Abstract
Multiple transposition procedures have been described for management of lateral rectus palsy. However, relative effect and indications of each procedure are unclear. This systematic review was planned to evaluate functional and anatomical outcomes of vertical rectus transposition (VRT) surgery in patients with lateral rectus palsy. We searched databases in English language, namely, MEDLINE, PubMed Central, EMBASE, Google Scholar, Scopus, and Index Copernicus without any date restrictions in electronic searches, using the search words ‘vertical rectus transposition for lateral rectus palsy,” “vertical rectus transposition for abducens palsy,” “superior rectus transposition,” “inferior rectus transposition,” and “Hummelsheim procedure.” References of the selected publications were also searched to find any relevant studies. We searched for studies that provided data on single VRT and double VRT surgeries for lateral rectus palsies. Three authors independently assessed the related studies gathered from electronic and manual searches. We found 27 studies which were relevant to the review question. As there were no randomized control trials (RCTs) available related to our study question, nonrandomized studies were used to arrive at summarization of outcomes of different transposition procedures. There is a need for prospective RCTs to investigate the different types of transposition procedures for lateral rectus palsy.
Keywords: Inferior rectus palsy, lateral rectus palsy, superior rectus palsy, transposition, vertical rectus palsy
The management of lateral rectus (LR) palsy is evolving. Numerous studies have published different surgeries involving single or multiple groups of muscles, to tackle the deviation and/or movement limitation, including vertical recti muscles. While all these vertical rectus procedures have shown significant correction in primary gaze, efficacy of each procedure is unclear. This review has been conducted to look into details of patient groups included in the surgical studies, their outcomes, and the complications to determine the effect of vertical rectus transposition (VRT) surgery in patients with lateral rectus palsy.
Methods
Types of studies
All studies published in English literature till 30 September 2018 relevant to our study question were included. After an extensive search, while no randomized control trial (RCTs) were found related to it, we also looked at studies that did not perform randomization to allocate patients to treatment groups. Many of the reports represented small case series of one single type of procedure. Few studies were found to be comparative, dividing the outcomes based on two or three different surgeries. In these studies, we only considered the findings of the participant subgroups that satisfied our inclusion criteria and were relevant to our review question.
Types of participants
We included studies having patients with the following characteristics:
Cases of chronic lateral rectus palsy
At least some kind of transposition procedure performed in all patients.
Studies having patient population with the following characteristics were excluded:
All other causes of esotropia
Patients with Duane's retraction syndrome.
Types of interventions
We included studies that evaluated interventions for lateral rectus palsy, with specific therapeutic interest being transposition of vertical recti muscles. Acceptable surgical interventions included any transposition procedure used to achieve the goal of reaching ocular alignment. In cases where multiple surgeries had been performed, the primary application of transposition procedure was the defining criterion for determining eligibility.
Types of outcome measures
Primary outcomes
The primary outcome for comparison in this review was the amount of correction achieved by individual transposition procedures.
Secondary outcomes
The following secondary outcomes were compared:
Improvement of abduction function
Improvement of binocular visual field
Complications related to each type of intervention.
Search methods for identification of studies
The databases that were searched to look for relevant literature in English language were MEDLINE, PubMed Central, EMBASE, Google Scholar, Scopus, and Index Copernicus without any date restrictions in electronic searches, using the search words “vertical rectus transposition for lateral rectus palsy,” “vertical rectus transposition for abducens palsy,” “SRT,” “superior rectus transposition,” “inferior rectus transposition,” and “Hummelsheim procedure.” The last search of databases was performed on 30 September 2018. Manual search was also performed from the relevant references in the reviewed studies.
Study selection
All titles and abstracts were independently reviewed by three authors who identified studies from searches which met the inclusion criteria for the review. We obtained full-length articles for all literature adjudged to be extremely relevant for our study and three authors independently rated them to determine their eligibility of inclusion. Data were analyzed using IBM SPSS Statistics for Windows, Version 21.0. (Armonk, NY: IBM Corp) to determine the weighted averages of the concerned data.
