ABSTRACT
BACKGROUND:
Poisoning among the pediatric population is an important public health concern that is responsible for frequent pediatric emergency department visits and hospital admissions. Surveillance of poisoning cases is essential for designing and implementing effective preventive strategies.
OBJECTIVE:
Describe the characteristics of acute poison exposure and related therapeutic interventions in children aged 12 years and younger.
DESIGN:
Prospective, descriptive cross-sectional study.
SETTING:
Two pediatric emergency departments in Riyadh.
PATIENTS AND METHODS:
We prospectively reviewed pediatric poisonings that presented to emergency departments over a period of two years.
MAIN OUTCOME MEASURES:
Epidemiological aspects of pediatric poisoning Riyadh.
SAMPLE SIZE:
1035 patients.
RESULTS:
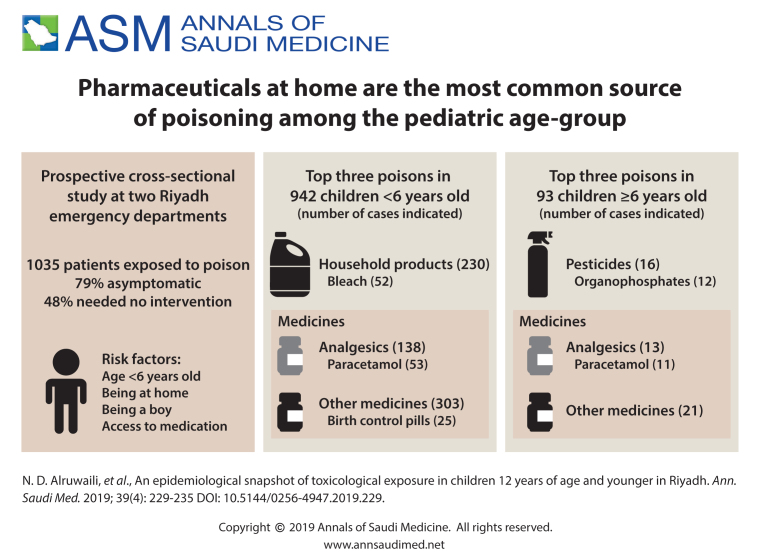
The median (IQR) age at the time of exposure was 27 (23–42) months. The most frequently involved substance class was toxic household products in children younger than 6 years and pesticides in children 6 years or older. A frequently involved single agent was paracetamol in younger and older children. The majority of patients (78.7%) were completely asymptomatic at the time of presentation and during the observation period. Almost half of the exposure incidents (47.8%) needed no intervention. Most exposure incidents (95%) did not require any pharmacological support and most (87%) did not require nonpharmacological intervention. Eight (0.7%) patients required intubation and mechanical ventilation. Activated charcoal was administered for 27% of cases. Gastric lavage, whole bowel irrigation, and ipecac were used in a few cases (1%, 0.3%, and 0.1%, respectively). Enhanced elimination interventions were performed for only 0.5% of exposure cases. Only two patients died.
CONCLUSIONS:
Household products were the commonest reason for pediatric poisonings in Saudi Arabia and most of them were asymptomatic. Our results suggest a need for strategic plans for prevention and care.
LIMITATIONS:
May not be representative of the experiences and practices of smaller hospitals in remote regions of the country.
CONFLICT OF INTEREST:
None.
