Abstract
A fracture liaison service (FLS) is a secondary fracture prevention program that is led by a coordinator. A program called the osteoporosis liaison service (OLS), which includes FLS, was first implemented in Japan and has become popular for solving problems related to osteoporosis treatment. OLS and FLS have the same purpose, namely preventing fragility fractures, but while FLS focuses mainly on secondary fracture prevention in fracture patients, OLS addresses this issue as well as primary fracture prevention at clinics and in communities.
Keywords: Osteoporosis liaison service, Fragility fractures
1. Introduction
Fragility fractures compromise physical function and impair daily activities in older people. In particular, hip fractures are the most common cause of reduced mobility and life expectancy in older people. In Japan, the annual incidence of hip fractures was estimated to be 190,000 in 2012, and is expected to be 300,000 in 2040 [1]. The incidences in China, India, and South Korea in 2018 were 484,941, 331,898, and 20,892, respectively, and are expected to markedly increase to 1,165,728, 792,334, and 59,466 in 2050, respectively [2]. Therefore, there is an urgent need to prevent fragility fractures, including hip fractures, in Asian countries.
Methods of preventing fragility fractures include treating osteoporosis and preventing falls. Dual-energy X-ray absorptiometry, invented in the 1980s, revealed a strong correlation between bone density and fracture risk. More recently, diagnostic criteria and drugs for osteoporosis have been developed. However, more than half of patients with hip fractures are not diagnosed with osteoporosis based on bone density before the start of follow-up [3]. This indicates that bone density alone is insufficient to accurately identify patients who will benefit from preventive care for fractures.
Fracture risk factors include bone density as well as a history of fragility fractures. A fracture liaison service (FLS) is a secondary fracture prevention program that is led by a coordinator (liaison) [4]. FLS programs were first implemented in European countries and are now used worldwide to effectively prevent hip fractures. A program called the osteoporosis liaison service (OLS), which includes FLS, was first implemented in Japan and has become popular for solving problems related to osteoporosis treatment.
2. Fracture liaison service
2.1. Background
A meta-analysis showed that histories of wrist fractures and vertebral fractures increased the risk of hip fractures by 1.9- and 2.3-fold, respectively [5]. Approximately 16% of all postmenopausal women have a history of fragility fractures, and this group accounts for 50% of all hip fracture cases [4]. This indicates that women with a history of fragility fractures have a very high risk of fractures; therefore, it is important to focus on this group when implementing preventive measures for primary or secondary fractures. Patients with fragility fractures are easily identified since they must visit medical facilities for treatment, and they are generally willing to provide consent to receive osteoporosis treatment to prevent fractures because they have already experienced fracture-related pain and limitation in daily activities.
However, it is known that the implementation rate of secondary fracture prevention is very low. A Japanese study in 1445 patients with a fracture of the distal end of the radius [6] reported that after the fracture, bone density was measured in only 126 patients (8.7%) and treatment for osteoporosis was performed in only 193 patients (13.4%). Another study in Japan [7] reported that the medication rates for osteoporosis in patients with hip fractures, fractures of the distal end of the radius, fractures of the proximal end of the humerus, and clinical fractures of the vertebrae were only 29%, 20%, 30%, and 50%, respectively. These low rates of secondary fracture prevention are seen in other countries as well, and increasing these rates is an important goal.
2.2. Development of FLS
To solve these issues, FLS, a program for secondary fracture prevention that is managed by a coordinator, was started in the late 1990s in the United Kingdom [4,8]. FLS can effectively prevent fractures of all kinds, and thus decreases the incidence of fragility fractures, including hip fractures [9,10]. In addition, it has been reported that FLS improves survival rates [11,12]. After the publication of guidelines on the use of antiosteoporosis therapies, including generic alendronate administration, 14% and 22% reductions were observed in the incidences of refractures of major fragility fractures and hip fractures, respectively, at 3 years after intervention [13].
Ganda et al. [14] grouped studies on FLS into 4 types based on the nature of the FLS — type A: identification, assessment, and treatment of patients as part of the service; type B: similar to A, without treatment initiation; type C: alerting patients and also primary care physicians; and type D: patient education only. Meta-analyses of each type of study revealed that type A resulted in the highest rate of bone density testing and treatment initiation, followed by type B.
