Abstract
Health inequalities exist across countries and populations, but little is known about their long-term trends and even less about factors shaping the trends. We examined the magnitude of absolute and relative educational inequalities in self-rated health over 36 years among Finnish adults, considering individual covariates and macro-economic fluctuations. Our data were derived from representative annual cross-sectional surveys in 1979–2014 conducted among adult men and women. Participants aged 25–64 were included and nine periods used (n = 8870–14235). Our health outcome was less-than-good self-rated health (SRH) and our socioeconomic indicator was completed years of education as a continuous variable. Educational inequalities in self-rated health were analysed using the relative index of inequality (RII) and the slope index of inequality (SII). Nine time-variant sociodemographic and health-related covariates were included in the analyses. Linear trends suggested stable or slightly curvilinear overall trends in both absolute and relative health equalities over 36 years. Among men, absolute and relative inequalities narrowed immediately after economic recession in Finland in 1993–1994. Among women, inequalities narrowed during financial crisis in 2008–2009. Adjusting for most covariates reduced the magnitude of inequalities throughout the nine periods, but affected little the temporal patterning of health inequalities. Educational inequalities in self-rated health remained during 36 years in Finland. While among men and women health inequalities narrowed during and after recessions, they widened soon back to the pre-recession level. The perseverance of the trends calls for novel and powerful measures to tackle health inequalities.
Keywords: Self-rated health, Inequalities, Trends, Determinants
Highlights
-
•
Inequalities in self-rated health covering many decades are poorly known.
-
•
Relative and absolute health inequalities persisted over 36 years among Finnish men and women.
-
•
The health inequalities narrowed transiently during economic recessions.
-
•
Health behaviours and employment status reduced the magnitude of inequalities.
Introduction
Socioeconomic inequalities in health have turned out to be a scourge much tougher than thought some decades ago. Nationwide egalitarian health programmes have been launched in countries like the UK, the Netherlands, Sweden and Finland to tackle health inequalities (Hu, van Lenthe, Judge et al., 2016; Khang, Lynch, Yun, & Lee, 2004; Mackenbach 2012). Despite these efforts, health inequalities have persisted across populations, including our focus country Finland (Bouchard et al., 2015; Hu, van Lenthe, Borsboom et al., 2016; Mackenbach et al., 2018; MSAH, 2008; Palosuo et al., 2009; Townsend, Davidson, 1982; WHO, 1985; WHO, 2008). Less is known about time trends in inequalities in self-rated health and even less about longer time trends covering several decades. It is vital for scientific progress as well as practical policies to understand the long-term trends in health inequalities, i.e. whether inequalities widen or narrow, and whether there are period-specific turns. Long-term trends also help distinguish random and short-term variation from major changes in underlying secular trends, shaped by micro and macro level factors.
Studies on health inequalities have often focused on relative inequalities and overlooked absolute inequalities, although methodological reviews suggest that both should be considered when studying the magnitude, direction, significance, determinants and implications of health inequalities (Mackenbach, Kunst, 1997; King, Harper, & Young, 2012; Mackenbach, 2015). The two measures of inequalities are particularly important when factors associated with trends in health inequalities are examined. Focusing on relative inequalities emphasises inequality per se, irrespective of the levels of ill health. Focusing on absolute inequalities emphasises a more pragmatic approach suggesting that levels of ill health matter most for those in lowest socioeconomic groups. Thus, the choice between absolute and relative measures of health inequalities is not only a methodological but also a moral and political one.
We follow the methodological recommendations and use both relative and absolute measures of health inequalities when studying 36-year trends in the magnitude of educational inequalities in self-rated health among Finnish adults.
Prior Finnish studies have reported shorter, i.e. 10-20-year trends in inequalities in self-rated health from the late 1970s until early 2000s (Heistaro, Vartiainen, & Puska, 1996; Rahkonen et al., 2009). This evidence confirms that educational inequalities in self-rated health have remained mostly stable over time and even narrowed somewhat towards the end of the last millennium. Studies report descriptive prevalence data whereas analytic measures are limited to odds ratios. The Finnish trend studies cover neither long-term trends nor current health inequalities.
Studies from further countries have examined trends in inequalities in self-rated health. A German study among middle-aged men and women spanned over 21 years from 1994-2014 and examined the magnitude of educational inequalities in self-rated health using the relative index of inequality (RII) for relative and the slope index of inequality (SII) for absolute inequalities (Moor et al., 2018). Overall, the magnitude of relative as well as absolute health inequalities remained and there was no increasing or decreasing trend. Two studies using the same Japanese survey data examined occupational class inequalities in self-rated health among middle-aged men and women over 27 years (Hiyoshi, Fukuda, Shipley, & Brunner, 2013; Sugisawa, Harada, Sugihara, Yanagisawa, & Shinmei, 2016). Both relative and absolute inequalities remained stable, and high unemployment rate was associated with smaller health inequalities. Studies from the USA (Liu, Hummer, 2008) and Britain (Maheswaran, Kupek, & Petrou, 2015) showed stable or slightly widening relative educational inequalities in self-rated health over 11-21-year trends. A South Korean study reported widening relative educational inequalities in self-rated health among men and women over an 11-year trend (Khang et al., 2004). A comparative European study covering 17 countries examined educational inequalities in self-rated health over two decades (Hu, van Lenthe, Borsboom et al., 2016). Taking all countries together absolute inequalities remained largely stable, with minor country-specific deviations. However, relative inequalities showed a widening trend among men and women, in particular, in England, the Netherlands and Switzerland.
Summarising the evidence suggests that trends in absolute educational inequalities in self-rated health have remained mostly stable, whereas relative inequalities have remained stable or widened. It is striking that even minor narrowing in relative or absolute inequalities is practically non-existent. Few studies examine the magnitude of health inequalities using both relative and absolute measures. Individual covariates are included in a couple of studies only. Focusing on macro-economic fluctuations, a number of studies have suggested that economic downturns would lead to worsening health and widening health inequalities (Edwards, 2008; Karanikolos et al., 2013; Bacigalupe, Escolar-Pujolar, 2014; Sugisawa et al., 2016; Thomson, Niedzwiedz, & Katikireddi, 2018). However, a number of other studies have suggested a divergent picture, as health inequalities have remained or narrowed even during economic downturns (Hiyoshi et al., 2013; Khang et al., 2004; Liu, Hummer, 2008; Maheswaran et al., 2015; Sugisawa et al., 2016).
Finally, as the prior trends cover about two decades at maximum, they are not ideally suited for examining long-term changes in health inequalities and their period-specific individual level and macro-economic covariates.
Context and purpose
Our study represents Finnish adult men and women over a 36-year time period. Finland is a Nordic welfare state, with institutional welfare arrangements and universal social policies (Beckfield et al., 2015). Among European countries, inequalities in mortality in Finland have been relative large (Mackenbach et al., 2018), whereas inequalities in self-rated health have been intermediate (Hu, van Lenthe, Borsboom et al., 2016). The overall social and economic development for indicators like life expectancy and Gross Domestic Product (GDP) has been favourable during our study period (Statistics Finland, 2014a). The country, nevertheless, underwent two economic downturns, i.e. a labour market crisis in 1993–1994 and the global financial crisis in 2008–2009, which led to cuts in social services and benefits. Over the last few decades, employment participation in Finland has shown relative gender equality, as men and women have taken full-time jobs almost as often, and recessions have hit both genders in terms of high unemployment and worsening financial resources (Statistics Finland, 2014b). Thus, our study offers an interesting case study of long-term trends in health inequalities and their individual level covariates in a Nordic welfare state under economic and political pressures.
Our aim was, firstly, to examine 36-year trends in 1979–2014 in the magnitude of absolute and relative educational inequalities in self-rated health among Finnish adult men and women. Secondly, we aimed to examine the bearing of sociodemographic and health-related covariates on the inequalities and their trends over time.
Data and methods
Data sources
The data were derived from the study on Health Behaviour and Health among the Finnish Adult Population by the National Institute for Health and Welfare in Finland, collected annually in 1979–2014 using cross-sectional mail surveys (Helldán & Helakorpi, 2015). The data are representative of Finnish men and women aged 15–64. We included ages from 25 to 64 years. Participants below age 25 may not yet have completed their education. The upper age limit in the data is 65 years. The annual data were pooled to nine periods: 1979–1982, 1983–1986, 1987–1990, 1991–1994, 1995–1998, 1999–2002, 2003–2006, 2007–2010 and 2011–2014. The periodisation helps smoothen the annual random variation and allows the examination of economic fluctuations in Finland during 1979–2014. The period-specific number of respondents ranged from 8870 to 14235 (Table 1). Annual response rates varied among men from 44% to 83% and among women from 58% to 86%, with a declining trend over time (Helldán & Helakorpi, 2015). Identical questions were asked with minor deviations to allow reliable examination of temporal trends.
Table 1.
Number of participants, prevalence (%) of self-rated health (SRH) below good and average years of completed education in study periods.
| Period | N | SRH below good % | Average years of education | |
|---|---|---|---|---|
| Men | ||||
| 1979–1982 | 7428 | 40 | 9.6 | |
| 1983–1986 | 5707 | 38 | 10.1 | |
| 1987–1990 | 5820 | 39 | 10.7 | |
| 1991–1994 | 5344 | 36 | 11.4 | |
| 1995–1998 | 5354 | 36 | 11.8 | |
| 1999–2002 | 4976 | 37 | 12.4 | |
| 2003–2006 | 4902 | 38 | 12.9 | |
| 2007–2010 | 4445 | 35 | 13.2 | |
| 2011–2014 | 3842 | 34 | 13.8 | |
| Women | ||||
| 1979–1982 | 6807 | 39 | 9.6 | |
| 1983–1986 | 6380 | 36 | 10.4 | |
| 1987–1990 | 6470 | 36 | 11.0 | |
| 1991–1994 | 6119 | 31 | 11.8 | |
| 1995–1998 | 6086 | 33 | 12.3 | |
| 1999–2002 | 5893 | 33 | 13.0 | |
| 2003–2006 | 5882 | 34 | 13.5 | |
| 2007–2010 | 5686 | 34 | 14.0 | |
| 2011–2014 | 5028 | 32 | 14.5 | |
Measures
Our health outcome was self-rated health (SRH), measured by a question asking whether the respondent's current health status is good, fairly good, average, fairly poor or poor. Following common practice, we collapsed categories poor, fairly poor and average to indicate less-than-good self-rated health (Mackenbach et al., 2018; Subramanian, Huijts, & Avendano, 2010). Self-rated health is a broad measure of ill health and health-related well-being, much used in population studies (Manderbacka, 1998).
