Abstract
The time it takes for clinical innovation and evidence-based practices to reach patients remains a major challenge for the health care sector. In 2015, the Veterans Health Administration (VHA) launched the Diffusion of Excellence Initiative aimed at aligning organizational resources with early-stage to midstage promising practices and innovations to replicate, scale, and eventually spread those with greatest potential for impact and positive outcomes. Using a 5-step systematic approach refined over time, frontline VHA staff have submitted more than 1676 practices since the initiative’s inception, 47 of which have been selected as high-impact, Gold Status practices. These Gold Status practices have been replicated more than 412 times in Veterans Affairs hospitals across the country, improving care for more than 100,000 veterans and approximately $22.6 million in cost avoidance for the VHA. More importantly, practices such as Project HAPPEN (Hospital-Acquired Pneumonia Prevention by Engaging Nurses to complete oral care) and rapid availability of intranasal naloxone have saved veterans’ lives. Several practices are now being implemented across the country, and the Diffusion of Excellence Initiative is playing a pivotal role as the VHA works to modernize its health care system. This initiative serves as a promising model for other health care systems seeking to accelerate the spread and adoption of clinical innovation and evidence-based practices.
Keywords: best practices, evidence-based practices, innovation health coaching, integrative, multimodal, psychiatry, wellness coaching
INTRODUCTION
The US health care environment is rapidly changing. Health care systems of all sizes struggle to balance consumerism with value-based care. Organizations that promote and facilitate a culture of learning alongside continuous improvement have emerged as leaders across this evolving landscape, but fostering continuous improvement is only part of the answer. Evidence-based best practices can take years to reach patients.1–4 Innovative solutions for everyday challenges are needed, and innovative approaches are also required to replicate and spread these solutions once they are identified.
Multiple factors contribute to a slow, widespread adoption of evidence-based clinical practices, including the complexity of the innovation, opportunity cost of change, limited resources, and lack of influential leadership or champions.3–6 In 2015, the Veterans Health Administration (VHA) launched the Diffusion of Excellence Initiative (hereafter referred to as Diffusion) to tackle these challenges and accelerate the spread and adoption of clinical innovation and promising practices across the VHA.
STEPS OF THE DIFFUSION PROCESS
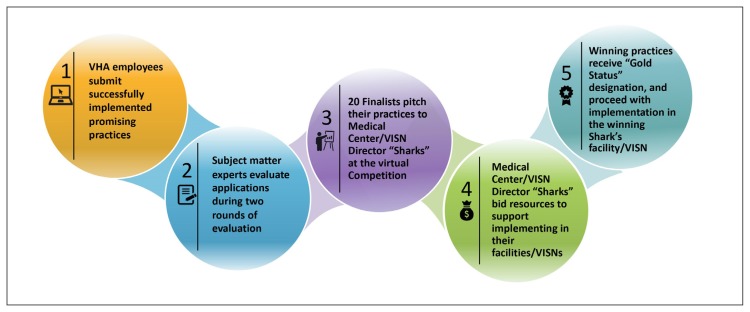
Diffusion uses a 5-step, systematic process to identify, replicate, and eventually scale and spread practices with the greatest potential for positive impact (Figure 1).
Figure 1.
Diffusion of Excellence Initiative’s Five-Step Process for Diffusing Promising Practices
Step 1: Identify Promising Practices
As summarized in Figure 2, the VHA hosts an annual, systemwide competition to identify promising administrative and clinical practices that have been previously implemented in 1 or more Department of Veterans Affairs (VA) locations. The competition invites all employees to submit innovations or practices that have demonstrated improvement in health care delivery or operational processes across priorities defined by VHA senior leadership.
Figure 2.
Steps in the VHA Diffusion of Excellence “Shark Tank”-style competition
VHA = Veterans Health Administration; VISN = Veterans Integrated Service Network.
As part of the application process, applicants report on key aspects of their practice, including evidence demonstrating their practice’s effectiveness against prior baseline data. Applications are reviewed by Diffusion staff to ensure they align with the competition’s eligibility requirements. Subject matter experts (ie, frontline clinical and administrative staff with relevant experience) from across the VHA are then engaged in evaluating applications. Review criteria include factors such as the demonstrated value of the practice, replication feasibility, and alignment to VHA priorities (Table 1).
Table 1.
