Abstract
Contrast extravasation is a common phenomenon in acute ischaemic stroke patients who are treated with endovascular therapy, but it is rarely reported in selective angioplasty of intracranial artery stenosis. In this case we present the treatment and follow-up studies of a patient with severe stenosis in the M1 segment of the middle cerebral artery. We observed extravasation of contrast medium in the brain tissue around the stent after the operation by a computed tomography scan taken immediately, but the patient did not experience any neurological deficits during the operation and the 4-year follow-up. Also the contrast extravasation did not transform into haemorrhage or hyperperfusion.
Keywords: Contrast extravasation, middle cerebral artery, symptomatic stenosis, angioplasty, stenting
Introduction
Contrast extravasation is a common phenomenon in acute ischaemic stroke patients who are treated with endovascular therapy. It always presents as a hyperdensity on computed tomography (CT) imaging and thus is sometimes difficult to distinguish from intracerebral haemorrhage.1 Previous studies have found that the hyperdense abnormalities detected on post-procedural CT scans may be a result of transitory disruption of the integrity of the blood–brain barrier (BBB),2 which may be one of the reasons why contrast extravasation is common in patients with acute stroke. Studies have also demonstrated that contrast enhancement following neuroendovascular procedures may be associated with intracranial haemorrhage, consequently leading to poor prognoses in patients with acute ischaemic stroke. However, contrast extravasation has rarely been reported in patients with intracranial arterial stenosis treated with angioplasty with stenting. Here, we report on a case in which contrast extravasation was experienced after endovascular procedures in a patient with severe middle cerebral artery (MCA) stenosis treated with angioplasty with stenting.
Case report
A 57-year-old man presented with paroxysmal left limb numbness and unclear speech for 2 months and was admitted to our hospital. He underwent endovascular angioplasty and stenting for the treatment of symptomatic MCA stenosis with 80% stenosis (by the WASID method). He had also experienced two episodes of ischaemic stroke in the past 8 years, with the most recent event, which was associated with the right MCA, occurring 2 months ago. He received medical therapy with aspirin, clopidogrel and statins for the ischaemic events. However, he still experienced two transient ischaemic attacks in the 2 months after treatment. The patient had a history of smoking and drinking for approximately 40 years. Neurological examination was normal. Cranial magnetic resonance imaging (MRI) showed a high signal in periventricular and internal watershed cerebral tissues without infarction lesions. Angiograms revealed severe stenosis in the M1 segment of the MCA.
The patient was prepared for angiography to treat the severe stenosis of the right MCA. He was treated with dual antiplatelet therapy consisting of aspirin and clopidogrel, as well as atorvastatin for over 2 months prior to the stenting procedures. All angiography procedures were performed through a femoral artery approach with the patient under general anaesthesia. First, the stenosis in the right MCA distal of the M1 segment was confirmed. Then, a microcatheter was carefully directed through the stenotic region into the distal part of M2. We chose a 2*9 mm balloon (Gateway; Boston Scientific Corporation, Maple Grove, USA) slowly and carefully to dilate the stenosis. After review of angiographic contrast, spillover and reduction of the branch vessel were not observed, and a self-expanding stent of 2.5*9 mm (Wingspan; Stryker Neurovascular, Cork, Ireland) was positioned across the stenotic plaque and released. After release, the angiogram showed that the stent was correctly positioned and the residual stenosis was less than 20% (Figure 1(a) to (c)). In addition, no branch vessel reduction or other abnormalities were found. An immediate routine post-procedure brain Dyna CT scan showed a diffuse hyperdensity (50∼78 HU) in the right basal ganglia without any mass effect (Figure 2(a1)). Protamine was used to neutralise heparin, and blood pressure was strictly controlled. After resuscitation, the patient awakened without any neurological deficits. The interventional therapy procedure was completed by using iohexol, a non-ionic contrast medium.
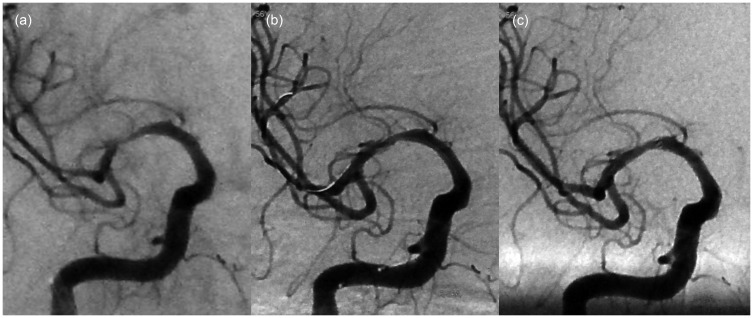
Figure 1.