Our socioeconomic indicator was education measured by years of completed education. For background information we categorised education into thirds and in the main analyses we used years of education as a continuous variable. Education is a key indicator of socioeconomic position, which forms an ordinal scale, and can be assigned to each person irrespective of employment status (Lynch, Kaplan, 2000; Galobardes, Shaw, Lawlor, Lynch, & Davey Smith, 2006; Lahelma, 2010). Education is typically completed by early adulthood and it contributes to occupational class and income. Average years of education increased among men from 9.6 years in period 1979–1982 to 13.8 years in period 2011–2014 and among women from 9.6 to 14.5 years (Table 1).
Covariates
We included individual-level time-variant sociodemographic and health-related covariates as they have been associated with health inequalities in previous trend studies (Dieker et al., 2019; Granström et al., 2015; Moor et al., 2018; Sugisawa et al., 2016). Marital status was categorised into married including cohabiting, unmarried, divorced and separated, employment status into employed, unemployed, retirees and others, and region of residence into Southern Finland, Western Finland, Middle Finland, South-eastern Finland, Eastern Finland, and Northern Finland. Smoking was categorised into current daily smoking and non-smoking (not available for period 1979–1982), vegetable use into using fresh vegetables daily and less often during the past week, alcohol drinking into 8 units or more and less at one occasion among men and 5 units or more and less among women (not available for period 1979–1982), and body mass index (BMI) into below 25, 25–30 or above 30.
Statistical methods
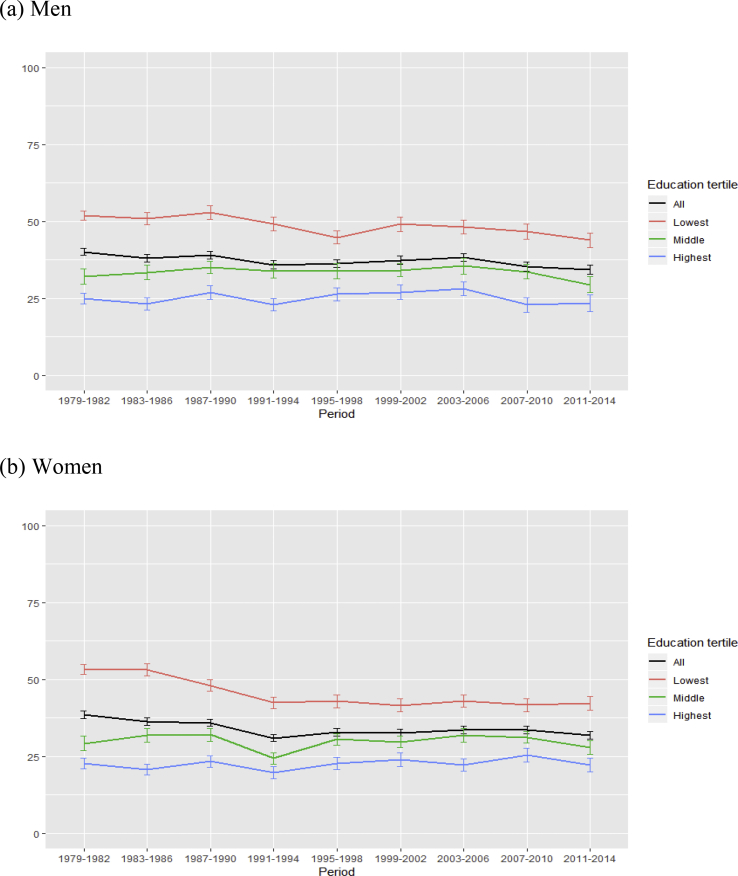
All analyses were stratified by gender as health and its background factors vary between men and women. For descriptive purposes we, firstly, calculated period-specific averages for the prevalence of less-than-good self-rated health (Table 1). Secondly, we classified years of education into tertiles and calculated for each tertile period-specific prevalence percentages of self-rated health with 95% confidence intervals (95% CI) (Fig. 1).
Fig. 1.
Prevalence (%) of less-than-good self-rated health with 95% confidence intervals by education tertile from period 1979–1982 to period 2011–2014, (a) men, (b) women (%).
The magnitude of educational inequalities in self-rated health was examined using the relative index of inequality (RII) and the slope index of inequality (SII) (Asada, 2010; King et al., 2012; Mackenbach, Kunst, 1997; Mackenbach, 2015; Moor et al., 2018). Both RII and SII are regression-based indices that take into account both the steepness of the gradient and the sizes of the groups compared. Years of education were converted to a relative rank indicator by taking the midpoint of the range in the cumulative distribution at that level of education. RII measures the magnitude of relative inequalities and reflects the prevalence ratio. RII was calculated with log-binomial regression models by using the rank indicator as an independent variable (Ernstsen, Strand, Nilsen, Espnes, & Krokstad, 2012). RII values above 1.0 indicate inequalities, and the higher the value, the larger the relative inequalities. SII measures the magnitude of absolute inequalities and reflects the prevalence difference. SII was calculated with binomial regression models with identity link function. SII values above 0.0 indicate inequalities, and the higher the value, the larger the absolute inequalities. RII and SII values and their 95% confidence intervals were calculated for each period.
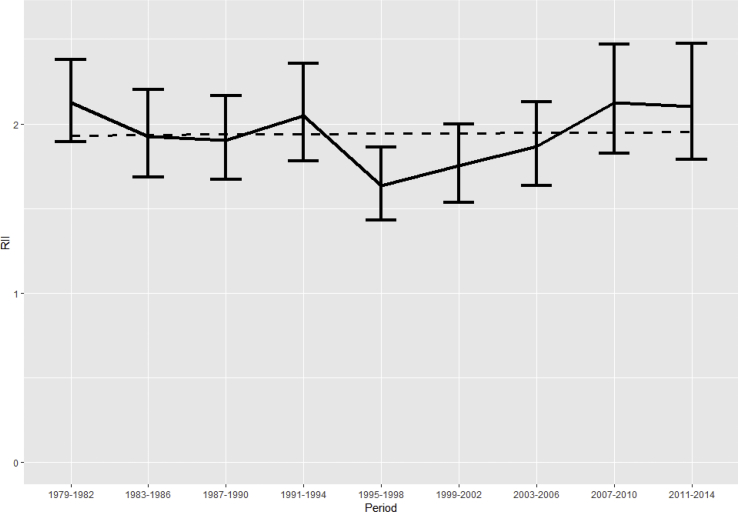
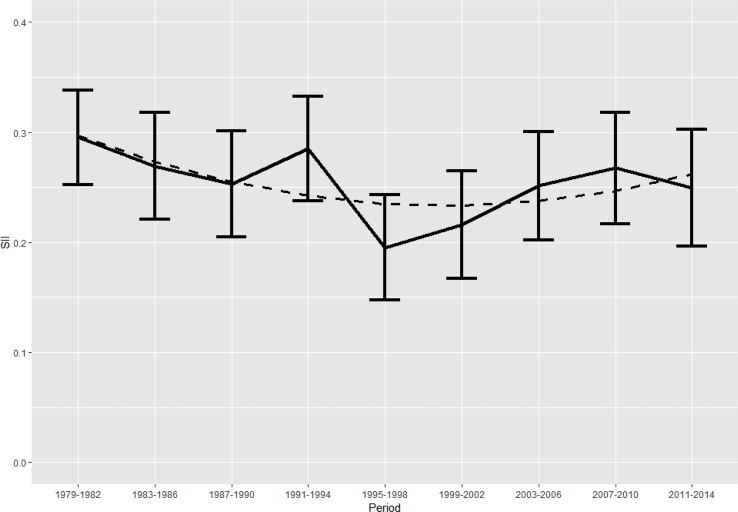
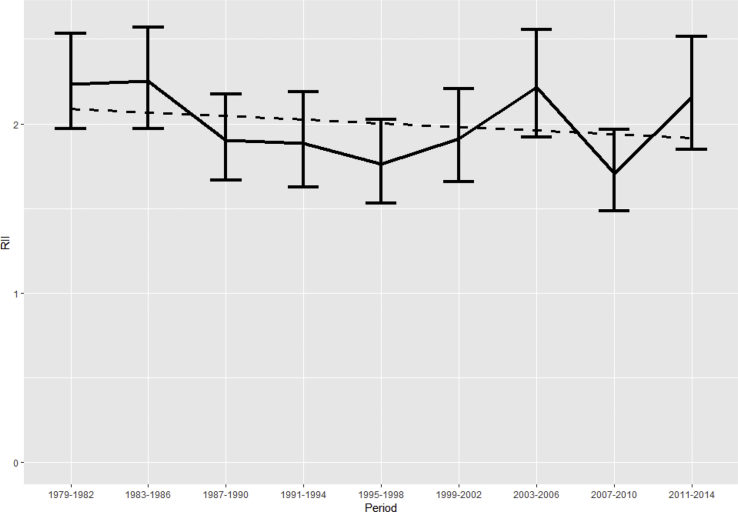
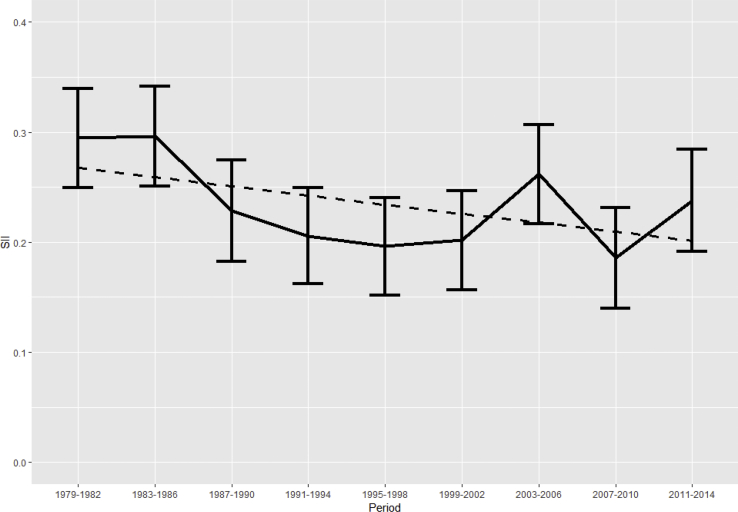
Firstly, Fig. 2, Fig. 3 present the age adjusted RII values and Fig. 4, Fig. 5 the age adjusted SII values for each period, men and women separately (solid line). Secondly, models were fitted adjusting for age and each covariate, one at a time, and the effects of the adjustments are reported in the text. The precise point estimates for RII and SII values, adjusted for each covariate with 95% confidence intervals, can be found in Appendix A, Appendix A. Thirdly, we fitted linear trend lines for the whole 36-year period to see the overall development of health inequalities. The linear trends are reported in Fig. 2, Fig. 3, Fig. 4, Fig. 5 (dashed line) and p-values for the slope being non-zero are given in the text. We also checked the curvilinearity of the trends and report this in the Results.
