Abstract
Background
To investigate the incidence of surgical intervention in very low birth weight (VLBW) infants and the impact of surgery on neurodevelopmental outcomes at corrected ages (CAs) of 18–24 months, using data from the Korean Neonatal Network (KNN).
Methods
Data from 7,885 VLBW infants who were born and registered with the KNN between 2013 to 2016 were analyzed in this study. The incidences of various surgical interventions and related morbidities were analyzed. Long-term neurodevelopmental outcomes at CAs of 18–24 months were compared between infants (born during 2013 to 2015, n = 3,777) with and without surgery.
Results
A total of 1,509 out of 7,885 (19.1%) infants received surgical interventions during neonatal intensive care unit (NICU) hospitalization. Surgical ligation of patent ductus arteriosus (n = 840) was most frequently performed, followed by laser therapy for retinopathy of prematurity and laparotomy due to intestinal perforation. Infants who underwent surgery had higher mortality rates and greater neurodevelopmental impairment than infants who did not undergo surgery (P value < 0.01, both). On multivariate analysis, single or multiple surgeries increased the risk of neurodevelopmental impairment compared to no surgery with adjusted odds ratios (ORs) of 1.6 with 95% confidence interval (CI) of 1.1–2.6 and 2.3 with 95% CI of 1.1–4.9.
Conclusion
Approximately one fifth of VLBW infants underwent one or more surgical interventions during NICU hospitalization. The impact of surgical intervention on long-term neurodevelopmental outcomes was sustained over a follow-up of CA 18–24 months. Infants with multiple surgeries had an increased risk of neurodevelopmental impairment compared to infants with single surgeries or no surgeries after adjustment for possible confounders.
Keywords: Surgery, Korean Neonatal Network, Very Low Birth Weight Infant, Neurodevelopmental Outcome
Graphical Abstract
INTRODUCTION
Neonatal complication rates in preterm infants have largely been stagnant for decades as survival rates of extreme premature infants are constantly increasing.1,2,3,4 Relatively few studies, however, have been conducted investigating the incidences of surgical interventions due to major neonatal morbidities and the impact of surgery on neurodevelopmental outcomes in very low birth weight (VLBW) infants.5,6,7,8,9,10,11,12 Studies investigating surgical outcomes using national registry data are even fewer.13 Although this data is useful for parents of preterm babies, neonatologists desiring quality improvement in their units, and government agencies seeking to determine the overall medical costs associated with preterm care, the current incidence of surgical interventions in preterm infants in Korea is not known.
The purpose of the present study was therefore to investigate the incidences of various surgical interventions in VLBW infants and the impact of surgery on neonatal neurodevelopmental outcomes at corrected ages (CAs) of 18–24 months, using data from the Korean Neonatal Network (KNN), with which more than 70% of VLBW infants born in Korea are registered.14 Additionally, the association between the number and type of surgical intervention and neurodevelopmental outcomes was evaluated in this study.
METHODS
Study population
The KNN is a nationwide neonatal registry of 70 neonatal intensive care units (NICUs) representing 70% of the NICU beds in Korea. The database provides prospectively collected clinical information on VLBW infants totaling 70%–80% of the VLBW infants born in Korea each year. Among all 8,287 infants registered in the KNN database over a four-year period from January 2013 to December 2016, infants with gestational age < 23 weeks (n = 105) or having life-threatening congenital anomalies (n = 297) were excluded, and the remaining 7,885 infants were included in this study. Among these infants, data on long-term neurodevelopmental outcomes at CAs of 18–24 months were available for infants born between January 2013 and December 2015 (n = 3,777), as long-term data on infants born in 2016 had not yet been reported.
Data collection and data monitoring
The study variables were defined according to a manual of definitions and operations. Data validation and monitoring at each site were performed on a regular basis by external monitoring agents.14 Demographic data included gestational age (GA), birth weight, sex, multiple gestation, cesarean section, Apgar score at 1 and 5 minutes, antenatal steroid use, pathologically confirmed chorioamnionitis, and other variables. The various surgical interventions and related morbidities were compared according to GA group which was set arbitrarily considering the number of patients and the survival rates: group I, GA ≤ 26 weeks (n = 2,135); group II, GA 27–29 weeks (n = 2,962); and group III, GA 30 weeks or higher (n = 2,788).
Surgical interventions included ventriculoperitoneal shunt (VP shunt), laser operation for retinopathy of prematurity (ROP), surgical ligation for patent ductus arteriosus (PDA), tracheostomy due to long-term mechanical ventilator support or airway maintenance, and laparotomy or peritoneal drainage due to necrotizing enterocolitis (NEC) or spontaneous intestinal perforation (SIP). Data on in-hospital morbidities related to surgical interventions were also collected.