(a) Angiogram of the distal M1 segment of the right middle cerebral artery (MCA) revealed severe stenosis. (b) Angiogram after balloon dilatation (Gateway 2*9 mm). (c) Angiogram after stent (2.5*9 mm Wingspan). In all cases, there was no extravasation of contrast media around the area of the right MCA. The right lenticulostriate artery could be observed at the proximal MCA during the procedure.
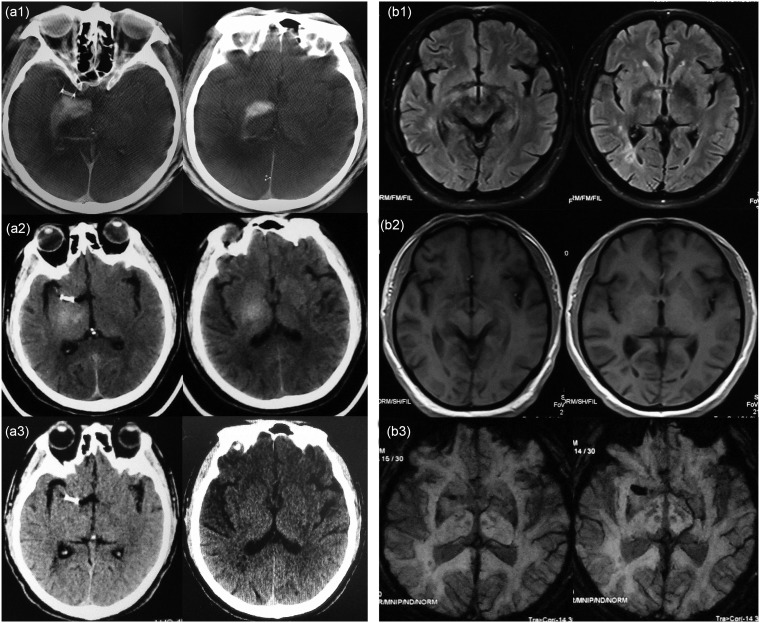
Figure 2.
(a1) A post-procedure plain Dyna computed tomography (CT) scan showed a hyperdensity (50∼78 HU) in the right basal ganglia, ipsilateral to the angioplasty and stenting of the middle cerebral artery. (a2) Twenty-four-hour CT follow-up showed that the hyperdensity became lighter compared to that in (a1). (a3) Three-day CT follow-up showed a compete resolution of all findings in (a1). (b). Two-day magnetic resonance imaging follow-up: (b1) T2 fluid-attenuated inversion recovery showed a slightly increased signal in the right basal ganglia. (b2) T1-weighted imaging showed equisignal and a slightly hyper-signal. (b3) Susceptibility-weighted imaging showed no low-signal in the right basal ganglia region.
The 24-hour postoperative CT follow-up revealed that the hyperdensity had become lighter compared to the postoperative density (Figure 2(a2)). The 3-day CT follow-up showed compete resolution of the hyperdensity (Figure 2(a3)). Head MRI, including susceptibility-weighted imagin (SWI) and computed tomography perfusion (CTP), was also performed and examined after the operation. The MRI scan was performed 2 days after the operation (Figure 2(b)). T1-weighted imaging showed equisignal and a slight hyper-signal of the right basal ganglia, respectively. T2 fluid-attenuated inversion recovery (FLAIR) showed a slightly high signal without mass effect. The only other abnormal signal was in the right medial temporal lobe, which was the infarct lesion that had occurred preoperatively. SWI showed no low-signal regions in these areas. The CTP scan was performed 3 days postoperatively, mean transmit time, cerebral blood volume and cerebral blood flow showed perfusion of the bilateral basal ganglia was normal.
After discharge, the patient was given dual antiplatelet therapy with clopidogrel and aspirin. Clopidogrel was discontinued 3 months later, while aspirin and atorvastatin were continued long term. During a one-month postoperative follow-up, head CT revealed no abnormalities. Transcranial Color-code Doppler at 6 and 12 months after the operation showed mild stenosis in the right MCA. MRI showed no new infarct lesions 12 months after stenting. To date, the patient has been followed up for 4 years with no recurrent ischaemic cerebral events.
Discussion
According to the literature, contrast exosmosis is rare in selective angioplasty of intracranial artery stenosis. In this case, due to the tortuosity of the stenosis in the right MCA and the extent of angulations of the vasculature, changes in the permeability of the local vascular wall increased the difficulty of completing the procedures, which may have resulted in aggravation of the damage to the vascular wall and endothelium. No cerebral haemorrhage or abnormal cerebral perfusion was found after close examination by CT, MRI (including SWI) and CTP scans. We speculate that this phenomenon was due to a change in the permeability of the vascular endothelium, not hyperperfusion or luxury perfusion, both of which are also insufficient to cause haemorrhage. MRI scans revealed no local cerebral oedema, which may indicate that hyperperfusion did not occur.