Results
Results of the search
We obtained 27 surgical studies from the databases, which were found relevant to be included in this review. Of these studies, only one study reported comparison between single and double vertical rectus transpositions (dVRTs), but it was not an RCT.[1] A list of the studies which were found relevant to the review question has been tabulated in Table 1 with the clinical outcomes. An analysis of the ranges of corrections of the different surgical procedures has been demonstrated in Table 2. We calculated the weighted average of the mean correction in esodeviation achieved in the studies.
Table 1.
Summary of included studies relevant to the review question
| Study | Type of surgery | No. of eyes | Preop esotropia (p.d.) | Postop esotropia (p.d.) | Success (%) | Preop Abduction limitation | Postop Abduction limitation | Average follow-up (months) | Binocular field improvement |
|---|---|---|---|---|---|---|---|---|---|
| Struck et al.[2] | Full-tendon double VRT with post augmentation | 5 | 36 | 10.2 | 90 | −3.9 | −1.75 | - | |
| Neugebauer et al.[3] | Partial tendon VRT | 13 | 22.33±6.74 | −0.2±2.61 | - | −3.07±1.99 | 1.11±1.76 | 1.5 | 3/7 patients |
| Modified Partial tendon VRT | 19 | 25.54±5.66 | 0.95±5.26 | - | −2.71±1.7 | 1.41±1.74 | 1.5 | 2/9 patients | |
| Hendler et al.[4] | Full- or partial tendon double VRT augmented by resection | 7 | 30.6±12.9 | 10.6±8.8 | - | −3.6 | −2.8 | 3.8 | |
| Gonzales et al.[5] | Full-tendon double VRT | 9 | 38.2 | 2.2 | - | −4.1 | −3.2 | 7.2 | |
| Full-tendon double VRT with resection | 7 | 48.9 | 2.5 | - | −4.4 | −2.7 | 6.7 | ||
| Full-tendon double VRT with post augmentation sutures | 11 | 60.3 | 19 | - | −4.7 | −3.3 | 9.5 | ||
| Nishida et al.[6] | Partial tendon VRT | 6 | Average correction=44.7 | - | - | - | 58.3 | 7/9 patients | |
| Partial tendon VRT + MRc | 6 | Average correction=62.7 | - | - | - | ||||
| Foster[7] | Full-tendon double VRT with post augmentation | 8 | 44.4 | 1.6 | 82 | −5 | −3.06 | 24 | |
| Full-tendon double VRT with post augmentation + MRc | 3 | 58.3 | 18 | 90 | −5 | −3.3 | |||
| Simons et al.[8] | Full-tendon double VRT with post augmentation | 7 | Average correction=41.2 | 42.8 | −3.8 | −2.6 | 3 | ||
| Paysse et al.[9] | Full-tendon double VRT with post augmentation | 10 | 45 | 4.8 | 50 | −3.5 | −2.5 | 10.8 | |
| Partial tendon double VRT with post augmentation | 1 | 30 | 2 | - | −3.2 | −3.0 | |||
| Yazdian et al.[10] | Full-tendon double VRT with post augmentation | 24 | 44.7±7.2 | 12.5±4.0 | - | −4.0 | −2.0 | - | |
| Hong et al.[11] | Full-tendon VRT with post augmentation | 11 | 59±15 | 16±12 | 69 | −5 | −4.7 | 19.8 | 13/16 patients |
| Akar et al.[12] | Full-tendon double VRT with post augmentation | 47 | 42.05±7.4 | 0.71±0.08 | 99 | −3.9±0.4 | −1.7±0.6 | 37.09 | 38/47 patients |
| Britt et al.[13] | Partial tendon VRT with post augmentation | 5 | 45.2±23.9 | −5±14.1 | 60 | −4.45 | −2.87 | 2.3 | |
| Bansal et al.[14] | Full-tendon double VRT | 21 | 48.3 | 16.08 | 55.6 | - | - | 4 | |
| Couser et al.[15] | Partial tendon VRT + MRc | 10 | 43±5 | 6±7 | 80 | −4 | −3 | 3 | |
| Singh et al.[16] | Partial tendon VRT + MRc | 15 | 58.3±10.8 | 7.2±5.1 | 80 | - | - | 6 | 6/15 patients |
| Brooks et al.[17] | Partial tendon double VRT + MRc | 4 | 54 | 2 | - | - | - | 1.5 | |
| Flanders et al.[18] | Full-tendon double VRT + Botox | 5 | Average correction=66 | - | −6 | −1.7 | 21 | ||
| Leiba et al.[19] | Full-tendon double VRT + Botox | 22 | 38.1±11.6 | 7.9±8.8 | 59 | - | - | 44.2 | 6/22 patients |
| Rosenbaum et al.[20] | Full-tendon double VRT + Botox | 10 | Average correction=55 | - | - | - | - | ||