Long-term neurodevelopmental outcomes at CAs of 18–24 months included cerebral palsy, Bayley scales of infant development (BSID)-II or III, and neurosensory impairment. Severe cognitive delay was defined as a mental developmental index (MDI) of less than 70 in BSID-II, or cognitive/language score of less than 85 in BSID-III according to the recent studies by Jary et al.15 and Johnson et al.16 Likewise, severe psychomotor delay was defined as a psychomotor developmental index (PDI) of less than 70 in BSID-II, or motor score of less than 85 in BSID-III. Neurosensory impairment included unilateral or bilateral visual or hearing loss. Neurodevelopmental impairment was defined as the presence of at least one of the following: cerebral palsy, severe cognitive or psychomotor delay, or neurosensory impairment. Cerebral palsy was defined as a non-progressive disorder of motor function affecting bilateral upper and lower extremities, diagnosed at CAs of 18–24 months by a pediatric neonatologist or a physician specializing in pediatric rehabilitation medicine.
Statistical analysis
Data on demographics, surgical interventions, surgery-related morbidities, and neurodevelopmental outcomes were evaluated in infants among different GA groups. Neurodevelopmental outcome data of infants who received one or more surgical interventions were compared with those of infants who received no surgical interventions. Continuous variables are shown as means ± standard deviations. Statistical differences were calculated with χ2 tests for categorical variables and a t-test or Mann-Whitney U test for quantitative variables. To test the impact of surgery, number of surgeries, and type of surgery on neurodevelopmental impairment at CAs of 18–24 months, multivariate analyses calculating adjusted ORs with 95% confidence intervals (CIs) were performed by using binary logistic regression. Multivariate analyses were adjusted for GA, antenatal steroid use, intraventricular hemorrhage grade 3–4, moderate to severe bronchopulmonary dysplasia, retinopathy of prematurity stage 3 or greater, necrotizing enterocolitis stage 2 or greater, and blood culture-proven sepsis. Data analysis was performed using STATA 14.0 (StataCorp LP, College Station, TX, USA).
Ethics statement
The KNN registry was approved by the Institutional Review Board at each participating hospital and informed consent was obtained from the parents at enrollment by the NICUs participating in KNN (Samsung Medical Center, 2013-03-002).
RESULTS
Demographic characteristics
The mean GA of the study population was 28.5 ± 3.0 weeks, ranging from 23.0 to 38.3 weeks, with a mean birth weight of 1,085 ± 280 g. In total, 1,509 infants from among 7,885 (19.1%) received surgical interventions during initial NICU hospitalization. Infants who underwent surgery had lower GAs, birth weights, Apgar scores at 1 and 5 minutes, lower rates of cesarean section, maternal hypertension, gestational diabetes, and higher rates of chorioamnionitis (Table 1).
Table 1. Demographic characteristics.
| Characteristics | Total (n = 7,885) | No surgery (n = 6,376) | Surgery (n = 1,509) | P value |
|---|---|---|---|---|
| GA, wk | 28.5 ± 3.0 | 29.0 ± 2.9 | 26.3 ± 2.2 | < 0.01 |
| Birth weight, g | 1,086 ± 280 | 1,135 ± 265 | 875 ± 239 | < 0.01 |
| Sex, male | 3,927 (49.8) | 3,176 (49.8) | 751 (49.8) | 0.98 |
| Multiple gestation | 2,832 (35.9) | 2,295 (36.0) | 537 (35.6) | 0.77 |
| Cesarean section | 6,122 (77.6) | 5,002 (78.5) | 1,120 (74.2) | < 0.01 |
| Apgar score, 1 min | 4.7 ± 2.0 | 4.9 ± 2.0 | 3.7 ± 1.9 | < 0.01 |
| Apgar score, 5 min | 6.8 ± 1.8 | 7.0 ± 1.7 | 6.0 ± 1.9 | < 0.01 |
| Antenatal steroid | 6,054 (76.8) | 4,868 (76.4) | 1,186 (78.6) | 0.06 |
| Chorioamnionitis | 2,246 (28.5) | 1,714 (26.9) | 532 (35.3) | < 0.01 |
| Maternal age, yr | 32.9 ± 4.2 | 32.9 ± 4.2 | 33.0 ± 4.3 | 0.39 |
| Maternal hypertension | 1,501 (19.0) | 1,306 (20.5) | 195 (12.9) | < 0.01 |
| In-vitro fertilization | 1,828 (23.2) | 1,466 (23.0) | 362 (24.0) | 0.41 |
| Gestational diabetes | 598 (7.6) | 508 (8.0) | 90 (6.0) | 0.02 |
Data are presented as mean ± standard deviation or number (%).
GA = gestational age.
