Abstract
Background and objective
Pneumothorax (PNX) detection is of the utmost clinical relevance because it may quickly progress to cause hemodynamic instability as a consequence of invasive ventilation. Radiography is characterized by a low sensitivity to detect this disease; in recent years, chest ultrasound (US) has gained increased visibility in the diagnosis of acute respiratory emergencies including PNX. The aim of this retrospective study was to evaluate the clinical impact of extended focused assessment with sonography in trauma (E-FAST) during the past 6 years of experience with this technique in our Level I trauma center.
Methods
Between January 2013 and December 2018, we performed a retrospective case-series study including 3320 consecutive patients admitted to the emergency department of our hospital because of major trauma. Extended-US was always performed and reported immediately after FAST during primary survey and before multidetector computed tomography (MDCT) scans. The presence of PNX was determined using the well-known accepted US criteria. US findings were compared with computed tomography (CT) findings, the reference standard for PNX detection.
Results
Of the 6640 lungs observed with E-FAST, there were 1244 PNX cases, while 1328 PNX cases were detected either on the basis of MDCT or on the basis of the presence of air flush during the thoracic decompression in the emergency room. Among the 84 false negatives, 12 patients had subcutaneous emphysema, 38 had a body mass index higher than 27, 6 had a thoracic wall hematoma, and 4 had chest penetrating trauma. There were 10 false positives in the diagnosis of PNX at US examination, with mild extension and not clinically significant. The overall sensitivity of E-FAST for PNX detection was 93.6% (1244/1328), the specificity of E-FAST was 99.8% (5312/5322), the negative predictive value (NPV) was 98.4% (5312/5396), and the positive predictive value (PPV) was 99.2% (1328/1338).
Conclusion
Our results demonstrate that bedside thoracic US is characterized by a very good accuracy in the diagnostic work-up of major trauma patients, even in difficult conditions, allowing rapid diagnosis of PNX.
Advances in knowledge
The novelty of this research lies in the possibility of diagnosing potential life-threatening conditions in a very short time by means of US, thus proposing a revision of the Advanced Trauma Life Support (ATLS) guidelines in order to incorporate it in the work-up of high-energy injured patients.
Keywords: Thoracic ultrasound, Pneumothorax, Major trauma, Extended-FAST, Advanced trauma life support
Background
Misdiagnosed pneumothorax (PNX) can quickly become life-threatening, so PNX requires early diagnosis and urgent treatment [1]. The literature has demonstrated that supine chest radiograph (CR) is a low-sensitive examination (about 50–60%) for detecting this disease [2–10], although until now the Advanced Trauma Life Support (ATLS) procedure considered it a basic examination for first-line pneumothorax diagnosis during major trauma primary survey [11]. A pneumothorax recognized on a computed tomography (CT) scan, but not seen on a previous supine CR, is defined as an “occult pneumothorax” (OP); it accounts for 52–63% of all traumatic pneumothoraces. Although CT is the gold standard diagnostic test for the identification of pneumothorax, it is limited by radiation exposure and by the difficulty of transporting unstable patients to the CT scan room [12–16].
For more than a decade, chest ultrasound (US) has found its way into the emergency and critical care setting, and has now become a feasible tool for the diagnosis of acute respiratory emergencies, including, but not limited to, PNX [17]. In a meta-analysis by Ding et al. [5], who compared the use of anteroposterior chest radiography with thoracic ultrasonography for the diagnosis of pneumothorax, pooled sensitivity and specificity were 88% and 99%, respectively, for ultrasonography and 52% and 100%, respectively, for CR. These results are encouraging because they underline the capability of US to recognize even the smallest pneumothoraces, hence avoiding serious potential consequences such as tension pneumothorax, especially in mechanically ventilated patients.
In patients with major trauma, after the initial focused assessment with sonography in trauma (FAST) survey, the US examination is extended to the thorax to rule out hemothorax and pneumothorax; this “extended-to-thorax” examination is called extended-FAST (E-FAST).
In a trauma setting, the E-FAST examination is usually performed in hypotensive and hemodynamically unstable patients because it helps determine whether immediate surgery is needed before the patient undergoes a multidetector computed tomography (MDCT) evaluation. Taking into consideration, however, the time interval from arrival to performing the MDCT, it would be advisable to perform the evaluation (during primary survey time) in order to avoid unexpected findings such as OP.
The aim of this retrospective study was to evaluate the clinical impact of a new imaging approach in a trauma-dedicated logistical context (shock room, CT room, operating room strictly closed, emergency radiologist, and a trauma team for 24 h a day, 7 days a week), extended only to E-FAST, during primary survey and with whole-body multidetector computed tomography (WB-MDCT) as the secondary survey, for the past 3 years of experience in our Level I trauma center.