| Mehendale et al.[21] | Single VRT (SRT) + post augmentation + MRc | 7 | 53.5 | 16.8 | - | −4.8 | −3 | 10 | |
| Patil-Chhablani et al.[22] | Single VRT (SRT) + post augmentation + MRc | 15 | 55.54±24 | 9.9±10 | 69 | −5 | −3.1 | 12 | |
| Agarwal et al.[23] | Single VRT (SRT) + MRc | 10 (7 underwent post augmentation) | 51.5±18.8 | 6.1±10.7 | - | −3.8 | −2 | 6 | 4/10 patients |
| Velez et al.[24] | Single VRT (IRT) with post augmentation | 7 | 47.42 | 8.71 | - | −4.4±0.5 | −3.4±0.9 | 2 | |
| Lee et al.[1] | Full-tendon double VRT (four lateral fixation) | 8 | 55.6 | 10.3 | - | −4.5 | −3.8 | 17.3 | |
| Single VRT (SRT) + MRc | 8 | 41.9 | 7.1 | - | −4.6 | −3 | 6.2 | ||
| Liu et al.[25] | Single VRT (SRT) +MRc | 11 | 82.27 | 32.72 | 46.15 | −5.6 | −3.6 | 9.5 | |
| Single VRT (SRT) | 2 | 80 | 10 | −4 | −3 | ||||
| Akbari et al.[26] | Single VRT (SRT) + post augmentation | 11 | 28±8.5 | 8.4±7.3 | - | −4 | −3 | 4 | |
| Kinori et al.[27] | Partial tendon double VRT with post augmentation + MRc + LR plication (single paper) | 9 | 70.55 | Variable corrections reported (residual resotropia to consecutive exotropia) | −6.4 | −3.06 | 7 | ||
p.d.=Prism diopters; VRT=Vertical rectus transposition; MRc=Medial rectus recession; post augmentation=Posterior augmentation Foster’s suture; LR=Lateral rectus; SRT=Superior rectus transposition
Table 2.
Surgical techniques described in relevant studies with their range of corrections
| Range of mean correction of studies (p.d.) | Weighted average of esodeviation corrections in studies (p.d.) | Weighted average of abduction improvement in studies (p.d.) | |
|---|---|---|---|
| Full-tendon double VRT without augmentation[1,4,5,14] | 20-36 | 34.71 | 0.39 |
| Full-tendon double VRT with post augmentation[2,4,5,7,8,10,11,12] | 25.8-43 | 38.05 | 1.62 |
| Full-tendon double VRT with Botox[18,19,20] | 30-66 | 41.74 | 0.58* |
| Full-tendon double VRT with post augmentation + MRc (single paper)[7] | 40.3 | ||
| Partial tendon double VRT without augmentation[3,4,6] | 25.1-44.7 | 31.99 | 2.72 |
| Partial tendon double VRT with post augmentation[9,13] | 37-62.7 | 58.25 | 0.29* |
| Partial tendon double VRT + MRc[6,15,17] | 37-52 | 46.92 | 1.35 |
| Partial tendon double VRT with post augmentation + MRc (single paper)[16] | 51.08 | ||
| Partial tendon double VRT with post augmentation + LR resection + MRc/chemodenervation (single paper)[27] | Variable corrections reported (residual esotropia to consecutive exotropia) | ||
| Single VRT + MRc[1,23,25] | 34.8-45.4 | 44.05 | 0.84 |
| Single VRT + post augmentation[24,26] | 19.6-38.7 | 27.03 | 1.82 |
| Single VRT + post augmentation + MRc[21,22] | 36.7-45.6 | 42.8 | 1.87 |
p.d.=Prism diopters, VRT=Vertical rectus transposition, MRc=Medial rectus recession, Post augmentation=Posterior augmentation Foster’s suture. *Single data
Discussion
The aim of the current review was to compare the outcomes of various surgeries reported in published studies so that the effect of each procedure could be evaluated. In the absence of any prospective RCTs evaluating the different types of transposition procedures for lateral rectus palsy, other type of studies were included. The main difficulty in comparing these studies was that the severity of lateral rectus palsy was quite variable among the different patient groups. Moreover, the outcome measures after transposition surgeries have also been differently reported as mean esotropia correction, residual esotropia, change in binocular visual field, and/or improvement of abduction function. The different types of transposition surgeries have been divided for the ease of understanding in the following manner. Fig. 1 summarizes these different options of surgeries available from literature.