INTRODUCTION
Poisoning among the pediatric population is an important public health concern that is responsible for frequent pediatric emergency department visits and hospital admissions.1 There is a bimodal age distribution among those exposed to poison, with a high incidence of toddlers, predominantly males, experiencing accidental exposure, and a high incidence of adolescents, predominantly female, experiencing intentional exposure.2,3 In 2015, the American Association of Poison Control Centers reported more than 1.3 million cases of poison exposure in the pediatric population. Children younger than 3 years comprised 40% of these cases, and children in all age groups accounted for approximately 60% of all human cases.4 Factors associated with the risk of poisoning in children include young age, female sex, low education level, and low socioeconomic status.5–9 A review conducted in Saudi Arabia reported that childhood poisonings accounted for 88% of the poison exposure cases reported to one poison control service in Riyadh, and 92% of these cases involved children younger than 5 years.10 Another study performed in Saudi Arabia reported that 7.2% of pediatric admissions were secondary to poisoning, and that hydrocarbon exposure was the cause of most of these admissions.11 The most common exposure categories vary from country to country, although medications were the main agents responsible for pediatric cases of poisoning in Saudi Arabia in previous studies.12–14 These exposure categories differ from that reported in other countries where toxic household products were implicated in the majority of pediatric exposure cases.5,15–17 Although most cases of pediatric exposure are asymptomatic or involve mild symptoms, ingesting a small amount of certain toxins can sometimes cause significant toxicity.18 Outcomes of poisoned pediatric patients in different areas are affected by the locally prevalent social, economic, and cultural practices, and by the availability and quality of medical facilities. Researchers from various countries have noted that significant toxic exposure-related problems are unique to their socioeconomic and cultural environments.19–26 Pediatric poisoning cases are increasing, particularly for children younger than 5 years, thereby indicating that efforts to prevent poisoning to date have been inadequate.27,28 Therefore, surveillance of poisoning cases is an essential step for designing and implementing effective preventive strategies. In this study, we reviewed patient characteristics, types of exposure, outcomes, clinical presentations, and the extent of therapeutic interventions for poisoning in pediatric patients presenting to emergency departments in Riyadh, Saudi Arabia.
PATIENTS AND METHODS
This multicenter prospective study was performed over the course of two years at two major pediatric emergency departments of two major community pediatric hospitals in Riyadh, Saudi Arabia (King Saud Medical City Hospital and Al Yamamah Pediatric Hospital). Each of these hospitals has approximately 150 000 annual pediatric emergency visits. These hospitals are affiliated with different institutes and were chosen to examine all socioeconomic population subgroups managed in Riyadh. We reviewed the characteristics of pediatric poisoning cases involving children 12 years or younger who presented to the emergency department. The investigation focused mainly on incidents involving medications or toxic household products; therefore, incidents of food poisoning, insect bites, scorpion stings, and snake bites were excluded from the analysis. Emergency physicians caring for the patients were required to complete a preformatted data collection sheet. All data were entered into a computerized database for subsequent analysis. These data included patient demographic data (age, sex), exposure time and place, time from exposure to presentation, duration of stay in the emergency department, type of exposure, route of exposure, clinical presentation, and management provided. Statistical analyses were performed using SPSS 16.0. Verbal informed consent was obtained by one of the investigators, and participants were informed about the goals of this study. The research ethical committee at our institute approved the study (project approval reference number 2131034), and a waiver of written consent was obtained. The investigator documented verbal consent in the medical chart. Patient confidentiality was protected throughout the study.
RESULTS
There were 1035 exposures involving children 12 years of age or younger except for 19 family members older than 12 years. Of these patients, 558 children (54%) presented to Al Yamamah Pediatric Hospital and 476 (46%) children presented to King Saud Medical City Hospital. The data were collected over the course of 2 years at these hospitals.
Age and Sex Distribution
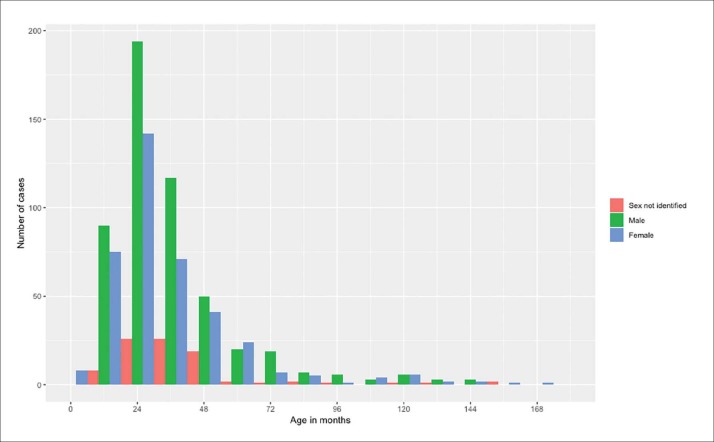
The median (IQR) age at the time of exposure was 27 (23-42) months. Children younger than 3 years were involved in 57% (n=586) of exposure cases, and children younger than 6 years accounted for 91% (n=942) of exposure cases (Figure 1). Male predominance was seen in all age groups (males: n=528 [51%]; females: 38% [n=394]). Sex was unidentified for 18% (n=113) of cases.
Figure 1.
Age and sex distribution of study population (n=1035).