Methods
Study protocol
We performed a retrospective case-series study that included 3320 consecutive patients admitted to the emergency department of our hospital (Level I trauma center) between January 2013 and December 2018 because of major trauma (Injury Severity Scale, or ISS, ≥ 15). Patients were eligible for inclusion in the present study if they had undergone chest US as part of the E-FAST examination before the WB-MDCT examination, the OR (operating room) for damage control, and the placement of a thoracostomy tube. All the E-FAST examinations were performed by the attending trauma radiologists (with at least 20 years of experience in clinical US and 5 years of experience in thoracic US and MDCT examinations) both at bedside and in the emergency room; the examinations were recorded on video. Extended (to the thorax)-US was always performed and reported immediately after FAST during primary survey (within the first 5 min after the arrival of the patient) and before the WB-MDCT scans. Due to the need to immobilize the patient, the thoracic investigation included an examination of the anterior and lateral wall only, not the posterior one.
The presence of pneumothorax was determined using the well-known accepted US criteria (absence of lung sliding and lung pulse, loss of B lines, and identification of the lung point).
The WB-MDCT images were read by a staff radiologist without knowledge of the US findings. For every patient, the arrival time in the emergency department, time of E-FAST, and time of MDCT were recorded. The final US reports and images were reviewed by two authors of this paper and by independent lecturers and compared with MDCT images for verification; all the images and reports have been collected by our RIS/PACS system.
Technical equipment
In our institution, E-FAST is performed at the bedside, inside the shock room, with the patient in the supine position, by using a US imaging unit (Esaote MyLab75, Italy) equipped with a 7.5–10 MHz linear probe. The linear high -frequency probe (7.5–10 MHz) is suitable for the visualization of the pleural line [18–20]; the convex probes are meant to evaluate the peritoneal cavity and the pericardium, and the lateral hemithoraces are used to detect hemothorax. WB-MDCT is performed using a 16-channel CT scanning unit (CT LightSpeed 16, GE Medical Systems, Milwaukee, Wis.); intravenous contrast material (Visipaque 320 mg/ml, GE Medical Systems, Milwaukee, Wis.) is always employed for the evaluation of whole-body trauma. MDCT sections were obtained with contiguous 2 mm axial sections from the apicothorax to the symphysis pubis at a pitch of 1.5; mediastinal and lung windows were then recorded on the PACS system.
Sonographic semeiology
Sonographic evaluation for pneumothorax begins from the anteroinferior chest wall and then moves on to the lateral chest. The patients were examined in the supine position, placing the probe at the second to fourth intercostal spaces anteriorly and at the sixth to eighth spaces in the mid-axillary line (Fig. 1). The presence of pneumothorax was recognized using the well-known US criteria: the disappearance of lung sliding and the loss of the comet-tail artifact at the pleural interface [18–23].The lung sliding represents the twinkling movement visible at the pleural line, corresponding to the contact of the visceral pleura with the parietal pleura. In the presence of a pneumothorax, the air between the two pleural layers causes abolition of the lung sliding, and the pleural line appears static. The B lines, which appear as comet-tail artifacts, arise from the pleural line, spread up without fading to the edge of the screen, and are synchronous with the respiratory movements. They become visible when a marked difference in acoustic impedance exists between an object and its surroundings. US detection of the comet-tail artifact allows pneumothorax to be ruled out.
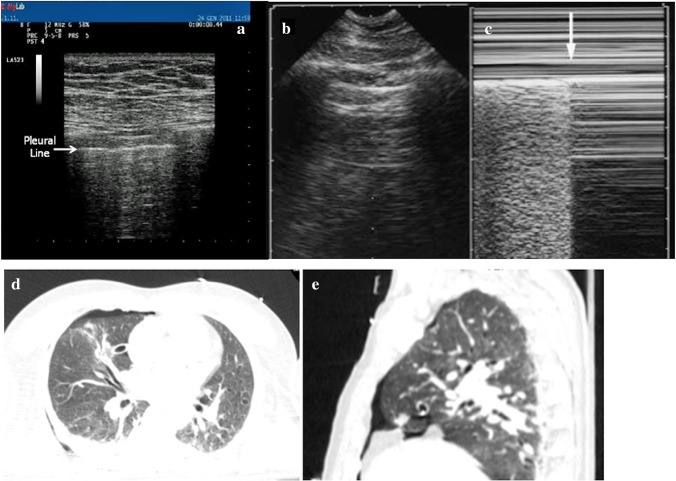
Fig. 1.
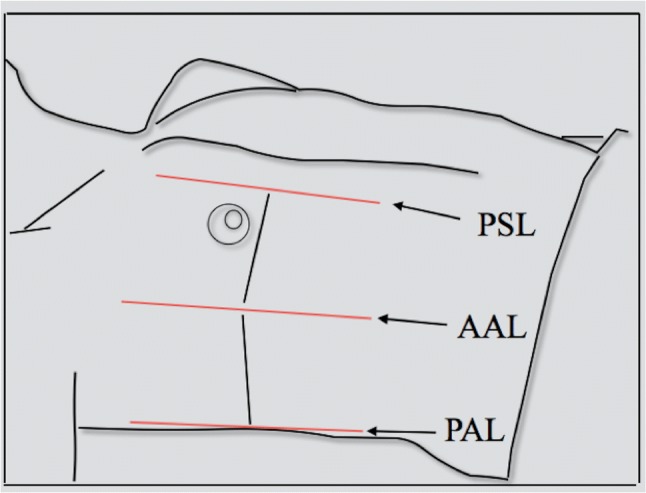
Pneumothorax extension, evaluation based on lung point localization (modified from Volpicelli et al., Intensive Care 2010). a Near the parasternal line: mild, b until the anterior axillar line: moderate, c until the posterior axillar line: massive
When these two signs are present in the anteroinferior chest area, one should check the lateral inferior chest wall for the lung point. This sign is defined as the border between aerated lung and pneumothorax; it confirms the diagnosis of pneumothorax with a specificity of 100% [21], and its location provides information about the extent and severity of pneumothorax (Figs. 2, 3).