Figure 1.
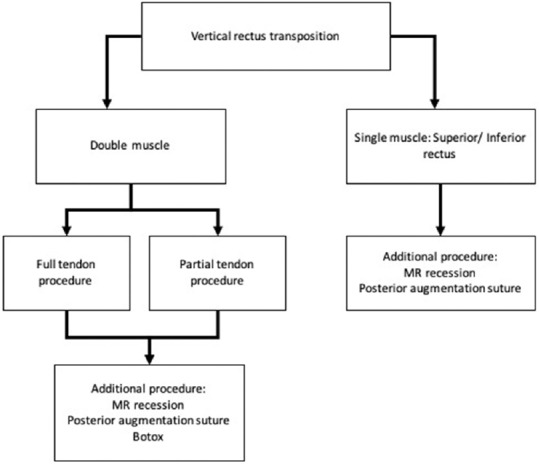
Summary of the different types of transposition surgeries and additional procedures described in literature for chronic lateral rectus palsy
Full-tendon double vertical rectus transpositions (dVRTs)
Full-tendon dVRT has been believed to be more effective than partial tendon dVRT, although there is always a risk of anterior segment ischemia in case of any additional interventions on horizontal recti. Rosenbaum et al. have described full-tendon dVRT without disinsertion of muscles, thereby sparing the ciliary vessels.[28] This technique of shifting the bellies of the two vertical recti closer to the anterior border of the lateral rectus muscle has also been elaborated by Hendler et al. and Nishida et al.[4,6]
Partial tendon double vertical rectus transpositions (pVRTs)
This involves transposition of partial tendons of superior and inferior recti to the paretic lateral rectus. The advantage of a partial tendon transfer is that at least one ciliary vessel (nasal) on each of the vertical rectus is spared, which reduces the possibility of anterior segment ischemia. This may also allow for a simultaneous or a subsequent recession of the ipsilateral medial rectus (MR) muscle especially in cases where the forced duction test is tight for the MR.[15] The authors have reported that subjectively more consistent and predictable outcomes are obtained with pVRT combined with medial rectus recession (MRc) than a full-tendon transposition procedure. Representative images of partial tendon double VRT are shown in Fig. 2.
Figure 2.
A case of left post traumatic lateral rectus palsy (top) treated with partial tendon double vertical rectus transposition with posterior augmentation suture (bottom)
Additional procedures (MR recession/chemodenervation/posterior fixation suture)
Simultaneous ipsilateral MR recession (MRc) or chemodenervation of the MR muscle may be synergistic to the effect of VRT. While chemodenervation weakens the antagonist and reduces the risk of anterior segment ischemia, the effect may wane over a period of time. However, Bansal et al. demonstrated that it is not essential to recess the MR muscle along with VRT and that it may be needed only in cases of a tight MR.[14] The posterior augmentation suture technique was demonstrated by Foster, to significantly reduce the need for ipsilateral MRc, thereby minimizing the risk of anterior segment ischemia.[10] A modified augmentation suture by Struck, which requires just one posterior suture instead of two, has shown similar efficacy as the original technique with added advantage of minimal risk of lateral slippage of muscles and a resultant unwanted vertical deviation.[2] A single article by Kinori et al. has evaluated lateral rectus (LR) plication along with MRc and posterior augmentation with partial tendon double VRT.[27] The included abducens palsy patients in this study had preoperative esotropias mostly in the range of ~95 prism diopter (p.d.), which after corrections led to residual esotropias and consecutive exotropias, and the results were quite variable.
