Abstract
Objectives. To assess the health impact of Hurricane Irma and Hurricane Maria on St Thomas, US Virgin Islands.
Methods. We collected data from interviews conducted 6 and 9 months after the hurricanes, a review of 597 randomly selected emergency department (ED) encounters, and administrative records from 10 716 ED visits 3 months before, between, and 3 months after the hurricanes.
Results. Informants described damaged hospital infrastructure, including flooding, structural damage, and lost staff. The greatest public health impact was on the elderly and persons with chronic diseases. In the setting of loss of the electronic medical record system, ED chart reviews were limited by problems with missing data. ED administrative data demonstrated that posthurricane patients, compared with prehurricane patients, were older and had less severe complaints. There was a significant increase in patients being seen for diabetes-related and respiratory complaints, especially asthma. Suboptimal recordkeeping for medical evacuees limited the ability to assess outcomes for patients with severe illnesses.
Conclusions. Hurricanes Irma and Maria caused major disruptions to health care on St Thomas. Emphasis should be given to building a resilient health care system that will optimally respond to future hurricanes.
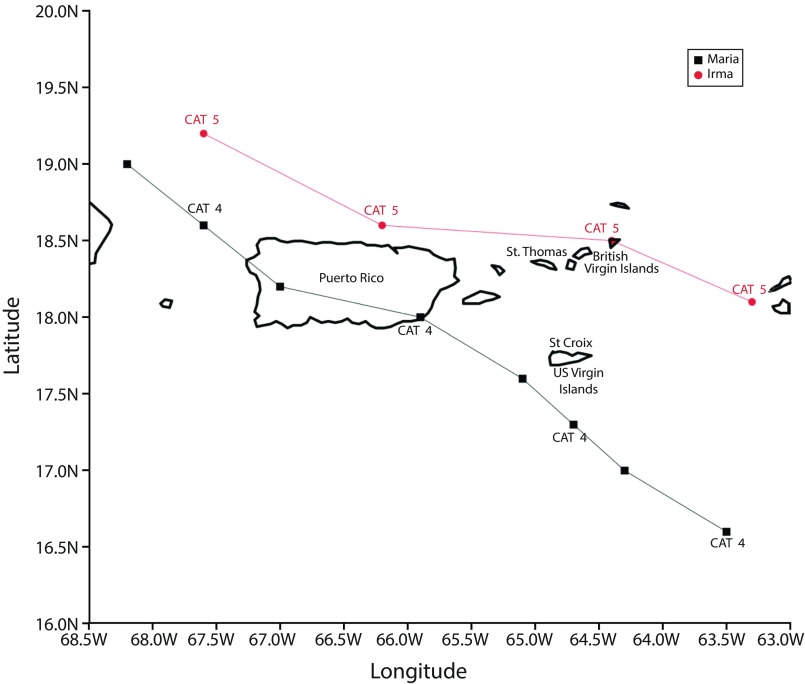
Hurricane Irma passed over St Thomas, US Virgin Islands (USVI) as a Category 5 storm on September 6, 2017, with peak winds of 178 miles per hour (Figure 1).1 Two weeks later, on September 20, 2017, Hurricane Maria hit St Croix, to the southeast, as a Category 5 storm, moved across Puerto Rico, and then brushed by St Thomas. Peak winds on St Thomas hit 64 miles per hour, with damage accrued primarily through flooding and mudslides.2,3 The impact of these storms on medical care in Puerto Rico4 has only recently become apparent. While 64 deaths were officially attributed to the storms in Puerto Rico, excess storm-related mortality in Puerto Rico has been estimated to be between 1139 (95% confidence interval [CI] = 1006, 1272)5 and 4645 (95% CI = 793, 8498) deaths.6
FIGURE 1—
Tracks of Hurricanes Irma and Maria: US Virgin Islands and Puerto Rico, 2017
Note. CAT = category.
Source. Courtesy of Vasubandhu Misra, PhD, Florida Climate Institute. Reprinted with permission.
Fewer data are available on the medical impact of these 2 storms on the USVI (Figure 1). St Thomas is the most populated island and home to the territorial capital. The Schneider Regional Medical Center (SRMC) on St Thomas is the only hospital on the island and has the only fully equipped emergency department (ED) for St Thomas and St John, serving a population of approximately 55 000.7 Following the landfall of Hurricane Irma, the SRMC experienced loss of power, collapse of the fourth floor of the hospital, destruction of the building housing its cancer center, and flooding of the ED (Appendix A, Figure A, available as a supplement to the online version of this article at http://www.ajph.org)8; there was also loss of the electronic medical record system, necessitating a shift to paper records for approximately 1 month.