Fig. 2.
Relative educational inequalities in self-rated health among Finnish men aged 25–64 from period 1979–1982 to period 2011–2014. Relative Index of Inequality (RII) and 95% confidence intervals adjusted for age (solid line), and linear trend line (dashed line).
Fig. 3.
Absolute educational inequalities in self-rated health among Finnish men aged 25–64 from period 1979–1982 to period 2011–2014. Slope Index of Inequality (SII) and 95% % confidence intervals adjusted for age (solid line), and linear trend line (dashed line).
Fig. 4.
Relative educational inequalities in self-rated health among Finnish women aged 25–64 from period 1979–1982 to period 2011–2014. Relative Index of Inequality (RII) and 95% confidence intervals adjusted for age (solid line), and linear trend line (dashed line).
Fig. 5.
Absolute educational inequalities in self-rated health among Finnish women aged 25–64 from period 1979–1982 to period 2011–2014. Slope Index of Inequality (SII) and 95% confidence intervals adjusted for age (solid line), and linear trend line (dashed line).
Results
The overall prevalence of less-than-good self-rated health over 36-years from period 1979–1982 to period 2011–2014 declined steadily from 40% to 34% among men and from 39% to 32% among women (Table 1, Fig. 1). The decline was primarily due to the first half of the study period when less-than-good self-rated health declined most in the lowest education tertile and more so among women than men.
Health inequalities among men
Among men, the magnitude of relative educational inequalities in less-than-good self-rated health, measured by the relative index of inequality (RII), suggested a stable linear overall trend (p = 0.922) for the whole 36-year study period (Fig. 2, dashed line). However, there was variation in the age-adjusted RII values among the nine study periods (solid line). The overall trend showed slight curvilinearity and the model including curvilinearity was somewhat better than the linear model (p = 0.006). During the four first periods in 1979–1994, the RII values remained relatively stable between 1.90 (95% CI 1.67–2.16) and 2.12 (1.89–2.38) (Appendix 1). In period 1995–1998, immediately after the 1993–1994 recession in Finland, relative health inequalities narrowed by 40% to the lowest RII value 1.63 (1.43–1.86). After the narrowing, relative health inequalities widened again and peaked at RII value 2.12 (1.83–2.47) in period 2007–2010 when the global financial crisis burst out in 2008–2009.
Adjusting for each covariate one at a time did not change the age-adjusted period-specific pattern. Except for alcohol use, all other covariates reduced the magnitude of relative inequalities throughout the nine study periods. Vegetable use reduced the inequalities most, i.e. by 24%–40%, followed by employment status and smoking.
Absolute inequalities in self-rated health, measured by the slope index of inequality (SII), suggested also a stable linear overall trend (p = 0.317) for the whole study period, with no curvilinearity (Fig. 3, dashed line). The period-specific pattern for absolute inequalities among men was similar to that for relative inequalities (solid line). The first four periods again showed relative stability with SII values between 0.25 (0.20–0.30) and 0.29 (0.25–0.34) (Appendix 1). In the immediate post-recession period 1995–1998 absolute health inequalities declined by 32% to the lowest SII value 0.19 (0.15–0.24). After that, health inequalities widened again to the pre-recession level.
Also for absolute inequalities, adjusting for each covariate one at a time reduced the magnitude of inequalities but did not affect the period-specific pattern. Vegetable use reduced most the absolute inequalities, i.e. by 21%–26%, followed by employment status and smoking.
Health inequalities among women
Among women as among men, the magnitude of relative educational inequalities in self-rated health suggested a stable linear overall trend (p = 0.471) for the whole study period, with no curvilinearity (Fig. 4, dashed line). However, the period-specific variation differed from men as for women there was no immediate decline in relative inequalities after the 1993–1994 recession (solid line). Instead, there was a 38% gradual narrowing of inequalities during the five first periods from 1979-1982 (RII 2.5, 1.97–2.53) to 1995–1998 (RII 1.76, 1.53–2.02) (Appendix 2). After that, relative inequalities widened and peaked in 2003–2006 with RII value 2.22 (1.92–2.56), followed by an immediate 42% narrowing during the financial crisis period 2007–2010, and a final widening.
Adjusting for covariates reduced the magnitude of relative inequalities but did not affect the period-specific pattern. For women BMI reduced the inequalities most, i.e. by up to 42%, and employment status and smoking led to smaller reductions in the later study periods, in particular.
Like among men, also among women, absolute inequalities in self-rated health suggested a stable linear trend (p = 0.132) for the whole study period (Fig. 5, dashed line). The overall trend showed slight curvilinearity and the model including curvilinearity was somewhat better than the linear model (p = 0.027). The period-specific pattern in absolute inequalities followed that for relative inequalities among women (solid line), with inequalities narrowing by 31% during the six periods from 1979-1982 (SII 0.29, 0.25–0.34) to 1999–2002 (0.20, 0.16–0.25) (Appendix 2). After that, inequalities widened, followed by an immediate 27% narrowing in the financial crisis period 2007–2010, and a final widening.
Adjustments again reduced the magnitude but did not contribute to the patterning of absolute inequalities. Adjusting for BMI, employment status and vegetable use reduced each inequalities by up to 20%.
Discussion
We examined the magnitude of relative and absolute educational inequalities in self-rated health among Finnish men and women over a 36-year study period. Our main findings were:
1. Linear trends over 36 years confirmed that clear relative and absolute health inequalities persisted over the whole study period among men as well as women. Overall, the trends suggested that inequalities remained stable over time.
2. Among men, the period-specific pattern was largely similar for both relative and absolute health inequalities. The conspicuous finding was a sudden narrowing of inequalities after deep economic recession in Finland peaking in 1993–1994.
4. Also among women, the period-specific pattern in both relative and absolute health inequalities was similar, but differed from men. The conspicuous finding was a sudden narrowing of inequalities during the global financial crisis period in 2007–2010.
5. Adjusting for sociodemographic and health-related covariates, in particular, vegetable use, BMI and employment status, reduced the magnitude of absolute and relative health inequalities largely in a similar way across the nine study periods.
Interpretation and comparison
Prior evidence confirms inequalities in self-rated health among national populations at least since the 1970s (Townsend, Davidson, 1982, Mackenbach et al., 2018). However, the evidence derives from 10-20-year trends compared to our 36-year trend. In a couple of countries, relative health inequalities have widened somewhat, whereas in most countries absolute inequalities have remained largely unchanged, with no country showing clearly narrowing inequalities (Hiyoshi et al., 2013; Hu, van Lenthe, Borsboom et al., 2016; Khang et al., 2004; Kondo, Subramanian, Kawachi, Takeda, & Yamagata, 2008; Maheswaran et al., 2015; Moor et al., 2018; Sugisawa et al., 2016). Our study suggests that in Finland the prior findings can be extended to cover a trend up to 36 years.
During our study period, two major economic recessions took place and these shaped the trends in health inequalities. The 1993–1994 recession in Finland led to a sudden decline in relative and absolute health inequalities among men, but not among women. The 2008–2009 global financial crisis, in turn, led to a sudden decline in relative and absolute health inequalities among women, but not among men. After the recessions, inequalities returned to the pre-recession level. One might have expected financially hard times to widen health inequalities, but our evidence points to the opposite. A number of earlier studies have equally shown narrowing health inequalities during economic downturns (Valkonen et al., 2000; Kondo et al., 2008; Hiyoshi et al., 2013; Sugisawa et al., 2016, Mackenbach et al., 2018; Thomson et al., 2018; van der Wel, Saltkjel, Chen, Dahl, & Halvorsen, 2018). However, our evidence is not fully consistent as during the first recession only men's health inequalities narrowed, whereas during the second recession only women's inequalities narrowed.
Our analyses adjusted for individual-level time-variant sociodemographic and health-related covariates. These reduced both relative and absolute health inequalities by about 20–40%. The largest reductions were due to vegetable use among men and BMI among women. Employment status, and further health behaviours also reduced the inequalities, except for alcohol, which showed no effects or minimal widening. The negligible effects of alcohol may be due to difficulties in capturing alcohol use and its socioeconomic differences by survey measurement (Tolonen et al., 2010). Using register data, alcohol related causes accounted for a substantial part of inequalities in mortality, in particular, among Finnish men (Östergren, Martikainen, Tarkiainen, Elstad, & Brønnum-Hansen, 2019).
