Abstract
Septorhinoplasty is particularly challenging among revision surgeries for cleft sequelae. The challenge of cleft septorhinoplasty is mainly due to the complex anatomy of nose, deformity of each of its components and the difficulty and lack of clarity in surgical management. From 2014 to 2017, 26 patients with cleft lip nose deformity were operated by the same cleft team. The study was conducted to assess the improvement in nasal airway and appearance following secondary rhinoplasty with extracorporeal septoplasty. Post operatively each patient was evaluated using the standard modified rhinoplasty outcome evaluation questionnaire, a validated instrument that aids in stratifying patients according to their subjective response. All patients reported great relief of nasal obstruction and improved breathing. More than 80% of our patients were satisfied with improved aesthetics and reported better self-confidence. Secondary cleft rhinoplasty with extracorporeal septoplasty surgery significantly improves the cosmesis and nasal airway opening, subsequently giving them improved self-confidence.
Keywords: Congenital cleft deformity, Cleft rhinoplasty, Extracorporeal septoplasty, Functional nasal airway, Rhinoplasty outcome evaluation
Introduction
The surgical approach to the cleft deformity requires an ongoing treatment plan from infancy to adulthood. The challenge of cleft septorhinoplasty is mainly due to the complex anatomy of nose, with structural deformity of each of its components and the difficulty in surgical management.
The prime objective of cleft lip nose revision surgery is to create a functional airway and aesthetically pleasing nose with minimal surgical stigmata. Most of the patients seek surgery primarily for aesthetic concerns, but all of them suffer from nasal airway obstruction also. In our study we aimed to see the nasal airway improvement after combining extracorporeal septoplasty [1] with secondary rhinoplasty in all patients. Hence pre-operative analysis of nasal airway is an essential step in operative planning even if the patient has no symptoms of nasal airway obstruction [2].
Several reasons contribute to the secondary cleft lip nose deformity, which includes residual primary deformity, inadequate tissue growth and iatrogenic deformity. Secondary rhinoplasty is aimed at straightening the nasal septum and nasal pyramid, augmentation of the nasal dorsum, definition and projection of nasal tip with adequate symmetry, improvement of nasal airway, augmentation of nasal base, aesthetic projection and symmetry of upper alveolus in all cases.
Materials and Methods
Between 2014 and 2017, all patients presenting with unilateral and bilateral cleft nose deformity undergoing rhinoplasty and extracorporeal septoplasty were included in the study after obtaining their consent.
Surgical Procedure
All patients underwent open rhinoplasty under general anaesthesia by step incision on columella and alar rim incision, exposing lower lateral cartilages and dorsal cartilage. Exposure of septum was done through the same rhinoplasty approach, by elevating mucoperichondrial flaps on either side. Chondrovomerine junction and anterior nasal spine were exposed and cartilaginous septum was taken out. Correction of bony septal deformity [3] was achieved by selective removal of deviated bony parts of vomer and perpendicular plate of ethmoid. Septal deviation was corrected by scoring on the concave side and by attaching pieces of cartilage together, when necessary. Corrected septum was fixed back to anterior nasal spine with quilt sutures to the mucoperichondrial flap. Whenever necessary to clear the airway, this was combined with reduction of middle and inferior turbinates, and opening sinus ostia by endoscopic sinus surgery. Cephalic trimming of lower lateral cartilage was done. Cartilage overgraft was also placed when indicated, to support and augment the columella, lower lateral cartilages and dorsum. Exposure of the alar base was achieved through sublabial incision. Costochondral graft and cortical bone was placed to enhance the pyriform aperture, if needed and closure was done. Hitched sutures to narrow alar base and Tajima sutures for suspension of alar cartilage was done for completion.
