki, Email: zeinaakiki@hotmail.com.
Sara Khansa, Email: sk77@aub.edu.lb.
Ali Taher, Phone: 00961-1-350000, Email: ataher@aub.edu.lb.
References
- 1.Nass SJ, Levit LA, Gostin LO. Beyond the HIPAA Privacy Rule: Enhancing Privacy, Improving Health Through Research, in Beyond the HIPAA Privacy Rule. Washington (DC): Enhancing Privacy, Improving Health Through Research; 2009. [PubMed] [Google Scholar]
- 2.Rohrig B, et al. Types of study in medical research: part 3 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2009;106(15):262–268. doi: 10.3238/arztebl.2009.0262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dagher MM, et al. Medical research volunteer program (MRVP): innovative program promoting undergraduate research in the medical field. BMC Med Educ. 2016;16:160. doi: 10.1186/s12909-016-0670-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Munabi IG, Katabira ET, Konde-Lule J. Early undergraduate research experience at Makerere University Faculty of medicine: a tool for promoting medical research. Afr Health Sci. 2006;6(3):182–186. doi: 10.5555/afhs.2006.6.3.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith M. Research in residency: do research curricula impact post-residency practice? Fam Med. 2005;37(5):322–327. [PubMed] [Google Scholar]
- 6.Fitz-Gerald M. J. Psychiatry Residents' Participation in Research: A Survey of Attitudes and Experience. Academic Psychiatry. 2001;25(1):42–47. doi: 10.1176/appi.ap.25.1.42. [DOI] [Google Scholar]
- 7.Seaburg LA, et al. Associations between resident physicians' publications and clinical performance during residency training. BMC Med Educ. 2016;16:22. doi: 10.1186/s12909-016-0543-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Atesok KI, et al. Perspective: integrating research into surgical residency education: lessons learned from orthopaedic surgery. Acad Med. 2012;87(5):592–597. doi: 10.1097/ACM.0b013e31824d2b57. [DOI] [PubMed] [Google Scholar]
- 9.Tsai AC, et al. Eleven-year outcomes from an integrated residency program to train research psychiatrists. Acad Med. 2013;88(7):983–988. doi: 10.1097/ACM.0b013e318294f95d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abrams MT, Patchan K, Boat TF. Research Training in Psychiatry Residency: Strategies for Reform, in Research Training in Psychiatry Residency. Washington (DC): Strategies for Reform; 2003. [PubMed] [Google Scholar]
- 11.Cull WL, et al. Research exposure during pediatric residency: influence on career expectations. J Pediatr. 2003;143(5):564–569. doi: 10.1067/S0022-3476(03)00324-X. [DOI] [PubMed] [Google Scholar]
- 12.Lowe B, et al. Effectiveness of a 1-year resident training program in clinical research: a controlled before-and-after study. J Gen Intern Med. 2008;23(2):122–128. doi: 10.1007/s11606-007-0397-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brubaker L, Kenton K. Clinical research education study teams: a research curriculum for obstetric and gynecology residents. Obstet Gynecol. 2011;117(6):1403–1407. doi: 10.1097/AOG.0b013e3182179705. [DOI] [PubMed] [Google Scholar]
- 14.Potti A, et al. Residents as researchers: expectations, requirements, and productivity. Am J Med. 2003;115(6):510–514. doi: 10.1016/j.amjmed.2003.08.017. [DOI] [PubMed] [Google Scholar]
- 15.Alhaider SA, Alshehri HA, Almedhesh SA. Research training, productivity and challenges among trainees of pediatric residency programs across Saudi Arabia. Int J Pediatr Adolesc Med. 2015;2:70–74. doi: 10.1016/j.ijpam.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eder M, Pierce JR., Jr Innovations in faculty development: study of a research assistance unit designed to assist clinician-educators with research. South Med J. 2011;104(9):647–650. doi: 10.1097/SMJ.0b013e3182294e82. [DOI] [PubMed] [Google Scholar]
- 17.Crawford P, Seehusen D. Scholarly activity in family medicine residency programs: a national survey. Fam Med. 2011;43(5):311–317. [PubMed] [Google Scholar]
- 18.Hobson WL, Bruse J, Bale JF., Jr Creating flexibility in pediatric resident education. Pediatrics. 2011;127(6):1088–1093. doi: 10.1542/peds.2010-2350. [DOI] [PubMed] [Google Scholar]
- 19.Kurahara DK, et al. A pediatric residency research requirement to improve collaborative resident and faculty publication productivity. Hawaii J Med Public Health. 2012;71(8):224–8. [PMC free article] [PubMed] [Google Scholar]
- 20.Torres D, Gugala Z, Lindsey RW. A dedicated research program increases the quantity and quality of orthopaedic resident publications. Clin Orthop Relat Res. 2015;473(4):1515–1521. doi: 10.1007/s11999-014-4080-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanna B, et al. The research rotation: competency-based structured and novel approach to research training of internal medicine residents. BMC Med Educ. 2006;6:52. doi: 10.1186/1472-6920-6-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Alkin MC, Christie CA. An evaluation theory tree, ed. M.C. Alkin. 2013. Thousand Oaks: CA: SAGE.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


