Abstract
Background
Localized lumbosacral hypertrichosis presenting as faun tail nevus often represents an underlying spinal occult or overt abnormality. This study was undertaken to study these abnormalities and assess their treatment outcome with Intense Pulse Light (IPL) for permanent hair reduction.
Methods
Patients reporting with localized spinal hypertrichosis underwent clinical examination and radio imaging. Symptomatic neurological deficit underwent definitive neurosurgical intervention (if indicated) before hair removal. IPL was administered as 30 J/cm2 four weekly for six sessions. Treatment assessment was based on a Global Physician Assessment Scale and by averaged terminal hair count at four quadrants in 1 cm2 area as observed through the hair densitometer before starting treatment, every four weeks and at the end of six months of follow up thereafter. Averaged hair count was interpreted with paired t-test.
Results
This neurocutaneous marker was observed in 15 patients out of a total of 360,767 patients (0.004%) over a four-year period. Age group of patients ranged from 3 to 26 years, comprising of all female patients. Radio imaging revealed diastematomyelia in 10, spina bifida in 04 and 01 had both as the primary spinal abnormality. Thirteen patients were treated with IPL for a period of six months, assessment after six months revealed a highly statistical significant p > 0.0001 reduction in hair growth consistent when followed up after 18 months.
Conclusion
This article aims to present a series of this rare neurocutaneous marker and highlight our experience in their management with IPL served as an effective alternative to traditional lasers.
Keywords: Faun tail nevus, Neurocutaneous marker, Intense Pulse Light, Spinal dysraphism
Introduction
A common ectodermal orin of skin and nervous system commonly results in co-existent anomalies in these tissues. Failure of closure of caudal neuropores by the fourth week of gestation may result in overt or occult spinal dysraphism. Midline cutaneous lesions often serve as markers for occult spinal dysraphism, and in a majority, serve as early indicators of these abnormalities.1 Lumbosacral lipomas, localized hypertrichosis, gluteal clefts and dimples or vascular malformations on skin may present in these cases on or near the midline. Hypertrichosis presenting as a lozenge shaped lumbosacral patch known as ‘faun tail’ is observed often with underlying spinal defects. Often these cases are brought for cosmetic reasons for management of hypertrichotic areas to the dermatologist while the rest may report to neurology and radiology centres. The importance of investigating these patients which present to the dermatology out patient, at an early age is to ensure they do not develop long term neurologic sequelae from missed spinal defects. We came across 15 cases of faun tail nevus at our tertiary level centre over a four-year period (Fig. 1, Fig. 2). Those reporting directly were investigated for underlying spinal dysraphism, others were already worked up and referred for management of localized hypertrichosis. The need for managing the hypertrichosis in these cases arises from the psychosocial impact they have on the growing child or adult if left untreated. Scant literature and absence of a larger series of these patients treated with Intense Pulse Light (IPL) led us to manage those already diagnosed as well as fresh cases between March 2014 and April 2016. Our cases were investigated for their spinal defect, provided definitive neurosurgical treatment and managed with IPL over a period of six months, and followed up for six months thereafter.
Fig. 1.
Cases 1–6 pre-treatment and post-treatment.
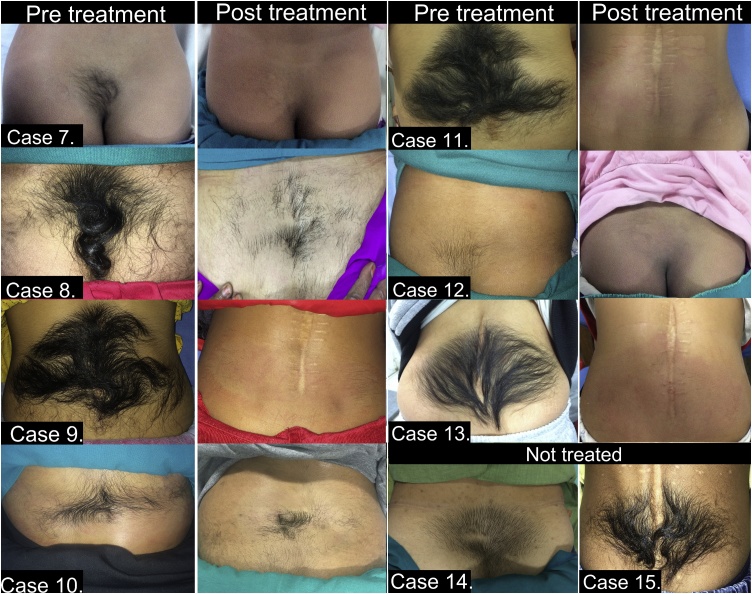
Fig. 2.