Fig. 2.
Thoracic US and E-FAST in a male patient who sustained a fall. a Absence of pleural sliding in the right lung and B lines: lung point identified on AAL, US diagnosis of moderate pneumothorax in an unstable patient, and immediate pleural tube drainage with the escape of intrapleural air in the emergency room. b, c M-mode of the same case. In c, we can see the inhomogeneous “seashore” sign, a typical depiction of pleural sliding; on the right side of the image, the typical homogeneous depiction of the absence of pleural sliding. US diagnosis and documentation of moderate pneumothorax. CT scan on axial (d) and sagittal reconstruction (e) confirms the diagnosis of moderate right pneumothorax
Fig. 3.
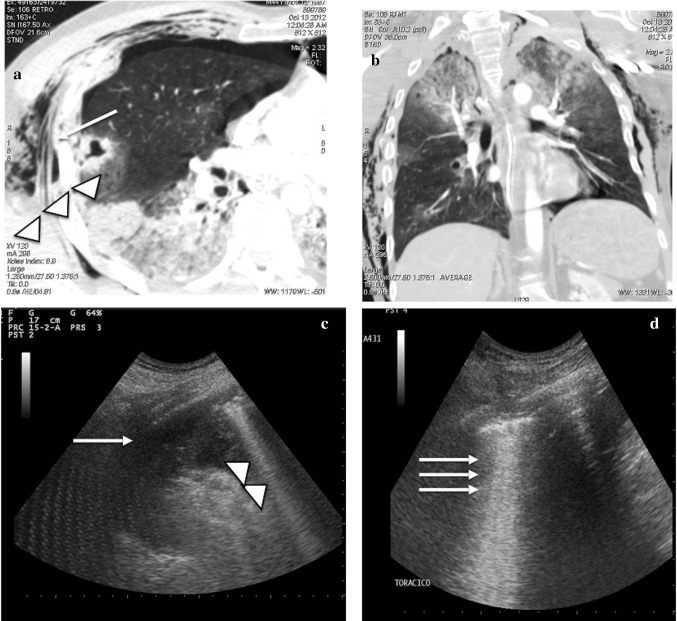
CT scan and thoracic US and E-FAST in a male patient who sustained a severe fall trauma. a The CT scan on the axial plane shows a small pneumothorax on the anterior chest wall associated with a parenchymal laceration (arrow) and wide areas of lung contusions in the right lower lobe (head arrow). b The CT scan on the coronal plane clearly demonstrates the contusions in both the lungs. c Lung US performed on the right side depicts a wide area of parenchymal consolidation (arrow) along with thick B lines and expression of contusions (head arrows). d Lung US on the left lung shows several B lines (arrows) and expression of parenchymal contusions
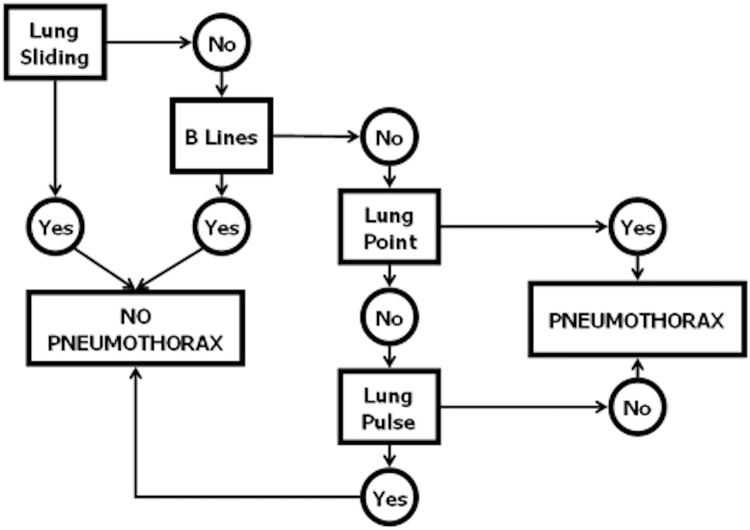
The diagnostic algorithm used to define the sonographic diagnosis of pneumothorax is shown in Fig. 4.
Fig. 4.
The diagnostic algorithm used to define the sonographic diagnosis of pneumothorax
(modified from Volpicelli et al., Intensive Care 2010)
Statistical analysis
Estimates of sensitivity, specificity, positive predictive value, negative predictive value, and overall accuracy were calculated for E-FAST using MDCT as the reference standard for pneumothorax detection in all patients. Ninety-five percent confidence intervals (CIs) based on a binomial distribution were calculated for all the estimates using a statistical software program (SPSS 10).