Incidence of surgical intervention and related morbidities
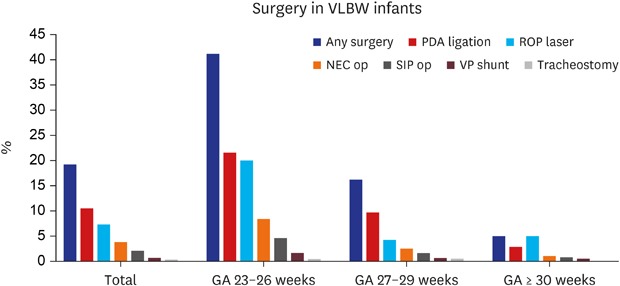
Table 2 shows the incidences of surgical interventions and related morbidities. Surgical ligation of patent ductus arteriosus (840/7,885; 10.7%) was most frequently performed, followed by laser therapy for retinopathy of prematurity (7.4%) and laparotomy due to intestinal perforation (5.7%). Surgical intervention was performed more frequently in infants in group I than in those in groups II (P value < 0.01) and III (P value < 0.01). There were 347 infants (4.4%) who received more than one surgical intervention (Table 3). Multiple surgeries were also more frequent in infants in the lower GA group. Additionally, congenital anomalies typically requiring surgical correction are presented in Supplementary Table 1.
Table 2. Surgical intervention and related morbidities in Korean VLBW infants.
| Variables | Total (n = 7,885) | Group I (n = 2,135) | Group II (n = 2,962) | Group III (n = 2,788) | ||
|---|---|---|---|---|---|---|
| Central nervous system | ||||||
| IVH (grade III–IV) | 703 (8.9) | 475 (22.3) | 184 (6.2) | 44 (1.6) | ||
| PHH | 316 (4.0) | 213 (10.0) | 85 (2.9) | 18 (0.7) | ||
| Ventriculo-peritoneal shunt operation | 41 (0.5) | 23 (1.1) | 14 (0.5) | 4 (0.1) | ||
| Mortality due to IVH and PHH | 79 (1.0) | 63 (2.9) | 16 (0.5) | 0 (0) | ||
| Mortality due to PHH before operation | 28 (0.4) | 10 (0.5) | 10 (0.3) | 8 (0.3) | ||
| Cystic periventricular leukomalacia | 261 (3.3) | 187 (8.8) | 54 (1.8) | 20 (0.7) | ||
| Retinopathy of prematurity | ||||||
| Highest stage ≥ III | 766 (9.7) | 396 (18.6) | 228 (7.7) | 142 (5.1) | ||
| Highest stage ≥ IV | 16 (0.2) | 12 (0.6) | 1 (0.0) | 3 (0.01) | ||
| Zone I retinopathy | 149 (1.9) | 101 (4.7) | 33 (1.1) | 15 (0.5) | ||
| Anti-VEGF treatment | 295 (3.6) | 153 (7.2) | 84 (2.8) | 46 (1.7) | ||
| Laser operation | 585 (7.4) | 443 (20.8) | 128 (4.3) | 14 (0.5) | ||
| Postnatal age of operation, day (IQR) | 85.2 ± 28.7 (69–93) | 88.1 ± 30.7 (70–95) | 76.3 ± 17.1 (60–87) | 66.3 ± 26.8 (48–85) | ||
| PDA | ||||||
| Intervention for symptomatic PDA | 2,008 (25.5) | 826 (38.7) | 828 (28.0) | 354 (12.7) | ||
| Prophylactic or pre-symptomatic treatment | 894 (11.3) | 345 (16.2) | 373 (12.6) | 176 (6.3) | ||
| Indomethacin or ibuprofen | 2,612 (33.1) | 1,036 (48.5) | 1,098 (37.1) | 478 (17.1) | ||
| Surgical ligation | 840 (10.7) | 480 (22.5) | 286 (9.7) | 74 (2.7) | ||
| Postnatal age of ligation, day (IQR) | 20.4 ± 22.4 (9–25) | 22.2 ± 25.8 (10–26) | 18.6 ± 16.2 (8–24) | 16.5 ± 17.4 (6–23) | ||
| Respiratory sequelae | ||||||
| BPD (moderate to severe) | 2,019 (25.6) | 896 (42.0) | 826 (27.9) | 297 (10.7) | ||
| Moderate | 797 (10.1) | 270 (12.7) | 380 (12.8) | 147 (5.3) | ||
| Severe | 1,222 (15.5) | 626 (29.3) | 446 (15.1) | 150 (5.4) | ||
| BPD (moderate to severe) or mortality before corrected age 36 weeks | 2,968 (37.6) | 1,562 (73.2) | 1,014 (34.2) | 392 (14.1) | ||
| Tracheostomy before hospital discharge | 8 (0.1) | 2 (0.1) | 4 (0.1) | 2 (0.1) | ||
| Tracheostomy before postnatal 24 months | 12 (0.2) | 3 (0.1) | 4 (0.1) | 5 (0.2) | ||
| Necrotizing enterocolitis | ||||||
| Stage ≥ 2b | 520 (6.6) | 284 (13.3) | 167 (5.6) | 69 (2.5) | ||
| Operation | 283 (3.6) | 185 (8.7) | 72 (2.4) | 26 (0.9) | ||
| Laparotomy | 231 (2.9) | 150 (7.0) | 61 (2.1) | 20 (0.7) | ||
| Peritoneal drainage | 10 (0.1) | 7 (0.3) | 2 (0.1) | 1 (0.0) | ||
| Peritoneal drain followed by laparotomy | 39 (0.5) | 26 (1.2) | 8 (0.3) | 5 (0.2) | ||