Our covariates reduced the magnitude of health inequalities in a similar way throughout the nine study periods and thus did not unravel any mechanisms behind the period-specific patterning of the inequalities and their gender differences. Prior studies have included similar sociodemographic and health-related covariates; these have equally reduced but not abolished health inequalities (Dieker et al., 2019; Granström et al., 2015; Maheswaran et al., 2015; Moor et al., 2018). In addition to the studied covariates, residual confounding is possible due to unmeasured covariates, such as housing, social support and working conditions (Dieker et al., 2019; Moor, Spallek, & Richter, 2017).
Like many prior trend studies, our study was also on educational inequalities in health. We used years of education as a continuous variable in the analyses. Compared to discrete educational classes, continuous education is advantageous as it allows a more sensitive analysis of long-term trends in health inequalities. The length of education has increased substantially across countries, in our study by about 4 years over 36 years. Such expansion of education may affect the trends in health inequalities and their interpretation. Education may have lost significance, as educational expansion has proceeded. A diminishing health returns hypothesis of education suggests that education may be losing its significance for the promotion of health and preventing health inequalities. There is evidence supporting such a development, as older cohorts have been found to gain more health benefits from an additional year of education than younger cohorts (Delaruelle, Buffel, & Bracke, 2015).
Macro-economic fluctuations provide important backgrounds for health inequalities and this was suggested also by our findings, which were shaped by the two recessions. A proposed macro-economic assumption has been that recessions contribute to worsening health and widening inequalities (Edwards, 2008; Bacigalupe, Escolar-Pujolar, 2014). We checked further, how macro indicators might be related to the period-specific variation of health inequalities in Finland. Unemployment rate increased from prior 3%–6% up to 17% during the 1993–1994 recession, whereas during the 2008–2009 financial crisis it was 6%–8%, i.e. at a level similar to that before and after the crisis (Statistics Finland, 2014b). Gross Domestic Product (GDP) per capita has increased steadily, except for decreases during both downturns. Trends in income inequalities remained unaffected by the downturns and the GINI coefficients were stably below 22 until 1997, with a subsequent increase to stable 25–26 (Statistics Finland, 2015). In our study, health inequalities narrowed among men by 32%–40% during the first downturn and among women by 31%–38% during the second one, with a subsequent return to the pre-recession level. Thus, the macro-economic indicators were not systematically associated with the trends in health inequalities in Finland. Instead, during the two downturns health inequalities narrowed and no widening was observed. The Finnish picture is in accordance to a European study across types of welfare regime, which examined trends in absolute and relative inequalities in self-rated health, and whether unemployment, GDP and GINI coefficients would affect the inequalities (Leão, Campos-Matos, Bambra, Russo, & Perelman, 2018). However, the effects were minor and the three macro-economic factors did not explain the trends in health inequalities.
Potential reasons for narrowing inequalities, instead of widening, during recessions include a drop in smoking, drinking, work strain, accidents and cardiovascular diseases that concern disproportionately the lower educated (Edwards, 2008; Valkonen et al., 2000). The reasons suggested for widening inequalities during recessions include austerity, poverty, lack of social protection and services (Hiyoshi et al., 2013; Bacigalupe, Escolar-Pujolar, 2014; Thomson et al., 2018). Country differences are potentially important as social and economic structures as well as health and welfare policies vary. Prior theoretical approaches have emphasised materialist, cultural-behavioural and psychosocial factors as determinants of health inequalities and their changes over time (Beckfield et al., 2015). We were able to examine individual level sociodemographic and behavioural factors as covariates for the trends of health inequalities. To have a fuller picture of the individual level factors these should be examined within the context of broader institutional arrangements in society. Welfare state policies and institutional arrangements, e.g. in the Nordic countries, may act as buffers against widening health inequalities as some studies suggest (Bacigalupe, Escolar-Pujolar, 2014; Edwards, 2008; Lahelma et al., 2002; Thomson et al., 2018; van der Wel et al., 2018).
While the evidence on the associations between economic downturns and health inequalities among men and women may seem mixed and even contradictory, it rather shows the complexity of the interplay between the micro and macro determinants in the production of health inequalities over longer periods. In our study, adjusting for vegetable use, BMI and employment status, in particular, narrowed health inequalities. Some other individual level determinants may contribute to widening inequalities, and in our analyses adjusting for alcohol use showed minor signs for wider health inequalities. It has been suggested that macro determinants, like recessions, may initially lead to narrowing health inequalities, but subsequent austerity may turn the trend to widening (Thomson et al., 2018; van der Wel et al., 2018). With regard to the complex production of health inequalities, it is unlikely that any single explanation would be suitable for different populations and their spatial and temporal contexts.
Methodological considerations
A major advantage of our study was the 36-year period allowing relative and absolute health inequalities to be examined using similar annual surveys with similar methods and data representative of Finnish adults.
The opposite side of the long study period is that there was a secular downward trend in the participation rate from round 80% to round 50%. To assess the potential effect of increasing non-response on the trends in self-rated health, we calculated adjusted weights for each study year based on age and gender distribution in the corresponding national population. However, the weighted self-rated health prevalence was throughout only slightly lower than the non-weighted prevalence, and weighting did not contribute to the magnitude of differences in self-rated health by education and gender. Thus, weighting was not used in our analyses of relative and absolute health inequalities. Prior analyses of these data have shown that young people, men, lower educated and those with poor health are overrepresented among the non-respondents (Tolonen et al., 2006,Tolonen et al., 2010). While non-response is a source of bias, its effects are likely conservative and the health inequalities reported in our study may be an underestimate.
We used self-rated health indicator, which may be susceptible to reporting bias. However, the indicator is well established, commonly used and recommended by the WHO (de Bruin, Picavet, & Nossikov, 1996; Subramanian et al., 2010). It has proven reliable and valid, predicting subsequent disability retirement and mortality (Lundberg, Manderbacka, 1996; Burström, Fredlund, 2001; Pietiläinen et al., 2011) . Further health indicators, in particular more objective ones, would have strengthened our study, but such were unavailable.
Our socioeconomic indicator was education, which reflects, in particular, non-material resources, cognitive capabilities as well as attitudes and values. Education is a well established and broad socioeconomic indicator, commonly used in studies on health inequalities. We lacked information on occupational class and income, which is a limitation, but education is correlated with these two other socioeconomic indicators. Further limitations include that education is attained by early adulthood and does not indicate directly the current socioeconomic position, and that early life health may influence later educational attainment (Lynch, Kaplan, 2000; Galobardes et al., 2006; Lahelma, 2010).
Conclusions
Relative and absolute educational inequalities in self-rated health remained during the whole 36-year study period. Adjusting for individual level covariates, including health behaviours and employment status, reduced the health inequalities throughout the study period. Among men, inequalities narrowed suddenly after the 1993–1994 recession and, among women, a similar narrowing took place during the 2008–2009 recession. However, health inequalities widened soon back to the pre-recession level. Despite the variations in the association between education and health, health inequalities remained even during recession periods and after considering the covariates.
Future trend studies would benefit from even longer study periods, further covariates, such as material and work-related factors, as well as objective health indicators. An updated comparative picture of long-term trends in health inequalities is equally needed. Macro-economic and labour market fluctuations should be systematically analysed as potential reasons for health inequalities. Finally, designs allowing causal analysis of proximal and distal reasons would add our understanding of the complex production of trends in health inequalities.
The perseverance of the trends calls for powerful policies to stop and narrow health inequalities. International and national health programmes have suggested many micro and macro level measures for promoting egalitarian health development and public health at large.
Ethical considerations
No formal ethical approval is available for our study. The work done is secondary analysis of survey data collected by the Finnish National Institute for Health and Welfare. We have no access to original data. Individuals cannot be identified in the data. All analyses are made at the group level. We follow ethical guidelines of ICMJE, STROBE and University of Helsinki, as well as Finnish data protection legislation. There are no conflicts of interest. All co-authors have contributed substantially to the study and its reporting.
Funding
Ossi Rahkonen was supported by Academy of Finland, grant number 1294514. The funding source has had no involvement in the preparation of the study.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2019.100504.
Contributor Information
Eero Lahelma, Email: eero.lahelma@helsinki.fi.
Olli Pietiläinen, Email: olli.k.pietilainen@helsinki.fi.
Oona Pentala-Nikulainen, Email: oona.pentala-nikulainen@stat.fi.
Satu Helakorpi, Email: satu.helakorpi@thl.fi.
Ossi Rahkonen, Email: ossi.rahkonen@helsinki.fi.