2.3. Effectiveness of FLS
It is known that FLS is cost-effective because it prevents fragility fractures [15,16]. When 740 of 1000 patients with fragility fractures are determined by a doctor to require treatment for osteoporosis, fracture prevention care is provided for only 193 of them; in a FLS program, on the other hand, it is provided for 686 patients. As a result, fractures can be prevented in 18 patients (11 with hip fractures) and the expenses for fracture treatment and associated care can be reduced [15]. Therefore, FLS contributes to the reduction of medical expenses. A study on the cost-effectiveness of FLS in Japanese people reported that secondary fracture prevention by FLS reduced costs relative to no therapy in patients with a family history of hip fracture and high alcohol intake [17]. These findings show that FLS effectively improves activities of daily living, quality of life, and life expectancy, and also lowers medical expenses.
FLS has been shown to be expected to be a breakthrough for the treatment of osteoporosis because of its high treatment efficacy and cost-effectiveness. Therefore, various organizations, including the International Osteoporosis Foundation, Fragility Fracture Network (http://fragilityfracturenetwork.org/), National Osteoporosis Foundation, International Society for Fracture Repair (http://www.fractures.com/index.html), and AO Foundation (https://www.aofoundation.org/), recommend and promote FLS.
FLS was initially launched in the United Kingdom and has spread to other European countries as well as the North America. In the Asia-Pacific region, it is actively provided in Australia and New Zealand [18]. A systematic review of the literature on FLS in the Asia-Pacific region [19] identified 37 studies.
3. Osteoporosis liaison service
3.1. Background
Issues in the treatment of osteoporosis are not only the lower rate of pharmaceutical treatment in patients with fragility fractures, that is secondary fracture prevention, but also primary fracture prevention. The rate of pharmaceutical treatment in patients with osteoporosis has been reported to be very low in Japan. Thus, it is necessary to initiate treatment for patients with fragility fractures and also to administer osteoporosis treatment in patients without fragility fractures. Only one-third of patients with vertebral fractures are diagnosed at a medical institution [7]; therefore, undiagnosed vertebral fractures and initiating treatment are important considerations. Additionally, the first-line treatment of osteoporosis is the weekly administration of bisphosphonates, but adherence decreases to 50% after 1 year [20]. Improving drug adherence will enable fracture prevention. Given these considerations, it is important to achieve a focus on primary fracture prevention through increased awareness of osteoporosis at regional medical institutions and to improve drug adherence, in addition to preventing secondary fractures through FLS. OLS was developed to address these considerations (Fig. 1).
Fig. 1.
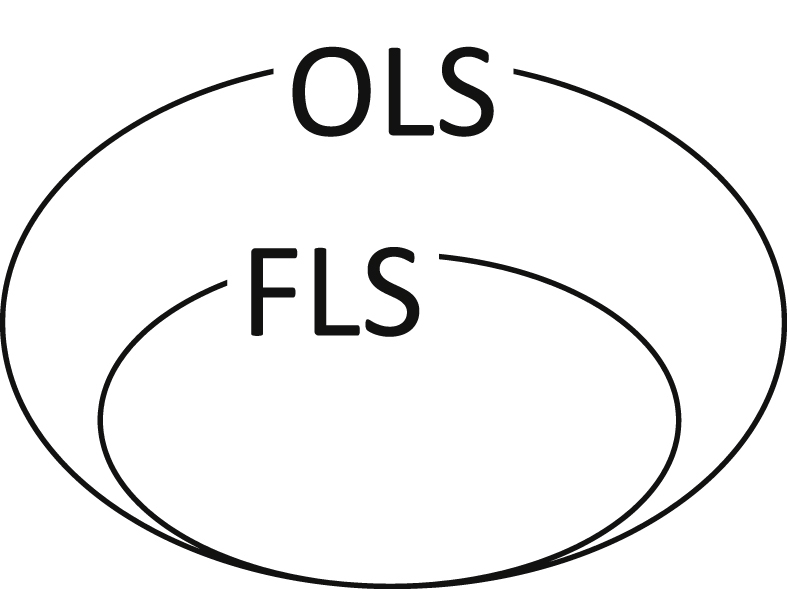
Concept of osteoporosis liaison service (OLS) and fracture liaison service (FLS) in Japan.