Single VRT (superior rectus/inferior rectus)
Superior rectus transposition (SRT) was described by Johnston et al. as an alternative to dVRT to reduce the risk of anterior segment ischemia.[1,6] It has been compared to isolated MR recession procedures and has been seen to have significantly greater improvement in abduction along with long-term alignment.[29] Representative images of SRT are shown in Fig. 3.
Figure 3.
A case of left posttraumatic lateral rectus (top) palsy treated with superior rectus transposition with posterior augmentation suture along with a medial rectus recession (bottom)
Inferior rectus transposition (IRT) was first described by Velez et al., who stated that IRT may address both the esotropia and hypertropia by intervening a single vertical rectus muscle in patients with lateral rectus palsy with a preexisting hypertropia.[24] None of the single VRT patients have shown postoperative symptomatic cyclotorsional diplopia or significant vertical tropias. A single nonrandomized study comparing patients undergoing single VRT with simultaneous MRc against those undergoing double VRT is included in the review and is discussed separately.[1] A median correction of 36.4 p.d. was found in the SRT + MRc group versus 45.4 p.d. in the double VRT group. Limitation of abduction improved from −4.6 to −3 in SRT group against an improvement of −4.5 to −3.8 in VRT group. There was no residual eso- or exotropia in primary gaze in any patient. However, there appears to be a selection bias in the population with VRT group having larger preexisting esodeviation (55.6 p.d.) than the SRT with MRc group (41.9 p.d.).
Correction achieved along with their weighted averages by various combinations of surgeries described in the studies included in this review is provided in Table 2. Maximum correction effect was seen in partial tendon double VRT with posterior augmentation (58.25 p.d.), followed by partial tendon double VRT with MRc (46.92 p.d.). Simultaneous additional procedures (posterior augmentation and MRc) to pVRT also appeared to have significant additional effect [Table 2]; however, only a single study[16] has evaluated it. Surprisingly, full-tendon double VRT procedures appear to have lesser overall correction effect than partial tendon double VRT procedures. Our analysis shows that a partial double VRT procedure with MRc may be preferred over a full-tendon VRT to achieve higher esodeviation corrections, as the latter even with additional procedures shows lower mean correction.