“Shark Tank” evaluation criteria
| Criteria | Definition | Examples |
|---|---|---|
| VHA “Shark Tank” priority impact | Demonstrated impact in the aligned VHA “Shark Tank” priority | Access: The practice reduced days to appointment or increased specialty care appointments within 30 d from preferred date |
| Care coordination: The practice reduced time spent coordinating referrals or improved health outcomes owing to coordination among multidisciplinary teams | ||
| Employee engagement: The practice improved retention or increased job competency | ||
| Medical-surgical nursing: The practice improved leadership initiatives or clinical operations in nurse practice environments | ||
| Provider recruitment and retention in rural facilities: The practice improved practitioner recruitment or retention in rural facilities | ||
| Quality and safety: The practice reduced hospital readmissions or reduced infection rates | ||
| Suicide prevention: The practice improved the time required to connect veterans who contacted the Veteran Crisis Line with local mental health resources or reduced the number of suicides through increasing the understanding and awareness of suicide prevention strategies among veterans and their caregivers | ||
| Veteran experience: The practice improved understanding of a veterans’ diagnosis or treatment plan or increased feelings of trust or engagement in care | ||
| Data-based improvement | Measured improvements of impact to operations, veterans, and/or staff | Sample practice-specific primary success metric: The practice reduced veteran’s wait time for limb prosthetics by 39%, from 33 d to 20 d |
| Participant satisfaction | Improved satisfaction or experience for the practice user and/or target population | The practice improved patient satisfaction or experience metrics |
| The practice improved employee job satisfaction or experience metrics | ||
| The practice improved experience for a key population (eg, rural veterans, women veterans) | ||
| Implementation feasibility | Can be implemented in another facility through the Diffusion of Excellence model | The practice can be implemented in another VHA facility within 6 mo to 12 mo |
| The practice is process-focused (eg, has developed training manuals or timeline others can use to achieve similar results) | ||
| The practice has clearly specified resource requirements (eg, infrastructure, technology, processes) | ||
| The practice integrates into existing VHA facility systems (eg, infrastructure, technology, processes) | ||
| Alignment to VHA policies and processes | The practice does not conflict with existing VHA processes or policies | The practice aligns with VHA policies (or) prescribed mandatory procedures and operational requirements (eg, directives, handbooks, memorandums) |
| The practice aligns appropriately with system relationships (eg, contracted partners, unions) | ||
| Alignment to VHA priorities | The practice addresses key areas of improvement identified by VHA | The practice aligns with a specialty topic (eg, community care, consult management, open access, Strategic Analytics for Improvement and Learning [SAIL] improvement) |
| The practice aligns with strategic initiatives of VHA program offices (or) senior leadership |
VHA = Veterans Health Administration.
The review results in the selection of approximately 100 semifinalists whose applications undergo evaluation by VHA program office leadership and, in the most recent competition, researchers from the VA Quality Enhancement Research Initiative (QUERI). The QUERI researchers rated the semifinalists on a scale of 1 to 5 using a standardized assessment tool based on clinical soundness, potential for impact, and feasibility of implementation in the VHA. On the basis of the rankings and evaluation responses from program office leadership, VHA leaders select approximately 20 finalist practices to advance in the competition.
Step 2: Find the Champions: Selecting Gold Status Practices
Finalists pitch their practices during a live, virtual “Shark Tank”-style competition. VA Medical Center (VAMC) and Veterans Integrated Service Network “sharks” bid resources and compete for a chance to have a select practice replicated at their site through 6 months of facilitated implementation. To prepare their bids, “sharks” reference 90-second pitch videos, a summary grid comparing key practice attributes, practice applications, and 90-second, live-competition presentations. Bids might include staff, funding for equipment, capital investments, or facility space. Additionally, “sharks” must demonstrate their facilities’ need for the practice through quality or operational data. For instance, a facility whose heart failure readmission rate is 1 standard deviation higher (ie, worse) than the national average would describe this when bidding 2 full-time equivalents to assist with implementing a practice aimed at reducing the readmission rate for patients with heart failure.
After the “Shark Tank”-style competition, a governance board composed of national VHA leaders, including the VA Under Secretary for Health, Deputy Under Secretaries for Health, and senior representatives of operational, quality, and research offices, select practices and “sharks” as winners of the competition. Practices selected for further implementation through the “Shark Tank” are termed Gold Status practices. Each Gold Status practice is paired with 1 to 3 sites, referred to as implementing facilities, which are the sites with winning bids. The selection of implementing facilities is based on the strength of the “shark’s” bid and the demonstrated need for the practice, aiming to optimize the alignment of organizational resources with the hope of achieving maximum return on investment.