The rhinoplasty outcome evaluation (ROE) questionnaire was used to evaluate the patient satisfaction. The ROE questionnaire was first described by Alsarraf et al. [4] to measure facial aesthetic surgery outcome, and was used by Sawyer et al. [5] for cleft rhinoplasty patients. The questionnaire included six questions (Table 1) which the patient has to score preoperatively and postoperatively (at or after 6 months) [5]. Each question was scored on a scale of 0 to 4 points with the maximum score of 24 points. The total scores were compared using a paired t test (IBM SPSS statistics ver25), p value was considered significant at 0.005.
Table 1.
Rhinoplasty outcome evaluation (ROE) questionnaire
| Q. no | Parameters | Scoring | Score |
|---|---|---|---|
| Q1 | How well do you like the appearance of your nose? | Not at all [0]—somewhat [1]—moderately [2]—very much [3]—completely [4] | |
| Q2 | How well are you able to breathe through your nose? | Not at all [0]—somewhat [1]—moderately [2]—very much [3]—completely [4] | |
| Q3 | How much do you feel your friends and those close to you like your nose? | Not at all [0]—somewhat [1]—moderately [2]—very much [3]—completely [4] | |
| Q4 | Do you think the current nasal appearance limits your social or professional activities? | Always [0]—usually [1]—sometimes [2]—rarely [3]—never [4] | |
| Q5 | How confident are you that your nasal appearance is the best that it can be? | Not at all [0]—somewhat [1]—moderately [2]—very much [3]—completely [4] | |
| Q6 | Would you like to surgically alter the appearance or function of your nose? | Definitely[0]—Most likely [1]—Possibly [2]—Probably not [3]—Never [4] | |
| Total score | 0–24 |
Results
A total of 26 patients with combined cleft lip and nose deformities underwent surgery and completed the questionnaire. 19 patients had unilateral and 7 patients had bilateral cleft lip deformity. There were 15 males and 11 females, their ages varied from 18 to 23 with an average age of 20 years.
The scores were tabulated and analysis was done using paired t test and a statistically significant p value (p < 0.001) was obtained (Table 2). The graphical comparison between the pre- and postoperative total scores is shown (Fig. 1) along with comparison of unilateral and bilateral patient subgroups. Individual subjective parameters (questions 1–6) were analysed using paired t test and significant improvement (Fig. 2) was noted in each of those (p < 0.001 for all parameters). Data of the same is shown (Table 3). Pre-operative and post-operative photos of representative cases are shown (Fig. 3).
Table 2.
Rhinoplasty Outcome Evaluation (ROE) questionnaire results showing Pre-op and Post-op mean scores with difference in scores and p-value
| Data | n | Pre-op mean (SD) | Post-op mean (SD) | Difference mean (SD) | p value |
|---|---|---|---|---|---|
| Total scores | 26 | 8.35 (1.79) | 19.85 (2.09) | 11.5 (2.17) | < 0.001 |
| Unilateral group | 19 | 8.0 (1.86) | 19.53 (2.09) | 11.53 (2.46) | < 0.001 |
| Bilateral group | 7 | 9.26 (1.25) | 20.71 (1.98) | 11.43 (1.27) | < 0.001 |
n number of patients, SD standard deviation
Fig. 1.
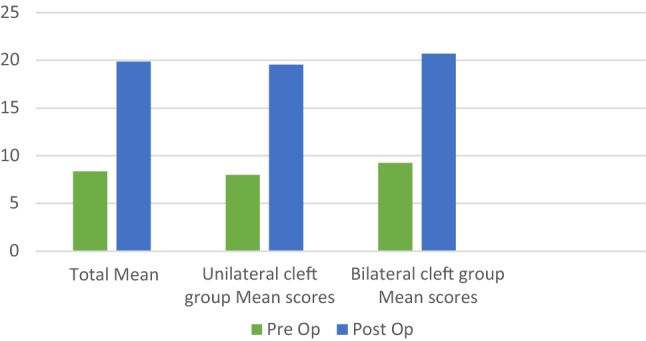
Comparison of pre-op and post-op total mean scores based on rhinoplasty outcome evaluation (ROE) questionnaire results. Similar comparison for unilateral and bilateral subgroups is also shown
Fig. 2.