In response to this hurricane-related disaster, the SRMC emergency department moved all operations to medical tents pitched in the parking lot.9 During these operations, hospital patients whose care exceeded the resources of SRMC, including as many as 200 dialysis patients,10–12 were evacuated to St Croix, Puerto Rico, and locations in the continental United States. On September 19, 2017, hospital staff received an order to disassemble their tent ED and shelter for a second Category 5 storm, Hurricane Maria, which was headed for the island.
While St Croix and Puerto Rico took the brunt of Maria’s impact, widespread flooding and additional wind damage led to further destruction and halted recovery operations on St Thomas. The emergency response to both hurricanes in all 3 USVI islands brought in an estimated 13 000 service and rescue personnel, resulted in the evacuation of close to 800 patients, left almost 40 000 without power, and generated in excess of 200 000 million cubic yards of debris10,13,14 (Appendix A, Figure B).
Five USVI deaths were officially attributed to the hurricanes.15 Based on the data cited previously from Puerto Rico, it is likely that there were excess hurricane-related deaths in the USVI. With the recognized increases in sea surface temperatures in the Caribbean, there is a reasonable likelihood that the USVI will face storms of similar or greater magnitude in the coming years.16 A clear understanding of the medical impact of the 2017 hurricanes on the islands is essential in optimizing current recovery strategies and in planning for future storms. We present here initial data on the medical impact of the 2017 storms on St Thomas, with a focus on data from SRMC and its ED.
METHODS
In collaboration with SRMC staff and administration, our investigative team from the University of Florida and the University of Maryland visited SRMC in March and July 2018. We assembled original data from 3 sources: key informant interviews, retrospective chart review, and administrative record review. We established data use agreements to permit the review of de-identified ED records from the SRMC electronic medical record system and the administrative database.
Key Informant Interviews
In March 2018, we collected structured interview data from 10 ED nursing personnel, guided by 7 specific questions related to their posthurricane patient experiences working in the ED; sampling was stopped once saturation was reached and because staff shortages limited interview opportunities. In July 2018, we conducted more comprehensive semistructured and open-ended qualitative interviews with hospital administrators, physicians, and medical records staff. For these interviews, 2 key informants were initially identified by an intermediary between the research team and SRMC, and the sample expanded to 29 via snowball sampling. Interviews were based upon themes of hurricane experiences at the SRMC, ED, and medical community and efforts to respond to urgent and nonurgent patient care needs. Interviews were documented by detailed note taking by a dedicated investigator. These interviews were summarized via content analysis for common, recurring themes, and the content analysis was verified by the interviewees; thereafter, the analysis was integrated into a hurricane narrative for the SRMC.
Timeline
We searched local newspaper reports and Federal Emergency Management Agency (FEMA) releases for Hurricane Irma and Hurricane Maria (FEMA identification DR-4340 and DR-4335) for information relating to storm debris, federal funding, electricity restoration, medical evacuees, and recovery personnel, summarized in Figures A and B. A list of all articles and an archive of all FEMA releases reviewed can be found in Appendix B (available as a supplement to the online version of this article at http://www.ajph.org).
Emergency Department Chart and Administrative Data Review
Our objectives were to identify determinants of posthurricane ED attendance and to determine disease-specific variations among study periods. Hurricane Irma damaged the SRMC electronic medical record system, resulting in a shift from electronic to paper records for approximately 1 month, at a chaotic time when the medical care system was being moving into (and out of) tents in the parking lot. Available paper records were subsequently scanned into the electronic medical records. Data were also entered directly into the electronic administrative records for insurance purposes.
For the ED chart review, we randomly selected and reviewed 597 ED encounters from the SRMC: 200 records represented encounters occurring during the interhurricane period (September 6, 2017, to September 21, 2017) and 388 represented encounters occurring during the posthurricane period (September 22, 2017, to December 31, 2017); 9 charts had missing encounter dates.
Administrative record data review included hospital encounters and ED admissions that occurred between June 1, 2017, and December 31, 2017. We reviewed a total of 10 716 administrative records, which included 4804 pre-, 957 inter-, and 4955 posthurricane cases. Primary data collection included patient demographics, past and current diagnoses, medications, payer status, emergency severity index, ED service times, length of stay, ED disposition, and ED diagnoses (International Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10-CM]).17
Statistical Methodology
The primary outcome in our initial analysis was posthurricane ED attendance. In subsequent models, outcomes were disease-specific incidence by ICD-10-CM classification; the primary predictor in these models was hurricane time period (pre, post) defined by hurricane landfall dates. Covariates of interest included patient’s age, gender, race, insurance status (Medicare, Medicaid, private or commercial, self-pay), and triage priority level at time of visit (critical–urgent, semiurgent, nonurgent). We examined the association between the covariates and each outcome variable by using generalized estimating equations because of the correlated structure of data from repeated measures of ED visits.18,19 We further analyzed disease groupings that showed significant change in a bivariate model for multivariable models, with adjustments for repeated visits by patients. We completed data management and analysis by using Microsoft Excel, version 1908 (Microsoft, Redmond, WA), and SPSS software, version 24.0 (IBM, Somers, NY), and performed all modeling exercises in Stata SE version 15.0 (StataCorp LP, College Station, TX).