3.2. Development of OLS
OLS was started in 2011 in Japan. Coordinators who are knowledgeable about osteoporosis and who play a central role in OLS began to be certified as osteoporosis managers (OMs) by the Japan Osteoporosis Society in 2015 [21]. Candidate OMs are medical staff who engage in medical, healthcare, and educational practices at a hospital, clinic, or nursing care facility. Specifically, they are staff who are nationally certified as nurses, public health nurses, pharmacists, physical therapists, registered dietitians, social workers, care workers, and so on. The OM certification is given to those who participate in a specific lecture course and pass a qualification test (http://www.josteo.com/). Total 3061 people had been certified as OMs until March 2019, and of these, 51% were nurses, 18% were physical therapists, and 17% were pharmacists, 14% were others.
3.3. Features of OLS
Table 1 shows the differences between OLS and FLS. Both have the same purpose, namely preventing fragility fractures, but while FLS focuses mainly on secondary fracture prevention in fracture patients, OLS addresses this issue as well as primary fracture prevention at clinics and in communities. At hospitals where FLS is provided, an OM functions as a coordinator. In clinics, OMs provide instruction on the use of drugs, encourage patients to continue taking drugs, screen patients who visit the clinic for other diseases to identify those who require evaluation of fracture risk, and provide lifestyle guidance. In communities, OMs lead public awareness campaigns about osteoporosis and promote osteoporosis screening.
Table 1.
Fracture liaison service (FLS) and osteoporosis liaison service (OLS).
| Institution type | FLS |
OLS |
||||||
|---|---|---|---|---|---|---|---|---|
| Objective | Content | Patient population | Implemented by | Objective | Content | Patient population | Implemented by | |
| Hospital specializing in fracture treatments | Secondary fracture prevention | 5Isa | Fragile fracture | Coordinatorb | Secondary fracture prevention | 5Isa, OLS7c | Fragile fracture | Coordinatord |
| Walk-in clinic | Not applicable | – | – | – | Primary and secondary fracture prevention | OLS7c | Osteoporosis with no prior fractures/receiving treatment for nonosteoporosis conditions | Coordinatord |
| Outpatient pharmacy | Not applicable | – | – | – | Primary and secondary fracture prevention | Investigation of drug treatment/education on improving adherence/collaborative healthcare consultation regarding osteoporosis | Receiving treatment for osteoporosis | Coordinatord |
| Other institutions in the community | Not applicable | – | – | – | Primary fracture prevention | Societal awareness of osteoporosis/education on osteoporosis diagnosis | Local residents | Coordinatord |
a Identification, investigation, information, intervention, integration, b Nurses or other health professionals, c Risk evaluation using the fracture risk tool, confirmation of fractures and comorbidities, evaluation of nutritional status, evaluation of exercise and fall risk, evaluation of medications, quality of life and activities of daily living, structure of collaborative health care system, d Osteoporosis managers (Nurses, therapists, pharmacists, registered dietitians, radiologists, and so on).
The main reason why FLS has been promoted is because it is highly cost-effective. Screening for osteoporosis and providing interventions for patients without fractures are less cost-effective than FLS. Nevertheless, these activities are necessary because there is insufficient public understanding about the severity and treatment of osteoporosis and the importance of preventing fragility fractures. In Japan, FLS has been promoted through OM certification by the Japan Osteoporosis Society and by OLS activities.
OMs perform a variety of activities related to primary and secondary fracture prevention. Individuals involved in the former operate mostly at the regional or clinic level. An example of how primary fracture prevention is accomplished is through awareness-related activities for osteoporosis during health examinations and consultations. Bone density measurements and/or fracture risk assessment using fracture risk assessment tool (ex. Fracture Risk Assessment Tool, FRAX [22]) are conducted during these health examinations, which is in turn used to raise awareness about osteoporosis. Patients with suspected osteoporosis or a high fracture risk are subsequently referred to a hospital. OMs also provide guidance regarding osteoporosis drugs, guidance on improving adherence, and fracture risk evaluations at medical institutions as a part of their activities related to primary fracture prevention.
