Abstract
The tympanic membrane retraction pocket is a pathological invagination of tympanic membrane into the middle ear space. The most common sites for formation of retraction pocket are pars flaccida and postero-superior parts. Decision about the procedure and the timing of the treatment of retraction pockets is debatable and depends on the functional and anatomic condition of the ear. To evaluate the results of the technique of two handed endoscopic management of retraction pockets with sliced tragal cartilage. Prospective Non Randomized Clinical Study. The study included 41 ears operated with the technique of two handed endoscopic cartilage tympanoplasty for retraction pockets with endoscope holders from November 2013 to May 2016 with a follow up period ranging from 22 to 53 months. Cases of cholesteatoma and tympanic membrane perforation were excluded from the study. Pre and postoperative symptoms and air–bone gaps were recorded. The average preoperative air–bone gap in the study group was 24.53 ± 4.326 dB. 28 ears were of pars tensa retractions (stage II-4, stage III-15, and stage IV-9) and 13 were pars flaccida retractions (stage III-8 and stage IV-5). 24 ears had ossicular erosion. The follow up revealed that, the results of two handed endoscopic sliced cartilage tympanoplasty for retraction pockets were stable and there was no recurrence of the retraction and the post-operative air–bone–gap closure was achieved to 13.62 ± 4.78, 14.13 ± 5.91 dB, 14.32 ± 3.46 and 14.57 ± 3.88 dB at 6 months, 1 year, 2 years, 3 years respectively. Though, indications for surgery are based mostly on anatomic status and observation of behaviour of retraction pocket over time, we recommend early management of retraction pockets by the technique of endoscopic sliced tragal cartilage tympanoplasty with tragal cartilage of 0.5 mm thickness using endoscope holder.
Level of Evidence: Level 4.
Electronic supplementary material
The online version of this article (10.1007/s12070-019-01682-2) contains supplementary material, which is available to authorized users.
Keywords: Retraction pockets, Two handed endoscopic ear surgery, Endoscope holders, Endoscopic sliced cartilage tympanoplasty
Introduction
The tympanic membrane retraction pocket is a pathological invagination of tympanic membrane into the middle ear cavity as a result of chronic otitis media [1]. Tympanic membrane (TM) retractions are also called as TM atelectasis (derived from Greek words, ateleˆs meaning “incomplete” and ektasis meaning “extension”). It is defined as the inward displacement of the tympanic membrane from its normal position [2]. It may vary from small retraction pocket (RP) to marked retraction leading to adherence of the tympanic membrane onto the promontory. At present, there is no clear aetiology proposed to explain the pathophysiology of the condition. It is usually regarded to be a sequel of chronic otitis media with effusion [3–6]. TMRP formation is believed to be multifactorial. First, there is a natural weakness in the PF due to the lack of a middle fibrous layer. Second, retractions of the PT are believed to result from chronic inflammatory process in chronic otitis media with effusion (OME) and Eustachian tube (ET) dysfunction. Prolonged dysfunction of the Eustachian tube and excessive negative pressure in the middle ear may lead to atrophic changes in the middle fibrous layer of tympanic membrane and to development of localized or generalized TM atelectasis. Third, other factors like developmental incoordination of the posterosuperior region of the annulus and middle ear aeration pathways have been also described [7]. The most common sites of RP are pars flaccid and postero-superior parts of TM [8].
Progression of the retraction causes the atrophic membrane to drape over the incus and stapes, often resulting in necrosis of the ossicles. Over time RP may form adhesions with the surrounding structures making changes irreversible. Another problem is that some of deep RP loses self-cleansing ability and start to accumulate debris and epithelium which are prone to infections. Infected retraction pockets may be regarded as precholesteatoma [9]. Tympanic membrane retraction pockets are of clinical significance in the pathophysiology of middle ear cholesteatoma formation. Hence correct diagnosis and management of the retraction pocket is important to prevent cholesteatoma formation. Progressive retraction onto the incus can result in erosion of the long process and adhesion to the head of stapes. The TM then retracts into the sinus tympani. As the pocket grows, the stapes superstructure may erode, but often remains intact. The TM may eventually become adherent to the promontory, extending superiorly into the attic and inferiorly into the hypotympanum towards the Eustachian tube [10].