Step 3: Adapt and Replicate Gold Status Practices
Diffusion provides extensive facilitated support for the implementation of Gold Status practices whereas the implementing facilities ensure executive-level buy-in and resource support. Creators of the Gold Status practices, referred to as Gold Status fellows, serve as the de facto quarterback for the spread of their practice. They assist the implementing facilities by describing the history of the practice, lessons learned, and components of the practice that might be different at new facilities (eg, the type of staff members involved). Most importantly, Gold Status fellows help define core components of their practice. Implementing sites select an implementing facility fellow to oversee the replication at their site. Either VAMC or Veterans Integrated Service Network’s Directors are given guidance on the selection of implementing facility fellows, including their professional expertise in the relevant practice topic, passion for the practice, and tenure at the facility.
The Gold Status and implementing facility fellows come together during a 3-day face-to-face workshop aimed at introducing employees to the constructs of implementation science, quality improvement, practical guidance on leadership principles, and marketing and communications. The workshop is referred to as the Diffusion Base Camp.
Additionally, each practice is paired with program management support leaders and an implementation scientist to complete the implementation team. The Program Management Leader receives support from an external consulting team. The support team arranges weekly implementation meetings (including additional members from implementing facilities), helps track project milestones, identifies individuals in the VA Central Office who can help address barriers to implementation, and helps develop materials to encourage implementations (eg, handbooks with practice procedures and promotional materials).
The implementation scientists represent 1 of 8 implementation hubs sponsored by the VA QUERI, which is a nationwide office for connecting implementation researchers with VA operations. In addition to an Evidence Synthesis Program, QUERI consists of 15 large programs that develop and test strategies for implementation, 15 highly partnered evaluation initiatives that use implementation science to address high-priority programmatic needs of the VHA, and 2 resource centers that offer expertise in evaluation methods and use of VA data resources. The QUERI Implementation hubs offer the Diffusion teams expertise on evidence-based strategies for implementing new programs and for direct measurement of the impact of Gold Status practice replication.
Implementation teams spend most of the 2 and a half days at Base Camp discussing and learning practice components, outlining goals for implementing the practice in new facilities, and creating initial implementation plans. The teams carefully consider how to adapt a practice at a new site without losing the practice’s core components. Implementation plans consist of a timeline and milestones for implementation, stakeholders to involve in the implementation, specific practice components that must be in place, strategies for implementation, measures of success, and mitigation strategies for potential risks. Teams conclude the Diffusion Base Camp by presenting their practice implementation plan to a panel of subject matter experts and former Gold Status fellows. After the presentation, practices proceed with a 6-month facilitated implementation. During implementation, teams are guided by these implementation plans, with a strong emphasis placed on ensuring local adaptation and customization while maintaining the original practice’s fidelity.
Step 4: Measure Real-World Impact
The 6-month facilitated replication period provides a valuable opportunity for real-time evaluation and assessment of practice replication while providing support to the implementation teams to optimize success. During the 6 months, project management support leaders document barriers and assist in developing risk mitigation strategies during weekly implementation team huddles and project status calls. This information is used to develop a sense of a practice’s ease of replication. Cost of implementation is also assessed throughout the replication phase, for instance, assessing whether the proposed “bid” from a winning facility (ie, 2 full-time equivalents) is the optimal allocation of resources to replicate a select practice. Implementation teams often find that improvements in workflows or leveraging technology can aid in the replication of a practice while reducing required resources.
Implementation teams may also identify lacking health system protocols, clear policies, directives, or standard operating procedures for a specific practice. This information often informs senior leadership about challenges and opportunities to scale larger efforts across the enterprise. In turn, new policies or directives can clear the way for further replication of a practice. The QUERI representatives offer expertise to implementation teams in evaluation measurement and use of key data sources to track potential success. This, perhaps, is one of the most essential aspects to conducting a well-facilitated replication phase because it ensures sound measurement of a practice’s impact and the ability to determine future impact. For example, Project VIONE (Vital, Important, Optional, Not indicated, and Every medication has a specific indication for use), a medication management optimization practice, is leveraging structured query language and other advanced analytics to communicate with the VA’s corporate data warehouse to pull structured data files to develop cost avoidance and impact metrics (eg, costs of medications, number of medications used). This method ensures a unified and consistent approach from site to site and allows for sound estimates of the real-world impact should this practice be implemented at each VA site.