Appendix 1. Men. Period-specific estimates for relative index of inequality (RII) and slope index of inequality (SII) with 95% confidence intervals (95% CI). (a) Age-adjusted models and (b) models adjusting for age and each covariate, one at a time
| Model |
Period |
RII |
95% CI low high |
|
|---|---|---|---|---|
| RII, men | ||||
| (a) | ||||
| Age | 1979–1982 | 2.12 | 1.89 | 2.38 |
| Age | 1983–1986 | 1.93 | 1.68 | 2.20 |
| Age | 1987–1990 | 1.90 | 1.67 | 2.16 |
| Age | 1991–1994 | 2.05 | 1.78 | 2.36 |
| Age | 1995–1998 | 1.63 | 1.43 | 1.86 |
| Age | 1999–2002 | 1.75 | 1.53 | 2.00 |
| Age | 2003–2006 | 1.87 | 1.63 | 2.13 |
| Age | 2007–2010 | 2.12 | 1.83 | 2.47 |
| Age | 2011–2014 | 2.10 | 1.79 | 2.47 |
| (b) | ||||
| Marital status | 1979–1982 | 2.06 | 1.83 | 2.31 |
| Marital status | 1983–1986 | 1.87 | 1.63 | 2.14 |
| Marital status | 1987–1990 | 1.85 | 1.62 | 2.11 |
| Marital status | 1991–1994 | 1.98 | 1.72 | 2.28 |
| Marital status | 1995–1998 | 1.56 | 1.37 | 1.78 |
| Marital status | 1999–2002 | 1.68 | 1.47 | 1.92 |
| Marital status | 2003–2006 | 1.80 | 1.57 | 2.04 |
| Marital status | 2007–2010 | 2.00 | 1.72 | 2.33 |
| Marital status | 2011–2014 | 1.97 | 1.68 | 2.32 |
| Employment status | 1979–1982 | 1.95 | 1.74 | 2.19 |
| Employment status | 1983–1986 | 1.77 | 1.55 | 2.03 |
| Employment status | 1987–1990 | 1.70 | 1.49 | 1.94 |
| Employment status | 1991–1994 | 1.82 | 1.58 | 2.10 |
| Employment status | 1995–1998 | 1.50 | 1.32 | 1.71 |
| Employment status | 1999–2002 | 1.58 | 1.39 | 1.81 |
| Employment status | 2003–2006 | 1.63 | 1.43 | 1.86 |
| Employment status | 2007–2010 | 1.82 | 1.56 | 2.11 |
| Employment status | 2011–2014 | 1.88 | 1.601 | 2.21 |
| Region of residence | 1979–1982 | 2.08 | 1.85 | 2.34 |
| Region of residence | 1983–1986 | 1.89 | 1.65 | 2.16 |
| Region of residence | 1987–1990 | 1.88 | 1.65 | 2.14 |
| Region of residence | 1991–1994 | 2.02 | 1.75 | 2.32 |
| Region of residence | 1995–1998 | 1.59 | 1.39 | 1.81 |
| Region of residence | 1999–2002 | 1.74 | 1.52 | 1.99 |
| Region of residence | 2003–2006 | 1.84 | 1.61 | 2.11 |
| Region of residence | 2007–2010 | 2.06 | 1.77 | 2.40 |
| Region of residence | 2011–2014 | 2.02 | 1.72 | 2.38 |
| Smoking | 1979–1982 | NA | ||
| Smoking | 1983–1986 | 1.84 | 1.61 | 2.11 |
| Smoking | 1987–1990 | 1.78 | 1.57 | 2.03 |
| Smoking | 1991–1994 | 1.96 | 1.70 | 2.25 |
| Smoking | 1995–1998 | 1.55 | 1.36 | 1.76 |
| Smoking | 1999–2002 | 1.61 | 1.41 | 1.84 |
| Smoking | 2003–2006 | 1.75 | 1.53 | 2.00 |
| Smoking | 2007–2010 | 1.90 | 1.64 | 2.21 |
| Smoking | 2011–2014 | 1.88 | 1.60 | 2.21 |
| Alcohol drinking | 1979–1982 | NA | ||
| Alcohol drinking | 1983–1986 | 1.98 | 1.73 | 2.26 |
| Alcohol drinking | 1987–1990 | 1.94 | 1.71 | 2.21 |
| Alcohol drinking | 1991–1994 | 2.07 | 1.80 | 2.38 |
| Alcohol drinking | 1995–1998 | 1.67 | 1.47 | 1.91 |
| Alcohol drinking | 1999–2002 | 1.81 | 1.58 | 2.07 |
| Alcohol drinking | 2003–2006 | 1.89 | 1.66 | 2.16 |
| Alcohol drinking | 2007–2010 | 2.15 | 1.85 | 2.50 |
| Alcohol drinking | 2011–2014 | 2.12 | 1.80 | 2.49 |
| Physical activity | 1979–1982 | 1.94 | 1.73 | 2.18 |
| Physical activity | 1983–1986 | 1.84 | 1.60 | 2.10 |
| Physical activity | 1987–1990 | 1.71 | 1.50 | 1.94 |
| Physical activity | 1991–1994 | 1.90 | 1.66 | 2.19 |
| Physical activity | 1995–1998 | 1.52 | 1.34 | 1.73 |
| Physical activity | 1999–2002 | 1.59 | 1.39 | 1.81 |
| Physical activity | 2003–2006 | 1.62 | 1.43 | 1.85 |
| Physical activity | 2007–2010 | 1.85 | 1.60 | 2.15 |
| Physical activity | 2011–2014 | 1.75 | 1.50 | 2.04 |
| Vegetable use | 1979–1982 | 1.85 | 1.64 | 2.08 |
| Vegetable use | 1983–1986 | 1.67 | 1.45 | 1.92 |
| Vegetable use | 1987–1990 | 1.68 | 1.47 | 1.92 |
| Vegetable use | 1991–1994 | 1.76 | 1.52 | 2.03 |
| Vegetable use | 1995–1998 | 1.38 | 1.20 | 1.58 |
| Vegetable use | 1999–2002 | 1.56 | 1.36 | 1.79 |
| Vegetable use | 2003–2006 | 1.62 | 1.41 | 1.87 |
| Vegetable use | 2007–2010 | 1.80 | 1.54 | 2.10 |
| Vegetable use | 2011–2014 | 1.69 | 1.43 | 1.99 |
| BMI | 1979–1982 | 2.07 | 1.84 | 2.32 |
| BMI | 1983–1986 | 1.85 | 1.62 | 2.12 |
| BMI | 1987–1990 | 1.77 | 1.55 | 2.01 |
| BMI | 1991–1994 | 1.92 | 1.67 | 2.21 |
| BMI | 1995–1998 | 1.52 | 1.34 | 1.73 |
| BMI | 1999–2002 | 1.63 | 1.43 | 1.86 |
| BMI | 2003–2006 | 1.66 | 1.46 | 1.89 |
| BMI | 2007–2010 | 1.83 | 1.58 | 2.13 |
| BMI | 2011–2014 | 1.75 | 1.50 | 2.05 |
|
| ||||
|
Model |
Period |
SII |
95% CI low high |
|
|
SII, men |
||||
| (a) | ||||
| Age | 1979–1982 | 0.29 | 0.25 | 0.34 |
| Age | 1983–1986 | 0.27 | 0.22 | 0.32 |
| Age | 1987–1990 | 0.25 | 0.20 | 0.30 |
| Age | 1991–1994 | 0.28 | 0.24 | 0.33 |
| Age | 1995–1998 | 0.19 | 0.15 | 0.24 |
| Age | 1999–2002 | 0.22 | 0.17 | 0.26 |
| Age | 2003–2006 | 0.25 | 0.20 | 0.30 |
| Age | 2007–2010 | 0.27 | 0.22 | 0.32 |
| Age | 2011–2014 | 0.25 | 0.20 | 0.30 |
| (b) | ||||
| Marital status | 1979–1982 | 0.28 | 0.24 | 0.32 |
| Marital status | 1983–1986 | 0.26 | 0.21 | 0.31 |
| Marital status | 1987–1990 | 0.24 | 0.20 | 0.29 |
| Marital status | 1991–1994 | 0.27 | 0.23 | 0.32 |
| Marital status | 1995–1998 | 0.18 | 0.14 | 0.23 |
| Marital status | 1999–2002 | 0.20 | 0.16 | 0.25 |
| Marital status | 2003–2006 | 0.23 | 0.18 | 0.28 |
| Marital status | 2007–2010 | 0.25 | 0.20 | 0.30 |
| Marital status | 2011–2014 | 0.24 | 0.18 | 0.29 |
| Employment status | 1979–1982 | 0.27 | 0.22 | 0.31 |
| Employment status | 1983–1986 | 0.23 | 0.18 | 0.28 |
| Employment status | 1987–1990 | 0.21 | 0.16 | 0.25 |
| Employment status | 1991–1994 | 0.23 | 0.18 | 0.28 |
| Employment status | 1995–1998 | 0.16 | 0.11 | 0.20 |
| Employment status | 1999–2002 | 0.17 | 0.12 | 0.22 |
| Employment status | 2003–2006 | 0.20 | 0.15 | 0.25 |
| Employment status | 2007–2010 | 0.21 | 0.16 | 0.27 |
| Employment status | 2011–2014 | 0.21 | 0.15 | 0.26 |
| Region of residence | 1979–1982 | 0.29 | 0.24 | 0.33 |
| Region of residence | 1983–1986 | 0.26 | 0.21 | 0.31 |
| Region of residence | 1987–1990 | 0.25 | 0.20 | 0.30 |
| Region of residence | 1991–1994 | 0.28 | 0.23 | 0.32 |
| Region of residence | 1995–1998 | 0.18 | 0.13 | 0.23 |
| Region of residence | 1999–2002 | 0.21 | 0.16 | 0.26 |
| Region of residence | 2003–2006 | 0.25 | 0.20 | 0.30 |
| Region of residence | 2007–2010 | 0.26 | 0.21 | 0.31 |
| Region of residence | 2011–2014 | 0.24 | 0.18 | 0.29 |
| Smoking | 1979–1982 | NA | ||
| Smoking | 1983–1986 | 0.24 | 0.19 | 0.29 |
| Smoking | 1987–1990 | 0.23 | 0.18 | 0.28 |
| Smoking | 1991–1994 | 0.26 | 0.21 | 0.30 |
| Smoking | 1995–1998 | 0.17 | 0.12 | 0.21 |
| Smoking | 1999–2002 | 0.19 | 0.14 | 0.24 |
| Smoking | 2003–2006 | 0.22 | 0.17 | 0.27 |
| Smoking | 2007–2010 | 0.23 | 0.17 | 0.28 |
| Smoking | 2011–2014 | 0.21 | 0.16 | 0.27 |
| Alcohol drinking | 1979–1982 | NA | ||
| Alcohol drinking | 1983–1986 | 0.28 | 0.23 | 0.33 |
| Alcohol drinking | 1987–1990 | 0.26 | 0.21 | 0.31 |
| Alcohol drinking | 1991–1994 | 0.29 | 0.24 | 0.34 |
| Alcohol drinking | 1995–1998 | 0.20 | 0.15 | 0.25 |
| Alcohol drinking | 1999–2002 | 0.22 | 0.17 | 0.27 |
| Alcohol drinking | 2003–2006 | 0.26 | 0.21 | 0.31 |
| Alcohol drinking | 2011–2014 | 0.25 | 0.20 | 0.30 |
| Physical activity | 1979–1982 | 0.27 | 0.23 | 0.31 |
| Physical activity | 1983–1986 | 0.25 | 0.20 | 0.30 |
| Physical activity | 1987–1990 | 0.23 | 0.19 | 0.28 |
| Physical activity | 1991–1994 | 0.27 | 0.21 | 0.32 |
| Physical activity | 1995–1998 | 0.19 | 0.14 | 0.23 |
| Physical activity | 1999–2002 | 0.20 | 0.15 | 0.25 |
| Physical activity | 2003–2006 | 0.22 | 0.17 | 0.26 |
| Physical activity | 2007–2010 | 0.24 | 0.19 | 0.29 |
| Physical activity | 2011–2014 | 0.22 | 0.17 | 0.27 |
| Vegetable use | 1979–1982 | 0.23 | 0.18 | 0.28 |