| Postnatal age of operation, day | 21.9 ± 20.0 | 19.6 ± 15.8 | 28.7 ± 27.0 | 11.5 ± 7.7 | ||
| Hospital discharge with ostomy | 44 (0.6) | 19 (0.9) | 18 (0.6) | 7 (0.3) | ||
| Spontaneous intestinal perforation | ||||||
| Operation | 163 (2.1) | 101 (4.7) | 46 (1.6) | 16 (0.6) | ||
| Laparotomy | 125 (1.6) | 61 (2.9) | 37 (1.3) | 27 (1.0) | ||
| Peritoneal drainage | 10 (0.1) | 7 (0.3) | 2 (0.1) | 1 (0.0) | ||
| Peritoneal drain followed by laparotomy | 18 (0.2) | 7 (0.3) | 4 (0.1) | 7 (0.3) | ||
| Postnatal age of operation, day | 24.9 ± 53.2 | 25.8 ± 57.9 | 26.6 ± 46.8 | 3.3 ± 2.1 | ||
Data are presented as mean ± standard deviation or number (%).
VLBW = very low birth weight, IVH = intraventricular hemorrhage, PHH = post-hemorrhagic hydrocephalus, VEGF = vascular endothelial growth factor, IQR = interquartile range, PDA = patent ductus arteriosus, BPD = bronchopulmonary dysplasia.
Table 3. Infants who underwent multiple surgeries.
| Variables | Total (n = 7,885) | Group I (n = 2,135) | Group II (n = 2,962) | Group III (n = 2,788) |
|---|---|---|---|---|
| Any surgery | 1,509 (19.1) | 905 (42.4) | 477 (16.1) | 127 (4.6) |
| 1 time | 1,162 (14.7) | 632 (29.6) | 413 (13.9) | 117 (4.2) |
| 2 times | 280 (3.6) | 216 (10.1) | 54 (1.8) | 10 (0.4) |
| 3 times | 62 (0.8) | 52 (2.4) | 10 (0.3) | 0 (0) |
| ≥ 4 times | 5 (0.1) | 5 (0.2) | 0 (0) | 0 (0) |
Data are presented as number (%).
In-hospital mortality and long-term neurodevelopmental outcomes
Mortality rates during initial NICU hospitalization were significantly higher in infants who underwent surgery than in infants who did not undergo surgery (15.6% vs. 11.8%; P value < 0.01) (Table 4). Among 3,777 infants followed up until 18–24 months of CA, infants who underwent surgery had significantly higher incidences of cerebral palsy, severe cognitive or psychomotor delay, and neurosensory impairment. The higher the number of surgeries, the higher the likelihood of exhibiting neurodevelopmental impairment was.
Table 4. In-hospital mortality rates and long-term neurodevelopmental outcomes in VLBW infants who underwent single or multiple surgeries.
| Variables | No surgery | Any surgery | 1 time | 2 times | ≥ 3 times | |
|---|---|---|---|---|---|---|
| No. (%) | 6,376 (80.9) | 1,509 (19.1) | 1,162 (14.7) | 280 (3.6) | 67 (0.9) | |
| Mortality during NICU hospitalization | 753 (11.8) | 235 (15.6)a | 176 (11.2)a | 49 (17.5)a | 10 (14.9)a | |
| Hospital day | 55.6 ± 32.5 | 100.6 ± 51.4a | 95.2 ± 49.1a | 115.8 ± 55.0a | 130.3 ± 53.8a | |
| Follow-up at CA 18-24 months (total n = 3,777) | ||||||
| No. (%) | 2,960 (78.4) | 817 (21.6) | 608 (16.1) | 164 (4.3) | 45 (1.2) | |
| Cerebral palsy | 25 (0.8) | 38 (4.7)a | 17 (2.8)a | 14 (8.5)a | 7 (15.6)a | |
| MDI score (BSID-II) | 84.0 ± 23.7 | 83.3 ± 20.7 | ||||
| Cognition score (BSID-III) | 97.4 ± 14.8 | 94.1 ± 17.5 | ||||
| Language score (BSID-III) | 93.9 ± 15.2 | 90.6 ± 18.3 | ||||
| Severe cognitive delay | 101 (3.4) | 41 (5.0)a | 27 (4.4)a | 13 (7.9)a | 1 (2.2) | |
| PDI score (BSID-II) | 83.2 ± 22.0 | 84.9 ± 20.3 | ||||
| Motor score (BSID-III) | 94.0 ± 16.5 | 90.4 ± 18.5 | ||||
| Severe psychomotor delay | 80 (2.7) | 30 (3.3)a | 23 (3.8)a | 7 (4.3)a | 0 (0) | |
| Neurosensory (hearing or visual) impairment | 10 (0.3) | 12 (1.5)a | 7 (1.2)a | 2 (1.2)a | 3 (6.7)a | |
| Any neurodevelopmental impairment | 98 (3.3) | 40 (4.9)a | 28 (4.6)a | 8 (4.9)a | 4 (8.9)a | |
Data are presented as mean ± standard deviation or number (%).