Often, retraction pockets can be small and self-cleansing, without producing any symptoms. When they become progressive, eroding the adjacent structures, they can cause otorrhoea, hearing loss and otalgia. Effective management depends on the thorough understanding of the mechanisms involved in the formation of retraction pockets. It is known that a weakened pars tensa in the presence of persistent Eustachian tube dysfunction is the main reason for retraction [11]. Most of these classifications have followed the otoscopic description of the retracted membrane: topography, relations to ossicular chain, fundus visibility, self-cleaning, retracted membrane mobility, otorrhea and presence of keratin. Recent studies introduced endoscopic ability to visualize the TMRP fundus as criterion [12].
Tympanic membrane retraction pockets are divided into three broad categories: (1) Retraction of the Pars flacida (2) localized retraction of the Pars tensa, and (3) generalized retraction of the pars tensa or atelectasis [13]. Tos and Poulsen [14] classification is for pars flaccida retractions whereas Sade [15] classified pars tensa retractions.
From 1976 to 2007, 12 different staging systems have been described for the three different categories of TMRPs mentioned earlier. Several classifications of tympanic membrane retraction are proposed. The number of classifications itself suggests that there has not been general consensus and satisfaction with any one type. The traditional Sade classification demonstrates the progression of retraction but does not specifically mention the exact site of the pars tensa retraction and can therefore be regarded as more pathophysiological than anatomical [16].
Sade et al. [13] found that in both pars tensa and pars flaccida regions, 2% of untreated retractions developed cholesteatoma during an average 3 years follow up period. In cases of patients with OME treated with ventilation tube insertion with or without adenoidectomy, between 1 and 4% of ears developed attic cholesteatoma [14].
Early intervention surgery, though technically much easier to perform, there is always a risk of hearing deterioration and other complication in the ear with minor pathology. On the other hand “wait and watch policy” may lead to extent adhesions in the middle ear which may negatively influence final result of the treatment. This dilemma regarding the timing and the management option arises because both in early and in advanced stages the symptoms can be rather minimal, and hearing even after destruction of the long process of incus may remain almost normal. The decision about aggressive surgical treatment is not a problem in a patient with significant conductive hearing loss, but it is especially difficult in patient with normal hearing [6, 17].
The advantages of endoscope in management of retraction pocket is better visualisation of the extent of the pocket with minimal bone removal and correction of the defects in ventilation. The use of angled endoscopes allows meticulous, precise and complete removal of the retraction pocket. Till 2013, we were managing retraction pockets microscopically with endaural incision. Since 2013, after development of the endoscope holders (Patent Application No. 2313-Mum-2013 and Patent Application No. 3300-Mum-2013) [18–20], we adopted the two handed technique in endoscopic ear surgery. The endoscope holders impart stability to the endoscope, decrease the surgeon fatigue (as in single handed technique), and have better application in situations needing the simultaneous coordinated actions of both hands like drilling, fogging, haemorrhage and ossiculoplasty [20]. The aim of this study is to evaluate the results of our two handed technique of endoscopic cartilage tympanoplasty with endoscope holder. This is the first study describing the two handed technique of endoscopic management of retraction pockets with sliced tragal cartilage.
Materials and Methods
A prospective study consisting of consecutive operated 41 ears with retraction pockets with the two handed technique of endoscopic cartilage tympanoplasty with Endoscope Holders from November 2013 to April 2016 was carried out in M.I.M.E.R Medical College and Sushrut ENT Hospital with a follow up period ranging from 22 to 53 months. The institutional Ethic Review Board has approved the study. The study included 23 males and 18 females. The mean age of the study group was 32.6 ± 4.5 years. The youngest patient was 14 years of age and the oldest was 47 years of age. 28 ears were of pars tensa retractions (stage II-4, stage III-15, and stage IV-9) and 13 were pars flaccida retractions (stage III-8 and stage IV-5). 24 ears had ossicular erosion (Table 1). 8 patients were operated under local anaesthesia with intravenous sedation and 33 were operated under general anaesthesia. The details of the operative procedure was explained to all the patients and to their parents (in case of children). Written consent was taken. The average preoperative Air-Bone Gap in the study group was 36.5 ± 3.32 dB and post-operative Air–Bone gap closed to 14.13 ± 5.91 dB.