Exposure
The most common location of exposure was the home (83%). However, 17% of exposure incidents happened at other places like health care facilities or schools. Most cases (46.6%; n=482) occurred between 6:00 pm and 12:00 am; however, cases that occurred between 12:00 pm and 6:00 pm and 12:00 am and 8:00 am comprised 25% (n=258) and 28% (n=290) of exposure cases, respectively. Poisoning incidents were significantly high (P<.001) during March (n=166; 16%) and April (n=207; 20%). Unintentional exposure incidents comprised 906 cases (87.7%) and were the most common reason for emergency visits reported in this study. Intentional exposure incidents were reported for 2.1% (n=22) of cases. The reason for exposure (intentional or unintentional) was not mentioned for approximately 10% (n=104) of incidents. Ingestion was the most common route of exposure (93%), followed by dermal exposure (2.7%), inhalation (1.6%), and eye exposure (0.9%).
The most frequently involved substance category was toxic household products, followed by analgesics in children younger than 6 years of age (Table 1A). For children 6 years of age or older, the top classes were pesticides and analgesics (Table 1B). In younger children, the most frequent single agent involved was paracetamol, followed by sodium hypochlorite (Table 2A). In about half of cases, the exact amount ingested was unknown (52.5%). For older children, pesticides, particularly organophosphorus compounds, were the most common cause of poisoning in children 6 years or older (Table 2B). A single substance was reported in most cases of exposure (974 exposure cases; 94%). However, 6% of patients were exposed to two or more substances. Fifty percent of exposure incidents were reported within 1 hour (median time, 1 hour; range, 7 minutes-48 hours), and 79% of exposure incidents were reported within 2 hours.
Table 1A.
Top ten classes of poisons in children younger than 6 years of age.
| Toxic household product (not caustics) | 178 (17.2) |
| Analgesics | 138 (13.4) |
| Other pharmaceuticals | 99 (9.6) |
| Anticholinergics/antihistamines | 57 (5.5) |
| Cardiovascular drugs | 56 (5.4) |
| Endocrine/hormones/steroids | 52 (5.0) |
| Herbal/dietary supplements/vitamins | 42 (4.1) |
| Hydrocarbons (petroleum products) | 40 (3.9) |
| Antipsychotics | 39 (3.8) |
| Other nonpharmaceuticals | 37 (3.6) |
Data are number (percentage). Analgesics: paracetamol, aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs. Toxic household products such as perfumes, essential oils and products with acetone.
Table 1B.
Top ten classes of poisons in children and in children 6 years of age or older.
| Pesticides | 16 (1.6) |
| Analgesics | 13 (1.3) |
| Other pharmaceutical | 8 (0.8) |
| Antipsychotics | 7 (0.7) |
| Other non pharmaceuticals | 5 (0.5) |
| Gas/vapors/irritants/dusts | 4 (0.4) |
| Alcohols | 4 (0.4) |
| Households (not caustics) | 4 (0.4) |
| Anticholinergics/antihistamines | 3 (0.3) |
| Antimicrobials | 3 (0.3) |
Data are number (percentage). Analgesics: paracetamol, aspirin, acetaminophen, nonsteroidal anti-inflammatory drugs.
Table 2B.
Top single agents of poisoning in children and children 6 years of age or older.
| Organophosphorus pesticides | 12 (1.2) |
| Paracetamol | 11 (1.1) |
| Carbon monoxide | 3 (0.3) |
| Lyrica | 3 (0.3) |
| Amlodipine | 3 (0.3) |
| Risperidone | 3 (0.3) |
| Amphetamine | 2 (0.2) |
| Metronidazole | 2 (0.2) |
| Scorpion sting | 2 (0.2) |
| Insecticides | 2 (0.2) |
Data are number (percentage).
Table 2A.
Top single agents of poisoning in children younger than 6 years of age.
| Paracetamol | 53 (5.1) |
| Sodium hypochlorite (Clorox bleach) | 52 (5.0) |
| Ibuprofen | 40 (3.9) |
| Rat poison | 26 (2.5) |
| Birth control pills | 25 (2.2) |
| Kerosene | 23 (2.2) |
| Aspirin | 22 (2.1) |
| Salbutamol (Ventolin inhaler) | 17 (1.6) |
| Loratadine | 17 (1.6) |
| Perfume | 16 (1.6) |
Data are number (percentage).