On the basis of concerns regarding missing data in the administrative data set, we applied multiple imputation via a fully conditional specification algorithm using the Blimp software application, version 2.0 (Los Angeles, CA), and generated 20 imputed data sets for further analysis.20 Variables (and respective rates of missing data) that were imputed included age (17.3%), gender (17.3%), priority level (27.6%), race (17.3%), payer status (17.3%), and disease diagnosis classification (17.4%). When we repeated the models reported in the article (Figure 2 and Appendix C, Figures C, D, E, and F, available as supplements to the online version of this article at http://www.ajph.org) using imputed data, there were no significant changes in the results of the imputed model versus original data models; data presented represent the original data without imputation unless otherwise noted.
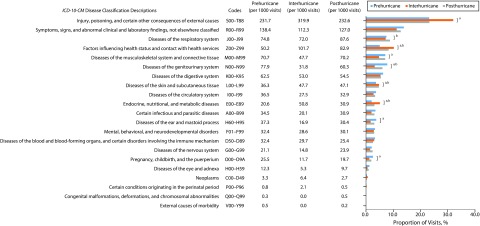
FIGURE 2—
Distribution of Emergency Department International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) Diagnosis Classification by Hurricane Period: Schneider Regional Medical Center, St. Thomas, US Virgin Islands; June 2017–December 2017
aDenotes significant (< .05) difference between ICD-10-CM disease incidence among 3 (pre-, inter-, and posthurricane) periods.
bDenotes significant (< .05) difference between ICD-10-CM disease incidence between pre- and posthurricane periods.
RESULTS
The following sections summarize results of key informant interviews and the review of ED charts and administrative data.
Key Informant Interviews
Emergency department nursing staff (structured interviews; March 2018).
Eighty percent of the ED nurses questioned reported the perception that illness severity increased in patients who visited the ED after the hurricanes; 100% reported that more than half of the adults who visited the ED had complaints related to a chronic medical illness, and 70% indicated that the ED visit could have been prevented if the patients had access to routine medical care or medications after hurricanes. Of the respondents, 90% reported that there was an island-wide decline in the ability of families, friends, and neighbors to provide social support to older, ill people after hurricanes.
Hospital administration (open-ended interviews; July 2018).
Major structural damages to the medical center included the destruction of the SRMC cardiac catheterization laboratory and the Kimelman Cancer Institute, which was adjacent to the hospital; neither had been fully rebuilt at the time of the interviews. In addition, the hospital experienced wind damage and flooding on multiple floors and lost diagnostic tools, including x-ray equipment; there was also damage to the only magnetic resonance imaging machine on the island, which had been located with a private radiology group. Hospital operations were affected by the loss of locum and permanent staff during and after the hurricanes and the temporary relocation of hospital operations to the SRMC parking lot between hurricanes. Financially, the hospital was already short of funds for needed improvements before the hurricanes. After the hurricanes, the hospital had accrued hundreds of millions of dollars in damages, and substantial questions remain about the best way to move forward, weighing the relative benefits of rebuilding, replacing, or accepting the loss of facilities.
Physician and medical records staff (semistructured interviews; July 2018).
The ED medical staff expressed concerns about 2 major groups that were felt to have been disproportionately affected by the hurricane: the elderly and people with chronic conditions. Among the elderly, there were damaged social and support networks, which affected the ability of patients to live independently and manage health. Even more, the elderly were the least capable of evacuating the USVI to seek a setting where health care needs could be addressed.
Inability to obtain medication was noted repeatedly, particularly for patients with chronic illness. There was a perception that there were high rates of diabetes-related morbidities, including infections, amputations, and ketoacidosis, in part because of the acute lack of availability of insulin. There was also a perception that respiratory illnesses increased, with particular vulnerabilities among persons who used nebulizers or oxygen compressors. Of particular concern were 2 asthma-related deaths, noted in part because of the young age of the patients, both in their 40s. Disrupted medication adherence was felt to be a particularly important factor in rates of myocardial infarction, with all myocardial infarction cases having to be promptly transferred off-island because of the closure of the cardiac catheterization laboratory. Patients who were dependent on dialysis were mentioned less frequently, as efforts had been made to transport them off of the island before or between the hurricanes.