Table 1.
Ossicular erosion
| Ossicle eroded | Number of ears |
|---|---|
| Malleus only | 2 |
| Incus only | 15 |
| Stapes only | 2 |
| Incus and malleus | 3 |
| All ossicles | 2 |
| Total | 24 |
Operative Set Up and Surgical Technique
The operative set up includes 18 cm 4 mm Karl Storz Zero degree endoscope, triple charge coupled device Camera (Karl Storz, Germany), Endoscope holder (Patent Application No. 2313-Mum-2013 or Patent Application No. 3300-Mum-2013), Slice !t (Dr Khan’s Creations, India) and the micro-ear instruments. The patient is prepared and draped in the usual fashion. The patient is in supine position with the head turned to the opposite side and the ipsilateral shoulder down. The ear canal is infiltrated with 2 percent lidocaine with 1:200000 adrenaline. The endoscope is mounted on the endoscope holder.
Design of the First Endoscope Holder- (Patent Application No. 2313-Mum-2013)
It is a modification of the otomicroscope (Optofine Microscope, India), from which the microscope head is removed and is mounted with a metallic plate of 70 × 40 × 10 mm in dimensions with a slot measuring 16 × 16 mm in diameter with tightening screws (Fig. 1).
Fig. 1.

First endoscope holder, Endohold
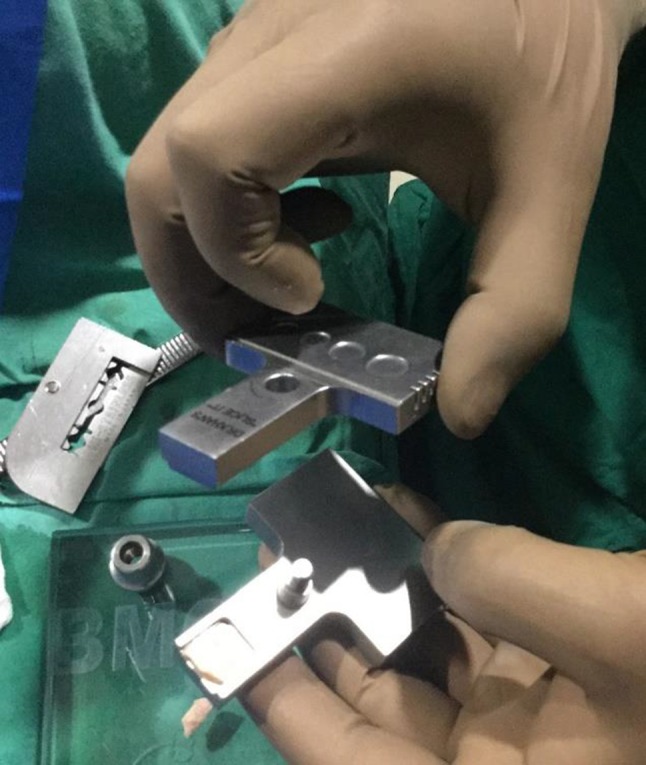
Design of Second Endoscope Holder- (Patent Application No. 3300-Mum-2013)
It is a metallic plate of 170 × 70 × 12 mm in dimensions with a circular slot measuring 16 × 16 mm in diameter and square slot to hold rigid endoscope (Fig. 2). It has to be fixed to the optical system of any operating ENT microscope with the built in tightening screws and converts a pre-existing microscope into an endoscope holder.
Fig. 2.
Second endoscope holder, Justtach
The basic idea behind both endoscope holders is to apply and utilise all the microscope motions in space to drive the endoscope into the middle ear cavity. It also allows to tilt the endoscope in any direction (rotated forwards, rotated backwards, upwards, downwards and sidewise angular rotation).