Rosenbaum et al. have discussed that if the initial esodeviation in primary gaze was more than 20 p.d., augmentation sutures were very effective in correction of esotropia with a residual esotropia of 5 p.d. in the augmentation group against 12 p.d. in the group without augmentation.[27] While our analysis also shows that augmentation sutures are synergistic to the transposition procedure, MR weakening also significantly enhances its effect and being adjustable has an added advantage of providing better postoperative alignment. Though intraoperative chemodenervation may have similar effect as MRc, the effect may be transient lasting for up to 3 months and may wean off by 12 months.[19,20]
According to our analysis, single VRT with MRc appears to be an effective procedure (mean correction = 44.05 p.d.) and has lower risk of anterior segment ischemia along with the opportunity of postoperative adjustment. From Table 2, we can observe that augmented suture with single VRT does not appear to significantly affect the amount of correction achieved. A recent study by Liu et al. has evaluated the outcomes of SRT with posterior augmentation sutures and investigated the prognostic factors for predicting successful outcome.[25] They found that preoperative abduction deficit was the only important prognostic factor towards a successful outcome. They also evaluated IRT as an additional procedure in patients with residual esotropia and the success rate after second surgery improved from 46% to 100%. As single VRT is increasingly becoming the first choice for lateral rectus palsy, the question of whether IRT or MRc should be chosen as the secondary surgery for residual esotropia needs further investigation. Table 1 also tabulates the improvement of binocular single vision reported in the studies; however, no quantification could be done since none of the studies has reported the fields quantitatively. Rosenbaum et al. have reported that binocular field of vision improves significantly more with transposition procedures compared with MRc with lateral rectus resection for abducens palsy.[28] Addition of posterior augmentation sutures may further increase the binocular field of vision.[7,12] Similarly, residual face turn may also be significantly smaller with augmentation sutures.[7,12] Moreover, torticollis correction has been reported in two studies, and Velez et al. have reported a correction of 27° of torticollis.[2,24]
The most important concern with single VRT alone has been the possibility of induced vertical deviations and torsional diplopia. Patients particularly at risk for these complications include younger patients and patients with preoperative hypertropia or incyclotropia.[30] Lee and Lambert found that two patients in the SRT group who had small angle hypertropia preoperatively showed a resolution of the same after surgery. However, none of the patients reported any torsional diplopia postoperatively. Although lateral transposition of SR during SRT is expected to theoretically cause incyclotorsion, significant clinical torsional deviation has not been documented in literature till now.[21,31] Velez et al. have reported incyclotorsions with IRT which were not clinically significant. However, it is important to note any preexisting incyclotorsion in patients that can get aggravated following the intervention.[30] The effect on abduction improvement after the procedures is difficult to assess as there is great variability in its evaluation and reporting in the various studies. However, augmentation sutures do seem to enhance abduction particularly in single VRT procedures.[1]
Quality of the evidence and biases
Three independent authors applied an extensive search method to identify relevant studies, which included multiple sources like electronic literature databases and citation lists to avoid missing any study which might be relevant. However, we could not account for the studies in other languages which might have been missed from inclusion in this review. The nonrandomized studies which were identified as relevant to the study question contained mild underlying differences among groups on grounds such as age groups, differences in duration of follow-up, reasons for not completing recommended follow-up period, and difference in scale for evaluation of abduction limitation. The criterion for inclusion for all the studies was alignment at the last follow-up, and the amount of correction achieved was compared among the studies. It is clear from the review that while there is no rigorous evidence with regard to preferring any particular type of transposition procedure, partial tendon double VRT with augmentation or MR recession and single VRT may be preferred, depending on preexisting esodeviation and also experience and choice of surgeon.