Step 5: Scale and Spread High-Impact, Gold Status Practices
After practices are adapted and replicated at additional sites, practices fall into 4 potential categories for implementation: 1) being packaged for potential organic implementation by other VA facilities; 2) partnering with VA program offices that take the operational lead on implementation in partnership with Diffusion; 3) nationwide implementation and standardization with support of Diffusion; or 4) a decision to discontinue implementation. Practices are selected for inclusion in these groups on the basis of factors such as availability of outcome metrics, the degree of enterprise-wide need, complexity of implementation, and projected impact.
Given limitations to provide staff and programmatic support to diffuse each Gold Status practice, Diffusion works to make information about these practices available to VA facilities that may wish to adopt the practices to address similar challenges without specific assistance from centralized resources (termed “organic implementation”). Projects are packaged for potential grassroots implementation by other VA facilities and include an implementation guide, clinician- and patient-facing information and marketing materials (eg, brochures), and contact information for new sites to access practice support networks. Examples of projects targeted for organic diffusion include Chaplain Groups for Veterans with Moral Injury, a practice that helps veterans embrace the concept of forgiveness of self and others, and Unit Tracking Board, a practice that uses a physical poster board in inpatient units to present clinical outcome data to staff and veterans. To date, projects have been promoted by traditional means, such as email newsletters, national call forums, and word of mouth. Diffusion is currently developing a Diffusion Marketplace that will provide a digital forum similar to Amazon to enable search and discovery of innovative clinical practices. The Marketplace is scheduled to launch internally to all VA employees in summer 2019, and subsequently implement new capabilities and enhancements of user experiences after the launch.
A subset of projects cooperates with a specific VA program office in the VA Central Office. The VA program offices provide subject matter expertise, develop policy, lead innovative efforts, spread best practices, and provide operational oversight of specific clinical and administrative aspects of the VHA. The program offices might decide to partner with Diffusion to spread key aspects of Gold Status practices that align with their respective goals. For example, the VA Mental Health and Chaplaincy Program (part of the VA Office of Mental Health and Suicide Prevention) is partnering with Diffusion to help spread key aspects of 2 former Gold Status practices: Treatment groups focused on addressing the needs of veterans facing challenges relating to feelings of guilt or life purpose (termed moral injury) and partnering with community faith-based organizations to spread awareness of VA suicide prevention efforts. As part of the evolution of this partnership, these program offices are partnering with Diffusion and VA health services researchers to hold a summit that initiates a Dynamic Diffusion Network that will allow for rapid evolution of the Gold Status practice components while measuring and reporting on the impact of the evaluation.
A small subset of practices is selected for nationwide implementation. After each cycle of facilitated implementation (generally annually), the full Gold Status practice portfolio is reviewed and scored on the basis of veteran and health system impact, level of national stakeholder endorsement, ease of implementation, cost-effectiveness, and alignment with departmental priorities. Final endorsement of a practice for national diffusion is determined by VHA leadership. The Diffusion team works to develop national implementation plans that detail the appropriate natural market within the VA for the practice and the steps needed to more widely roll out the practice to those sites. Similar to the initial facilitated replication, local practice champions are identified at each facility to be accountable for the successful implementation of the practice and to work with their teams to adapt the practice as needed to fit the unique needs of the veterans and/or facility staff.
The decision is sometimes made to discontinue implementation efforts for a select practice for a myriad of reasons. One Gold Status practice used a computer macro to optimize ordering and processing of home oxygen. However, during the replication phase it was discovered that updates to the Veterans Information Systems and Technology Architecture resulted in the need to update the macro code at each site. Considering electronic health record modernization efforts, the level of effort required to maintain this practice was not believed to be practical.
CURRENT STATUS AND ONGOING EVALUATION
Since its launch in 2015, the Diffusion has received 1676 submissions of employee-designed promising practices across 4 rounds of competition. Forty-seven practices have been selected as high-impact, Gold Status practices. Table 2 provides a summary of 6 sample Gold Status practices identified through or supported by Diffusion.
Table 2.