Previous studies have found that contrast extravasation after endovascular procedures may be associated with reversible BBB damage of varying degrees.3 There are differences in the location of the brain in which extravasation has occurred. CT hyperdensities within gyri and the subarachnoid space were observed after CAS associated with hyperperfusion or haemorrhage4,5 and within the basal ganglia and lentiform nucleus after intra-arterial thrombolysis associated with parenchymal haemorrhage.6 In our case, the contrast extravasation may have been associated with a temporary disruption of the vascular endothelium that occurred during the process of using balloons and stents during the surgery, leading to short-term destruction of the BBB.7 This destruction not only led to the endothelium of the MCA itself, but also acts on the branches of the M1 branch, particularly on the initial segment of the right lenticulostriate artery (LSA), which due to the damage leads to limited extravasation of contrast media that was located in the LSA perfusion area, exactly on the right basal ganglia. BBB damage is usually pronounced following restoration of blood flow after ischaemia.8 In contrast to intracerebral haemorrhage, contrast extravasation is generally absorbed within 24–72 hours, depending on the volume of the extravasation. In this case, the contrast extravasation was not fully absorbed until 3 days later. This phenomenon may be related to the volume of contrast medium (80–100ml) used during the procedures. The alteration of the BBB by the contrast medium can be explained osmotically. It is hypothesised that hypertonic solutions draw water out of the endothelial cells of brain vessels, causing the cells to shrink, which separates the tight junctions.9
In general, for distinguishing the contrast extravasation, in addition to observing the manifestations and imaging characteristics of the patients, inspection methods are also crucial. Dual-energy head CT has been found to be useful to distinguish between contrast extravasation and intracranial haemorrhage and subarachnoid haemorrhage.10 However, due to the high requirements for hardware equipment and software parameters, this method is still limited in clinical practice. In this case, continuous monitoring of clinical manifestations and cranial CT and MRI could also distinguish contrast extravasation from intracerebral haemorrhage. Therefore, for institutions without dual-energy head CT, we suggest that continuous monitoring of clinical manifestations and cranial imaging may be an effective strategy for distinguishing intracerebral haemorrhage from contrast extravasation.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.An H, Zhao W, Wang J, et al. Contrast staining may be associated with intracerebral hemorrhage but not functional outcome in acute ischemic stroke patients treated with endovascular thrombectomy. Aging Dis. Epub ahead of print April 2019. DOI: 10.14336/AD.2018.0807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ito U, Ohno K, Nakamura R, et al. Brain edema during ischemia and after restoration of blood flow: measurement of water, sodium, potassium content and plasma protein permeability. Stroke 1979; 10: 542–547. [DOI] [PubMed] [Google Scholar]
- 3.Vangosa AB, Totyora D, Modestina F, et al. Reversible and asymptomatic gyral and subarachnoid contrast enhancement after carotid stenting. Neuroradiol J 2015; 28: 184–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilkinson ID, Griffiths PD, Hoggard N, et al. Unilateral leptomeningeal enhancement after carotid stent insertion detected by magnetic resonance imaging. Stroke 2000; 31: 848–851. [DOI] [PubMed] [Google Scholar]
- 5.Kawabata Y, Fumihiko H, Miyake H, et al. Follow-up outcomes of self-expanding stents for carotid artery angioplasty at a single hospital. Neuroradiol J 2010; 23: 622–628. [DOI] [PubMed] [Google Scholar]
- 6.Yoon W, Seo JJ, Kim JK, et al. Contrast enhancement and contrast extravasation on computed tomography after intra-arterial thrombolysis in patients with acute ischemic stroke. Stroke 2004; 35: 876–881. [DOI] [PubMed] [Google Scholar]
- 7.Nakano S, Iseda T, Kawano H, et al. Parenchymal hyperdensity on computed tomography after intra-arterial reperfusion therapy for acute middle cerebral artery occlusion: incidence and clinical significance. Stroke 2001; 32: 2042–2048. [DOI] [PubMed] [Google Scholar]
- 8.Ito U, Ohno K, Nakamura R, et al. Brain edema during ischemia and after restoration of blood flow: measurement of water, sodium, potassium content and plasma protein permeability. Stroke 1979; 10: 542–547. [DOI] [PubMed] [Google Scholar]
- 9.Rapoport SI, Thompson HK, Bidinger JM. Equi-osmoral opening of the blood-brain barrier in the rabbit by different contrast media. Acta Radiol (Stockh) 1974; 15: 21–32. [DOI] [PubMed] [Google Scholar]
- 10.Phan CM, Yoo AJ, Hirsch JA, et al. Differentiation of hemorrhage from iodinated contrast in different intracranial compartments using dual-energy head CT. Am J Neuroradiol 2012; 33: 1088–1094. [DOI] [PMC free article] [PubMed] [Google Scholar]