Comparison of difference in scores for individual questions of rhinoplasty outcome evaluation (ROE) questionnaire. Difference in score = post-op score − pre-op score (x axis—questions, y axis—mean scores of each question)
Table 3.
Analysis of Individual questions of the questionnaire
| Q. no | Questions | n | Pre-op mean (SD) | Post-op mean (SD) | Difference mean (SD) | p value |
|---|---|---|---|---|---|---|
| Q1 | How well do you like the appearance of your nose? | 26 | 1.54 (0.51) | 3.23 (0.59) | 1.69 (0.62) | < 0.001 |
| Q2 | How well are you able to breathe through your nose? | 26 | 1.61 (0.5) | 3.54 (0.58) | 1.92 (0.74) | < 0.001 |
| Q3 | How much do you feel your friends and those close to you like your nose? | 26 | 1.88 (0.52) | 3.42 (0.50) | 1.54 (0.76) | < 0.001 |
| Q4 | Do you think the current nasal appearance limits your social or professional activities? | 26 | 1.73 (0.67) | 3.5 (0.65) | 1.77 (0.71) | < 0.001 |
| Q5 | How confident are you that your nasal appearance is the best that it can be? | 26 | 0.84 (0.73) | 3.04 (0.45) | 2.19 (0.8) | < 0.001 |
| Q6 | Would you like to surgically alter the appearance or function of your nose? | 26 | 0.73 (0.53) | 3.11 (0.59) | 2.38 (0.75) | < 0.001 |
n number of patients, SD standard deviation
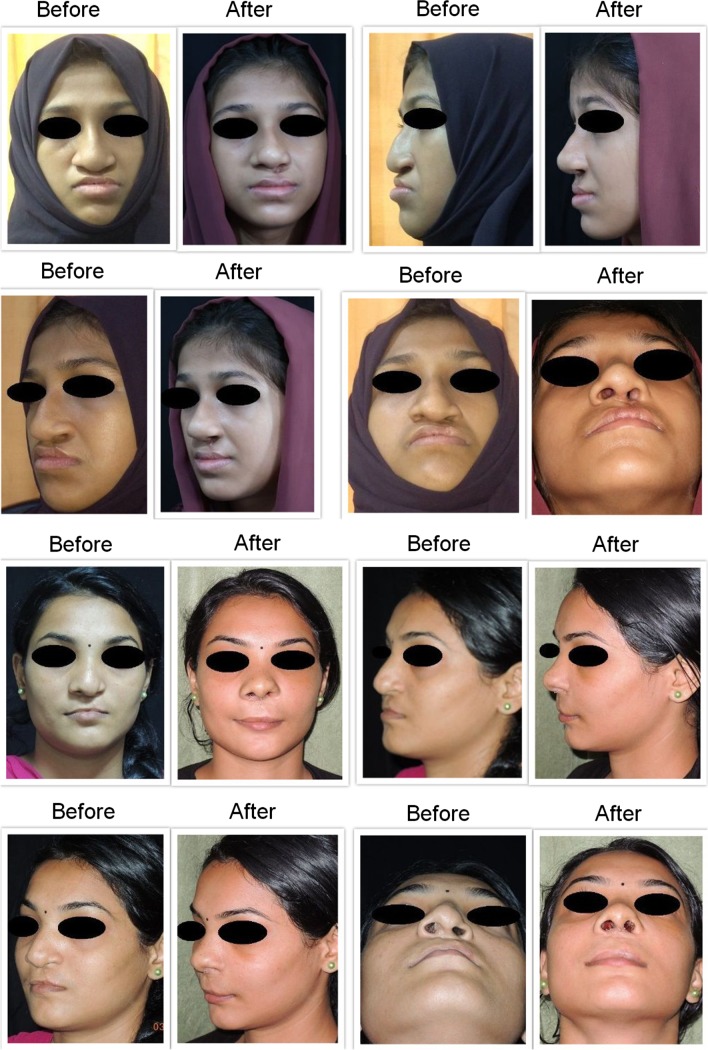
Fig. 3.