The hurricanes had a direct health effect on motor vehicle collisions, primarily because of downed traffic lights, damaged streetlights, and damaged roadways. The hurricanes were also perceived to have amplified behavioral and mental health issues on the island, such as thefts resulting in gunshot wounds, domestic violence, alcohol use disorders, and depression.
Medical evacuations were done by the federal government and its contractors working through a network of military and other federal agencies and private companies. Evacuation took, on average, 12 to 18 hours and cost tens of thousands of dollars per patient, with more wealthy patients perceived as having greater access to private air evacuation services. It was also noted that undocumented residents faced unique challenges, as their undocumented status created problems in dealing with federal government efforts to track and transfer them during care. In the chaotic time before and during the hurricanes, some patients whose care requirements were immediately recognized as exceeding SRMC capacity were transferred off-island before records could be maintained. Hospital staff had some type of record for 171 air transfers, including transfers that did not originate in the hospital.
Patients with long-term care needs, including patients who were dialysis-dependent, were sent to designated hospitals off-island, with hospitals in Fort Lauderdale and Miami, Florida, and Atlanta, Georgia, taking a large proportion of the transfers. However, concerns were expressed about the fact that evacuees were often separated from their families with no emotional support or medical advocacy.
Review of Emergency Department Charts and Administrative Data
The review of ED charts in the interhurricane and posthurricane periods indicated substantial problems with incomplete data in a number of data categories, particularly for the interhurricane period when paper charts were being used. Vital signs were the highest quality data obtained but still had substantial missing data ranging from 9% (heart rate) to 23% (blood oxygen saturation). Text data for information including chief complaint, home medications, and ED resources utilized, when available, were found to be limited, with most data categories having greater than 50% missing data. Because of the data quality issues with the charts, we did not attempt more formal analysis of the chart review data.
We found administrative data to be more complete, in part because efforts had been made to directly enter data from paper records into the electronic administrative database for insurance purposes. Between June 1, 2017, and December 31, 2017, 10 716 ED visits were recorded at the SRMC: 4804 (44.8%), 957 (8.9%), and 4955 (46.2%) of these visits were eligible for inclusion in the prehurricane, interhurricane, and posthurricane periods, respectively. Results of pre-, inter-, and posthurricane period univariate analyses are shown in Table 1. While overall numbers of patients were comparable, persons seen in the posthurricane period were more likely to be older, male, and self-pay. By contrast with the perception in the structured interviews, an analysis of the reported triage priority level indicated that overall severity of illness was reduced in the posthurricane period (although length of ED visits was increased), with patients more likely to be discharged home. Findings were consistent in multivariable generalized estimating equation models predicting the adjusted odds ratios (AORs) of posthurricane ED attendance (Figure C), showing a significant association with age (AOR = 1.36; 95% confidence interval [CI] = 1.20, 1.56), male gender (AOR = 1.29; 95% CI = 1.15, 1.46), and self-pay payer status (AOR = 1.33; 95% CI = 1.14, 1.54); there was also a significant decrease in case severity.
TABLE 1—
Demographic and Medical Factors of Emergency Department Visits Occurring in Pre-, Inter-, and Posthurricane Periods: Schneider Regional Medical Center, St. Thomas, US Virgin Islands; June 2017–December 2017
| Prehurricane (n = 4804), No. (%) or Mean ±SD | Interhurricane (n = 957), No. (%) or Mean ±SD | Posthurricane (n = 4955), No. (%) or Mean ±SD | Total (n = 10 716), No. (%) or Mean ±SD | P | |
| Gendera,b | < .001 | ||||
| Female | 2160 (55.6) | 457 (48.4) | 1958 (48.6) | 4575 (51.6) | |
| Male | 1728 (44.4) | 487 (51.6) | 2069 (51.4) | 4284 (48.4) | |
| Age, ya,b,c | 40.8 ±23.6 | 46.6 ±23.9 | 43.1 ±24.0 | 42.4 ±23.8 | < .001 |
| Age groupsa,b,c | < .001 | ||||
| < 65 y | 3198 (82.3) | 702 (74.4) | 3197 (79.4) | 7097 (80.1) | |
| ≥ 65 y | 690 (17.7) | 242 (25.6) | 831 (20.6) | 1763 (19.9) | |