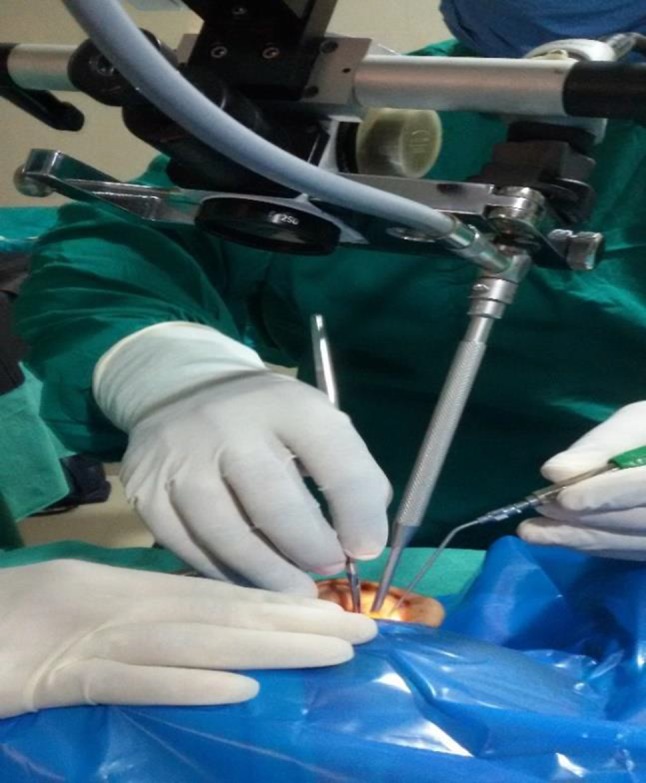
Tragal Cartilage Graft Harvest and its Preparation [20–27] (Fig. 3)
Fig. 3.
Slicing with slice it
A horizontal incision is taken on the tragal skin retaining the superior 5 mm for cosmesis. The tragal cartilage of desired size of approximately 15 x 15 mm is harvested. Slicing of the cartilage is done with Slice !t (Dr. Khan’s Creations, India) to achieve the acoustic benefit. The metallic thickness plates 0.15 mm, 0.25 mm, 0.35 mm and 0.5 mm are provided with the slicer so as to achieve the graft of desired respective thickness. The advantage of the slicing is not only thinning of the graft but also obtaining multiple grafts of varied thickness from a single 15 mm x 15 mm graft. We usually prefer graft thickness less than 0.5 mm with perichondrium retained on one side for tympanic membrane reconstruction and retraction pocket reinforcement [5–11].
Endoscopic examination is done to evaluate the retraction pocket for its depth, extent, adhesion to the ossicle and for the presence of keratin debris (Figs. 4–6). Transcanal incision is taken. The tympanomeatal flap is elevated to the annulus. The middle ear is entered by elevating the fibrous annulus below the chorda tympani. Gentle elevation of the TM is done over the eroded ossicles to prevent any residual epithelial remnant. Transcanal atticotomy (Fig. 7) is performed with a microdrill system under endoscopic visualisation to elevate the retraction pocket completely. The surgical field is irrigated frequently during all surgical steps. The antrum is then checked for any pathology by the use of the angled endoscope. Due to the panoramic view of the endoscope, it is possible to see behind the corners and allows correction of the pathology without much bone removal. In the two handed technique of endoscopic ear surgery with our endoscope holders, the suction is held in the left hand and the micro-ear instruments in the right hand similar to the microscopic ear surgery. During drilling too, simultaneous drilling with the right hand and the suction cannula in the left hand is possible. Continuous suction and intermittent irrigation is possible only with two handed endoscopic technique using endoscope holder. After removal of the pathology, the attic is reinforced with sliced tragal cartilage. In case of ossicular erosion, ossiculoplasty is done. The reconstruction of the tympanic membrane is done with the sliced tragal cartilage. The tympanomeatal flap is repositioned. Gelfoam is placed. Meatal pack is placed. The patients are operated on a day care basis.