VLBW = very low birth weight, NICU = neonatal intensive care unit, CA = corrected age, MDI = mental developmental index, BSID = Bayley scales of infant development, PDI = psychomotor developmental index.
aCompared with no surgery.
Multivariate analysis
On multivariate analysis, surgery increased the risk of neurodevelopmental impairment with an adjusted OR of 1.7 (95% CI, 1.1–2.7) compared to no surgery (Table 5). The risk of surgery on the neurodevelopmental impairment increased by an adjusted OR of 1.7 (95% CI, 1.1–2.7) as the number of surgeries increased by one. Additionally, there was an increased incidence of cerebral palsy, severe cognitive delay, and any neurodevelopmental impairment as the number of surgeries increased. Each major surgery, with the exception of PDA ligation and surgery due to SIP, increased the risk of neurodevelopmental impairment with statistical significance.
Table 5. Increased risk of neurodevelopmental impairment according to the frequency and type of surgical intervention.
| Variables | Adjusted ORa | 95% CI | |
|---|---|---|---|
| Any surgery | 1.7 | 1.1–2.7 | |
| No. of surgeries, per each additional surgery | 1.5 | 1.1–2.1 | |
| Single surgery vs. no surgery | 1.6 | 0.9–2.6 | |
| Two surgeries vs. no surgery | 1.8 | 0.9–4.4 | |
| Three or more surgeries versus no surgery | 4.8 | 1.4–15.9 | |
| PDA ligation | 1.5 | 0.9–2.6 | |
| ROP laser operation | 2.2 | 1.2–3.9 | |
| NEC surgery | 2.0 | 1.1–2.5 | |
| SIP surgery | 1.8 | 0.9–3.4 | |
| VP shunt | 7.6 | 2.7–20.9 | |
| Tracheostomy | 5.0 | 1.6–43.5 | |
OR = odds ratio, CI = confidence interval, PDA = patent ductus arteriosus, ROP = retinopathy or prematurity, NEC = necrotizing enterocolitis, SIP = spontaneous intestinal perforation, VP = ventriculoperitoneal.
aAdjusted gestational age and antenatal steroid use, intraventricular hemorrhage grade 3 or 4, retinopathy or prematurity stage 3 or greater, moderate to severe bronchopulmonary dysplasia, necrotizing enterocolitis stage 2 or greater, blood culture proven sepsis.
DISCUSSION
In the present study, 1,509 VLBW infants (19.1%) underwent surgical intervention during NICU hospitalization; PDA ligation (n = 840) was performed most frequently, followed by laser operation for ROP (n = 585) and laparotomy due to necrotizing enterocolitis (n = 283). Infants with a lower GA underwent surgery more frequently: 42.4% of infants born at GA 23–26 weeks received one or more surgical interventions.17 The incidence of surgery in our study was similar to that reported in previous studies in which approximately 20%–30% of VLBW infants received surgical interventions.13
Relatively few studies have specifically investigated the impact of surgery on long-term neurodevelopmental outcomes. Morriss et al.13 showed the independent risk of surgery on neurodevelopmental outcome using data from the National Institute of Child Health and Human Development Neonatal Research Network Generic Database (n = 2,186). The study by Filan et al.18 showed the association between surgery, particularly intestinal surgery, and brain volume in infants born at < 30 weeks gestation (n = 227). The authors showed that infants exposed to surgery had smaller deep nuclear gray matter volumes and greater white matter injury. The authors also showed that the adverse effects of surgery on neurodevelopmental outcome were more pronounced in infants received intestinal surgery than those received PDA ligation. However, these authors did not include VP shunt and tracheostomy in their main analysis; these two surgical procedures were found to be associated with the highest risk of neurodevelopmental impairment in our study. The adverse effects of surgery on neurodevelopmental outcome were also demonstrated in children with noncardiac congenital anomalies through the systematic review by Stolwijk et al.19 The results from the pooled data showed that cognitive and motor developmental delay was found in 23% children who received surgery in neonatal period due to noncardiac congenital anomalies. The study by Flick et al.20 also showed that repeated exposure to surgery and anesthesia before the age of 2 was associated with learning disability in later school life. The authors included children from a birth cohort in Minnesota, USA, however few VLBW infants were included in the study. With the exception of the study by Morriss et al.,13 there have been no reports presenting national data on surgical outcomes in extremely preterm infants. Our data show great significance in presenting national data on VLBW infants by showing that surgical intervention performed during initial NICU hospitalization was associated not only with the risk of short-term in-hospital morbidity and mortality but also with long-term neurodevelopmental outcomes after adjusting for possible confounders, including the severity of underlying morbidities. We also provided the additional evidence suggested by Morriss et al.,13 that is, that the number of surgeries matters: the more surgical interventions, the greater risk of neurodevelopmental impairment.
