Introduction
Hydralazine is a commonly prescribed antihypertensive medication that has been associated with both drug-induced lupus erythematosus and vasculitis.1 There is significant clinical, histopathologic, and serologic overlap between these entities. We present an unusual case of hydralazine-induced autoimmune syndrome with elements of both drug-induced lupus and vasculitis, as well as Sweet syndrome–like cutaneous lesions with distinctive histopathologic cryptococcoid inflammatory cells.
Case report
A woman in her 70s with a history of hypertension, type 2 diabetes mellitus, remote bladder cancer with prior cystectomy and diversion complicated by ureteral stricture, and chronic kidney disease (stage III) presented to an outside institution with 2 weeks of joint pain, eye swelling, and discharge and blisters over her extremities and trunk. The patient's home medications included hydralazine, amlodipine, clonidine, aspirin, clopidogrel, furosemide, simvastatin, and insulin. Bacterial culture and viral polymerase chain reaction analysis of the eye exudate were unremarkable, although empiric valacyclovir was initiated. Other laboratory findings were significant for an elevated erythrocyte sedimentation rate (>100 mm/h; reference range, 0-30 mm/h) and C-reactive protein (108 mg/L; reference range, 0.0-7.4 mg/L), which, in the setting of her skin lesions, raised concern for a vasculitic process; oral steroids (prednisone 60 mg daily) were initiated. Failure of eye and skin symptoms to improve after 4 days of treatment prompted transfer of the patient to our institution.
At the time of transfer, the patient's vital signs were normal. Physical examination was notable for severe eyelid ectropion, edematous and umbilicated papules on the face, oral pseudobullae, and hemorrhagic bullous plaques on the arms and legs (Figs 1 and 2). There was also mild swelling of bilateral knee joints, but with no erythema or tenderness, as well as normal cardiac and lung examination findings. The patient continued taking oral prednisone pending further workup. Initial laboratory test results were significant for leukocytosis (white blood cell count of 15,600 leukocytes/μL), normocytic anemia (hemoglobin of 8.6 g/dL with mean corpuscular volume of 83 fL), and creatinine of 2.68 mg/dL. Urinalysis showed hematuria with no red blood cell casts; this was ultimately attributed to ureteral obstruction and inflammation rather than glomerulonephritis because the acute kidney injury resolved promptly after ureteral stent replacement, with creatinine down-trending to 1.24 mg/dL. Serum bacterial, mycobacterial, and fungal culture results were negative, as were results from specific tests for mycoplasma, herpes simplex, varicella zoster, Aspergillus, Cryptococcus, and histoplasma.
Fig 1.
Edematous umbilicated papules on the face with bilateral eyelid ectropion.
Fig 2.
Hemorrhagic bulla of the left thumb.
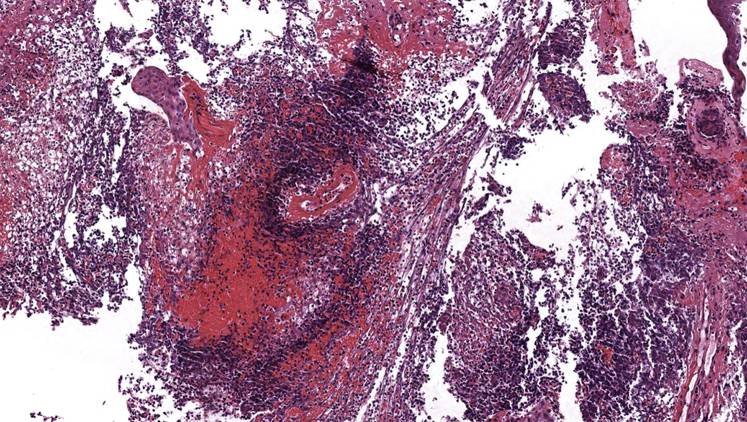
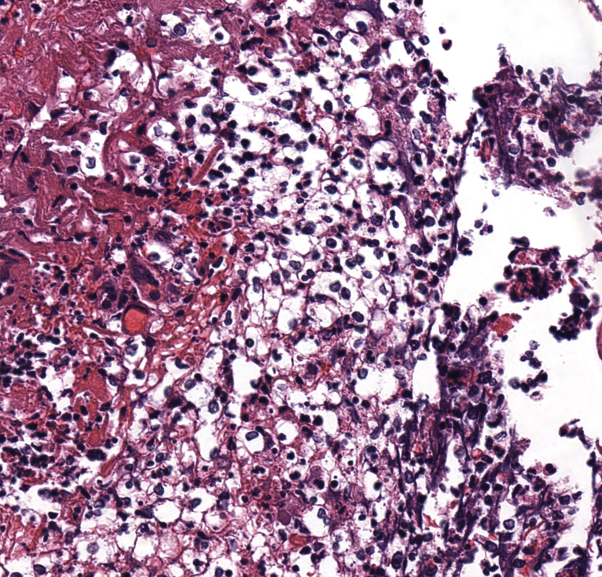
Skin biopsy of the cutaneous lesions showed a dense perivascular neutrophilic infiltrate with prominent fibrinoid necrosis, neutrophilic degeneration, and hemorrhage (Fig 3). Histopathology also showed small-appearing, morphologically unusual cells surrounded by vacuolated spaces resembling the characteristic polysaccharide capsule of Cryptococcus neoformans (Fig 4). However, the cells showed negative staining for periodic-acid Schiff, and the pseudocapsular spaces were negative for mucicarmine. Cytoplasmic staining with CD68 and myeloperoxidase (MPO) confirmed myeloid derivation. Tissue culture and direct immunofluorescence study results were negative.