Furthermore, the same values were calculated separately for each year of evaluation to take into account an extended learning curve. In those patients in which US showed massive pneumothorax and in which a chest drainage was placed before MDCT, we considered the escape or aspiration of intrapleural air at the time of drainage in the emergency room (as documented in case history), a criterion that is suggestive of the presence of pneumothorax. The right and left lungs were considered separately for each patient (Fig. 5).
Fig. 5.
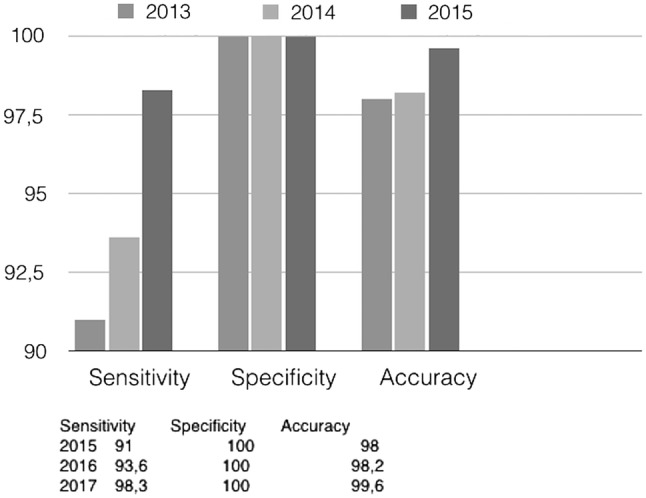
Sensitivity, specificity, accuracy during first three years of experience
Results
Between January 2013 and December 2018, 3320 consecutive major traumatic patients (ISS ≥ 15) were admitted to our emergency department (1844 men and 1476 women, with a median age of 41 years and an age range of 18–81 years). Of these patients, 3088 suffered a blunt trauma, and 232 a penetrating trauma; these patients underwent an E-FAST at admission in the emergency room (during primary survey, from 0 to 5 min after the patient’s arrival) for the detection of pneumothorax, hemothorax, hemopericardium, and hemoperitoneum. E-FAST, followed by WB-MDCT, was performed in all patients. Chest X-ray (XR) and pelvis XR were performed only in unstable patients upon arrival in the OR; cervical spine XR was not performed at all. WB-MDCT is our choice of secondary survey; a three-phase or two-phase technique was decided upon case by case based on the specific findings. The technical advantages of performing a WB-MDCT are summarized in Table 1.
Table 1.
Diagnostic performance values of Extended (to thorax) ultrasound
| Parameters | Thoracic ultrasound (%) |
|---|---|
| Overall sensitivity (%) | 93.6 |
| Specificity (%) | 99.8 |
| FP rate (%) | 0.7 |
| FN rate (%) | 6.3 |
| PPV (%) | 99.2 |
| NPV (%) | 98.4 |
| Overall accuracy (%) | 98.6 |
These patients represent our study population (a total of 6640 hemithoraces). The results about the diagnostic performance of thoracic US are summarized in Table 1.
The time interval between US and WB-MDCT ranged from 10 to 75 min (median 36 min), depending on the clinical conditions at admission and the necessity for urgent maneuvers. Out of 6640 lungs in 3320 patients, E-FAST detected 1244 pneumothoraces, while 1328 pneumothoraces were detected either on the basis of MDCT or on the basis of the presence of air flush during thoracic decompression in the emergency room. Of these, 236 pneumothoraces were bilateral, and 1092 were monolateral. US missed 84 out of 1328 cases (6.3%) of pneumothorax; 54 out of 84 (64%) of them were mild (thickness less than 5 mm at the MDCT scan), 30 out of 84 (36%) were moderate (extension at the basal anterior region; thickness less than 2 cm), and none of them were massive. Of these, 84 cases were false negative, 12 patients had subcutaneous emphysema, 38 had a body mass index (BMI) higher than 27, 3 had a thoracic wall hematoma, and 4 had chest penetrating trauma. There were 10 (out of 1328) false positives (all emphysematous bullae) in the diagnosis of pneumothorax at US examination, with mild extension; they were not clinically significant and not treated.
For the thoracic US results, all false negatives occurred during the initial five E-FAST examinations performed by each radiologist; likewise, there is no evidence for an association with false positives, since all occurred in emphysematous patients. Consequently, the overall sensitivity of E-FAST for pneumothorax detection was 93.6% (1244/1328), the specificity of E-FAST was 99.8% (5312/5322), the negative predictive value (NPV) was 98.4% (5312/5396), and the positive predictive value (PPV) was 99.2% (1328/1338). Over the past 3 years of experience in our Level I trauma center, the overall diagnostic accuracy of this diagnostic tool for pneumothorax in major trauma in the emergency room was 98.6%. The 95% CIs for sensitivity and specificity of transthoracic sonography were 84–100% and 90.5–100%, respectively.
The median time to recognize a pneumothorax diagnosis by means of E-FAST was 3 min (1–5 min). E-FAST does not prevent each step of the primary survey, but it has become strictly connected to it. Furthermore, it is repeatable every time it is needed, if hemodynamic conditions change (Table 2).
Table 2.