Figs. 4 to 6.
Retraction pockets
Fig. 7.

Transcanal atticotomy for retraction pocket
Follow Up
First follow up is after 48 h for the meatal pack removal. The patient is advised analgesics (paracetamol and ibuprofen), antibiotics (amoxillin 500 mg and clavulanic acid 125 mg) for 5 days. Thereafter the next follow up is after 15 days, and then monthly for 6 months and then 6 monthly for 2 years (Fig. 8). The postoperative pure tone audiogram is done at 3 months, 6 months, 1 year, 2 and 3 years.
Fig. 8.

Post-operative picture of cartilage tympanoplasty for retraction pocket
Results
A total of 41 ears with retractions pockets were operated with two handed transcanal endoscopic cartilage tympanoplasty with endoscope holders from November 2013 to April 2016 in M.I.M.E.R Medical College and Sushrut ENT Hospital. Table 2 shows the age gender distribution of the study population. The preoperative air–bone–gap was 24.53 ± 4.326 dB and the post-operative air–bone–gap was 13.62 ± 4.78, 14.13 ± 5.91 dB, 14.32 ± 3.46 and 14.57 ± 3.88 dB at 6 months, 1 year, 2 years, 3 years respectively (Table 3). The operated patients were meticulously followed up by endoscopic recording to check for any anatomical (recurrence of retraction pocket) and audiologically to assess functional (hearing loss) defect. In our study with the follow up of 3 years, we did not encounter any recurrence of the disease.
Table 2.
Staging of the retraction pocket of the study population
| Retraction pocket | Number of ears | ||
|---|---|---|---|
| Pars tensa | Pars flaccida | Total | |
| Stage II | 4 | 0 | 4 |
| Stage III | 15 | 8 | 23 |
| Stage IV | 9 | 5 | 14 |
| Total | 28 | 13 | 41 |
Table 3.
Pre and post-operative AB gap of endoscopic cartilage tympanoplasty at 1 year, 2 years and 3 years
| Preop AB Gap | Post op 6 months | Post op one year | Post op 2 years | Post op 3 years |
|---|---|---|---|---|
| 24.53 ± 4.326 | 13.62 ± 4.78 | 14.13 ± 5.91 dB | 14.32 ± 3.46 | 14.57 ± 3.88 |
Discussion
The following staging systems [5, 13] are proposed for the retraction pockets:
Sadé
I: retracted tympanic membrane;
II: retraction with contact onto incus;
III: middle ear atelectasis (tympanic membrane on to the promontory, but mobile);
IV: adhesive otitis media (tympanic membrane on to the promontory, but fixed).
Tos
I: pars flaccida not in contact with malleus head;
II: pars flaccida in contact with malleus head;
III: limited outer attic wall erosion;
IV: severe outer attic wall erosion.
A further 3 stage classification system was proposed by Charachon et al. [28]:
Stage 1: mobile retraction pocket;
Stage 2: fixed and controllable retraction pocket;
Stage 3: fixed and uncontrollable retraction pocket.
In patients with RPs, hearing loss is not the complaint. In many cases of atelectatic ears in spite of advanced middle ear pathology, hearing is almost normal for long time. Therefore, it is improper taking hearing status only as the indication for surgery. As in these situations, unnecessary postponing of surgery can lead to cholesteatoma formation or advanced adhesions, creating difficulties for successful surgical correction [6].
The term preventive tympanoplasty [6, 17] was proposed in 1995 by Chiossone. It means surgery of ear with good hearing but with progressively developing pathology in the form of RP with potential of developing cholesteatoma. It meant that main indication for surgery was not hearing status, but anatomical state of TM and middle ear pathology, which if untreated, tend to progress over time. Chiossone treated the adhesions by separating them and placing a guitar-shaped silastic in middle ear cavity under tympanomeatal flap and annulus. In case of major retraction pockets, the retraction pocket was removed and overlay myringoplasty was performed. Successful preventive tympanoplasty means improvement of hearing rather than deterioration [6, 17]. In preventive tympanoplasty, the criteria for surgery should include meticulous follow up of the patient and the oto-endoscopic findings [6].