| Race/ethnicitya,b,c | < .001 | ||||
| Black | 2925 (75.2) | 715 (75.7) | 3009 (74.7) | 6649 (75.1) | |
| White | 469 (12.1) | 70 (7.4) | 439 (10.9) | 978 (11.0) | |
| Hispanic | 382 (9.8) | 92 (9.8) | 391 (9.7) | 865 (9.8) | |
| Other | 112 (2.9) | 67 (7.1) | 189 (4.7) | 368 (4.2) | |
| Origin of patienta,b,c | < .001 | ||||
| US Virgin Islands | 3596 (92.5) | 916 (97.0) | 3814 (94.7) | 8326 (94.0) | |
| Continental United States | 259 (6.6) | 20 (2.1) | 178 (4.4) | 457 (5.2) | |
| Other | 33 (0.8) | 8 (0.8) | 36 (0.9) | 77 (0.8) | |
| Insurance groupa,b,c | < .001 | ||||
| Medicaid | 1101 (28.3) | 176 (18.6) | 1032 (25.6) | 2309 (26.1) | |
| Medicare | 704 (18.1) | 248 (26.3) | 798 (19.8) | 1750 (19.8) | |
| Private or commercial | 998 (25.7) | 245 (26.0) | 900 (22.3) | 2143 (24.2) | |
| Self-pay | 988 (25.4) | 260 (27.5) | 1194 (29.6) | 2442 (27.6) | |
| Other | 97 (2.5) | 15 (1.6) | 104 (2.6) | 216 (2.4) | |
| Mode of arrivala,c | < .001 | ||||
| Walk-in | 3790 (85.5) | 895 (93.5) | 3911 (86.0) | 8596 (86.5) | |
| Ambulance | 593 (13.4) | 57 (6.0) | 583 (12.8) | 1233 (12.4) | |
| Police vehicle | 52 (1.2) | 5 (0.5) | 56 (1.2) | 113 (1.1) | |
| Triage priority levela | < .001 | ||||
| Critical–urgent (1–3) | 1929 (45.0) | . . . | 921 (26.6) | 2860 (36.9) | |
| Semiurgent (4) | 1966 (45.9) | . . . | 2133 (61.7) | 4101 (52.9) | |
| Nonurgent (5) | 289 (9.1) | . . . | 403 (11.7) | 796 (10.3) | |
| Dispositiona | < .001 | ||||
| Discharge home | 3698 (83.8) | . . . | 2151 (87.3) | 5865 (85.1) | |
| Admitted as inpatient | 534 (12.1) | . . . | 210 (8.5) | 744 (10.8) | |
| Other | 181 (4.1) | . . . | 104 (4.2) | 285 (4.1) | |
| ED length of stay, ha,b,c | 5.36 ±4.95 | 1.78 ±4.97 | 5.80 ±8.04 | 5.30 ±8.00 | < .001 |
Note. ED = emergency department. P values demonstrate comparison of frequency distributions between demographic variables by pre-, inter-, and posthurricane periods. The χ2 test was used for categorical variables; the student t test and analysis of variance test was used for continuous variables. Other insurance group includes veteran insurance, workers’ compensation, and unknown. Other race/ethnicity group includes Arab/Middle Eastern, Asian, American Indian/Native American, Filipino, Pacific Islander, unknown, and other. Hurricane periods: prehurricane (Jun 1, 2017–Sep 5, 2017); interhurricane (Sep 6, 2017–Sep 21, 2017); posthurricane (Sep 22, 2017–Dec 31, 2017).
Significant pairwise comparison (P < .05) between pre- and interhurricane periods.
Significant pairwise comparison (P < .05) between pre- and posthurricane periods.
Significant pairwise comparison (P < .05) between post- and interhurricane periods.
There were 14 ED deaths during the study period, 9 (1.87 per 1000 visits) in the prehurricane period and 5 (1.01 per 1000 visits) in the posthurricane period. Details on cause of death were limited, with 9 (64%) of the 14 ED deaths listed as being attributable to “cardiac arrest, cause unspecified.”
Figure 2 shows the distribution of pre-, inter-, and posthurricane ED visits by ICD-10-CM diagnostic classification. Visits because of injuries showed a significant increase in the interhurricane period, accounting for 66% of ED visits the day after passage of Hurricane Irma, with increases still apparent through the first week to 10 days after the storm. The percentage of patients seen with endocrine, nutritional, and metabolic diseases increased significantly in both the interhurricane and posthurricane periods; 55% of visits in this category were attributable to diabetes or diabetes-related illnesses (ICD-10-CM E10, E11, and E13). As shown in Figure D, patients with diabetes were more likely to be seen in the posthurricane period, to be Black, and to have nonurgent complaints; in the imputed models, they were also more likely to be self-pay. Although there was a slow decline in the rate of ED visits by patients with diabetes, numbers were still elevated 3 months after the second hurricane (Figure F).
As reflected in Figure 2, significant increases in percentage of patients with diseases of the skin and subcutaneous tissue were also seen during and after the hurricane. The percentage of patients with respiratory diseases did not increase during the interhurricane period but did show a significant increase after the hurricane (Figure 2); the highest case number (120 cases, 74% asthma) occurred in November, 2 months after the hurricanes, with a drop back to normal levels by December (Figure F). Patients in these cases tended to be younger Black men, average age 35 years, and on Medicaid (Figure E).