Advantages to perform a whole-body CT scan
| MDCT as the gold standard in the assessment of major trauma |
| 1. Whole body evaluation |
|
Hemoperitoneum, hemoretroperitoneum Active bleeding Grading of parenchymal lesions Vascular injuries Musculoskeletal injuries |
| 2. Rapid acquisition |
| 3. Reconstructions: MIP, MPR, VR. |
| 4. Can drive the therapeutic management |
| 4. Reproducible: |
|
Not operator dependent Less prone to motion artifacts |
Discussion
Since the late 1990s, MDCT has been considered the imaging modality of choice in patients who sustained major trauma [24–27]. Nowadays, there is a trend toward an increasing involvement of US, performed in association with MDCT, for the immediate evaluation of these patients, especially in Europe [28–38].
One of the most frequent life-threatening conditions encountered in this kind of trauma is pneumo-thorax, whose detection is of the utmost clinical relevance because it may quickly progress to cause hemodynamic instability as a consequence of invasive ventilation.
Bedsides, radiography has a notorious low accuracy in detecting pneumothorax, with values of sensitivities ranging between 50 and 90% [39–46]. The recognition of specific dynamic sonographic artifacts at the pleural line led to bedside US sensitivity values that are quite similar to the sensitivity values of CT scans [47]. The encouraging results coming from several studies performed on this topic, along with the logistic advantages of performing thoracic US at bedside patients, led ultrasonography to be incorporated into the ATLS guidelines as FAST [11].
A systematic review performed by Alrajhi et al. [48], involving 1047 patients, reported a sensitivity of 90.0% (95% CI 86.5–93.9) and a specificity of 98.2% (95% CI 97.0–99.0) for US. The same values for chest XR were, respectively, 50.2% (95% CI 43.5–57.0) and 99.4% (95% CI 98.3–99.8). A study reported by Soldati et al. [2] showed that only 13 out of 25 pneumothoraces were revealed by chest radiography (sensitivity: 52%; specificity: 100%), whereas 23 out of 25 pneumothoraces (92%) were identified by US with one false-positive result (sensitivity: 92%; specificity: 99.4%). They also reported that US had high sensitivity in the diagnosis of OP. Similarly, in a study by Nandipati et al., US and CT results were similar in 95% of the cases [49].
In our study, we investigated the diagnostic performance of thoracic US examination to rapidly detect pneumothorax during the initial evaluation of majorly injured patients in the emergency room.
In the emergency department of our hospital, patients suspected of having PNX on physical examination undergo immediate tube or needle thoracostomy without awaiting imaging studies [16]; those patients were excluded from the present study. In those patients who do not require immediate invasive interventions, a bedside US examination is performed immediately, during the primary survey, by a trauma radiologist. The patient undergoes a WB-MDCT examination immediately after the E-FAST examination if hemoperitoneum is absent; otherwise, if there is suspicion of solid organ injury that requires urgent surgical exploration, the CT examination takes place immediately after the laparotomy for damage control.
In our study, we evaluated the accuracy of E-FAST in the detection of pneumothorax using MDCT as the reference standard examination. In those patients in which US recognized a massive pneumothorax and in which a chest drainage was placed before CT, we used the air flush at the time of chest drainage as a criterion to confirm the US diagnosis.
According to our results, E-FAST proved to be a rapid and useful test for discovering pneumothorax with an overall diagnostic accuracy of 98.6%. There were 10 false-positive cases in the diagnosis of pneumothorax at US examination, caused by emphysematous bullae. In our study, 12 cases of significant subcutaneous emphysema caused false determination of the presence of pneumothorax. The most frequent association with false negative (45%) was the association with high BMI. In our series, US missed 84 out of 1328 cases of pneumothorax, 54 of which were not immediate life-threatening with a thickness of less than 5 mm at the MDCT scan. Pneumothorax was bilateral in 236 of our cases, but this fact did not affect the sensitivity of the E-FAST.
Several limitations of our study should, however, be taken into account. First, this is a retrospective study, meaning that US examinations were performed by different operators with different skills. All the operators of the radiology staff performed thoracic US under the most difficult conditions, including the restricted time interval required to carry out the examination, poor logistic organization (performing US at bedside and during the execution of other diagnostic maneuvers), and noncollaborative patients, but nevertheless the diagnostic performance of E-FAST was high.
Second, as this was a retrospective study, we could not evaluate the accuracy of US in predicting the extension of pneumothorax in comparison with MDCT. The extension of PNX allows semiquantification of its volume, accurately discriminating between mild, moderate, and massive cases. This information can drive treatment decision-making in most cases of PNX, even if the final decision depends on the clinical condition of the patient: for example, in mechanically ventilated patients, even a moderate PNX requires the insertion of a chest tube.
Our mortality rate within 24 h for hypertensive pneumothorax (0%) and our mortality for every traumatic lesion within 28 days (14% at first neurologic lesions) seem to demonstrate that this proposal of a new radiological ATLS approach (E-FAST + WB-MDCT) has good results, reduces time (E-FAST within 5 min; WB-MDCT within 40 min), and decreases the many diagnostic steps between clinical suspicion and definitive proof of injuries that require immediate therapeutic maneuvers. Beyond pneumothorax diagnosis, further studies will need to be conducted to analyze the clinical impact for every single traumatic lesion.