Cases 7–13 pre-treatment and post-treatment and Cases 14, 15 (not treated).
Material and methods
Failure of fusion of the midline mesenchymal, neural and bony structures of the spine results in spinal dysraphism. Intact skin with cutaneous markers, covering such defects serve as markers of occult defects. Faun tail nevus is one such cutaneous marker presenting in early childhood as a localised or rarely nevoid2 hypertrichotic patch which often alarms the parents. Fifteen cases (Fig. 1, Fig. 2) presented with faun tail nevus for hair removal to the skin centre over a four-year period. Ten cases reported directly for cosmetic treatment and five were referred from the centre of neurosciences for hair removal after their surgery. All were females, ranging in age from 3 years to 26 years. Two cases had associated dermal sinus in addition to the faun tail. Spinal dysraphism noted (Table 1) were diastematomyelia as the commonest (10 cases; 67%) followed by spina bifida (04 cases; 28%) and one had both diastematomyelia and spina bifida. None of the patients had sensorimotor deficit, bladder or bowel dysfunction, delayed walking, recurrent urinary tract infections, or a family history of similar complaints. Examination did not reveal any gait abnormality and none had kyphosis or scoliosis. All were born after a normal vaginal delivery, at term, after their mother had been on regular antenatal checkup.
Table 1.
Series, observation and results.
| No. | Age (years) | Spinal defect | Associated abnormality | Surgery* | PGAS# | Average hair count## |
|
|---|---|---|---|---|---|---|---|
| Pre-treatment | Post-treatment (after 6months) | ||||||
| 1 | 9 | Dilatation of cord T12-L1, bulbous thecal sac L5 | Nil | Nil | 4 | 34 | 8 |
| 2 | 3 | Diastematomelia Type II low thoracic type | Hydromyelia | Nil | 4 | 46 | 4 |
| 3 | 6 | Diastematomyelia Type I | Nil | Nil | 4 | 26 | 0 |
| 4 | 7 | Diastematomelia Type II | Bilateral Spondylolysis Spondylolisthesis L5 on S1 | Nil | 4 | 28 | 2 |
| 5 | 19 | Spina bifida L5, low lying cord | Conus medularis L2-3 | PS | 4 | 48 | 2 |
| 6 | 10 | Diastematomyelia Tethered cord |
Nil | Nil | 3 | 20 | 4 |
| 7 | 5 | Diastematomyelia Type I | Nil | Nil | 4 | 30 | 2 |
| 8 | 26 | Spina bifida L5 | Nil | Nil | 1 | 40 | 24 (Discontinued treatment after three sessions) |
| 9 | 16 | Diastematomyelia Type I | Nil | PS | 4 | 46 | 4 |
| 10 | 12 | Diastematomyelia, assymetric split cord | Multiple segmentation abnormalities, Low lying tethered cord, Left hemicord terminal lipoma, Dorsal dermal sinus | Nil | 1 | 26 | 16 |
| 11 | 16 | Diastematomelia Type I | Nil | PS | 4 | 44 | 2 |
| 12 | 3 | Diastematomyelia | Syringomyelia | Nil | 4 | 18 | 2 |
| 13 | 3 | Diastematomyelia Type 2 Spina bifida L4,5 |
Syringohydromyelia, Dorsal Dermal sinus | PS | 4 | 38 | 4 |
| 14 | 13 | Diastematomyelia Type I Low lying cord with tethered filum |
Nil | Nil | Did not undergo treatment in study period | ||
| 15 | 17 | Diastematomyelia Type I Low lying cord with tethered filum |
Multiple lumbar posterior neural arch defects Widened lumbosacral spinal cord |
PS | Did not undergo treatment in study period | ||
* PS: post-surgery.
# PGAS: Physician Global Assessment Score.
##p value < 0.0001.
Radiological screening was done in all cases with magnetic resonance imaging, underwent neurological assessment and were thereafter taken up for hair removal with IPL which was the light source available with us. Those cases referred after post-operative phase had no residual neurological damage. The other ten needed no active neurological intervention and were otherwise asymptomatic.