The cartilage is more rigid as compared to the temporalis fascia and forms the graft of choice in management of retraction pockets. The rigidity of the cartilage prevents retraction, re-perforation even in the mileau of continuous Eustachian tube dysfunction. It is of immense importance in the management of some situations such as advanced middle ear pathology, retraction pockets, and atelectatic ears. We prefer the tragal cartilage, a yellow fibro-elastic cartilage. Cartilage cells receive their nutrition by diffusions from vessels. Chondrocytes lie in lacunae in matrix. Ground substance is made of complex molecules containing proteins and carbohydrates (proteoglycans). These molecules form a meshwork that is filled by water and dissolved salts. The carbohydrates are chemically glycosaminoglycans including chondroitin sulfate, keratin sulfate, and hyaluronic acid. The core protein is aggrecan. The proteoglycan molecules are tightly bound. Along with the water content, these molecules form a firm gel that gives cartilage its firm consistency [29].
Zahnart and Huttenbrink [30] demonstrated the acoustic benefit by reducing the thickness of the cartilage to less than 0.5 mm. The rigidity of the cartilage is thought to interfere with the sound conduction. In our study, the retractions were treated with sliced tragal cartilage using the two handed technique of endoscopic ear surgery so as to impart rigidity as well as allow acoustic benefit. In our study, we achieved better sound conduction by precise slicing of the cartilage with Slice!t.
In the two handed technique, the endoscope is mounted on either of our two endoscope holders.it combines and imparts additional advantage of the endoscope along with the two handed technique. Due to endoscopic technique, the approach is the non-invasive one with permeatal incision. The panoramic view of the endoscope allows better clearance of the disease. At present, the world scenario of EES is single handed technique in which the endoscope is held in the left hand of the surgeon and the micro-ear instrument in the right hand. The problem of one handed endoscopic ear surgery is more evident during the drilling and hemorrhage (in which simultaneous suction and irrigation is not possible), during fogging of the endoscope (one needs to remove endoscope again and again for lens cleaning), during prosthesis fitting in ossiculoplasty (manipulation may be difficult with one hand). This necessitated the design and development of our endoscope holders [18–20] to allow the coordinated action of the two hands during EES.
The advantages of the two handed technique of EES for retraction pocket management are as follows [20]:
Allows two handed technique as both the hands are free for surgical intervention.
As endoscope is mounted on endoholder, stable, non-shaky image on monitor.
No fatigue of the surgeon holding the endoscope in the left hand.
Elevation of the tympanomeatal flap and excision of the retraction pocket is more precise due to the left hand suctioning and clearing the blood.
Better visualisation of the sinus tympani, facial recess, anterior tympanic cavity and hypotympanum and hence better removal of pathology.
Simultaneous suction and drilling possible during atticotomy.
Simultaneous use of suction during instrumentation brings about cooling effect.
Thermal effect of the light source can be decreased by the simultaneous irrigation.
Can be used without affecting sterility.
Fogging of the endoscope is avoided by use of suction cannula and irrigation.
Disadvantages [20]:
Narrow canal.
Additional cost of the endoscope holder.
Advantages of Sliced Cartilage Tymapnoplasty [21]
Helps to achieve acoustic benefit.
Slicing provides with multiple grafts of different thickness from a single 15 × 15 mm cartilage graft.
Improved results with closure of the tympanic membrane perforations in 98.20%.
Low recurrence in 2-year follow-up.
Resistant to repeated infection due to rigidity.
No retraction and adhesion of tympanic membrane in postoperative follow-up of 3 years.
To avoid curling of the sliced tragal cartilage, we prefer separating the perichondrium from both sides of the cartilage and then slicing the tragal cartilage to less than 0.5 mm thickness for reinforcement of the curetted posterosuperior meatal wall.
In our study of the two handed endoscopic management of retraction pocket with sliced tragal cartilage, we did not encounter any recurrence of the disease during the 3 year follow up period.