Photographs showing the surgical results of two representative patients
Discussion
Deformities in unilateral cleft nose includes slumped ala, deviated nasal septum, nostril size asymmetry, poor tip projection, deformity of nasal dorsum, poor lip scars, oronasal fistula, prealveolar fistula, underlying retromaxillism and persistent vestibular web. In bilateral cases there will be short or absent columella, alar collapse, inadequate lobule and tip projection [6]. Correction of malocclusion was addressed first with orthodontic surgical advancement before proceeding to definitive rhinoplasty whenever possible [7].
The factors which determine the secondary nasal deformity include original cleft lip-nose defect, previous surgery [8] and nasal growth. In secondary cleft septorhinoplasty, these key factors contributing to nasal deformity are identified. Once the patient has reached facial skeletal maturity, definitive septorhinoplasty can be planned. Structural cleft nose reconstruction requires graft materials from nasal septum, rib cartilage, pinna or iliac crest to produce good support. The goals of secondary rhinoplasty are the creation of symmetry and definition of the nasal base and tip, along with the relief of nasal obstruction and management of nasal scarring and webbing [9].
Surgery was done with the purpose of (a) correction of columellar and alar deformity (b) septal correction for deviation (c) correction of dorsal deviation (d) alar base augmentation with bone or cartilage graft [10] around pyriform aperture (e) lip revision, if needed.
Standard rhinoplasty involves rim incision, exposing both lower and upper lateral cartilages, dorsum and septum. Complete bilateral mucoperichondrial elevation of septum is done upto the floor of nose. Cartilaginous nasal septum is dissected out for extracorporeal correction of nasal septum with controlled resection of septal spur, replacement of septum in midline with anchoring to anterior nasal spine and to midline dorsum and finally addressing nasal tip in all rhinoplasty procedures. Placing cartilaginous grafts can immediately improve the nasal contour.
Cleft noses commonly have grossly deformed septum and its correction requires meticulous assessment and techniques. Vass et al. [11] studied the usefulness of modified ROE questionnaire in cleft lip and palate patients undergoing rhinoplasty and found it simple and adequate for evaluation of surgical results. The extracorporeal septoplasty procedure though is a well-known tool in aesthetic rhinoplasty, has been studied less frequently in cleft situations.
An extracorporeal septoplasty, done as the standard procedure in all the cases, involves harvesting the septal cartilage followed by reshaping and re-implantation [12]. It is usually combined with cartilage grafts for support and strength of re-implanted septum. Cartilage grafts over nasal tip improves tip symmetry, definition and projection. Concavity of lateral crus on cleft side lower lateral cartilage is often associated with alar malposition. It results in external nasal valve collapse and a functional nasal deformity, which can be addressed by cartilage grafting and or suture suspension [13]. Cleft alar-facial junction needs to be repositioned to create alar base symmetry [14]. Secondary deformity of nasal sill can arise due to original cleft lip repair. It can be corrected by realignment of superior portion of orbicularis oris muscle.
Sawyer et al. [5] in their study found that the functional outcome was less significant compared to the aesthetic improvement. In our study, all patients were satisfied with the improved postoperative aesthesis and function of their nose. The difference in pre and post-operative scores for each question was calculated. Though improvements were noted in both aesthetic and functional aspects, functional improvement (Q2) was more than aesthetic improvement (Q1, Q3) as shown in Fig. 2. The functional improvement was also found to be statistically significant (p < 0.001).
Conclusion
Secondary cleft rhinoplasty with extracorporeal septoplasty surgery significantly improves the cosmesis and nasal airway. The third dimension (nasal septum) must be invariably addressed in every secondary cleft rhinoplasty. Extracorporeal septal correction can provide promising results in cleft nose airway improvement. Attention must be paid to achieve both function and appearance.