Gold Status practice examples
| Practice name | Brief description |
|---|---|
| Hospital-Acquired Pneumonia Prevention by Engaging Nurses to complete oral care (Project HAPPEN) | Gold Status facility: Salem VAMC (Salem, VA) |
| Implementing facility: Michael E DeBakey VAMC (Houston, TX) | |
| Practice summary: To prevent nonventilator-associated, hospital-acquired pneumonia (NV-HAP), clinicians collaborate with dental services to improve oral care for hospitalized veterans, addressing the association between the oral microbiome and development of pneumonia. Improving teeth brushing among veterans hospitalized at the 8 facilities where the practice has been replicated has resulted in a decreased incidence rate of NV-HAP from 105 cases to 8.3 cases per 1000 patient-days, 13 lives saved, and a cost avoidance of more than $2.8 million (assuming each avoided case of NV-HAP saves the VA approximately $40,000).7,8 | |
| Chaplain Groups for Veterans with Moral Injury | Gold Status facility: South Texas VHCS (San Antonio, TX) |
| Implementing facility: W G (Bill) Hefner VAMC (Salisbury, NC) | |
| Practice summary: Chaplains use 2 types of group visits for veterans diagnosed with posttraumatic stress disorder and those struggling with service-connected moral injury. The first group is spiritually based and accessible without an appointment. The second group is a closed group with a higher level of commitment for veterans to engage in spiritual and psychological interventions to combat lingering guilt and shame. | |
| Unit Tracking Board | Gold Status facility: Bay Pines VA Healthcare System (Bay Pine, FL) |
| Implementing facilities: White River Junction VA Medical Center (White River Junction, VT) | |
| Practice summary: This practice displays a physical poster board on inpatient care units to present clinical outcome data to staff and veterans. It is an easy-to-read, low-cost, customizable tool that drives transparency and performance improvement. | |
| Partnering with Veteran Service Agencies and Faith-Based Organizations to prevent veteran and service member suicides | Gold Status VISN/facility: VISN 2, Albany VAMC: Samuel S Stratton (Albany, NY) |
| Implementing facilities and VISN: Fargo VA HCS (Fargo, ND), VA Salt Lake City HCS (Salt Lake City, UT), and VISN 10/VA Ann Arbor HCS (Ann Arbor, MI) | |
| Practice summary: This program trains clergy and their congregations to identify and refer at-risk veterans and service members to VA care. Trainees can refer by way of the Veterans Crisis Line and related resources, including local community-based outpatient clinics and other VA services. In partnership with the local Veterans Service Agency, this practice invites local clergy to a training that addresses the cross-section of spirituality and mental health. The Suicide Prevention Coordinator and lead chaplain present information on how to identify, interact with, and refer veterans and service members who may be at risk for suicide. | |
| VIONE—An innovative deprescribing approach to medication management | Gold Status VISN/facility: VISN 16, Central Arkansas Veterans HCS Eugene J Towbin Healthcare Center (Little Rock, AR) |
| Implementing facility: Iowa City VA HCS (Iowa City, IA) | |
| Practice summary: The use of multiple medications may be appropriate and necessary in some cases to optimize medical conditions or quality of life. However, polypharmacy can potentially expose patients to the risk of serious consequences because of age-related changes in pharmacokinetics and pharmacodynamics. VIONE (Vital, Important, Optional, Not indicated, and Every medication has a specific indication for use) is a model for clinical pharmacists to review each patient’s medication profile to identify appropriate medications to deprescribe. VIONE’s focus is on reducing drug cost waste while avoiding any adverse events. Polypharmacy elimination also reduces health risks and mental impairment for veterans. | |
| Veterans Information Systems and Technology Architecture (VistA) automation for prosthetics | Gold Status VISN/facility: VISN 23, Iowa City VA HCS (Iowa City, IA) |
| Implementing facility: Kansas City VAMC (Kansas City, MO) and VA Maine HCS (Augusta, ME) | |
| Practice summary: Prosthetic and Sensory Aids Service’s workload outpaces VHA growth every year by 5% or more. An analysis of 8 sites’ workload and staffing during the past 5 years identified a 40% increase in administrative workload, but only a 9% increase in staff. Approximately 37% of the workload consists of repetitive tasks. The average home oxygen bill is 200 pages long and contains 1500 line items. Iowa City VA HCS automated the home oxygen billing process by integrating Microsoft Excel (Redmond, WA) and VistA. Staff no longer need to print the bill and complete lengthy reviews to uncover incorrect entries when using this macro workbook. This eliminates a significant part of repetitive administrative tasks and allows employees to improve access elsewhere in prosthetics. |
HCS = Health Care System; VA = Veterans Administration; VAMC = Veterans Administration Medical Center; VHA = Veterans Health Administration; VHCS = Veterans Health Care System; VISN = Veterans Integrated Service Network.