It is difficult to differentiate the impact of surgery on neurodevelopmental outcomes from the adverse effects of anesthetic medications or from the effects of the underlying morbidities leading to surgery and simultaneously to brain injury through systemic inflammation, infection, or cellular hypoxia.21,22,23,24,25 Unfortunately, a randomized clinical trial does not seem to be an appropriate method, as it is unethical to deliberately divide infants with life-threatening conditions into surgical and medical arms. Because of emerging evidence suggesting the direct toxic effects of general anesthetic medications on the premature and developing brain,26,27,28,29 it is also unethical to administer unnecessary general anesthetics for study purposes. Although the data in the present study were collected retrospectively from infants registered prospectively, post-hoc analysis of this large-scale national cohort data seemed to be the most feasible and reasonable design to assess the impact of surgery on neonatal outcomes after adjusting for all possible confounders. Future studies need to include the type or duration of general anesthetic medications in the analysis as effect modifiers. Likewise, other medications known to affect neurodevelopmental outcome such as postnatal corticosteroid should need to be included in future studies. In addition, the timing, site, and degree of invasiveness of the surgery might have different effects on each neurodevelopmental impairment including cerebral palsy, cognitive or psychomotor delay, or neurosensory impairment. Further studies will therefore need to distinguish these points.
Another limitation encountered in our study was that the data from subsequent laparotomies after the initial laparotomy and other minor surgeries, including inguinal hernia operation, were unavailable in the KNN registry.30,31 Although the data on surgical intervention due to congenital anomalies typically requiring surgery were also unavailable, we showed the type and incidences of congenital anomalies registered in the KNN.10,19 Since long-term neurodevelopmental outcome data at CAs of 18–24 months were investigated in this study, follow-up studies are warranted to evaluate neurodevelopmental outcomes in these children at school ages or even after longer periods.20,32,33 On the other hand, one should pay attention to the possibility that the severity of the underlying morbidity which led to the surgery, rather than the operation itself, had affected the neurodevelopmental impairment. Our results should be interpreted considering that surgery may be another way of expressing the severity of morbidity.
In addition, in the present study, the infants in group 3 (GA ≥ 30 weeks) were expected to have a high rate of small-for-gestational age (SGA), however, the SGA data were not obtained and included in our analysis. In spite of these limitations, our study provided national data on the incidences of various surgical interventions in VLBW infants. Furthermore, we provided additional evidence showing that surgical intervention was associated with detrimental neurodevelopmental outcomes and that multiple surgeries increased the risk of neurodevelopmental impairment compared with single surgeries. Lastly, we showed that the impact of surgery on neurodevelopment was different according to the type of surgery.
In conclusion, approximately one fifth of VLBW infants underwent one or more surgical interventions during initial NICU hospitalization. The impact of surgical interventions on long-term neurodevelopmental outcomes was sustained over a follow-up at a CA of 18–24 months. We showed that infants with multiple surgical interventions were at a greater risk of neurodevelopmental impairment than infants with single surgeries or no surgeries after adjusting for all possible confounders. Our results provide a reference for surgical intervention to parents, neonatologists, and social workers and elucidated the impact of surgical interventions performed in the early period of life on long-term neurodevelopmental outcomes. Future studies should include the effect of general anesthesia on neurodevelopmental outcome.
Footnotes
Funding: Research Program funded by the Korean Centers for Disease Control and Prevention (2013-E63008-01).
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Chang YS, Park WS, Ahn SY.
- Data curation: Kim HS, Kim HH.
- Formal analysis: Sung SI, Kim HH.
- Investigation: Yang MS, Han YS.
- Methodology: Lee NH, Han YS.
- Software: Sung SI.
- Validation: Ahn SY.
- Writing - original draft: Sung SI.
- Writing - review & editing: Sung SI, Chang YS, Park WS.