Clinical presentation
The majority of patients (813 exposure cases; 78.7%) were completely asymptomatic at the time of presentation and during the observation period. For symptomatic patients, vomiting was the most common symptom (4.6%), followed by decreased consciousness (3.68%).
Duration of stay in the emergency department
Three hundred (29%) patients were discharged immediately after assessment in the emergency department, whereas 497 (48%) underwent extended observation in the emergency department before being discharged home; the median observation time was 6 hours. Two hundred twenty (21%) patients were admitted: 149 (14.4%) patients were admitted to the pediatric ward and 71 (6.8%) were admitted to the pediatric intensive care unit (Figure 2). Cardiovascular drugs (24%), followed by sedatives, hypnotics, and antipsychotics (14%) and anticonvulsants (10%), were the most common substances responsible for pediatric intensive care unit admissions (Table 3). Poison centers were called for advice for only 18% of all exposure cases.
Figure 2.
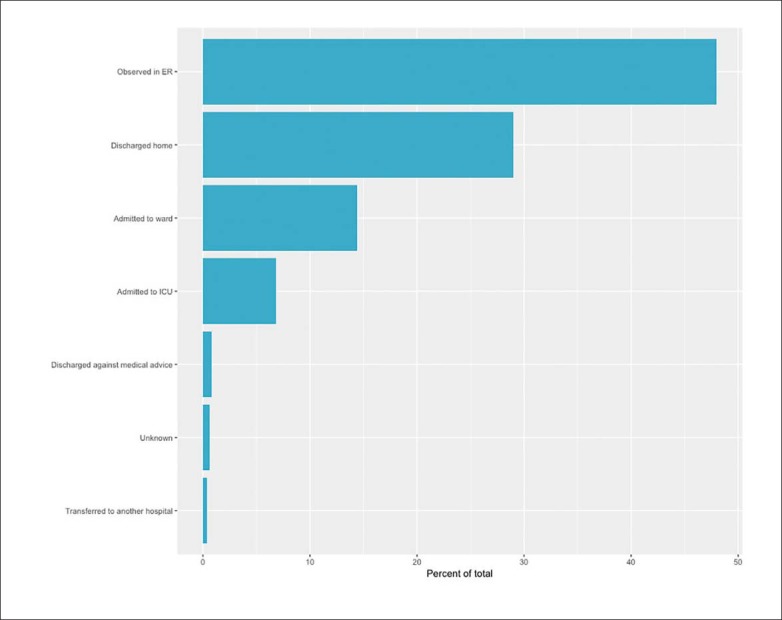
Outcomes of poison exposure cases (n=1035).
Table 3.
Substances involved in pediatric intensive care unit admissions (71 exposures).
| Cardiovascular drugs | 17 | 23.9 |
| Sedative/hypnotics/antipsychotics | 10 | 14.1 |
| Anticonvulsants | 7 | 9.9 |
| Organophosphates | 6 | 8.5 |
| Corrosives | 4 | 5.6 |
| Sulfonylurea | 2 | 2.8 |
| Antidepressants | 2 | 2.8 |
| Others (each one case) | 23 | 32.4 |
| Total | 71 | 100 |
Data are number (percentage).
Exposure-related fatalities
Two patients (0.19%) died due to pesticide exposure. These patients were 9- and 7-year-old siblings who presented 6 hours after a significant amount of an organophosphorus compound (Diazinon) was applied by their parents to their hair for lice treatment. Both presented with significantly decreased consciousness and severe bradycardia that progressed to asystole and death despite full resuscitative measures.
Management, decontamination, antidotes, and chelating agents
Almost half of the patients (495 exposure cases; 47.8%) did not need any intervention, and most patients (986 exposure cases; 95%) did not require any pharmacological support. The majority of exposure cases (901; 87%) did not require any nonpharmacological intervention, but eight (0.7%) patients required intubation and mechanical ventilation. Most patients (707 exposure cases; 68%) did not require any decontamination intervention. Activated charcoal was the main method of gastrointestinal decontamination (284 exposure cases; 27%), followed by skin or eye irrigation (24 exposure cases; 2%). Gastric lavage, whole bowel irrigation, and ipecac were rarely used (1%, 0.3%, and 0.1%, respectively). Most exposures (996 cases; 96.4%) did not require any antidote and were managed only with supportive symptomatic therapy; however, a few exposure cases required antidotes such as atropine (15 exposure cases; 1.5%) or N-acetyl cysteine (8 exposure cases; 0.7%). Enhanced elimination interventions like multiple doses of activated charcoal or urinary alkalinization were used for six (0.5%) poisoning cases. Chelating therapy was used for one case of exposure; the patient was administered deferoxamine for iron toxicity.