Fig 3.
Dense perivascular neutrophilic inflammation with vascular destruction, fibrinoid necrosis, and leukocytoclasis (hematoxylin-eosin stain; original magnification: ×80).
Fig 4.
Cryptococcoid inflammatory debris (hematoxylin-eosin stain; original magnification: ×280).
Serologic analyses showed positive antinuclear (ANA) (titer, 1:320; reference range, <1:160), antihistone (6.2 U; reference range, 0.0-0.9 U), and anti-double stranded DNA (dsDNA) (210 IU/mL; reference range, 0-90 IU/mL) antibodies, as well as positive antineutrophil cytoplasmic antibodies with perinuclear accentuation (p-ANCA) and anti-MPO (37 U; reference range, 0-20 U) antibodies. Rheumatoid factor, anti-cyclic citrullinated peptide antibodies, cryoglobulins, anti-SSA/SSB antibodies, and anti-Smith antibodies were all negative.
Six days after initial presentation to our hospital, in the setting of positive autoantibodies and clinical and histopathologic features of autoimmune disease, medications were reviewed to identify a possible causative agent; hydralazine was subsequently discontinued. The patient was also started on high-dose intravenous steroids (solumedrol 500 mg daily) with flattening of the skin lesions and decrease in eyelid ectropion over the following week. No new lesions formed. The patient was discharged on an oral steroid taper (prednisone 60 mg daily).
Eight weeks after hospitalization, on a lower dose of oral prednisone, the patient's examination showed continued gradual resolution of the Sweet syndrome–like lesions, although with persistent, slowly healing ulcers over her distal aspect of the upper and lower extremities at the sites of prior hemorrhagic plaques. Shortly thereafter, however, we received notice that the patient had passed away at home. Given her previously steady improvement, the cause of death was deemed likely secondary to the patient's age and multiple other medical comorbidities rather than worsening of her drug-induced autoimmune disease.
Discussion
Hydralazine is associated with both drug-induced lupus and vasculitis. Hydralazine-induced lupus is both a more commonly reported (incidence of approximately 5%-10% per year of therapy) and more benign entity compared with hydralazine-induced vasculitis, which can present with severe pulmonary and renal involvement.2 As our patient exemplifies, considerable overlap exists between these 2 conditions.3 A history of joint pain and normocytic anemia, as well as positive ANA, anti-dsDNA, and anti-histone antibodies, are consistent with drug-induced lupus, whereas dermal vessel necrosis with positive p-ANCA and anti-MPO antibodies point toward drug-induced vasculitis. It is thought that hydralazine induces autoimmunity by accumulating in neutrophils and causing apoptosis, thus exposing normally sequestered cell antigens to the immune system and leading to the formation of various autoantibodies (ANA, anti-dsDNA, anti-histone, ANCA)4; this may explain the overlapping serologies seen in our patient.
Our patient also showed features of Sweet syndrome, with characteristic edematous rash and neutrophilic infiltrate on histopathology; vasculitis is rare in this condition. Sweet syndrome is a reactive phenomenon that can occur in the setting of infection, underlying malignancy, or medications. The presence of inflammatory debris mimicking Cryptococcus has been reported in the setting of both neutrophilic dermatoses (termed cryptococcoid Sweet5) and vasculitis.1,6 These unusual vacuolated spaces are thought to represent ballooning degeneration of neutrophils.6
Conclusion
We report a unique presentation of hydralazine-induced autoimmune syndrome with overlapping serologic features of both lupus and vasculitis in addition to a striking Sweet syndrome–like clinical presentation and potentially confusing Cryptococcus-like histopathologic findings.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Levin L.E., Magro C., Horowitz J., Harp J. Hydralazine-associated cutaneous vasculitis presenting with aerodigestive tract involvement. Cutis. 2017;99:E25–E29. [PubMed] [Google Scholar]
- 2.Yokogawa N., Vivino F.B. Hydralazine-induced autoimmune disease: comparison to idiopathic lupus and ANCA-positive vasculitis. Mod Rheumatol. 2009;19(3):338–347. doi: 10.1007/s10165-009-0168-y. [DOI] [PubMed] [Google Scholar]
- 3.Kumar B., Strouse J., Swee M., Lenert P., Suneja M. Hydralazine-associated vasculitis: overlapping features of drug-induced lupus and vasculitis. Semin Arthritis Rheum. 2018;48(2):283–287. doi: 10.1016/j.semarthrit.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 4.Jiang X., Khursigara G., Rubin R. Transformation of lupus-inducing drugs to cytotoxic products by activated neutrophils. Science. 1994;266(5186):810–813. doi: 10.1126/science.7973636. [DOI] [PubMed] [Google Scholar]
- 5.Wilson J., Gleghorn K., Kelly B. Cryptococcoid Sweet's syndrome: Two reports of Sweet's syndrome mimicking cutaneous cryptococcosis. J Cutan Pathol. 2017;44:413–419. doi: 10.1111/cup.12921. [DOI] [PubMed] [Google Scholar]
- 6.Fresco A., Wang J., Krausz A. Cryptococcus-like changes in the setting of vasculitis. J Cutan Pathol. 2019;46:143–147. doi: 10.1111/cup.13380. [DOI] [PubMed] [Google Scholar]