Gold Status practices have been replicated 412 times in VHA facilities across the country, affecting more than 100,000 veterans and producing more than $22.6 million in cost avoidance for VHA. These figures were calculated on the basis of locally collected data on metrics relating to the number of veterans and/or employees affected and projected cost avoidance. Because the nature of practices varied, not all practices reported on each metric.
Several practices are spreading nationally on the basis of projected impact across the health system. For example, Project HAPPEN, a practice encouraging the use of oral care to reduce pneumonia, facilitated a decreased incidence rate of nonventilator, hospital-acquired pneumonia (NV-HP) from 105 cases to 8.3 cases per 1000 patient-days, as of October 2018, resulting in an estimated 13 lives saved and $2.8 million in cost avoidance (assuming each avoided case of NV-HAP saves VA approximately $40,000).7,8 In addition, Project HAPPEN continues to grow and impact more veterans.
In the spirit of continuous quality improvement, Diffusion has partnered with a multidisciplinary team of QUERI investigators to carry out a mixed-methods evaluation of Diffusion, anchored by implementation science theory and frameworks. Resulting from the VA’s rigorous peer-reviewed grant process, the evaluation is titled, Spreading Healthcare Access, Activities, Research, and Knowledge (SHAARK) QUERI Partnered Evaluation Initiative (PEI).
The SHAARK PEI seeks to better understand 1) the process used by VA facilities and individual staff members to make decisions about participation in Diffusion; 2) criteria used by facilities when deciding whether to adopt promising practices and interventions (eg, bid on a potential Gold Status practice); 3) barriers and facilitators to implementing practices in new settings; and 4) factors that influence the adoption of practices across the VHA. Guided by implementation science frameworks and theories including the Consolidated Framework for Implementation Research,9 the Theory of Organizational Readiness for Change,10 and the Theory of Diffusion of Innovation,11 this ongoing evaluation uses a variety of methods to assess the Diffusion process, including interviews, virtual focus groups, structured event observations of Diffusion Summits, surveys of “sharks,” and secondary data analysis (eg, practice spread, VA organizational characteristics).
To date, the SHAARK team has conducted 110 semistructured interviews with Gold Status fellows, implementing fellows, additional implementation team members working with the implementing fellows, and individuals who facilitate implementation. These interviews have provided insight into the reasons for developing Gold Status practices, the process of taking a practice though the Diffusion “Shark Tank” competition and facilitated implementation, and how and why facilities decided to bid on the practice and subsequently implement it. The evaluation also provides an in-depth understanding of practice features that might affect initial implementation and spread. For example, Diffusion was designed to identify potential best practices developed by frontline leaders and staff who are intrinsically motivated by a desire to improve care and/or stakeholder experience to implement promising practices in their facility. However, intrinsic motivation for developing new best practices might not transfer from the Gold Status fellows to those implementing the innovation/practice in new settings. It is important for key staff members to recognize the need to implement a practice. Furthermore, the practice must be compatible with existing workflows and have enough resources (eg, dedicated time and space).
In facilities attempting to replicate Gold Status practices where leaders do not engage staff early in their bidding process, resistance to implementation might be introduced. Implementation might be completed through the persistence and hard work of implementing facility fellows, with extrinsic motivation supplied by highly publicized national Diffusion events, and with the aid of strong, external facilitation; however, sustainability might be undermined in these instances, underscoring the importance of early engagement of all key stakeholders.
Finally, early observations indicate that practices with the widest spread have had longer exposure to Diffusion, a concretely defined tool, a clear national VA leadership expectation for implementation, and/or high-priority VA goals. Upcoming in-depth evaluations of Gold Status practices selected for national rollout will offer a deeper look at implementation challenges as well as outcomes (eg, clinical, cost).