DISCUSSION
Acute poisoning is considered one of the important causes of emergency department visits in the pediatric population. Recognizing the pattern of exposure, available interventions, and current practice is required to build a comprehensive approach and management guidelines for such cases as well as planning preventable measures. A study by Al-Sekait et al showed that accidental poisoning is a major problem in Saudi Arabia, and this was also demonstrated in our study.17 Studies from other countries such as United States, Taiwan, and Egypt showed similar findings.1,2,27 The high frequency of poisoning in the pediatric population is similar to that reported by many other studies performed in Saudi Arabia and other countries worldwide.4,5,7 Accidental poisoning is still the most common type of exposure in the pediatric population. The problem is always underestimated because of under-reporting.27 We found that exposure to toxic household products (17.6%) was the most common cause of pediatric poisoning, particularly sodium hypochlorite (54 exposure cases; 5.2% of the total exposure cases), followed by analgesics (14.6%), particularly paracetamol. Over the course of 2 years, there were two peaks of high numbers of cases in March and April. School breaks occur during these periods in Saudi Arabia; therefore, children spend more time at home, where they have more access to poisons if not supervised carefully. This could possibly explain the higher frequency of unintentional pediatric poisoning cases during those times.
The most common route of poisoning was ingestion (93%), followed by dermal exposure (3%). Age is always a significant factor associated with poison exposure in the pediatric population. In our study, the exposure was highest (91%) among children younger than 6 years. The mean age of exposure was 31 months, and these patients were predominantly male. This sex difference in exposure to poison was observed in other studies conducted in Saudi Arabia;29 however, it was not reported in one study conducted in Riyadh.17 The age distribution in our study was similar to that of other reports.10,17 Furthermore, 51% of exposure cases occurred in children 12 to 35 months of age. These findings highlight the challenges associated with the desire of children in this age group to put things in their mouths, thus necessitating the application of child-resistant packaging. Child-resistant containers are recommended because many studies have shown that their use significantly decreased the number of cases of accidentally ingested poison.27
The most common agents ingested in the study by children younger than 6 years were toxic household products (17.2%), followed by analgesics (13.4%) and other pharmaceuticals (9.6%). The most common pharmaceutical ingested was paracetamol (5.1%). These results are similar to those of other studies. Children older than 6 years were most commonly exposed to pesticides (1.6%), with organophosphates being the most common (1.2%); paracetamol (1.06%) was the second most common cause of poisoning in children older than 6 years. Another study performed in Jeddah in Saudi Arabia reported that pediatric patients in that region who visited the emergency department because of poisoning were most commonly exposed to a hydrocarbon.11 However, Al Hazmi et al analyzed patients admitted for poisoning so that study was different than our study. Additionally, the geographic location might have contributed to the differences in the types of exposure.
Outcomes of exposure to toxins depend on many factors, including age, whether the agent is pharmaceutical or non-pharmaceutical, amount of exposure, time of exposure, time from exposure to presentation to a healthcare facility, and time of intervention. The majority of patients were asymptomatic on presentation to the emergency department, and they remained so during their stay (78.7%). Among those who developed signs and symptoms, gastrointestinal manifestations were the most common symptoms (4.6%), followed by neurological manifestations (3.7%). Most of the exposed patients in this study required only a period of observation in the emergency department or were discharged home immediately (48% and 29%, respectively), with a median observation time of 6 hours. Admission was required for 21% of patients, of whom 6.8% required care in the pediatric intensive care unit. Cardiovascular drugs (24%), followed by sedatives, hypnotics, and antipsychotics (14%) and anticonvulsants (10%), were the most common substances responsible for pediatric intensive care unit admissions. This might have been related to the seriousness of the class of medication ingested rather than the dose. Although the most common pharmaceutical that patients were exposed to was paracetamol, only a small percentage of cases required the antidote, N-acetylcysteine. This can be explained by the limited amount of paracetamol per container and early detection and early presentation to the emergency department.