Secondary fracture prevention is conducted according to the 5Is proposed by the National Osteoporosis Society [23]: identification, investigation, information, intervention, and integration. OMs identify inpatients hospitalized for fracture-related surgeries or outpatients receiving conservative treatments for fractures, in order to request bone density measurements for these patients. They also evaluate the risks of fracture and fall. Patients requiring treatment or interventions receive education, treatment with osteoporosis drugs, nutritional guidance from a dietician, medication-related guidance from a pharmacist, and exercise and fall prevention guidance from a physical therapist. OMs share the gathered information with the primary care physician, and secondary fracture prevention is accomplished through this collaboration.
The effectiveness of OLS has been evaluated in 2 studies. The first study assessed medication adherence before and after the introduction of OLS in patients being treated for hip fractures or vertebral fractures in a general hospital and noted a significant improvement in adherence after OLS [24]. A similar study at a hospital, where from acute to rehabilitation treatment are performed, noted significant improvement in the diagnosis of osteoporosis and in medication adherence after OLS in patients with initial hip fractures [25]. There are also several reports about primary and secondary fracture prevention by OMs [26,27]. In one report registered dietitian propose appropriate nutrition guidance to patients with osteoporosis after evaluating their lifestyle [26]. In another report physical therapists evaluate the fall risk in patients with osteoporosis using the motor function tests [27]. In another report of OLS multidiscipline interventions for osteoporosis patients have improved their medication adherence [28]. These reports indicate that OLS might improve the overall treatment of osteoporosis; however, interventional studies with control are lacking, and future studies are warranted. Although there are many benefits of the multidisciplinary OLS approach, most OMs perform OLS in addition to other full-time duties, highlighting the need to address issues associated with the OLS approach (Table 2).
Table 2.
Benefits and difficulties associated with osteoporosis liaison service.
| Benefits | Health care professionals' deepened understanding of osteoporosis treatments |
| Broad improvements in osteoporosis treatment |
|
| Difficulties | Cost-effectiveness has not been investigated |
| Not yet covered by health insurance | |
| Osteoporosis managers have limited activities depending on institution or role |
Excludes fracture liaison service-related activities.
There are several issues with the Japanese OLS. One is that secondary fracture prevention is not covered by public health insurance. At present, FLS is supported by the voluntary efforts of individual medical facilities to prevent secondary fractures in fracture patients. Without further support for FLS by public health insurance coverage, the spread of FLS will be limited. Second, the diagnosis procedure combination reimbursement system has been introduced in many acute-care and rehabilitation hospitals. Under this system, the expense of prescribed drugs is included in the treatment expense specified for a condition. Therefore, hospitals tend to minimize drug prescriptions, including those for antiosteoporosis drugs. Third, OMs include various professionals as mentioned above. They conduct their OM activities, which include not only secondary but also primary fracture prevention, at a variety of facilities, including hospitals, clinics, dispensing pharmacies, and nursing care facilities, and their activities should be tailored according to their profession. While FLS has a 15-year history and relevant manuals have been prepared globally, there are only a few models of the Japanese OLS for primary fracture prevention that are helpful for OMs. Recently, however, reports on OLS activities have been provided by various professionals. Therefore, the prevention of primary and secondary fractures by OMs is expected to become more widespread.
To promote and develop OLS, it is essential to increase public understanding of the severity of fragility fractures and the importance of their prevention in Japan.
Conflicts of interest
HH has received consulting fees, lecture fees, or grants outside the submitted work from Asahi Kasei Pharma Corp., Astellas Pharma Inc., Chugai Pharmaceutical Co., Ltd., Eisai Co., Ltd., Eli Lilly Japan Co., Ltd., Mitsubishi Tanabe Pharma Corp., Mochida Pharmaceutical Corp., Ono Pharmaceutical Co., Ltd., Pfizer Inc., Taisho Toyama Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd.,Teijin Pharma Co., Ltd., and Daiichi Sankyo Co., Ltd.
Except for that, no potential conflict of interest relevant to this article was reported. ORCID. Hiroshi Hagino: 0000-0001-8053-1095. Takashi Wada: 0000-0002-2902-9427.