DISCUSSION
In the largest, fully integrated delivery system in the US, VA frontline employees at more than 1000 sites of care regularly identify opportunities for improvement and develop solutions to address challenges. Diffusion raises awareness of successful innovations across VA facilities and allows for enhanced organizational learning concerning how to improve clinical and administrative processes. It serves as a promising model for other health care systems seeking to accelerate the spread and adoption of clinical innovation and evidenced-based practices. Although not every process or step outlined in the methods will be applicable or relevant, there are foundational concepts that have been vital in our success. These concepts are discussed here.
Empower and Invest in the Front Line
Diffusion takes the approach that frontline employees are the most familiar with the VHA’s challenges and thus best positioned to solve them. Diffusion empowers and invests in frontline staff to drive the spread and adoption from the bottom up through customized training, financial support, and a collaborative network of peers. This approach is in stark contrast to top-down strategies, which often force adoption yet rarely succeed in achieving sustained utilization.6,12 Focusing on scaling innovation and promising practices from the bottom up also allows necessary adaptation and customization of practices and innovations. This, in turn, improves compatibility of innovations and practices from service line to service line or hospital to hospital, increasing rates of adoption.13,14
Stay Agile
Hospitals and health systems are complex organizations composed of diverse groups and teams of professionals from various disciplines. Continuously evolving to meet the needs of the organization, leadership, and frontline staff has been vital to ongoing support and participation in Diffusion. To continuously adapt and refine the Diffusion model, we have relied on rapid assessments of qualitative research to inform programmatic changes and improvements. Additionally, the Diffusion model remains “objective” to the types of innovations or practices that move through the process. This flexibility enables the initiative to support continuous innovation and progress at the VHA while maintaining a focus on helping the agency serve veterans.
Mission-Driven Innovation
New leadership and evolving priorities require hospitals and networks to quickly shift focus from 1 issue to the next. This constant cycle of change can lead to fatigue, resistance to new ideas, and a survival mentality that promotes adherence to the status quo. Additionally, frontline staff’s commitment to innovation efforts are often collateral, with little short-term gain or realization of their efforts. Diffusion focuses on the reasoning behind innovation in the VHA, creating a narrative that frontline innovation and best practices are changing and saving the lives of veterans across the country. In turn, the program challenges everyone to question why they are innovators and who they innovate for—the veteran. Diffusion’s mission is to improve the lives of veterans by positioning and empowering the frontline to advance the agency’s larger mission of serving and caring for our nation’s veterans. Participants in Diffusion have taken hold of this mission and created their own narratives, telling their personal stories of why they innovate in the VHA and the impact it is having on them and the veterans they serve.
Be Strategic in Diffusion
The matchmaking that occurs between Gold Status practices and implementing facilities has several important applications. The organization can provide outside, intensive facilitated support for the replication of promising practices at sites where there is a clear need for improvement. Concurrently, the commitment of resources upfront by leadership at implementing medical centers or networks provides leadership support, buy-in, and an eventual expectation for a return on investment. The facilitated implementation cycle allows for detailed evaluation of practices as they are replicated in settings other than their original environment to determine the best next step for these practices. Organizations must commit to the idea that not all best practices and innovations are created equal and thus not all should be scaled. Additionally, understanding challenges and barriers during guided replication helps the organization define a natural market for practice scale, following Rogers’ diffusion curve.11
Foster a Culture of Innovation
Diffusion provides a sustainable, established platform and process for engaging groups at all levels. Increasing opportunities for VHA employees to drive continuous improvement at the facility level is resulting in increased employee empowerment and engagement to solve challenges facing the VHA, demonstrated by the outpouring of participation in the Diffusion programs. This buy-in from employees at all levels is a key element to making any innovation successful, and Diffusion provides a pathway to foster multilevel stakeholder engagement across individual facilities and the VHA system.11,13 Generating solutions internally from frontline employees has the 2-fold benefit of engaging key stakeholder groups across the VA enterprise, including executive leadership and onsite employees, and ensuring that the VA remains competitive and current in its practices and care offered to veterans. Finally, the organization generates excitement through the “Shark Tank” competition, raising awareness on the importance of innovation, and celebrates small wins that have the potential for major impact. Acknowledging the attempt by employees to solve a challenge is as important as celebrating those whose practices are selected for national diffusion.