Conclusions
According to the ATLS recommendations, the following imaging studies are systematically performed at the resuscitation area for the initial evaluation of any trauma patients involved in a high-energy accident or with loss of consciousness [11]:
An anteroposterior (AP) chest radiograph
An AP pelvic radiograph
A lateral cervical spine radiograph
An abdominal sonograph
As soon as the vital functions have been stabilized, the patient is brought in the CT facility to undergo a total body CT examination.
Conventional radiograph examination of the limbs is usually performed immediately after CT, provided that it does not delay a life-saving procedure.
This approach can be considered anachronistic by now, because it dates back to an era when thoracic US was not as widespread and standardized as it is now [50].
Our results, in agreement with some previous studies [51], demonstrate that bedside thoracic US is characterized by very good accuracy in the diagnostic work-up of major trauma patients, even in difficult conditions, allowing rapid diagnosis of pneumothorax.
In our trauma room, thoracic US is always used during FAST in which time-saving is very important to guarantee immediate treatment. A protocol limited to the anterolateral chest wall is sufficient to definitely rule out pneumothorax because our MDCT analysis (with patients lying in the supine position) of OP showed that the anterior area was involved in almost all the cases.
In the perspective of a new radiological ATLS approach, E-FAST during primary survey, together with WB-MDCT as secondary survey, seems to demonstrate high enough accuracy to avoid pneumothorax-related death; the CT scanner should be placed very close to or at best in the trauma room. Further studies will be needed to strengthen this approach.
Author contributions
SI and VM performed the data interpretation and the critical revision. CL Piccolo contributed to the writing of the study, the study design data analysis and data interpretation. MT and CAA-C contributed to literature search and critical revision.
Funding
No funding was provided.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with participants or animals performed by any of the authors.
Informed consent
No patient information is included in this study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kirkpatrick AW, Sirois M, Laupland KB, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST) J Trauma. 2004;57:288–295. doi: 10.1097/01.TA.0000133565.88871.E4. [DOI] [PubMed] [Google Scholar]
- 2.Soldati G, Testa A, Sher S, et al. Occult traumatic pneumothorax: diagnostic accuracy of lung ultrasonography in the emergency department. Chest. 2008;133:204–211. doi: 10.1378/chest.07-1595. [DOI] [PubMed] [Google Scholar]
- 3.Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of Pneumothorax after blunt trauma. Acad Emerg Med. 2009;17(1):11–17. doi: 10.1111/j.1553-2712.2009.00628.x. [DOI] [PubMed] [Google Scholar]
- 4.Scalea TM, Rodriguez A, Chiu WC, et al. Focused assessment with sonography for trauma (FAST): results from an international consensus conference. J Trauma. 1999;46:466–472. doi: 10.1097/00005373-199903000-00022. [DOI] [PubMed] [Google Scholar]
- 5.Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest. 2011;140:859–866. doi: 10.1378/chest.10-2946. [DOI] [PubMed] [Google Scholar]
- 6.Saucier S, Motyka C, Killu K. Ultrasonography versus chest radiography after chest tube removal for the detection of pneumothorax. AACN Adv Crit Care. 2010;21(1):34–38. doi: 10.1097/nci.0b013e3181c8013a. [DOI] [PubMed] [Google Scholar]
- 7.Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005;12(9):844–849. doi: 10.1197/j.aem.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 8.Holmes JF, Brant WE, Bogren HG, London KL, Kuppermann N. Prevalence and importance of pneumothoraces visualized on abdominal computed tomographic scan in children with blunt trauma. J Trauma. 2001;50(3):516–520. doi: 10.1097/00005373-200103000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Xirouchaki N, Magkanas E, Vaporidi K, et al. Lung ultrasound in critically ill patients: comparison with bedside chest radiography. Intensive Care Med. 2011;37(9):1488–1493. doi: 10.1007/s00134-011-2317-y. [DOI] [PubMed] [Google Scholar]
- 10.Soccorsa S. Bedside US imaging in multiple trauma patients. Part 1: US findings and techniques. J Ultrasound. 2013;16(4):147–159. doi: 10.1007/s40477-013-0047-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soar J, Nolan JP, Bottiger BW, et al. European resuscitation council guidelines for resuscitation 2015: Section 3. Adult advanced life support. Resuscitation. 2015;95:100–147. doi: 10.1016/j.resuscitation.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 12.Korner M, Krotz MM, Degenhart C, Pfeifer KJ, Reiser MF, Linsenmaier U. Current role of emergency US in patients with major trauma. Radiographics. 2008;28:225–242. doi: 10.1148/rg.281075047. [DOI] [PubMed] [Google Scholar]