Limitations
Smaller study group.
Conclusion
We recommend management of retraction pockets by the non-invasive two handed technique of endoscopic sliced cartilage tympanoplasty. We prefer sliced tragal cartilage of 0.5 mm thickness due to its advantages as mentioned for the treatment of the retraction pockets. Indications for surgery should be based mostly on anatomic status and observation of behaviour of retraction pocket over time, as hearing usually continues to be normal for a long period of time.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Compliance with Ethical Standards
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee and with the 1964 Helsinski declaration and its later ammendments or comparable ethical standards.
Conflict of interest
None.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Michaels L. Biology of cholesteatoma. Otolaryngol Clin North Am. 1989;22:869–881. [PubMed] [Google Scholar]
- 2.Yoon TH, Schachern PA, Paparella MM, Aeppli DM. Pathology and pathogenesis of tympanic membrane retraction. Am J Otolaryngol. 1990;11(1):10–17. doi: 10.1016/0196-0709(90)90164-Q. [DOI] [PubMed] [Google Scholar]
- 3.Li Y, Hunter LL, Margolis RH, Levine SC, Lindgren B, Daly K, Giebink GS. Prospective study of tympanic membrane retraction, hearing loss, and multifrequency tympanometry. Otolaryngol Head Neck Surg. 1999;121(5):514–522. doi: 10.1016/S0194-5998(99)70049-5. [DOI] [PubMed] [Google Scholar]
- 4.Maw AR, Bawden R. Tympanic membrane atrophy, scarring, atelectasis and attic retraction in persistent, untreated otitis media with effusion and following ventilation tube insertion. Int J Pediatr Otorhinolaryngol. 1994;30(3):189–204. doi: 10.1016/0165-5876(94)90060-4. [DOI] [PubMed] [Google Scholar]
- 5.Sade J, Berco E. Atelectasis and secretory otitis media. Ann Otol Rhinol Laryngol. 1976;85(2 Suppl 25 Pt 2):66–72. doi: 10.1177/00034894760850S214. [DOI] [PubMed] [Google Scholar]
- 6.Mierzwiński J, Fishman AJ (2014) Retraction pockets of tympanic membrane: protocol of management and results of treatment. Otorynolaryngologia 13(2)
- 7.Huy PTB. Otites moyennes chroniques. Histoire e´le´mentaire et formes cliniques. EMC-Oto-rhino-laryngologie. 2005;2(1):26–61. doi: 10.1016/j.emcorl.2004.08.002. [DOI] [Google Scholar]
- 8.Ars BM. Tympanic membrane retraction pockets. Etiology, pathogeny, treatment. Acta Otorhinolaryngol Belg. 1991;45(3):265–277. [PubMed] [Google Scholar]
- 9.Kasbekar AV, Patel V, Rubasinghe M, Srinivasan V. The surgical management of tympanic membrane retraction pockets using cartilage tympanoplasty. Indian J Otolaryngol Head Neck Surg. 2014;66(4):449–454. doi: 10.1007/s12070-014-0764-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Akyildiz N, Akbay C, Ozgirgin ON, Bayramoglu I, Sayin N. The role of retraction pockets in cholesteatoma development: an ultrastructural study. Ear Nose Throat J. 1993;72(3):210–212. doi: 10.1177/014556139307200307. [DOI] [PubMed] [Google Scholar]
- 11.Ramakrishnan Y, Kotecha A, Bowdler DA. A review of retraction pockets: past, present and future management. J Laryngol Otol. 2007;121:521–525. doi: 10.1017/S0022215106003550. [DOI] [PubMed] [Google Scholar]
- 12.Bours AF, Decat M, Gersdorff M. Our classification of tympanic retraction pockets. Acta Otorhinolaryngol Belg. 1998;52(1):25–28. [PubMed] [Google Scholar]
- 13.Sadæ J, Avraham S, Brown M. Atelectasis, retraction pockets and cholesteatoma. Acta Otolaryngol. 1981;92(5–6):501–512. doi: 10.3109/00016488109133289. [DOI] [PubMed] [Google Scholar]