DISCUSSION
In this study, we sought to systematically document the medical impact of 2 back-to-back hurricanes in 2017 in the USVI, a geographically isolated region (i.e., an island). In keeping with the key informant descriptions of the chaotic nature of events—with a loss of electronic records, a switch to paper records, and moving in and out of tents in the parking lot between hurricanes, with limited staff, resources, and supplies—we found that available ED charts had substantial missing data, leading to a decision to rely primarily on the hospital administrative database for our analysis. Although the number of patients seen in the ED did not differ significantly before versus after the hurricane, posthurricane patients were more likely to be older, self-paying, and male, with problems that were less severe, but for which visit time increased. This follows the pattern reported after Hurricane Sandy and other hurricanes, with an increase in older patients, more commonly male, with problems that were less acute, generally reflecting breakdowns in the routine medical infrastructure (e.g., need for prescription refills; issues related to power outages, including oxygen; social issues).
As noted by the key informants, older, chronically ill patients were at particular risk because of the breakdown of family and social support networks and their associated support systems. With a tendency for disaster recovery operations to be dominated by a focus on physical as opposed to social infrastructure, nurturing social support networks are often neglected, and this impedes the resilience of the elderly.21 These social networks are of critical importance in this cultural setting during times of crisis22 with “aging in place” the norm in the St Thomian, Afro-Caribbean culture, as reflected in the fact that there are no rehabilitation, nursing home, or assisted living facilities on the island.
Not unexpectedly, there were significant increases in the number of ED patients with injuries seen during the interhurricane period and, in particular, in the days immediately after passage of Hurricane Irma, which hit the island with Category 5 winds; increases in diseases of the skin and subcutaneous tissue have also been reported in association with hurricanes.21 The increase in the rate at which diabetic patients were seen is almost certainly attributable to the overall disruption of the health care system and, again, has been reported in association with other hurricanes. However, by contrast with studies after Hurricane Sandy, in which service rates returned to prehurricane levels within a matter of weeks,21,23 the increase that we observed persisted (albeit with a slow decline) for the 3 months following the hurricanes, indicative of the slow speed with which health care services returned to “normal” levels of operation. Somewhat unexpectedly, we also saw a significant increase in the rate of adult patients presenting with asthma, with the increase seen not in the interhurricane period but 2 months after passage of the hurricanes. Although we lack data to identify factors responsible for this increase, studies after Hurricane Sandy suggested an association between posthurricane lower respiratory symptoms and exposure to reconstruction material24; increased sensitization to mold allergens, as measured by intradermal skin testing, has also been noted following hurricanes.25
Of greater concern are the data that we do not have. Officially, 5 USVI deaths were associated with Hurricanes Irma and Maria. Extrapolating from the ratio of official deaths to hurricane-related excess deaths in Puerto Rico,5,6 it is possible that there were several hundred hurricane-related excess deaths in the USVI. However, as in Puerto Rico, data on which to base such estimates are limited.
A key problem was the lack of data on off-island transfers. Given the condition of the hospital after Hurricane Irma, virtually everyone with serious or life-threatening conditions was air-evacuated. In keeping with the already noted problems with missing data in the ED charts, there is a paucity of data on such transfers, with a fairly wide range in the estimated number of air evacuations that occurred: the hospital had a line listing with 171 transfers, the territorial health department noted 796 transfers for both St Thomas and St Croix, and a paper from the Atlanta area reported that there were 282 patients (97% from the USVI) air evacuated to Georgia hospitals by the National Disaster Medical System.11 Even less is known about the fate of these patients, with the territorial health department reporting to the territorial legislature in April of 2018 that they had follow-up data on only 536 of the total USVI evacuees, including 49 known deaths.26–28 Only 125 patients were reported to have returned to St Thomas and St John, with more than 500 of the total evacuees said to still be receiving treatment off-island.28 Under these circumstances, it becomes virtually impossible to assess the impact of the hurricanes on these, the most severely ill patients on the island.