Conclusion
The aim of this review was to look at the effect of transposition procedures for the management of lateral rectus palsy. In the absence of any good quality RCTs, this study has evaluated nonrandomized case series and summarized the impact of different procedures with relation to transposition surgery. Till well-designed RCTs are available, it may be advisable that surgeons continue practicing a case-based approach in deciding the choice of surgery based on the available evidence and their own experience and expertise.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lee YH, Lambert SR. Outcomes after superior rectus transposition and medial rectus recession versus vertical recti transposition for sixth nerve palsy. Am J Ophthalmol. 2017;177:100–5. doi: 10.1016/j.ajo.2017.02.019. [DOI] [PubMed] [Google Scholar]
- 2.Struck MC. Augmented vertical rectus transposition surgery with single posterior fixation suture: Modification of Foster technique. J AAPOS. 2009;13:343–9. doi: 10.1016/j.jaapos.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 3.Neugebauer A, Fricke J, Kirsch A, Rüssmann W. Modified transposition procedure of the vertical recti in sixth nerve palsy. Am J Ophthalmol. 2001;131:359–63. doi: 10.1016/s0002-9394(00)00805-9. [DOI] [PubMed] [Google Scholar]
- 4.Hendler K, Pineles SL, DemerJL, Yang D, Velez FG. Adjustable augmented rectus muscle transposition surgery with or without ciliary vessel sparing for abduction deficiencies. Strabismus. 2014;22:74–80. doi: 10.3109/09273972.2014.904901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gonzales MP, Kraft SP. Outcomes of three different vertical rectus muscle transposition procedures for complete abducens nerve palsy. J AAPOS. 2015;19:150–6. doi: 10.1016/j.jaapos.2015.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Nishida Y, Inatomi A, Aoki Y, Hayashi O, Iwami T, Oda S, et al. A muscle transposition procedure for abducens palsy, in which the halves of the vertical rectus muscle bellies are sutured onto the sclera. Jpn J Ophthalmol. 2003;47:281–6. doi: 10.1016/s0021-5155(03)00021-2. [DOI] [PubMed] [Google Scholar]
- 7.Foster RS. Vertical muscle transposition augmented with lateral fixation. J AAPOS. 1997;1:20–30. doi: 10.1016/s1091-8531(97)90019-7. [DOI] [PubMed] [Google Scholar]
- 8.Simons BD, Siatkowski RM, Neff AG. Posterior fixation suture augmentation of full tendon vertical rectus muscle transposition for abducens palsy. J Neuroophthalmol. 2000;20:119–22. doi: 10.1097/00041327-200020020-00012. [DOI] [PubMed] [Google Scholar]
- 9.Paysse EA, Brady McCreery KM, Ross A, Coats DK. Use of augmented rectus muscle transposition surgery for complex strabismus. Ophthalmology. 2002;109:1309–14. doi: 10.1016/s0161-6420(02)01072-2. [DOI] [PubMed] [Google Scholar]
- 10.Yazdian Z, Rajabi MT, Ali Yazdian M, Rajabi MB, Akbari MR. Vertical rectus muscle transposition for correcting abduction deficiency in Duane's syndrome type 1 and sixth nerve palsy. J Pediatr Ophthalmol Strabismus. 2010;47:96–100. doi: 10.3928/01913913-20100308-07. [DOI] [PubMed] [Google Scholar]
- 11.Hong S, Chang YH, Han SH, Lee JB. Effect of full tendon transposition augmented with posterior intermuscular suture for paralytic strabismus. Am J Ophthalmol. 2005;140:477–83. doi: 10.1016/j.ajo.2005.04.028. [DOI] [PubMed] [Google Scholar]
- 12.Akar S, Gokyigit B, Pekel G, Demircan A, Demirok A. Vertical muscle transposition augmented with lateral fixation (Foster) suture for Duane syndrome and sixth nerve palsy. Eye (Lond) 2013;27:1188–95. doi: 10.1038/eye.2013.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Britt MT, Velez FG, Thacker N, Alcorn D, Foster RS, Rosenbaum AL. Partial rectus muscle–augmented transpositions in abduction deficiency. J AAPOS. 2003;7:325–32. doi: 10.1016/s1091-8531(03)00180-0. [DOI] [PubMed] [Google Scholar]
- 14.Bansal S, Khan J, Marsh IB. Unaugmented vertical muscle transposition surgery for chronic sixth nerve paralysis. Strabismus. 2006;14:177–81. doi: 10.1080/09273970601026201. [DOI] [PubMed] [Google Scholar]