SUPPLEMENTARY MATERIAL
Major congenital anomalies requiring surgery in Korean VLBW infants
References
- 1.Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA. 2015;314(10):1039–1051. doi: 10.1001/jama.2015.10244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim JK, Chang YS, Sung S, Ahn SY, Yoo HS, Park WS. Trends in survival and incidence of bronchopulmonary dysplasia in extremely preterm infants at 23–26 weeks gestation. J Korean Med Sci. 2016;31(3):423–429. doi: 10.3346/jkms.2016.31.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443–456. doi: 10.1542/peds.2009-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adams-Chapman I, Heyne RJ, DeMauro SB, Duncan AF, Hintz SR, Pappas A, et al. Neurodevelopmental impairment among extremely preterm infants in the neonatal research network. Pediatrics. 2018;141(5):e20173091. doi: 10.1542/peds.2017-3091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mirea L, Sankaran K, Seshia M, Ohlsson A, Allen AC, Aziz K, et al. Treatment of patent ductus arteriosus and neonatal mortality/morbidities: adjustment for treatment selection bias. J Pediatr. 2012;161(4):689–694.e1. doi: 10.1016/j.jpeds.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Kabra NS, Schmidt B, Roberts RS, Doyle LW, Papile L, Fanaroff A, et al. Neurosensory impairment after surgical closure of patent ductus arteriosus in extremely low birth weight infants: results from the Trial of Indomethacin Prophylaxis in Preterms. J Pediatr. 2007;150(3):229–234. doi: 10.1016/j.jpeds.2006.11.039. [DOI] [PubMed] [Google Scholar]
- 7.Hull MA, Fisher JG, Gutierrez IM, Jones BA, Kang KH, Kenny M, et al. Mortality and management of surgical necrotizing enterocolitis in very low birth weight neonates: a prospective cohort study. J Am Coll Surg. 2014;218(6):1148–1155. doi: 10.1016/j.jamcollsurg.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 8.Blakely ML, Lally KP, McDonald S, Brown RL, Barnhart DC, Ricketts RR, et al. Postoperative outcomes of extremely low birth-weight infants with necrotizing enterocolitis or isolated intestinal perforation: a prospective cohort study by the NICHD Neonatal Research Network. Ann Surg. 2005;241(6):984–989. doi: 10.1097/01.sla.0000164181.67862.7f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wadhawan R, Oh W, Hintz SR, Blakely ML, Das A, Bell EF, et al. Neurodevelopmental outcomes of extremely low birth weight infants with spontaneous intestinal perforation or surgical necrotizing enterocolitis. J Perinatol. 2014;34(1):64–70. doi: 10.1038/jp.2013.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walker K, Badawi N, Holland AJ, Halliday R. Developmental outcomes following major surgery: what does the literature say? J Paediatr Child Health. 2011;47(11):766–770. doi: 10.1111/j.1440-1754.2010.01867.x. [DOI] [PubMed] [Google Scholar]
- 11.Gurtner P, Bass T, Gudeman SK, Penix JO, Philput CB, Schinco FP. Surgical management of posthemorrhagic hydrocephalus in 22 low-birth-weight infants. Childs Nerv Syst. 1992;8(4):198–202. doi: 10.1007/BF00262844. [DOI] [PubMed] [Google Scholar]
- 12.Sharma R, Tepas JJ, 3rd, Mollitt DL, Pieper P, Wludyka P. Surgical management of bowel perforations and outcome in very low-birth-weight infants (< or =1,200 g) J Pediatr Surg. 2004;39(2):190–194. doi: 10.1016/j.jpedsurg.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Morriss FH, Jr, Saha S, Bell EF, Colaizy TT, Stoll BJ, Hintz SR, et al. Surgery and neurodevelopmental outcome of very low-birth-weight infants. JAMA Pediatr. 2014;168(8):746–754. doi: 10.1001/jamapediatrics.2014.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang YS, Park HY, Park WS. The Korean neonatal network: an overview. J Korean Med Sci. 2015;30(Suppl 1):S3–S11. doi: 10.3346/jkms.2015.30.S1.S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jary S, Whitelaw A, Walløe L, Thoresen M. Comparison of Bayley-2 and Bayley-3 scores at 18 months in term infants following neonatal encephalopathy and therapeutic hypothermia. Dev Med Child Neurol. 2013;55(11):1053–1059. doi: 10.1111/dmcn.12208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson S, Moore T, Marlow N. Using the Bayley-III to assess neurodevelopmental delay: which cut-off should be used? Pediatr Res. 2014;75(5):670–674. doi: 10.1038/pr.2014.10. [DOI] [PubMed] [Google Scholar]