| Vegetable use | 1983–1986 | 0.20 | 0.15 | 0.25 |
| Vegetable use | 1987–1990 | 0.21 | 0.15 | 0.26 |
| Vegetable use | 1991–1994 | 0.23 | 0.18 | 0.28 |
| Vegetable use | 1995–1998 | 0.14 | 0.09 | 0.19 |
| Vegetable use | 1999–2002 | 0.17 | 0.12 | 0.22 |
| Vegetable use | 2003–2006 | 0.20 | 0.15 | 0.25 |
| Vegetable use | 2007–2010 | 0.21 | 0.15 | 0.26 |
| Vegetable use | 2011–2014 | 0.18 | 0.13 | 0.24 |
| BMI | 1979–1982 | 0.28 | 0.24 | 0.33 |
| BMI | 1983–1986 | 0.26 | 0.21 | 0.31 |
| BMI | 1987–1990 | 0.23 | 0.18 | 0.28 |
| BMI | 1991–1994 | 0.27 | 0.22 | 0.32 |
| BMI | 1995–1998 | 0.18 | 0.13 | 0.23 |
| BMI | 1999–2002 | 0.21 | 0.16 | 0.25 |
| BMI | 2003–2006 | 0.22 | 0.17 | 0.27 |
| BMI | 2007–2010 | 0.23 | 0.18 | 0.28 |
| BMI | 2011–2014 | 0.22 | 0.17 | 0.27 |
Appendix 2. Women. Period-specific estimates for relative index of inequality (RII) and slope index of inequality (SII) with 95% confidence intervals (95% CI). (a) Age-adjusted models and (b) models adjusting for age and each covariate, one at a time
| Model |
Period |
RII |
95% CI low high |
|
|---|---|---|---|---|
| RII, women | ||||
| (a) | ||||
| Age | 1979–1982 | 2.23 | 1.97 | 2.53 |
| Age | 1983–1986 | 2.25 | 1.97 | 2.57 |
| Age | 1987–1990 | 1.90 | 1.66 | 2.18 |
| Age | 1991–1994 | 1.89 | 1.63 | 2.19 |
| Age | 1995–1998 | 1.76 | 1.53 | 2.02 |
| Age | 1999–2002 | 1.91 | 1.66 | 2.20 |
| Age | 2003–2006 | 2.22 | 1.92 | 2.56 |
| Age | 2007–2010 | 1.71 | 1.48 | 1.96 |
| Age | 2011–2014 | 2.16 | 1.85 | 2.52 |
| (b) | ||||
| Marital status | 1979–1982 | 2.22 | 1.96 | 2.52 |
| Marital status | 1983–1986 | 2.25 | 1.97 | 2.57 |
| Marital status | 1987–1990 | 1.93 | 1.69 | 2.20 |
| Marital status | 1991–1994 | 1.92 | 1.65 | 2.22 |
| Marital status | 1995–1998 | 1.77 | 1.54 | 2.04 |
| Marital status | 1999–2002 | 1.91 | 1.65 | 2.20 |
| Marital status | 2003–2006 | 2.23 | 1.93 | 2.57 |
| Marital status | 2007–2010 | 1.70 | 1.48 | 1.96 |
| Marital status | 2011–2014 | 2.13 | 1.82 | 2.48 |
| Employment status | 1979–1982 | 2.00 | 1.75 | 2.25 |
| Employment status | 1983–1986 | 2.04 | 1.78 | 2.33 |
| Employment status | 1987–1990 | 1.72 | 1.50 | 1.97 |
| Employment status | 1991–1994 | 1.74 | 1.50 | 2.02 |
| Employment status | 1995–1998 | 1.58 | 1.37 | 1.82 |
| Employment status | 1999–2002 | 1.74 | 1.50 | 2.01 |
| Employment status | 2003–2006 | 1.96 | 1.70 | 2.26 |
| Employment status | 2007–2010 | 1.57 | 1.36 | 1.81 |
| Employment status | 2011–2014 | 1.89 | 1.62 | 2.21 |
| Region of residence | 1979–1982 | 2.15 | 1.89 | 2.44 |
| Region of residence | 1983–1986 | 2.19 | 1.91 | 2.51 |
| Region of residence | 1987–1990 | 1.86 | 1.62 | 2.13 |
| Region of residence | 1991–1994 | 1.87 | 1.61 | 2.17 |
| Region of residence | 1995–1998 | 1.72 | 1.50 | 1.98 |
| Region of residence | 1999–2002 | 1.88 | 1.63 | 2.17 |
| Region of residence | 2003–2006 | 2.23 | 1.93 | 2.57 |
| Region of residence | 2007–2010 | 1.71 | 1.48 | 1.97 |
| Region of residence | 2011–2014 | 2.10 | 1.80 | 2.46 |
| Smoking | 1979–1982 | NA | ||
| Smoking | 1983–1986 | 2.21 | 1.92 | 2.53 |
| Smoking | 1987–1990 | 1.90 | 1.66 | 2.18 |
| Smoking | 1991–1994 | 1.79 | 1.54 | 2.08 |
| Smoking | 1995–1998 | 1.69 | 1.46 | 1.95 |
| Smoking | 1999–2002 | 1.80 | 1.56 | 2.08 |
| Smoking | 2003–2006 | 2.11 | 1.82 | 2.43 |
| Smoking | 2007–2010 | 1.56 | 1.36 | 1.80 |
| Smoking | 2011–2014 | 2.09 | 1.79 | 2.45 |
| Alcohol drinking | 1979–1982 | NA | ||
| Alcohol drinking | 1983–1986 | 2.25 | 2.00 | 2.57 |
| Alcohol drinking | 1987–1990 | 1.90 | 1.66 | 2.18 |
| Alcohol drinking | 1991–1994 | 1.89 | 1.63 | 2.19 |
| Alcohol drinking | 1995–1998 | 1.73 | 1.51 | 2.00 |
| Alcohol drinking | 1999–2002 | 1.91 | 1.65 | 2.21 |
| Alcohol drinking | 2003–2006 | 2.20 | 1.91 | 2.54 |
| Alcohol drinking | 2007–2010 | 1.71 | 1.49 | 1.97 |
| Alcohol drinking | 2011–2014 | 2.16 | 1.85 | 2.52 |
| Physical activity | 1979–1982 | 2.21 | 1.95 | 2.51 |
| Physical activity | 1983–1986 | 2.23 | 1.95 | 2.55 |
| Physical activity | 1987–1990 | 1.81 | 1.58 | 2.07 |
| Physical activity | 1991–1994 | 1.88 | 1.62 | 2.18 |
| Physical activity | 1995–1998 | 1.73 | 1.51 | 1.99 |
| Physical activity | 1999–2002 | 1.81 | 1.57 | 2.09 |
| Physical activity | 2003–2006 | 2.05 | 1.79 | 2.36 |
| Physical activity | 2007–2010 | 1.61 | 1.41 | 1.83 |
| Physical activity | 2011–2014 | 2.05 | 1.76 | 2.37 |
| Vegetable use | 1979–1982 | 2.07 | 1.81 | 2.36 |
| Vegetable use | 1983–1986 | 2.08 | 1.81 | 2.39 |
| Vegetable use | 1987–1990 | 1.70 | 1.47 | 1.95 |
| Vegetable use | 1991–1994 | 1.67 | 1.43 | 1.95 |
| Vegetable use | 1995–1998 | 1.61 | 1.39 | 1.86 |
| Vegetable use | 1999–2002 | 1.75 | 1.51 | 2.03 |
| Vegetable use | 2003–2006 | 2.00 | 1.73 | 2.32 |
| Vegetable use | 2007–2010 | 1.58 | 1.36 | 1.82 |
| Vegetable use | 2011–2014 | 2.01 | 1.72 | 2.36 |
| BMI | 1979–1982 | 2.13 | 1.87 | 2.41 |
| BMI | 1983–1986 | 2.00 | 1.75 | 2.29 |
| BMI | 1987–1990 | 1.70 | 1.48 | 1.94 |
| BMI | 1991–1994 | 1.66 | 1.44 | 1.93 |
| BMI | 1995–1998 | 1.58 | 1.38 | 1.82 |
| BMI | 1999–2002 | 1.63 | 1.42 | 1.88 |
| BMI | 2003–2006 | 1.78 | 1.55 | 2.04 |
| BMI | 2007–2010 | 1.41 | 1.23 | 1.61 |
| BMI | 2011–2014 | 1.79 | 1.55 | 2.08 |
|
| ||||
|
Model |
Period |
SII |
95% CI low high |
|
|
SII, women |
||||
| (a) | ||||
| Age | 1979–1982 | 0.29 | 0.25 | 0.34 |
| Age | 1983–1986 | 0.30 | 0.25 | 0.34 |
| Age | 1987–1990 | 0.23 | 0.18 | 0.27 |
| Age | 1991–1994 | 0.21 | 0.16 | 0.25 |
| Age | 1995–1998 | 0.20 | 0.15 | 0.24 |
| Age | 1999–2002 | 0.20 | 0.16 | 0.25 |
| Age | 2003–2006 | 0.26 | 0.22 | 0.31 |
| Age | 2007–2010 | 0.19 | 0.14 | 0.23 |
| Age | 2011–2014 | 0.24 | 0.19 | 0.28 |
| (b) | ||||
| Marital status | 1979–1982 | 0.29 | 0.25 | 0.34 |
| Marital status | 1983–1986 | 0.31 | 0.25 | 0.35 |
| Marital status | 1987–1990 | 0.23 | 0.19 | 0.28 |
| Marital status | 1991–1994 | 0.21 | 0.16 | 0.25 |
| Marital status | 1995–1998 | 0.19 | 0.15 | 0.24 |
| Marital status | 1999–2002 | 0.20 | 0.15 | 0.24 |
| Marital status | 2003–2006 | 0.26 | 0.22 | 0.31 |
| Marital status | 2007–2010 | 0.18 | 0.14 | 0.23 |
| Marital status | 2011–2014 | 0.23 | 0.19 | 0.28 |
| Employment status | 1979–1982 | 0.26 | 0.21 | 0.30 |
| Employment status | 1983–1986 | 0.25 | 0.21 | 0.20 |
| Employment status | 1987–1990 | 0.18 | 0.14 | 0.23 |
| Employment status | 1991–1994 | 0.18 | 0.13 | 0.22 |
| Employment status | 1995–1998 | 0.15 | 0.11 | 0.20 |
| Employment status | 1999–2002 | 0.16 | 0.12 | 0.21 |
| Employment status | 2003–2006 | 0.21 | 0.17 | 0.26 |
| Employment status | 2007–2010 | 0.15 | 0.10 | 0.19 |
| Employment status | 2011–2014 | 0.20 | 0.15 | 0.24 |
| Region of residence | 1979–1982 | 0.29 | 0.24 | 0.33 |
| Region of residence | 1983–1986 | 0.29 | 0.24 | 0.33 |
| Region of residence | 1987–1990 | 0.22 | 0.17 | 0.27 |
| Region of residence | 1991–1994 | 0.21 | 0.162 | 0.25 |
| Region of residence | 1995–1998 | 0.19 | 0.14 | 0.23 |
| Region of residence | 1999–2002 | 0.20 | 0.15 | 0.24 |
| Region of residence | 2003–2006 | 0.26 | 0.22 | 0.31 |
| Region of residence | 2007–2010 | 0.18 | 0.14 | 0.23 |
| Region of residence | 2011–2014 | 0.23 | 0.18 | 0.28 |
| Smoking | 1979–1982 | NA | ||
| Smoking | 1983–1986 | 0.28 | 0.23 | 0.33 |
| Smoking | 1987–1990 | 0.22 | 0.17 | 0.27 |
| Smoking | 1991–1994 | 0.18 | 0.14 | 0.23 |
| Smoking | 1995–1998 | 0.18 | 0.13 | 0.22 |
| Smoking | 1999–2002 | 0.18 | 0.14 | 0.23 |
| Smoking | 2003–2006 | 0.24 | 0.20 | 0.29 |
| Smoking | 2007–2010 | 0.16 | 0.11 | 0.20 |
| Smoking | 2011–2014 | 0.22 | 0.18 | 0.27 |
| Alcohol drinking | 1979–1982 | NA | ||
| Alcohol drinking | 1983–1986 | 0.30 | 0.25 | 0.34 |
| Alcohol drinking | 1987–1990 | 0.23 | 0.18 | 0.27 |
| Alcohol drinking | 1991–1994 | 0.21 | 0.16 | 0.25 |