Acknowledgements
Authors would like to thank Dr. Aarathi Krishnan for statistical guidance.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest and there was no funding or grants involved.
Informed Consent
Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gubisch W. Twenty-five years’ experience with extracorporeal septoplasty. Fac Plast Surg. 2006;22(4):230–239. doi: 10.1055/s-2006-954841. [DOI] [PubMed] [Google Scholar]
- 2.Wang Z, Wang P, Zhang Y, Shen G. Nasal airway evaluation after Le Fort I osteotomy combined with septoplasty in patients with cleft lip and palate. J Craniofac Surg. 2017;28(1):207–211. doi: 10.1097/SCS.0000000000003259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Parrilla C, Artuso A, Gallus R, Galli J, Paludetti G. The role of septal surgery in cosmetic rhinoplasty. Acta Otorhinolaryngol Ital. 2013;33(3):146–153. [PMC free article] [PubMed] [Google Scholar]
- 4.Alsarraf R, Larrabee WF, Jr, Anderson S, Murakami CS, Johnson CM., Jr Measuring cosmetic facial plastic surgery outcomes: a pilot study. Arch Fac Plast Surg. 2001;3(3):198–201. doi: 10.1001/archfaci.3.3.198. [DOI] [PubMed] [Google Scholar]
- 5.Sawyer AR, Robinson S, Cadier M. Prospective patient—related outcome evaluation of secondary cleft rhinoplasty using a validated questionnaire. Cleft Palate Craniofac J. 2017;54(4):436–441. doi: 10.1597/14-168. [DOI] [PubMed] [Google Scholar]
- 6.Pawar S, Wang TD. Secondary cleft rhinoplasty. JAMA Fac Plast Surg. 2014;16(1):58–63. doi: 10.1001/jamafacial.2013.1562. [DOI] [PubMed] [Google Scholar]
- 7.Posnick JC, Tompson B. Modification of the maxillary Le Fort I osteotomy in cleft-orthognathic surgery: the bilateral cleft lip and palate deformity. J Oral Maxillofac Surg. 1993;51(1):2–11. doi: 10.1016/S0278-2391(10)80379-9. [DOI] [PubMed] [Google Scholar]
- 8.Allori AC, Mulliken JB. Evidence-based medicine: secondary correction of cleft lip nasal deformity. Plast Reconstr Surg. 2017;140(1):166e–176e. doi: 10.1097/PRS.0000000000003475. [DOI] [PubMed] [Google Scholar]
- 9.Hsieh T, Dedhia R, Del Toro D, Tollefson T. Cleft septorhinoplasty: form and function. Fac Plast Surg Clin N Am. 2017;25(2):223–238. doi: 10.1016/j.fsc.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Shih CW, Sykes JM. Correction of the cleft-lip nasal deformity. Fac Plast Surg. 2002;18(4):253–262. doi: 10.1055/s-2002-36493. [DOI] [PubMed] [Google Scholar]
- 11.Vass G, Mohos G, Bere Z, Ivan L, Varga J, Piffko J, et al. Secondary correction of nasal deformities in cleft lip and palate patients: surgical technique and outcome evaluation. Head Face Med. 2016;12(1):34. doi: 10.1186/s13005-016-0132-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Most SP. Anterior septal reconstruction: outcomes after a modified extracorporeal septoplasty technique. Arch Fac Plast Surg. 2006;8(3):202–207. doi: 10.1001/archfaci.8.3.202. [DOI] [PubMed] [Google Scholar]
- 13.Haack J, Papel ID. Caudal septal deviation. Otolaryngol Clin N Am. 2009;42(3):427–436. doi: 10.1016/j.otc.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 14.Fisher DM, Mann RJ. A model for the cleft lip nasal deformity. Plast Reconstr Surg. 1998;101(6):1448–1456. doi: 10.1097/00006534-199805000-00003. [DOI] [PubMed] [Google Scholar]