Thirteen patients were treated with IPL after counselling and consent and observed thereafter between March 2014 and April 2016 as a prospective study after institutional ethical and scientific committee clearance was taken. Parental consent was taken in case of minors. Clinical assessment was done before treatment, and at end of follow up period of at least 6 months. All patients were administered topical anesthesia with eutactic mixture of lidocaine and prilocaine for 45 min after clipping of hair. They were administered seven, four-weekly sessions with IPL using filter 750–1200 nm, single pass of pulse duration 10 ms, and pulse interval of 10 ms. The first session of IPL in all cases was with 16 J/cm2 followed by a review at one week and four weeks to watch for side effects. Subsequent doses were administered at 30 J/cm2 four weekly for six sessions. This protocol was developed in house at this centre after our experience in epilation with IPL.3
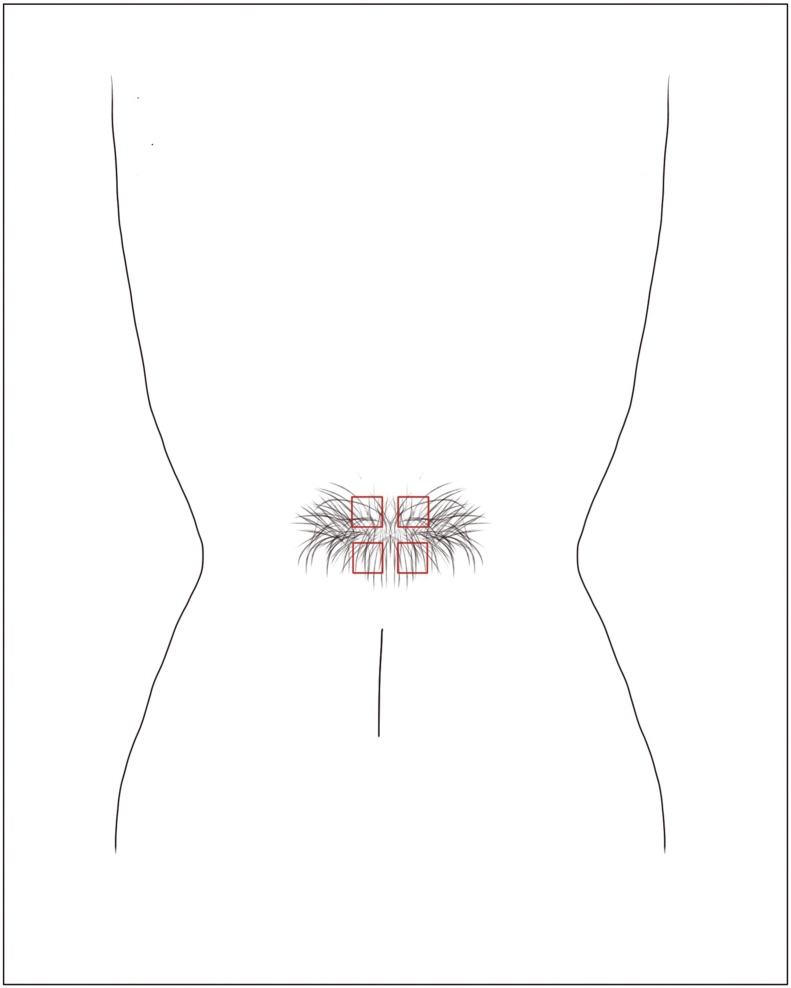
The patients were assessed and the results graded according to a 4-point Global Physician Assessment scale (GPAS) as excellent, >75% reduction in surface area; good, 50–75% reduction; fair; 25–50% reduction; and poor, <25% reduction in terminal hair density. Average terminal hair count was done of four quadrants in 1cm2 area as observed through the hair densitometer (Fig. 3) before starting treatment, at end of treatment sessions and end of six months of follow up thereafter.
Fig. 3.
Figure representing areas used for average hair count using hair-densitometer.
Results
All cases in the series were advised IPL treatment after they expressed willingness for hair removal management. Twelve cases completed their treatment and one discontinued after three sessions (Case No. 8) due to pregnancy and two patients did not report for treatment during the study period. Statistical analysis of the averaged hair count before and after treatment using paired t test showed highly statistically significant (p value < 0.0001) outcome after intervention (Table 1). All 13 cases were followed up for a period of six months after their treatment. Their improvement at end of treatment was maintained in all except case No. 5, aged 19. She initially responded with a fall in hair count from 26 to 10 at the end of six treatment sessions, with a relapse to 16 observed at the end of follow up period. She was thereafter subjected to further six sessions which reduced the average hair count to 12. She was not keen to undergo further treatment, was reviewed every six months for the next two years. No further regrowth was observed. Averaged terminal hair count as per GPAS in our study showed excellent improvement in 10 (77%), while 01 each achieved good and fair result.