- 15.Couser NL, Lenhart PD, Hutchinson AK. Augmented Hummelsheim procedure to treat complete abducens nerve palsy. J AAPOS. 2012;16:331–5. doi: 10.1016/j.jaapos.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh P, Vijayalakshmi P, Shetty S, Vora P, Kalwaniya S. Double augmented vertical rectus transposition for large-angle esotropia due to sixth nerve palsy. J Pediatr Ophthalmol Strabismus. 2016;53:369–74. doi: 10.3928/01913913-20160810-01. [DOI] [PubMed] [Google Scholar]
- 17.Brooks SE, Olitsky SE, de BRG. Augmented Hummelsheim procedure for paralytic strabismus. J Pediatr Ophthalmol Strabismus. 2000;37:189–95. doi: 10.3928/0191-3913-20000701-04. [DOI] [PubMed] [Google Scholar]
- 18.Flanders M, Qahtani F, Gans M, Beneish R. Vertical rectus muscle transposition and botulinum toxin for complete sixth nerve palsy. Can J Ophthalmol. 2001;36:18–25. doi: 10.1016/s0008-4182(01)80062-4. [DOI] [PubMed] [Google Scholar]
- 19.Leiba H, Wirth GM, Amstutz C, Landau K. Long-term results of vertical rectus muscle transposition and botulinum toxin for sixth nerve palsy. J AAPOS. 2010;14:498–501. doi: 10.1016/j.jaapos.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 20.Rosenbaum AL, Kushner BJ, Kirschen D. Vertical rectus muscle transposition and botulinum toxin (Oculinum) to medial rectus for abducens palsy. Arch Ophthalmol. 1989;107:820–3. doi: 10.1001/archopht.1989.01070010842025. [DOI] [PubMed] [Google Scholar]
- 21.Mehendale RA, Dagi LR, Wu C, Ledoux D, Johnston S, Hunter DG. Superior rectus transposition and medial rectus recession for duane syndrome and sixth nerve palsy. Arch Ophthalmol. 2012;130:195–201. doi: 10.1001/archophthalmol.2011.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Patil-Chhablani P, Kothamasu K, Kekunnaya R, Sachdeva V, Warkad V. Augmented superior rectus transposition with medial rectus recession in patients with abducens nerve palsy. J AAPOS. 2016;20:496–500. doi: 10.1016/j.jaapos.2016.07.227. [DOI] [PubMed] [Google Scholar]
- 23.Agarwal R, Sharma M, Saxena R, Sharma P. Surgical outcome of superior rectus transposition in esotropic Duane syndrome and abducens nerve palsy. J AAPOS. 2018;22:12–6. doi: 10.1016/j.jaapos.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 24.Velez FG, Chang MY, Pineles SL. Inferior rectus transposition: A novel procedure for abducens palsy. Am Jour Ophthalmol. 2017;177:126–30. doi: 10.1016/j.ajo.2017.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu Y, Wen W, Zou L, Wu S, Wang S, Liu R, et al. Application of SRT plus MR recession in supra-maximal esotropia from chronic sixth nerve palsy. Graefes Arch Clin Exp Ophthalmol. 2019;257:199–205. doi: 10.1007/s00417-018-4102-x. [DOI] [PubMed] [Google Scholar]
- 26.Akbari M, Shomali S, Mirmohammadsadeghi A, Fard MA. Augmented superiorrectustransposition procedure in Duane retraction syndrome compared with sixthnervepalsy. Graefes Arch Clin Exp Ophthalmol. 2018;256:983–7. doi: 10.1007/s00417-017-3885-5. [DOI] [PubMed] [Google Scholar]
- 27.Kinori M, Miller KE, Cochran M, Patil PA, El Sahn M, Khayali S. Plication augmentation of the modified Hummelsheim procedure for treatment of large-angle esotropia due to abducens nerve palsy and type 1 Duane syndrome. J AAPOS. 2015;19:311–5. doi: 10.1016/j.jaapos.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 28.Rosenbaum AL. Costenbader Lecture: The efficacy of rectus muscle transposition surgery in esotropic Duane syndrome and VI nerve palsy. J AAPOS. 2004;8:409–19. doi: 10.1016/j.jaapos.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 29.Johnston SC, Crouch ER, Jr, Crouch ER. An innovative approach to transposition surgery is effective in treatment of Duane's syndrome with esotropia [ARVO abstract] Invest Ophthalmol Vis Sci. 2006;47 e-abstract 2475. [Google Scholar]
- 30.Velez FG, Oltra E, Isenberg SJ, Pineles SL. Assessment of torsion after superior rectus transposition with or without medial rectus recession for Duane syndrome and abducens nerve palsy. J AAPOS. 2014;18:457–60. doi: 10.1016/j.jaapos.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tibrewal S, Sachdeva V, Ali MH, Kekunnaya R. Comparison of augmented superior rectus transposition with medial rectus recession for surgical management of esotropic Duane retraction syndrome. J AAPOS. 2015;19:199–205. doi: 10.1016/j.jaapos.2015.02.006. [DOI] [PubMed] [Google Scholar]