In our study, only two fatal cases were reported (0.19%); these two fatalities were due to exposure to an organophosphorus compound that was misused at home, resulting in cardiopulmonary arrest and death. Previous studies in the same region have higher reported mortality rates ranging from 1.5% to 4.6%. The lower mortality rate in our study might have been related to easy access and early presentation to the emergency department (within 60 minutes for 57% of exposureincidents and within 61–120 minutes for 12% of exposure incidents) where necessary lifesaving interventions can be done immediately. Furthermore, this could be attributed to under-reporting of poisoning cases, which is considered one of the major challenges of poisoning management. The majority of cases only required observation. Poison consultation services were utilized for only 18% of total exposure cases. However, the benefits of involving the poison control center in managing poisoning cases have been well-documented and proven by different studies. Therefore, increased awareness of the importance of consulting the poison control center is warranted to improve patient care.
There were some limitations to this study. It was performed at two large community hospitals in the capital city of Saudi Arabia; therefore, it may not be representative of the experiences and practices of smaller hospitals in remote regions of the country. Moreover, some cases that did not require medical care were not included in this study. Furthermore, our search showed that the literature is lacking in evaluations of the demographics of poisoning cases and of the circumstances of toxic exposure in a large pediatric population-based studies in Saudi Arabia. We believe that a multicenter pediatric hospital-based study will help fill this void. In conclusion, childhood toxic exposures are quite significant in Saudi Arabia, which dictates rapid recognition and institution of measures of prevention and early intervention. An integration of an established national poison control center with healthcare facilities is highly recommended.
ACKNOWLEDGMENTS
The authors thank all the physicians, nurses, and epidemiologists who contributed to this study.
Funding Statement
None.
REFERENCES
- 1.Franklin RL, Rodgers GB. Unintentional child poisonings treated in United States hospital emergency departments: national estimates of incident cases, population-based poisoning rates, and product involvement. Pediatrics 2008;122(6):1244–51. [DOI] [PubMed] [Google Scholar]
- 2.Azab SM, Hirshon JM, Hayes BD, El-Setouhy M, Smith GS, Sakr ML, et al. . Epidemiology of acute poisoning in children presenting to the poisoning treatment center at Ain Shams University in Cairo, Egypt, 2009-2013. Clin Toxicol (Phila) 2016;54(1):20–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hincal F, Hincal AA, Müftü Y, Sarikayalar F, Ozer Y, Cevik N, et al. . Epidemiological aspects of childhood poisonings in Ankara: a 10-year survey. Hum Toxicol. 1987;6(2):147–52. [DOI] [PubMed] [Google Scholar]
- 4.Mowry JB, Spyker DA, Brooks DE, Zimmerman A, Schauben JL. 2015 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 33rd Annual Report. Clin Toxicol (Phila) 2016;54(10):924–1109. [DOI] [PubMed] [Google Scholar]
- 5.Lamireau T, Llanas B, Kennedy A, Fayon M, Penouil F, Favarell-Garrigues JC, et al. . Epidemiology of poisoning in children: a 7-year survey in a paediatric emergency care unit. Eur J Emerg Med 2002;9(1):9–14. [DOI] [PubMed] [Google Scholar]
- 6.Andiran N, Sarikayalar F. Pattern of acute poisonings in childhood in Ankara: what has changed in twenty years? Turk J Pediatr 2004;46(2):147–52. [PubMed] [Google Scholar]
- 7.Mintegi S, Fernández A, Alustiza J, Canduela V, Mongil I, Caubet I, et al. . Emergency visits for childhood poisoning: a 2-year prospective multicenter survey in Spain. Pediatr Emerg Care 2006;22(5):334–8. [DOI] [PubMed] [Google Scholar]
- 8.Shannon M. Ingestion of toxic substances by children. N Engl J Med 2000;342(3):186–91. [DOI] [PubMed] [Google Scholar]