| Alcohol drinking | 1995–1998 | 0.19 | 0.15 | 0.24 |
| Alcohol drinking | 1999–2002 | 0.20 | 0.16 | 0.25 |
| Alcohol drinking | 2003–2006 | 0.26 | 0.21 | 0.31 |
| Alcohol drinking | 2007–2010 | 0.19 | 0.14 | 0.23 |
| Alcohol drinking | 2011–2014 | 0.24 | 0.19 | 0.28 |
| Physical activity | 1979–1982 | 0.29 | 0.25 | 0.34 |
| Physical activity | 1983–1986 | 0.29 | 0.25 | 0.34 |
| Physical activity | 1987–1990 | 0.23 | 0.18 | 0.27 |
| Physical activity | 1991–1994 | 0.21 | 0.17 | 0.25 |
| Physical activity | 1995–1998 | 0.20 | 0.15 | 0.24 |
| Physical activity | 1999–2002 | 0.21 | 0.16 | 0.25 |
| Physical activity | 2003–2006 | 0.25 | 0.21 | 0.29 |
| Physical activity | 2007–2010 | 0.19 | 0.14 | 0.23 |
| Physical activity | 2011–2014 | 0.22 | 0.18 | 0.27 |
| Vegetable use | 1979–1982 | 0.26 | 0.21 | 0.31 |
| Vegetable use | 1983–1986 | 0.26 | 0.21 | 0.30 |
| Vegetable use | 1987–1990 | 0.18 | 0.13 | 0.23 |
| Vegetable use | 1991–1994 | 0.17 | 0.12 | 0.21 |
| Vegetable use | 1995–1998 | 0.16 | 0.11 | 0.21 |
| Vegetable use | 1999–2002 | 0.18 | 0.13 | 0.22 |
| Vegetable use | 2003–2006 | 0.23 | 0.18 | 0.27 |
| Vegetable use | 2007–2010 | 0.15 | 0.11 | 0.20 |
| Vegetable use | 2011–2014 | 0.21 | 0.16 | 0.26 |
| BMI | 1979–1982 | 0.27 | 0.23 | 0.32 |
| BMI | 1983–1986 | 0.25 | 0.21 | 0.30 |
| BMI | 1987–1990 | 0.20 | 0.15 | 0.24 |
| BMI | 1991–1994 | 0.17 | 0.13 | 0.22 |
| BMI | 1995–1998 | 0.16 | 0.12 | 0.21 |
| BMI | 1999–2002 | 0.17 | 0.12 | 0.21 |
| BMI | 2003–2006 | 0.21 | 0.16 | 0.25 |
| BMI | 2007–2010 | 0.15 | 0.10 | 0.19 |
| BMI | 2011–2014 | 0.20 | 0.15 | 0.24 |
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Asada Y. On the choice of absolute or relative inequality measures. Milbank Q. 2010;88:616–622. doi: 10.1111/j.1468-0009.2010.00614.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bacigalupe A., Escolar-Pujolar A. The impact of economic crises on social inequalities in health: What do we know so far? International Journal for Equity in Health. 2014 25;13:52. doi: 10.1186/1475-9276-13-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckfield J., Bambra C., Eikemo T., Huijts T., McNamara C., Wendt C. An institutional theory of welfare state effects on the distribution of population health. Social Theory & Health. 2015;13:227–244. [Google Scholar]
- Bouchard L., Albertini M., Batista R., Montigny J. Research on health inequalities: A bibliometric analysis (1966-2014) Social Science & Medicine. 2015;141:100–108. doi: 10.1016/j.socscimed.2015.07.022. [DOI] [PubMed] [Google Scholar]
- Burström B., Fredlund P. Self rated health: Is it as good a predictor of subsequent mortality among adults in lower as well as in higher social classes? Journal of Epidemiology & Community Health. 2001;55:836–840. doi: 10.1136/jech.55.11.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Bruin A., Picavet H.S., Nossikov A., editors. Health interview surveys: Towards international harmonization of methods and instruments. WHO Regional Office for Europe; Copenhagen: 1996. http://www.who.int/iris/handle/10665/107328 [PubMed] [Google Scholar]
- Delaruelle K., Buffel V., Bracke P. Educational expansion and the education gradient in health: A hierarchical age-period-cohort analysis. Social Science & Medicine. 2015;145:79–88. doi: 10.1016/j.socscimed.2015.09.040. [DOI] [PubMed] [Google Scholar]
- Dieker A.C.M., IJzelenberg W., Proper K.I., Burdorf A., Ket J.C.F., van der Beek A.J. The contribution of work and lifestyle factors to socioeconomic inequalities in self-rated health? A systematic review. Scandinavian Journal of Work, Environment & Health. 2019;45:114–125. doi: 10.5271/sjweh.3772. [DOI] [PubMed] [Google Scholar]
- Edwards R. Who is hurt by procyclical mortality? Social Science & Medicine. 2008;67:2051–2058. doi: 10.1016/j.socscimed.2008.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernstsen L., Strand B.H., Nilsen S.M., Espnes G.A., Krokstad S. Trends in absolute and relative educational inequalities in four modifiable ischaemic heart disease risk factors: Repeated cross-sectional surveys from the Nord-Trøndelag health study (HUNT) 1984-2008. BMC Public Health. 2012;12:266. doi: 10.1186/1471-2458-12-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galobardes B., Shaw M., Lawlor D., Lynch J., Davey Smith G. Indicators of socioeconomic position (Part 1) Journal of Epidemiology & Community Health. 2006;60:7–12. doi: 10.1136/jech.2004.023531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granström F., Molarius A., Garvin P., Elo S., Feldman I., Kristenson M. Exploring trends in and determinants of educational inequalities in self-rated health. Scandinavian Journal of Public Health. 2015;43:677–686. doi: 10.1177/1403494815592271. [DOI] [PubMed] [Google Scholar]
- Heistaro S., Vartiainen E., Puska P. Trends in self-rated health in Finland 1972-1992. Preventive Medicine. 1996;25:625–632. doi: 10.1006/pmed.1996.0098. [DOI] [PubMed] [Google Scholar]
- Helldán A., Helakorpi S. National Institute for Health and Welfare; Helsinki: 2015. Health behaviour and health among the Finnish adult population, spring 2014. Report 6. [Google Scholar]
- Hiyoshi A., Fukuda Y., Shipley M., Brunner E. Inequalities in self-rated health in Japan 1986-2007 according to household income and a novel occupational classification: National sampling survey series. Journal of Epidemiology & Community Health. 2013;67:960–965. doi: 10.1136/jech-2013-202608. [DOI] [PubMed] [Google Scholar]
- Hu Y., van Lenthe F., Borsboom G., Looman C., Bopp M., Burström B.…Mackenbach J. Trends in socioeconomic inequalities in self-assessed health in 17 European countries between 1990 and 2010. Journal of Epidemiology & Community Health. 2016;70:644–652. doi: 10.1136/jech-2015-206780. [DOI] [PubMed] [Google Scholar]
- Hu Y., van Lenthe, Judge K., Lahelma E., Costa G., Mackenbach J.P. Did the English strategy reduce inequalities in health? A difference-in-difference analysis comparing England with three other European countries. BMC Public Health. 2016;16:865. doi: 10.1186/s12889-016-3505-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karanikolos M., Mladovsky P., Cylus J., Thomson S., Basu S., Stuckler D. Financial crisis, austerity, and health in Europe. Lancet. 2013;381:1323–1331. doi: 10.1016/S0140-6736(13)60102-6. [DOI] [PubMed] [Google Scholar]
- Khang Y.H., Lynch J., Yun S., Lee S.I. Trends in socioeconomic health inequalities in Korea: Use of mortality and morbidity measures. Journal of Epidemiology & Community Health. 2004;58:308–314. doi: 10.1136/jech.2003.012989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King N.B., Harper S., Young M.E. Use of relative and absolute effect measures in reporting health inequalities: Structured review. BMJ. 2012;345:e5774. doi: 10.1136/bmj.e5774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kondo N., Subramanian S.V., Kawachi I., Takeda Y., Yamagata Z. Economic recession and health inequalities in Japan: Analysis with a national sample 1986-2001. Journal of Epidemiology & Community Health. 2008;62:869–875. doi: 10.1136/jech.2007.070334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahelma E. Health and social stratification. In: Cockerham W., editor. The New Blackwell companion to medical Sociology. Wiley-Blackwell; Chichester: 2010. pp. 71–96. [Google Scholar]
- Lahelma E., Kivelä K., Roos E., Tuominen T., Dahl E., Diderichsen D.…Åberg Yngwe M. Analysing changes of health inequalities in the Nordic welfare states. Social Science & Medicine. 2002;55:609–625. doi: 10.1016/s0277-9536(01)00191-5. [DOI] [PubMed] [Google Scholar]