The steady rise in sea surface temperatures in the Caribbean presages more storms and, in particular, severe storms that fall into the Category 4 and 5 range.16 Although US government investment in the islands of St Thomas and St John through March 2018 has been substantial, about $530 million from FEMA Public Assistance, much of this funding, about half, has gone into repair of power and water systems.29,30 The FEMA Public Assistance allocation for health care–related agencies totaled $5.4 million; SRMC received a $2.6 million in FEMA Public Assistance grants and $28 million in FEMA Community Disaster Loans.29 With these levels of funding, the island has struggled to rebuild its health care infrastructure, and there has been little opportunity to systematically plan and develop a resilient system that can respond to the inevitable future hurricanes. As part of such planning, there needs to be careful considerations of the most advantageous way to rebuild the SRMC, to optimize the availability of health care personnel and supplies in advance of future hurricanes, and to have procedures in place to maintain electronic recordkeeping, track patients, and monitor outcomes, particularly for air-evacuations from the island. In addition, interviews with key informants highlight the fact that disasters tend to magnify existing weaknesses in health care infrastructure and arrangements. Further hurricanes will come, both to the Virgin Islands and to the US Gulf and Atlantic coasts; it is our hope that their impact can at least be minimized, particularly for highly vulnerable patient groups such as the chronically ill and elderly.
ACKNOWLEDGMENTS
Research Electronic Data Capture data collection was supported by the University of Florida Clinical and Translational Science Institute, funded in part by the National Institutes of Health National Center for Advancing Translational Sciences under award UL1TR001427. Support for the project was provided in part by a grant from the National Institutes of Health (R21MD013762) awarded to J. G. Morris.
We thank the many staff members of the Schneider Regional Medical Center and Margaret Abbott who assisted with this study; the work would not have been possible without their help. We thank Vasubandhu Misra, PhD, Florida Climate Institute, for providing Figure 1.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
HUMAN PARTICIPANT PROTECTION
The study was approved by the University of Florida and University of Maryland institutional review boards under study numbers IRB201801543 and HP-00079561.
REFERENCES
- 1.National Oceanic and Atmospheric Administration, National Weather Service. National Hurricane Center tropical cyclone report: Hurricane Irma. 2017. Available at: https://www.nhc.noaa.gov/data/tcr/AL112017_Irma.pdf. Accessed February 6, 2019.
- 2.National Oceanic and Atmospheric Administration, National Weather Service. National Hurricane Center tropical cyclone report: Hurricane Maria. 2017. Available at: https://www.nhc.noaa.gov/data/tcr/AL152017_Maria.pdf. Accessed February 6, 2019.
- 3.Shultz JM, Kossin JP, Shepherd JM et al. Risks, health consequences, and response challenges for small-island-based populations: observations from the 2017 Atlantic hurricane season. Disaster Med Public Health Prep. 2019;13(1):5–17. doi: 10.1017/dmp.2018.28. [DOI] [PubMed] [Google Scholar]
- 4.Zorrilla CD. The view from Puerto Rico—Hurricane Maria and its aftermath. N Engl J Med. 2017;377(19):1801–1803. doi: 10.1056/NEJMp1713196. [DOI] [PubMed] [Google Scholar]
- 5.Santos-Lozada AR, Howard JT. Use of death counts from vital statistics to calculate excess deaths in Puerto Rico following Hurricane Maria [erratum JAMA. 2019;321(19):1939]. JAMA. 2018;320(14):1491–1493. [DOI] [PubMed]
- 6.Kishore N, Marqués D, Mahmud A et al. Mortality in Puerto Rico after Hurricane Maria. N Engl J Med. 2018;379(2):162–170. doi: 10.1056/NEJMsa1803972. [DOI] [PubMed] [Google Scholar]
- 7.US Census Bureau. US Census Bureau, 2010 Census, US Virgin Islands. Population, housing units, land area, and density. October 2013. Available at: https://www.census.gov/population/www/cen2010/cph-t/t-8tables/table4a.pdf. Accessed January 31, 2018.
- 8.Smith K, Janine B. Full interview with Tina Comissiong. WRAL-TV. September 18, 2018. Available at: https://www.wral.com/weather/hurricanes/video/16957725. Accessed February 1, 2019.
- 9.O’Connor B. Hospital expands capacity, with federal help. The Virgin Islands Daily News. September 13, 2017. Available at: http://www.virginislandsdailynews.com/breaking/hospital-expands-capacity-with-federal-help/article_41a0ae0a-983e-11e7-baf8-dfa420029c68.html. Accessed November 30, 2018.
- 10.Carlson S. Medical evacuees still being transported out of the territory. The Virgin Islands Daily News. February 21, 2018. Available at: http://www.virginislandsdailynews.com/news/medical-evacuees-still-being-transported-out-of-the-territory/article_4d9e5cd4-f790-5f0d-ac88-c8e91394231e.html. Accessed December 14, 2018.
- 11.Vora NM, Grober A, Goodwin BP et al. Challenges of service coordination for evacuees of Hurricane Maria through the National Disaster Medical System. J Emerg Manag. 2018;16(3):203–206. doi: 10.5055/jem.2018.0369. [DOI] [PubMed] [Google Scholar]
- 12.Carlson S. St. Croix’s Luis Hospital, Harwood complex hard-hit by Maria. The Virgin Islands Daily News. September 21, 2017. Available at: http://www.virginislandsdailynews.com/news/st-croix-s-luis-hospital-harwood-complex-hard-hit-by/article_e7840dfa-a591-5f3d-a4a2-368e6cb66253.html. Accessed February 19, 2019.