- 13.Hassan M, Rizk R, Essam M, Abouelnour A. Validation of equations for pleural effusion volume estimation by ultrasonography. J Ultrasound. 2017;20(4):267–271. doi: 10.1007/s40477-017-0266-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lichtenstein DA, Menu Y, et al. A bedside ultrasound sign ruling-out pneumothorax in the critically ill. Lung sliding. Chest. 1995;108:1345–1348. doi: 10.1378/chest.108.5.1345. [DOI] [PubMed] [Google Scholar]
- 15.Rowan KR, Kirkpatrick AW, Liu D, Forkheim K, Mayo JR, Nicolaou S. Traumatic pneumothorax detection with thoracic US: correlation with chest radiography and CT—initial experience. Radiology. 2002;225(1):210–214. doi: 10.1148/radiol.2251011102. [DOI] [PubMed] [Google Scholar]
- 16.Zhang M, Liu ZH, Yang JX, Gan JX, Xu SW, You XD, Jiang GY. Rapid detection of pneumothorax by ultrasonography in patients with multiple trauma. Crit Care. 2006;10:R112. doi: 10.1186/cc5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ianniello S, Piccolo CL, Buquicchio GL, Trinci M, Miele V. First-line diagnosis of paediatric pneumonia in emergency: lung ultrasound (LUS) in addition to chest-X-ray (CXR) and its role in follow-up. Br J Radiol. 2016;89(1061):20150998. doi: 10.1259/bjr.20150998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Volpicelli G. Sonographic diagnosis of pneumothorax. Intensive Care Med. 2011;37(2):224–232. doi: 10.1007/s00134-010-2079-y. [DOI] [PubMed] [Google Scholar]
- 19.Garofalo G, Busso M, Perotto F, De Pascale A, Fava C. Ultrasound diagnosis of pneumothorax. Radiol Med. 2006;111:516–525. doi: 10.1007/s11547-006-0047-y. [DOI] [PubMed] [Google Scholar]
- 20.Lichtenstein DA, Meziere G, Biderman P, Gepner A, Barrè O. The comet tail artifact. An ultrasound sign of alveolar-interstizial syndrome. Am J Respir Crit Care Med. 1997;156:1640–1646. doi: 10.1164/ajrccm.156.5.96-07096. [DOI] [PubMed] [Google Scholar]
- 21.Lichtenstein DA, Meziere G, Biderman P, Gepner A. The lung point: an ultrasound sign specific to pneumothorax. Intensive Care Med. 2000;26:1434–1440. doi: 10.1007/s001340000627. [DOI] [PubMed] [Google Scholar]
- 22.Lichtenstein DA. Ultrasound in the management of thoracic disease. Crit Care Med. 2007;35:S250–S261. doi: 10.1097/01.CCM.0000260674.60761.85. [DOI] [PubMed] [Google Scholar]
- 23.Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:577–591. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 24.Miele V, Andreoli C, Grassi R. The management of emergency radiology: key facts. Eur J Radiol. 2006;59:311–314. doi: 10.1016/j.ejrad.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 25.Anderson SW, Lucey BC, Varghese JC, Soto JA. Sixtyfour multi-detector row computed tomography in multitrauma patient imaging: early experience. Curr Probl Diagn Radiol. 2006;35:188–198. doi: 10.1067/j.cpradiol.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 26.Lomoschitz FM, Eisenhuber E, Linnau KF, Peloschek P, Schoder M, Bankier AA. Imaging of chest trauma: radiological patterns of injury and diagnostic algorithms. Eur J Radiol. 2003;48:61–70. doi: 10.1016/S0720-048X(03)00202-X. [DOI] [PubMed] [Google Scholar]
- 27.Hammer S, Kroft LJ, Hidalgo AL, Leta R, de Roos A. Chest CT examination in patients presenting with acute chest pain: a pictorial review. Insights Imaging. 2015;6:719–728. doi: 10.1007/s13244-015-0429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reissig A, Copetti R, Kroegel C. Current role of emergency ultrasound of the chest. Crit Care Med. 2011;39(4):839–845. doi: 10.1097/CCM.0b013e318206d6b8. [DOI] [PubMed] [Google Scholar]
- 29.Ojaghi Haghighi SH, Adimi I, Shams Vahdati S, Sarkhoshi Khiavi R. Ultrasonographic diagnosis of suspected hemopneumothorax in trauma patients. Trauma Mon. 2014;19(4):e17498. doi: 10.5812/traumamon.17498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kumar S, Agarwal R, Aggarwal AN, Gupta D, Jindal SK. Role of ultrasonography in the diagnosis and management of pneumothorax following transbronchial lung biopsy. J Bronchol Interv Pulmonol. 2015;22(1):14–19. doi: 10.1097/LBR.0000000000000125. [DOI] [PubMed] [Google Scholar]
- 31.Ku BS, Fields JM, Carr B, Everett WW, Gracias VH, Dean AJ. Clinician-performed beside ultrasound for the diagnosis of traumatic pneumothorax. West J Emerg Med. 2013;14(2):103–108. doi: 10.5811/westjem.2012.12.12663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ianniello S, Di Giacomo V, Sessa B, Miele V. First-line sonographic diagnosis of pneumothorax in major trauma: accuracy of e-FAST and comparison with multidetector computed tomography. Radiol Med. 2014;119(9):674–680. doi: 10.1007/s11547-014-0384-1. [DOI] [PubMed] [Google Scholar]