Footnotes
Peer review under responsibility of The Korean Society of Osteoporosis.
References
- 1.Hagino H. Fragility fracture prevention: review from a Japanese perspective. Yonago Acta Med. 2012;55:21–28. [PMC free article] [PubMed] [Google Scholar]
- 2.Cheung C.L., Ang S.B., Chadha M., Chow E.S., Chung Y.S., Hew F.L. An updated hip fracture projection in Asia: the Asian Federation of Osteoporosis Societies study. Osteoporos Sarcopenia. 2018;4:16–21. doi: 10.1016/j.afos.2018.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wainwright S.A., Marshall L.M., Ensrud K.E., Cauley J.A., Black D.M., Hillier T.A. Hip fracture in women without osteoporosis. J Clin Endocrinol Metab. 2005;90:2787–2793. doi: 10.1210/jc.2004-1568. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell P.J. Fracture liaison services: the UK experience. Osteoporos Int. 2011;22(Suppl 3):487–494. doi: 10.1007/s00198-011-1702-2. [DOI] [PubMed] [Google Scholar]
- 5.Klotzbuecher C.M., Ross P.D., Landsman P.B., Abbott T.A., 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 6.Baba T., Hagino H., Nonomiya H., Ikuta T., Shoda E., Mogami A. Inadequate management for secondary fracture prevention in patients with distal radius fracture by trauma surgeons. Osteoporos Int. 2015;26:1959–1963. doi: 10.1007/s00198-015-3103-4. [DOI] [PubMed] [Google Scholar]
- 7.Tsukutani Y., Hagino H., Ito Y., Nagashima H. Epidemiology of fragility fractures in Sakaiminato, Japan: incidence, secular trends, and prognosis. Osteoporos Int. 2015;26:2249–2255. doi: 10.1007/s00198-015-3124-z. [DOI] [PubMed] [Google Scholar]
- 8.Marsh D., Akesson K., Beaton D.E., Bogoch E.R., Boonen S., Brandi M.L. Coordinator-based systems for secondary prevention in fragility fracture patients. Osteoporos Int. 2011;22:2051–2065. doi: 10.1007/s00198-011-1642-x. [DOI] [PubMed] [Google Scholar]
- 9.Frederiksen A., Abrahamsen B., Johansen P.B., Sørensen H.A. Danish, national cross-sectional observational study on the prevalence of prior major steoporotic fractures in adults presenting with hip fracture-limitations and scope for fracture liaison services in prevention of hip fracture. Osteoporos Int. 2018;29:109–114. doi: 10.1007/s00198-017-4247-1. [DOI] [PubMed] [Google Scholar]
- 10.Nakayama A., Major G., Holliday E., Attia J., Bogduk N. Evidence of effectiveness of a fracture liaison service to reduce the re-fracture rate. Osteoporos Int. 2016;27:873–879. doi: 10.1007/s00198-015-3443-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huntjens K.M., van Geel T.A., van den Bergh J.P., van Helden S., Willems P., Winkens B. Fracture liaison service: impact on subsequent nonvertebral fracture incidence and mortality. J Bone Joint Surg Am. 2014;96:e29. doi: 10.2106/JBJS.L.00223. [DOI] [PubMed] [Google Scholar]
- 12.van Geel T.A.C.M., Bliuc D., Geusens P.P.M., Center J.R., Dinant G.J., Tran T. Reduced mortality and subsequent fracture risk associated with oral bisphosphonate recommendation in a fracture liaison service setting: a prospective cohort study. PLoS One. 2018;13 doi: 10.1371/journal.pone.0198006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hawley S., Leal J., Delmestri A., Prieto-Alhambra D., Arden N.K., Cooper C. Anti-osteoporosis medication prescriptions and incidence of subsequent fracture among primary hip fracture patients in england and wales: an interrupted time-series analysis. J Bone Miner Res. 2016;31:2008–2015. doi: 10.1002/jbmr.2882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ganda K., Puech M., Chen J.S., Speerin R., Bleasel J., Center J.R. Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int. 2013;24:393–406. doi: 10.1007/s00198-012-2090-y. [DOI] [PubMed] [Google Scholar]