Limitations, Challenges, and Opportunities for Diffusion
During the course of Diffusion, the program has evolved to address observed challenges including balancing needed evidence with the need to quickly move innovation into the field. The extensive evaluation of Diffusion is designed in large part to help us learn more about this balance. We have also added new tools to help the VA facility and region directors work with their teams to make decisions about the adoption of practices. Innovation and implementation often require multiple people with complementary skill sets; there is a need to clarify roles and skills within this process. Finally, there is a need to build implementation and evaluation skills. Diffusion and the QUERI, which focuses on implementation science and evaluation, have partnered to infuse the concepts of implementation science into the selection of promising practices, evaluation of the VA’s Innovation Ecosystem, and moving practices into the health care system.
CONCLUSION
To help foster a culture of learning and innovation, the VHA is using the Diffusion framework to identify promising grassroots solutions and then scale and spread them systemwide. By engaging frontline VHA personnel, Diffusion is empowering employees and harnessing their ingenuity to generate ideas that can be easily implemented, replicated, and evaluated with actionable outcomes at facilities across the nation. Diffusion is thus providing invaluable benefits to veterans and ultimately transforming the health care system.
Acknowledgments
Funding for the evaluation of the Diffusion of Excellence Initiative comes from the Department of Veterans Affairs Quality Enhancement Research Initiative (PEC 17-002).
The views expressed in this paper are those of the authors and do not reflect the position or policy of the Department of Veterans Affairs or the US Government.
Kathleen Louden, ELS, of Louden Health Communications performed a primary copy edit.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
References
- 1.Kilbourne A, Atkins D. Evidence-based policy making: Balancing rigor with real-world health care for veterans and military personnel. N C Med J. 2015 Nov-Dec;76(5):339–42. doi: 10.18043/ncm.76.5.339. [DOI] [PubMed] [Google Scholar]
- 2.Atkins D, Kilbourne AM, Shulkin D. Moving from discovery to system-wide change: The role of research in a learning health care system: Experience from three decades of health systems research in the Veterans Health Administration. Annu Rev Public Health. 2017 Mar 20;38:467–87. doi: 10.1146/annurev-publhealth-031816-044255. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 4.Berwick DM. Disseminating innovations in health care. JAMA. 2003 Apr 16;289(15):1969–75. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- 5.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovation in service organizations: Systematic review and recommendations. Milbank Q. 2004;82(4):581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gawande A. Slow ideas [Internet] New York, NY: The New Yorker; 2013. Jul 29, [cited 2018 Mar 7]. Available from: www.newyorker.com/magazine/2013/07/29/slow-ideas. [Google Scholar]
- 7.Tedja R, Gordon S. Hospital-acquired, health care-associated, and ventilator-associated pneumonia. Cleveland Clinic. 2013. Available from: https://teachmemedicine.org/cleveland-clinic-2.
- 8.Munro S, Haile-Mariam A, Greenwell C, Demirci S, Farooqi O, Vasudeva S.Implementation and dissemination of a Department of Veterans Affairs oral care initiative to prevent hospital-acquired pneumonia among nonventilated patients Nurs Admin Q 2018October/December424363–72. 10.1097/naq.0000000000000308 [DOI] [PubMed] [Google Scholar]
- 9.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement Sci. 2009 Aug 7;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weiner BJ. A theory of organizational readiness for change. Implement Sci. 2009 Oct 19;4:67. doi: 10.1186/1748-5908-4-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rogers EM. Diffusion of innovations. New York, NY: Free Press; 1995. [Google Scholar]
- 12.Denis JL, Hebert Y, Langley A, Lozeau D, Trottier LH. Explaining diffusion patterns for complex health care innovations. Health Care Manage Rev. 2002 Summer;27(3):60–73. doi: 10.1097/00004010-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Foy R, MacLennan G, Grimshaw J, Penney G, Campbell M, Grol R. Attributes of clinical recommendations that influence change in practice following audit and feedback. J Clin Epidemiol. 2002 Jul;55(7):717–22. doi: 10.1016/S0895-4356(02)00403-1. [DOI] [PubMed] [Google Scholar]
- 14.Barsh J, Capozzi MM, Davidson J. Leadership and innovation [Internet] New York, NY: McKinsey Q; 2008. Jan, [cited 2019 Mar 18]. Available from: www.mckinsey.com/business-functions/strategy-and-corporate-finance/our-insights/leadership-and-innovationwww.mckinsey.com/business-functions/strategy-and-corporate-finance/our-insights/leadership-and-innovation. [Google Scholar]