- Leão T., Campos-Matos I., Bambra C., Russo G., Perelman J. Welfare states, the Great Recession and health: Trends in educational inequalities in self-reported health in 26 European countries. PLoS One. 2018;13:e0193165. doi: 10.1371/journal.pone.0193165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Hummer R.A. Are educational differences in U.S. Self-rated health increasing?: An examination by gender and race. Social Science & Medicine. 2008;67:1898–1906. doi: 10.1016/j.socscimed.2008.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundberg O., Manderbacka K. Assessing reliability of a measure of self-rated health. Scandinavian Journal of Social Medicine. 1996;24:218–224. doi: 10.1177/140349489602400314. [DOI] [PubMed] [Google Scholar]
- Lynch J., Kaplan G. Socioeconomic position. In: Berkman L., Kawachi I., editors. Social epidemiology. Oxford University Press; New York: 2000. pp. 13–35. [Google Scholar]
- Mackenbach J. The persistence of health inequalities in modern welfare states: The explanation of a paradox. Social Science & Medicine. 2012;75:761–769. doi: 10.1016/j.socscimed.2012.02.031. [DOI] [PubMed] [Google Scholar]
- Mackenbach J. Should we aim to reduce relative or absolute inequalities in mortality? The European Journal of Public Health. 2015;25:185. doi: 10.1093/eurpub/cku217. [DOI] [PubMed] [Google Scholar]
- Mackenbach J., Kunst A. Measuring the magnitude of socio-economic inequalities in health: An overview of available measures illustrated with two examples from Europe. Social Science & Medicine. 1997;44:757–771. doi: 10.1016/s0277-9536(96)00073-1. [DOI] [PubMed] [Google Scholar]
- Mackenbach J., Valverde J.R., Artnik B., Bopp M., Brønnum-Hansen H., Deboosere P. Trends in health inequalities in 27 European countries. Proceedings of the National Academy of Sciences. 2018;115:6440–6445. doi: 10.1073/pnas.1800028115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maheswaran H., Kupek E., Petrou S. Self-reported health and socio-economic inequalities in England, 1996-2009: Repeated national cross-sectional study. Social Science & Medicine. 2015;136–137:135–146. doi: 10.1016/j.socscimed.2015.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manderbacka K. Examining what self-rated health question is understood to mean by respondents. Scandinavian Journal of Social Medicine. 1998;26:145–153. doi: 10.1177/14034948980260020301. [DOI] [PubMed] [Google Scholar]
- Moor I., Günther S., Knöchelmann A., Hoebel J., Pförtner T.K., Lampert T. Educational inequalities in subjective health in Germany from 1994 to 2014: A trend analysis using the German socio-economic panel study (GSOEP) BMJ Open. 2018;8:e019755. doi: 10.1136/bmjopen-2017-019755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moor I., Spallek J., Richter M. Explaining socioeconomic inequalities in self-rated health: A systematic review of the relative contribution of material, psychosocial and behavioural factors. Journal of Epidemiology & Community Health. 2017;71:565–575. doi: 10.1136/jech-2016-207589. [DOI] [PubMed] [Google Scholar]
- Ministry of Social Affairs and Health . Publications 16; Helsinki: 2008. National action plan to reduce health inequalities 2008-2011.http://julkaisut.valtioneuvosto.fi/bitstream/handle/10024/71185/Julk200825.pdf?sequence=1&isAllowed=y Accessed 24 April 2019. [Google Scholar]
- Östergren O., Martikainen P., Tarkiainen L., Elstad J.I., Brønnum-Hansen H. Contribution of smoking and alcohol consumption to income differences in life expectancy: Evidence using Danish, Finnish, Norwegian and Swedish register data. Journal of Epidemiology & Community Health. 2019 doi: 10.1136/jech-2018-211640. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palosuo H., Koskinen S., Lahelma E., Kostiainen E., Prättälä R., Martelin T., …Linnanmäki E., editors. Vol. 9. Ministry of Social Affairs and Health, Publications; Helsinki: 2009. Health inequalities in Finland. (Trends in socioeconomic health differences 1980-2005). [Google Scholar]
- Pietiläinen O., Laaksonen M., Rahkonen O., Lahelma E. Self-rated health as apredictor of disability retirement–the contribution of ill-health and working conditions. PLoS One. 2011;6 doi: 10.1371/journal.pone.0025004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahkonen O., Talala K., Sulander T., Laaksonen M., Lahelma E., Uutela A., Prättälä R. In: Socio-economic health inequalities and how they have changed. Palosuo H., editor. Ministry of Social Affairs and Health, Publications; Helsinki: 2009. pp. 61–69. [Google Scholar]
- Statistics Finland . Statistics Finland; Helsinki: 2014. Annual national accounts.http://www.stat.fi/til/vtp/2014/vtp_2014_2015-03-02_tie_001_en.html Accessed 24 April 2019. [Google Scholar]
- Statistics Finland . Statistics Finland; Helsinki: 2014. Employment and unemployment.http://www.stat.fi/til/tyti/2014/13/tyti_2014_13_2015-04-28_kat_002_en.html Accessed 24 April 2019. [Google Scholar]
- Statistics Finland . Statistics Finland; Helsinki: 2015. Total statistics on income distribution. Income inequality 2015.http://www.stat.fi/til/tjkt/2015/02/tjkt_2015_02_2016-12-20_tie_002_en.html Accessed 24 April 2019. [Google Scholar]
- Subramanian S.V., Huijts T., Avendano M. Self-reported health assessments in the 2002 world health survey: How do they correlate with education? Bulletin of the World Health Organization. 2010;88:131–138. doi: 10.2471/BLT.09.067058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugisawa H., Harada K., Sugihara Y., Yanagisawa S., Shinmei M. Socioeconomic status and self-rated health of Japanese people, based on age, cohort, and period. Population Health Metrics. 2016;14:27. doi: 10.1186/s12963-016-0095-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson R., Niedzwiedz C., Katikireddi V. Trends in gender and socioeconomic inequalities in mental health following the great recession and austerity: A repeat cross-sectional analysis of the health survey for England. BMJ Open. 2018;8:e022924. doi: 10.1136/bmjopen-2018-022924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolonen H., Helakorpi S., Talala K., Helasoja V., Martelin T., Prättälä R. 25-year trends and socio-demographic differences in response rates: Finnish adult health behaviour survey. European Journal of Epidemiology. 2006;21:409–415. doi: 10.1007/s10654-006-9019-8. [DOI] [PubMed] [Google Scholar]
- Tolonen H., Laatikainen T., Helakorpi S., Talala K., Martelin T., Prättälä R. Marital status, educational level and household income explain part of the excess mortality of survey non-respondents. European Journal of Epidemiology. 2010;25:69–76. doi: 10.1007/s10654-009-9389-9. [DOI] [PubMed] [Google Scholar]
- Townsend P., Davidson N. Penguin; London: 1982. Inequalities in health: The black report. [Google Scholar]
- Valkonen T., Martikainen P., Jalovaara M., Koskinen S., Martelin T., Mäkelä P. Changes in socioeconomic inequalities in mortality during an economic boom and recession among middle-aged men and women in Finland. The European Journal of Public Health. 2000;10:274–280. [Google Scholar]
- van der Wel K.A., Saltkjel T., Chen W.H., Dahl E., Halvorsen K. European health inequality through the “great recession”: Social policy matters. Sociology of Health & Illness. 2018;40:750–768. doi: 10.1111/1467-9566.12723. [DOI] [PubMed] [Google Scholar]
- WHO . Regional Office for Europe; Copenhagen: 1985. Targets for health for all. World health organization. [Google Scholar]
- WHO . World Health Organization; Geneva: 2008. Closing the gap in a generation: Health equity through action on the social determinants of health. Final report of the commission on social determinants of health.http://whqlibdoc.who.int/publications/2008/9789241563703_eng.pdf Accessed 24 April 2019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.