- 17.Limpert JN, Limpert PA, Weber TR, Bower RJ, Trimble JA, Micelli A, et al. The impact of surgery on infants born at extremely low birth weight. J Pediatr Surg. 2003;38(6):924–927. doi: 10.1016/s0022-3468(03)00125-8. [DOI] [PubMed] [Google Scholar]
- 18.Filan PM, Hunt RW, Anderson PJ, Doyle LW, Inder TE. Neurologic outcomes in very preterm infants undergoing surgery. J Pediatr. 2012;160(3):409–414. doi: 10.1016/j.jpeds.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Stolwijk LJ, Lemmers PM, Harmsen M, Groenendaal F, de Vries LS, van der Zee DC, et al. Neurodevelopmental outcomes after neonatal surgery for major noncardiac anomalies. Pediatrics. 2016;137(2):e20151728. doi: 10.1542/peds.2015-1728. [DOI] [PubMed] [Google Scholar]
- 20.Flick RP, Katusic SK, Colligan RC, Wilder RT, Voigt RG, Olson MD, et al. Cognitive and behavioral outcomes after early exposure to anesthesia and surgery. Pediatrics. 2011;128(5):e1053–61. doi: 10.1542/peds.2011-0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Loepke AW, Soriano SG. An assessment of the effects of general anesthetics on developing brain structure and neurocognitive function. Anesth Analg. 2008;106(6):1681–1707. doi: 10.1213/ane.0b013e318167ad77. [DOI] [PubMed] [Google Scholar]
- 22.Rappaport B, Mellon RD, Simone A, Woodcock J. Defining safe use of anesthesia in children. N Engl J Med. 2011;364(15):1387–1390. doi: 10.1056/NEJMp1102155. [DOI] [PubMed] [Google Scholar]
- 23.Williams RK. The pediatrician and anesthesia neurotoxicity. Pediatrics. 2011;128(5):e1268–70. doi: 10.1542/peds.2011-2489. [DOI] [PubMed] [Google Scholar]
- 24.Shah DK, Doyle LW, Anderson PJ, Bear M, Daley AJ, Hunt RW, et al. Adverse neurodevelopment in preterm infants with postnatal sepsis or necrotizing enterocolitis is mediated by white matter abnormalities on magnetic resonance imaging at term. J Pediatr. 2008;153(2):170–175. doi: 10.1016/j.jpeds.2008.02.033. [DOI] [PubMed] [Google Scholar]
- 25.Volpe JJ. Postnatal sepsis, necrotizing entercolitis, and the critical role of systemic inflammation in white matter injury in premature infants. J Pediatr. 2008;153(2):160–163. doi: 10.1016/j.jpeds.2008.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ikonomidou C, Bosch F, Miksa M, Bittigau P, Vöckler J, Dikranian K, et al. Blockade of NMDA receptors and apoptotic neurodegeneration in the developing brain. Science. 1999;283(5398):70–74. doi: 10.1126/science.283.5398.70. [DOI] [PubMed] [Google Scholar]
- 27.Jevtovic-Todorovic V, Hartman RE, Izumi Y, Benshoff ND, Dikranian K, Zorumski CF, et al. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J Neurosci. 2003;23(3):876–882. doi: 10.1523/JNEUROSCI.23-03-00876.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zou X, Liu F, Zhang X, Patterson TA, Callicott R, Liu S, et al. Inhalation anesthetic-induced neuronal damage in the developing rhesus monkey. Neurotoxicol Teratol. 2011;33(5):592–597. doi: 10.1016/j.ntt.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Brambrink AM, Back SA, Riddle A, Gong X, Moravec MD, Dissen GA, et al. Isoflurane-induced apoptosis of oligodendrocytes in the neonatal primate brain. Ann Neurol. 2012;72(4):525–535. doi: 10.1002/ana.23652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DiMaggio C, Sun LS, Kakavouli A, Byrne MW, Li G. A retrospective cohort study of the association of anesthesia and hernia repair surgery with behavioral and developmental disorders in young children. J Neurosurg Anesthesiol. 2009;21(4):286–291. doi: 10.1097/ANA.0b013e3181a71f11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kim GS, Song JG, Gwak MS, Yang M. Postoperative outcome in formerly premature infants undergoing herniorrhaphy: comparison of spinal and general anesthesia. J Korean Med Sci. 2003;18(5):691–695. doi: 10.3346/jkms.2003.18.5.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.The Victorian Infant Collaborative Study Group. Surgery and the tiny baby: sensorineural outcome at 5 years of age. J Paediatr Child Health. 1996;32(2):167–172. doi: 10.1111/j.1440-1754.1996.tb00916.x. [DOI] [PubMed] [Google Scholar]
- 33.McCormick MC, Brooks-Gunn J, Workman-Daniels K, Turner J, Peckham GJ. The health and developmental status of very low-birth-weight children at school age. JAMA. 1992;267(16):2204–2208. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Major congenital anomalies requiring surgery in Korean VLBW infants