- 9.Lin YR, Liu TH, Liu TA, Chang YJ, Chou CC, Wu HP. Pharmaceutical poisoning exposure and outcome analysis in children admitted to the pediatric emergency department. Pediatr Neonatol 2011;52(1):11–7. [DOI] [PubMed] [Google Scholar]
- 10.Saddique A. Poisoning in Saudi Arabia: ten-year experience in King Khaled University Hospital. Ann Saudi Med 2001;21(1-2):88–91. [DOI] [PubMed] [Google Scholar]
- 11.Al Hazmi AM. Patterns of accidental poisoning in children in Jeddah, Saudi Arabia. Ann Saudi Med 1998;18(5):457–9. [DOI] [PubMed] [Google Scholar]
- 12.Al-Shehri MA. Pattern of childhood poisoning in Abha city - southwestern Saudi Arabia. J Family Community Med 2004;11(2):59–63. [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Barraq A, Farahat F. Pattern and determinants of poisoning in a teaching hospital in Riyadh, Saudi Arabia. Saudi Pharm J 2011;19(1):57–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahdi AH, Taha SA, Al Rifai MR. Epidemiology of accidental home poisoning in Riyadh (Saudi Arabia). J Epidemiol Community Health 1983;37(4):291–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marchi AG, Renier S, Messi G, Barbone F. Childhood poisoning: a population study in Trieste, Italy, 1975-1994. J Clin Epidemiol 1998;51(8):687–95. [DOI] [PubMed] [Google Scholar]
- 16.Oguche S, Bukbuk DN, Watila IM. Pattern of hospital admissions of children with poisoning in the Sudano-Sahelian North eastern Nigeria. Niger J Clin Pract 2007;10(2):111–5. [PubMed] [Google Scholar]
- 17.Al-Sekait MA. Accidental poisoning of children in Riyadh, Saudi Arabia. J R Soc Health 1989;109(6):204–5, 208. [DOI] [PubMed] [Google Scholar]
- 18.Liebelt EL, DeAngelis CD. Evolving trends and treatment advances in pediatric poisoning. JAMA 1999;282(12):1113–5. [DOI] [PubMed] [Google Scholar]
- 19.Fathelrahman AI, Ab Rahman AF, Mohd Zain Z. MS 04-044: demographic features of drug and chemical poisoning in northern Malaysia. Clin Toxicol (Phila) 2005;43(2):89–94. [PubMed] [Google Scholar]
- 20.Akkose S, Bulut M, Armagan E, Cebicci H, Fedakar R. Acute poisoning in adults in the years 1996-2001 treated in the Uludag University Hospital, Marmara Region, Turkey. Clin Toxicol (Phila) 2005;43(2):105–9. [PubMed] [Google Scholar]
- 21.Afshari R, Majdzadeh R, Balali-Mood M. Pattern of acute poisonings in Mash-had, Iran 1993-2000. J Toxicol Clin Toxicol 2004;42(7):965–75. [DOI] [PubMed] [Google Scholar]
- 22.Goksu S, Yildirim C, Kocoglu H, Tutak A, Oner U. Characteristics of acute adult poisoning in Gaziantep, Turkey. J Toxicol Clin Toxicol 2002;40(7):833–7. [DOI] [PubMed] [Google Scholar]
- 23.Hanssens Y, Deleu D, Taqi A. Etiologic and demographic characteristics of poisoning: a prospective hospital-based study in Oman. J Toxicol Clin Toxicol 2001;39(4):371–80. [DOI] [PubMed] [Google Scholar]
- 24.Thomas SH, Bevan L, Bhattacharyya S, Bramble MG, Chew K, Connolly J, et al. . Presentation of poisoned patients to accident and emergency departments in the north of England. Hum Exp Toxicol 1996;15(6):466–70. [DOI] [PubMed] [Google Scholar]
- 25.Chan TY, Critchley JA, Chan MT, Yu CM. Drug overdosage and other poisoning in Hong Kong–the Prince of Wales Hospital (Shatin) experience. Hum Exp Toxicol 1994;13(7):512–5. [DOI] [PubMed] [Google Scholar]
- 26.Liu Y, Wolf LR, Zhu W. Epidemiology of adult poisoning at China Medical University. J Toxicol Clin Toxicol 1997;35:175–180 [DOI] [PubMed] [Google Scholar]
- 27.Yang CC, Wu JF, Ong HC, Kuo YP, Deng JF, Ger J. Children poisoning in Taiwan. The Indian Journal of Pediatrics 1997 Jul 1;64(4):469–83. [DOI] [PubMed] [Google Scholar]
- 28.Bond GR, Woodward RW, Ho M. The growing impact of pediatric pharmaceutical poisoning. J Pediatr. 2012. Feb;160(2):265–270.e1. [DOI] [PubMed] [Google Scholar]
- 29.Izuora GI, Adeoye A. A seven-year review of accidental poisoning in children at a military hospital in Hafr Al Batin, Saudi Arabia. Ann Saudi Med. 2001;21(1-2):13–15. [DOI] [PubMed] [Google Scholar]