- 13.Federal Emergency Management Agency. Mitigation Assessment Team report: Hurricanes Irma and Maria in the US Virgin Islands. 2018. 202. Available at: https://www.fema.gov/media-library/assets/documents/170486. Accessed September 18, 2019.
- 14.Federal Emergency Management Agency. Six months after two Category 5 hurricanes struck, the US Virgin Islands is recovering. 2018. Available at: https://www.fema.gov/news-release/2018/03/02/six-months-after-two-category-5-hurricanes-struck-us-virgin-islands. Accessed February 18, 2019.
- 15.Gilbert E. Even as death toll of medical evacuees rises, attorney general says official number of hurricane-related deaths will remain at 5. The Virgin Islands Consortium. May 31, 2018. Available at: https://viconsortium.com/featured/hurricane-related-deaths-usvi. Accessed December 14, 2018.
- 16.Knutson TR, McBride JL, Chan J et al. Tropical cyclones and climate change. Nat Geosci. 2010;3(3):157–163. [Google Scholar]
- 17.International Classification of Diseases, Tenth Revision, Clinical Modification. Hyattsville, MD: National Center for Health Statistics; 2000. Available at: https://www.cdc.gov/nchs/icd/icd10cm.htm. Accessed September 23, 2019. [Google Scholar]
- 18.Zeger SL, Liang K-Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 19.Zeger SL, Liang K-Y, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44(4):1049–1060. [PubMed] [Google Scholar]
- 20.Enders CK. Multiple imputation as a flexible tool for missing data handling in clinical research. Behav Res Ther. 2017;98:4–18. doi: 10.1016/j.brat.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 21.Saulnier DD, Brolin Ribacke K, von Schreeb J. No calm after the storm: a systematic review of human health following flood and storm disasters. Prehosp Disaster Med. 2017;32(5):568–579. doi: 10.1017/S1049023X17006574. [DOI] [PubMed] [Google Scholar]
- 22.Koffman J, Morgan M, Edmonds P, Speck P, Higginson IJ. “The greatest thing in the world is the family”: the meaning of social support among Black Caribbean and White British patients living with advanced cancer. Psychooncology. 2012;21(4):400–408. doi: 10.1002/pon.1912. [DOI] [PubMed] [Google Scholar]
- 23.Malik S, Lee DC, Doran KM et al. Vulnerability of older adults in disasters: emergency department utilization by geriatric patients after Hurricane Sandy. Disaster Med Public Health Prep. 2018;12(2):184–193. doi: 10.1017/dmp.2017.44. [DOI] [PubMed] [Google Scholar]
- 24.Gargano LM, Locke S, Jordan HT, Brackbill RM. Lower respiratory symptoms associated with environmental and reconstruction exposures after Hurricane Sandy. Disaster Med Public Health Prep. 2018;12(6):697–702. doi: 10.1017/dmp.2017.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saporta D, Hurst D. Increased sensitization to mold allergens measured by intradermal skin testing following hurricanes. J Environ Public Health. 2017;2017:2793820. doi: 10.1155/2017/2793820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Legislature of the United States Virgin Islands. Bill to provide a registry for the elderly moves forward and Senators receive update on medical evacuations—Legislature of the Virgin Islands. 2018. Available at: http://www.legvi.org/bill-to-provide-a-registry-for-the-elderly-moves-forward-senators-receive-update-on-medical-evacuations. Accessed February 5, 2019.
- 27.Shimel J. Senate hears painful, incomplete picture on medical evacuees. St John Source. April 11, 2018. Available at: https://stjohnsource.com/2018/04/11/senate-hears-painful-incomplete-picture-on-medical-evacuees. Accessed February 5, 2019.
- 28.Carlson S. Medical evacuees struggled to survive after hurricanes. The Virgin Islands Daily News. April 11, 2018. Available at: http://www.virginislandsdailynews.com/news/medical-evacuees-struggled-to-survive-after-hurricanes/article_a5a221a1-c42a-536f-a1b2-629cd9d1a700.html. Accessed February 18, 2019.
- 29.Virgin Islands Public Finance Authority. USVI Hurricane Recovery. 2019. Available at: http://www.usvipfa.com/hurricanehome.html. Accessed February 13, 2019.
- 30.Federal Emergency Management Agency. Federal funding for US Virgin Islands tops $1 billion. 2018. Available at: https://www.fema.gov/news-release/2018/03/20/federal-funding-us-virgin-islands-tops-1-billion. Accessed February 5, 2019.