One patient aged 13 years developed a superficial burn after third session which healed in one week. No other side effects were noted.
Discussion
Faun tail nevus represents congenital localised hypertrichosis in the lumbosacral region which often presents over an occult or occasionally an overt underlying spinal defect. Factors inducing terminal conversion of affected hair are unknown.4 The possible explanation proposed is a non-androgen dependent mechanism where an unknown factor may stimulate terminal conversion and, or prolonged anagen growth phase.5 Polygenic inheritance, a possibility of folic acid deficiency in mother during antepartum period with an increased risk in subsequent pregnancies have been proposed as other contributory factors.6 None of our cases had a positive family history of similar markers or spinal defect. All mothers had received folic acid supplementation in their antepartum period.
During the same 4-year study period, department of Radio-diagnosis, conducted magnetic resonance imaging for lumbosacral spinal dysraphism in 41 cases. Males accounted for 31 (76%) cases and females for 10 (24%) cases. Lumbosacral cutaneous markers were present in 16 cases (39%). Of these 8 (19.5%) had faun tail nevus, 03 (7%) dorsal dermal sinuses (two of these had faun tail nevus too), 03 (7%) myelomeningocoele, 01 sacral leiomyoma and 01 sacral lipomatosis. A literature search on larger series of spinal dysraphism reveals a coexistent faun tail with incidence ranging from 40 to 50% as a cutaneous marker for spinal dysraphisme.7, 8, 9 It is reported to be the third most common sign of occult spinal dysraphism with others being presence of a myelomeningocele sac, dermal sinus, hemangioma, lipoma or a sacral dimple.10
Reported faun tail nevi have a predominance of female gender affected with isolated case reports of males affected.11, 12 All our cases were females. The incidence noted in our outpatient of this abnormality was 0.004% (of a total of 380,547 patients seen in the four-year period). Associated abnormalities may progressively worsen if underlying spinal abnormalities are not detected.11, 13 None of the cases in this series had any permanent neurological deficit. Definite treatment if indicated of these neurological abnormalities must precede the management of faun tail nevus.
Neurosurgical intervention does not treat the faun tail nevus with hair, growing back in a few months. Management thus needs permanent hair reduction to reduce the psychosocial impact on the affected. Laser light sources are monochromatic while IPL which is a polychromatic light source is used with cutoff filters to select the emitted wavelengths depending on the target chromophore such as melanin in treatment of pigmented lesions and hair removal. Alexandrite laser,14 Diode laser15 and IPL12 all have been reported in isolated cases as successful. Our series of patients responded well to IPL treatment (Table 1). Our protocol included initial low fluence session to watch for side effects followed by six, monthly sessions and assessment, monthly, at the end of treatment and after six months of follow up.3, 16 Improvement at the end of treatment was maintained in all but patient No. 10. She initially responded with a fall in hair count from 26 to 10 at the end of six treatment sessions, with a relapse to 16 observed at the end of follow up period. She was thereafter subjected to further six sessions which reduced the average hair count to 12. Possible explanations for the poorer response could be the older age with thicker terminal hair, inadequacy of IPL to target these persistent faun tail nevi or need for a higher fluence in these cases. All other patients who completed treatment responded well. Other workers have not reported the follow up period although the response to lasers have been reported as adequate. Statistical analysis was done on our outcome of 13 cases. A higher statistical significance of IPL treatment would be possible if a much larger series of cases were undertaken and followed up for a longer period which in our case was limited to 6 months.
Our concerns in management of children with IPL were an anticipated refusal of younger children for the procedure and adverse effects to IPL. All children were counselled by the authors and none refused the procedure. The initial low fluence session coupled with topical anesthesia convinced them of the painlessness of procedure. Laser epilation may produce superficial burns especially in Fitzpatrick skin type IV to VI which was our cases skin type. IPL has a cooled hand piece which reduces the chances of epidermal injury. Using a 755–1200 nm filter further reduces chances of this injury. An early review after seven days of the procedure addressed these concerns. None of our cases had any evidence of persisting pain, erythema or pigmentation after the procedure.
In absence of a consensus on the most beneficial or effective hair removal laser or IPL, the IPL has established itself as an effective modality of treatment in hair removal.17 It’s efficacy has been reported to be up to 80% after 12 months of follow up.16 This is comparable to lasers used in hair removal.