- 33.Hyacinthe AC, Broux C, Francony G, Genty C, Bouzat P, Jacquot C, et al. Diagnostic accuracy of ultrasonography in the acute assessment of common thoracic lesions after trauma. Chest. 2012;141:1177–1183. doi: 10.1378/chest.11-0208. [DOI] [PubMed] [Google Scholar]
- 34.Rocco M, Carbone I, Morelli A, et al. Diagnostic accuracy of bedside ultrasonography in the ICU: feasibility of detecting pulmonary effusion and lung contusion in patients on respiratory support after severe blunt thoracic trauma. Acta Anaesthesiol Scand. 2008;52(6):776–784. doi: 10.1111/j.1399-6576.2008.01647.x. [DOI] [PubMed] [Google Scholar]
- 35.Ashton-Cleary DT. Is thoracic ultrasound a viable alternative to conventional imaging in the critical care setting? Br J Anaesth. 2013;111(2):152–160. doi: 10.1093/bja/aet076. [DOI] [PubMed] [Google Scholar]
- 36.Chan SS. Emergency bedside ultrasound to detect pneumothorax. Acad Emerg Med. 2003;10(1):91–94. doi: 10.1197/aemj.10.1.91. [DOI] [PubMed] [Google Scholar]
- 37.Volpicelli G. The double lung point. Am J Emerg Med. 2011;29(7):832–833. doi: 10.1016/j.ajem.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 38.Chung MJ, Goo JM, Im JG, Cho JM, Cho SB, Kim SJ. Value of high-resolution ultrasound in detecting a pneumothorax. Eur Radiol. 2005;15:930–935. doi: 10.1007/s00330-004-2518-7. [DOI] [PubMed] [Google Scholar]
- 39.Langdorf MI, Medak AJ, Hendey GW, et al. Prevalence and clinical import of thoracic injury identified by chest computed tomography but not chest radiography in blunt trauma: multicenter prospective cohort study. Ann Emerg Med. 2015;66(6):589–600. doi: 10.1016/j.annemergmed.2015.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wolfman NT, Gilpin JW, Bechtold RE, Meredith JW, Ditesheim JA. Occult pneumothorax in patients with abdominal trauma: CT studies. J Comput Assist Tomogr. 1993;17(1):56–59. doi: 10.1097/00004728-199301000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Ball CG, Kirkpatrick AW, Feliciano DV. The occult pneumothorax: what have we learned? Can J Surg. 2009;52(5):E173–E179. [PMC free article] [PubMed] [Google Scholar]
- 42.Ball CG, Dente CJ, Kirkpatrick AW, et al. Occult pneumothoraces in patients with penetrating trauma: does mechanism matter? Can J Surg. 2010;53(4):251–255. [PMC free article] [PubMed] [Google Scholar]
- 43.Ball CG, Kirkpatrick AW, Laupland KB, et al. Factors related to the failure of radiographic recognition of occult posttraumatic pneumothoraces. Am J Surg. 2005;189(5):541–546. doi: 10.1016/j.amjsurg.2005.01.018. [DOI] [PubMed] [Google Scholar]
- 44.Ball CG, Kirkpatrick AW, Laupland KB, et al. Incidence, risk factors, and outcomes for occult pneumothoraces in victims of major trauma. J Trauma. 2005;59(4):917–924. doi: 10.1097/01.ta.0000174663.46453.86. [DOI] [PubMed] [Google Scholar]
- 45.Yadav K, Jalili M, Zehtabchi S. Management of traumatic occult pneumothorax. Resuscitation. 2010;81(9):1063–1068. doi: 10.1016/j.resuscitation.2010.04.030. [DOI] [PubMed] [Google Scholar]
- 46.Alrajab S, Alrajab A, Assaad U. Bedside ultrasonography for evaluation of pneumothorax. Chest. 2012;141:827–828. doi: 10.1378/chest.11-2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Richards JR, McGahan JP. Focused assessment with sonography in trauma (FAST) in 2017: what radiologists can learn. Radiology. 2017;283(1):30–48. doi: 10.1148/radiol.2017160107. [DOI] [PubMed] [Google Scholar]
- 48.Alrajhi K, Woo MY, Vaillancourt C. Test characteristics of ultrasonography for the detection of pneumothorax: a systematic review and meta-analysis. Chest. 2012;141(3):703–708. doi: 10.1378/chest.11-0131. [DOI] [PubMed] [Google Scholar]
- 49.Nandipati KC, Allameni S, Kakarla R, Wong A, Richards N, Satterfield J, et al. Extended focused assessment with sonography for trauma (EFAST) in the diagnosis of pneumothorax: experience at a community based level I trauma center. Injury. 2011;42:511–514. doi: 10.1016/j.injury.2010.01.105. [DOI] [PubMed] [Google Scholar]
- 50.Michalke JA. An overview of emergency ultrasound in the United States. World J Emerg Med. 2012;3(2):85–90. doi: 10.5847/wjem.j.1920-8642.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Abdulrahman Y, Musthafa S, Hakim SY, et al. Utility of extended FAST in blunt chest trauma: is it the time to be used in the ATLS algorithm? World J Surg. 2015;39(1):172–178. doi: 10.1007/s00268-014-2781-y. [DOI] [PubMed] [Google Scholar]