- 14.Tos M, Poulsen G. Attic retractions following secretory otitis. Acta Otolaryngol. 1980;89:479–486. doi: 10.3109/00016488009127165. [DOI] [PubMed] [Google Scholar]
- 15.Sade J. The atelectatic ear. In: Sade J, editor. Monograms in clinical otolaryngology, secretory otitis media and its sequelae. New York: Churchill-Livingstone; 1979. pp. 64–88. [Google Scholar]
- 16.Alzahrani M, Saliba I. Tympanic membrane retraction pocket staging: is it worthwhile? Eur Arch Oto-Rhino-Laryngol. 2014;271(6):1361–1368. doi: 10.1007/s00405-013-2644-4. [DOI] [PubMed] [Google Scholar]
- 17.Chiossone E. Preventive tympanoplasty in children: a new approach. Rev Laryngol Otol Rhinol (Bord) 1995;116(2):137–139. [PubMed] [Google Scholar]
- 18.Khan MM, Parab SR. Novel concept of attaching endoscope holder to microscope for two handed endoscopic tympanoplasty. Indian J Otolaryngol Head Neck Surg. 2016;68(2):230–240. doi: 10.1007/s12070-015-0916-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khan MM, Parab SR. Concept, design and development of innovative endoscope holder system for endoscopic otolaryngological surgeries. Indian J Otolaryngol Head Neck Surg. 2015;67(2):113–119. doi: 10.1007/s12070-014-0738-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khan MM, Parab SR. Endoscopic cartilage tympanoplasty: a two-handed technique using an endoscope holder. Laryngoscope. 2016;126:1893–1898. doi: 10.1002/lary.25760. [DOI] [PubMed] [Google Scholar]
- 21.Khan MM, Parab SR. Primary cartilage tympanoplasty: our technique and results. Am J Otolaryngol. 2011;32(5):381–387. doi: 10.1016/j.amjoto.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 22.Khan MM, Parab SR. Reinforcement of Sliced Tragal Cartilage Perichondrium Composite Graft with Temporalis Fascia in Type I Tympanoplasty: Our Techniques and Results. J Rhinol-Otol. 2013;1:57–62. [Google Scholar]
- 23.Khan MM, Parab SR. Day care ear surgery: our experience of 4 years. Indian J Otolaryngol Head Neck Surg. 2012;64(3):280–284. doi: 10.1007/s12070-011-0303-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khan MM, Parab SR. Sliced Island tragal cartilage perichondrial composite graft: early results and experience. J Rhinol-Otol. 2014;2:4–9. [Google Scholar]
- 25.Khan MM, Parab SR. Comparative study of sliced tragal cartilage and temporalis fascia in type I tympanoplasty. J Laryngol Otol. 2015;129(1):16–22. doi: 10.1017/S0022215114003132. [DOI] [PubMed] [Google Scholar]
- 26.Khan MM, Parab SR. Average thickness of tragal cartilage for slicing techniques in tympanoplasty. J Laryngol Otol. 2015;129(05):435–439. doi: 10.1017/S0022215115000055. [DOI] [PubMed] [Google Scholar]
- 27.Parab SR, Khan MM. New cartilage slicer for slicing techniques in tympanoplasty: design and applications. Indian J Otolaryngol Head Neck Surg. 2018 doi: 10.1007/s12070-018-1467-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Charachon R, Barthez M, Lejeune JM. Spontaneous retraction pockets in chronic otitis media medical and surgical therapy. Ear Nose Throat J. 1992;71(11):578–583. doi: 10.1177/014556139207101109. [DOI] [PubMed] [Google Scholar]
- 29.Singh I (ed) (2004) Textbook of human histology. New Delhi: Jaypee Brothers Medical Publishers. 89–93
- 30.Zahnert T, Huttenbrink KB, Murbe D, et al. Experimental investigations of the use of cartilage in tympanic membrane reconstruction. Am J Otol. 2000;21:322–328. doi: 10.1016/S0196-0709(00)80039-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