Conclusion
Faun tail nevus is a rare neurocutaneous marker of spinal dysraphism. Neurosurgical intervention if necessary is a must which however shall not address the hypertrichosis. Managing the faun tail nevi must be undertaken to reduce their psychosocial impact on the affected. In the absence of a gold standard for management of hypertrichosis in faun tail nevus, IPL offers an excellent option with long lasting effect in permanent hair reduction. The earlier in age it is instituted the better is the result.
Conflicts of interest
The authors have none to declare.
References
- 1.Arora S., Rawat S., Banerjee A. Faun tail nevus – a case report. Med J Armed Forces India. 2006;62:286–287. doi: 10.1016/S0377-1237(06)80025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antony F.C., Holden C.A. Diffuse hypertrichosis and faun-tail nevus as cutaneous markers of spinal dysraphism. Clin Exp Dermatol. 2002;27:645–648. doi: 10.1046/j.1365-2230.2002.01091.x. [DOI] [PubMed] [Google Scholar]
- 3.Arora S., Arora G. Laser hair removal. Proceedings of Newer Vistas in Dermatology: Lotions to Lasers; Pune, India; 2014. Available from: Accessed 01.01.16. [Google Scholar]
- 4.Vashi R.A., Mancini A.J., Paller A.S. Primary generalized and localized hypertrichosis in children. Arch Dermatol. 2001;137:877–884. [PubMed] [Google Scholar]
- 5.McAtee-Smith J., Hebert A.A., Rapini R.P., Goldberg N.S. Skin lesions of the spinal axis and spinal dysraphism. Fifteen cases and a review of the literature. Arch Pediatr Adolesc Med. 1994;148:740–748. doi: 10.1001/archpedi.1994.02170070078015. [DOI] [PubMed] [Google Scholar]
- 6.Wilson R.D., Genetics Committee, Wilson R.D. Pre-conception folic acid and multivitamin supplementation for the primary and secondary prevention of neural tube defects and other folic acid-sensitive congenital anomalies. J Obstet Gynaecol Can. 2015;37:534–552. doi: 10.1016/s1701-2163(15)30230-9. [DOI] [PubMed] [Google Scholar]
- 7.Kumar R., Singh S.N. Spinal dysraphism: trends in Northern. India Pediatr Neurosurg. 2003;38:133–145. doi: 10.1159/000068819. [DOI] [PubMed] [Google Scholar]
- 8.Miller A., Guille J.T., Bowen J.R. Evaluation and treatment of diastematomyelia. J Bone Joint Surg Am. 1993;75:1308–1316. doi: 10.2106/00004623-199309000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Keim H.A., Greene A.F. Diastematomyelia and scoliosis. J Bone Joint Surg Am. 1973;55:1425–1435. [PubMed] [Google Scholar]
- 10.Yamini M., Sridevi K.S., Babu N.P., Chetty N.G. Faun tail nevus. Indian Dermatol Online J. 2011;2:23–24. doi: 10.4103/2229-5178.79865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gupta R., Singal A., Pandhi D. Faun tail naevus a cutaneous marker of spinal dysraphism. Indian Pediatr. 2005;42:67–69. [PubMed] [Google Scholar]
- 12.Lee H.I., Rho Y.K., Kim B.J., Kim M.N. A case of faun tail naevus treated by intense pulsed light. Ann Dermatol. 2009;21:147–149. doi: 10.5021/ad.2009.21.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sethuraman G., Handa S., Singh P., Ghosh D., Kumar B. Spinal dysraphism presenting as acro-osteolysis: report of four cases. Pediatr Dermatol. 2001;18:97–101. doi: 10.1046/j.1525-1470.2001.018002097.x. [DOI] [PubMed] [Google Scholar]
- 14.Kaptanoglu A.F., Kaptanoglu E. Faun tail nevus and spinal dysraphism: cosmetic improvement with alexandrite laser epilation. Ann Dermatol. 2011;23:S296–S298. doi: 10.5021/ad.2011.23.S3.S296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chembolli L. Faun tail overlying spinal dysraphism (diastematomyelia) at the mid thoracic level: cosmetic improvement achieved with diode laser epilation. Indian J Dermatol. 2015;60(638) doi: 10.4103/0019-5154.169165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldberg D.J., Hussain M. Laser treatment of unwanted hair. In: Goldberg D.J., editor. Laser Dermatology. 1st ed. Springer; New York: 2005. pp. 61–80. [Google Scholar]
- 17.Buddhadev R.M. Standard guidelines of care: laser and IPL hair reduction. Indian J Dermatol Venereol Leprol. 2008;74(suppl S1):68–74. [PubMed] [Google Scholar]