- 15.McLellan A.R., Wolowacz S.E., Zimovetz E.A., Beard S.M., Lock S., McCrink L. Fracture liaison services for the evaluation and management of patients with osteoporotic fracture: a cost-effectiveness evaluation based on data collected over 8 years of service provision. Osteoporos Int. 2011;22:2083–2098. doi: 10.1007/s00198-011-1534-0. [DOI] [PubMed] [Google Scholar]
- 16.Yong J.H., Masucci L., Hoch J.S., Sujic R., Beaton D. Cost-effectiveness of a fracture liaison service--a real-world evaluation after 6 years of service provision. Osteoporos Int. 2016;27:231–240. doi: 10.1007/s00198-015-3280-1. [DOI] [PubMed] [Google Scholar]
- 17.Moriwaki K., Noto S. Economic evaluation of osteoporosis liaison service for secondary fracture prevention in postmenopausal osteoporosis patients with previous hip fracture in Japan. Osteoporos Int. 2017;28:621–632. doi: 10.1007/s00198-016-3777-2. [DOI] [PubMed] [Google Scholar]
- 18.Inderjeeth C.A., Raymond W.D., Briggs A.M., Geelhoed E., Oldham D., Mountain D. Implementation of the Western Australian Osteoporosis Model of Care: a fracture liaison service utilising emergency department information systems to identify patients with fragility fracture to improve current practice and reduce re-fracture rates: a 12-month analysis. Osteoporos Int. 2018;29:1759–1770. doi: 10.1007/s00198-018-4526-5. [DOI] [PubMed] [Google Scholar]
- 19.Chang Y., Huang C., Hwang J., Kuo J., Lin K., Huang H. Fracture liaison services for osteoporosis in the Asia-Pacific region: current unmet needs and systematic literature review. Osteoporos Int. 2018;29:779–792. doi: 10.1007/s00198-017-4347-y. [DOI] [PubMed] [Google Scholar]
- 20.Kishimoto H., Maehara M. Compliance and persistence with daily, weekly, and monthly bisphosphonates for osteoporosis in Japan: analysis of data from the CISA. Arch Osteoporos. 2015;10:231. doi: 10.1007/s11657-015-0231-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suzuki A., Sekiguchi-Ueda S., Kakita A. Hip fracture--epidemiology, anagement and liaison service. Osteoporosis liaison service in Japan. Clin Calcium. 2015;25:559–563. [PubMed] [Google Scholar]
- 22.Kanis J.A., Oden A., Johnell O., Johansson H., De Laet C., Brown J. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int. 2007;18:1033–1046. doi: 10.1007/s00198-007-0343-y. [DOI] [PubMed] [Google Scholar]
- 23.National Osteoporosis Society . National Osteoporosis Society; Somerset (England): 2014. Effective secondary prevention of fragility fractures: clinical standards for fracture liaison services. [Google Scholar]
- 24.Yoshizawa S., Ishibashi H. Investigation of the intervention effects of osteoporosis liaison service on hip fracture and vertebral fracture cases. J Jpn Osteoporos Soc. 2018;4:503–512. [Japanese] [Google Scholar]
- 25.Morisaki T., Hoshino T., Shiotsu K., Murayama T., Saito S., Murao M. The effect of osteoporosis liaison service for the improvement of the osteoporosis examination and treatment rates in patients with hip fracture at a mixed-care hospital. J Jpn Osteoporos Soc. 2019;5:259–265. [Japanese] [Google Scholar]
- 26.Abe A., Ishizuka M. The current status and issues of osteoporosis liaison service-from the standpoint of registered dietitian. Prog Med. 2018;38:45–49. [Japanese] [Google Scholar]
- 27.Tanaka N., Kuratsu S. The current status and issues of osteoporosis liaison service-from the standpoint of physical therapist. Prog Med. 2018;38:51–55. [Japanese] [Google Scholar]
- 28.Ishigaki T., Terakado A. The OLS activity in orthopedic clinic: approach at Kitachiba Spine & Sports Clinic. Prog Med. 2018;38:65–67. [Japanese] [Google Scholar]


