Abstract
Type 2 diabetes mellitus contributes to poor health outcomes including mortality, yet there is a gap in the literature when seeking to understand the influence of psychosocial factors on coping in this population. The paper presents a systematic review of quantitative studies that examined relationships among psychosocial determinants and coping in adults with type 2 diabetes. This review is the second layer of knowledge discovery for the concept, “Taking on a life-altering change is a rhythmical journey of experiencing ups and downs on the way to acceptance.” The life-altering change was determined to be a diagnosis of type 2 diabetes, the journey is the ups and downs of coping with the diagnosis as people work toward acceptance of type 2 diabetes. The review includes a synthesis of findings from 22 quantitative studies of psychosocial factors and coping in adults with type 2 diabetes. Anxiety, depression, stress, and diabetes distress were identified as key influential psychosocial factors. Increased social support was inversely related to emotional distress and coping styles were related to social well-being, psychological health, and physical health outcomes. The positive coping style of problem-focused coping was linked to improved psychological and physical health. Emotional responses to diagnosis were related to depression and anxiety. Negative coping styles of resignation, protest, or isolation were higher in women and linked to poorer quality of life, while avoidance was linked to increased diabetes-related distress and depressive symptoms.
Keywords: Coping, Social psychology, Social support, Type 2 diabetes mellitus
What is known?
-
•
The last systematic review to include the relationships among psychosocial factors and coping in adult men and women with type 2 diabetes mellitus was in 2008.
-
•
The problem-focused coping did not reveal a significant relationship to type 2 diabetes mellitus.
-
•
Also, coping methods aimed at addressing negative feelings and stressors commonly associated with diabetes management would have the potential to improve psychological health in persons with type 2 diabetes mellitus.
What is new?
-
•
This systematic review adds to the current literature includes three main findings.
-
•
First, gender differences in support and coping further complicate the care of persons with type 2 diabetes mellitus.
-
•
Second, knowing that poorer psychological states and low social support negatively influence outcomes in persons with type 2 diabetes mellitus dictates a critical need for interventions that reflect comprehensive, precise, and collaborative care.
-
•
Finally, identifying effective interventions for diminishing negative psychosocial factors while facilitating coping is essential to improved health outcomes for persons with type 2 diabetes mellitus.
1. Introduction
Diabetes mellitus is a major cause of disease morbidity and mortality in the United States and globally [1]. There are 29.1 million people in the United States with diabetes which is 9.3% of the population [2]. Diabetes is a complex, debilitating illness that, if poorly controlled, results in significant and numerous negative health outcomes. In order to prevent the known negative health consequences of diabetes, persons with diabetes must improve their self-management ability and make lifestyle adjustments [3].
Healthcare providers recognize that there are modifiable and non-modifiable determinants of health which include factors of the social, economic, and physical environment, as well as individual characteristics and behaviors. People with type 2 diabetes mellitus often suffer concurrently with known psychological and/or social determinants of health. These determinants have recently been reported as being in the top-10 determinants of comorbidity in persons with diabetes, indicating that addressing determinants is key to improved outcomes [4]. Overall, it is consistently reported in studies of persons with diabetes that greater social support from family, friends, and community are linked to better outcomes in persons with diabetes [5].
Psychological problems such as depression, anxiety, and disease-related distress are known to be problematic for persons with diabetes. People with a diagnosis of diabetes are twice as likely to develop depression [6,7] which is concerning because it has been reported that, persons with diabetes and depressive symptoms cope more poorly when compared to those without depressive symptoms [7]. There is a higher prevalence of anxiety in persons with type 2 diabetes, compared to those without type 2 diabetes [8]. Different from anxiety but equally important is diabetes-related distress [9] which is the psychological distress related to being diagnosed with type 2 diabetes. Diabetes-related distress stems from concerns or worries associated with living with the condition of diabetes. Persons with distress report negative emotional responses to the diagnosis such as self-blame [10].
There is a critical need to understand coping in persons with diabetes because it has been reported as being instrumental in the adaptation to self-care. The aim of coping is to manage or avoid the anxiety caused by a situation [11]. When caring for persons with diabetes who have comorbid depressive symptoms, anxiety, or distress, it is important to understand coping because coping responses may differ yet they have been determined to play a fundamental influential role in physical and psychological well-being [3]. Lazarus and Folkman's Transactional Model of Stress and Coping (TMSC) is well-recognized as the theoretical underpinning for coping. In the TMSC, the cognitive appraisal of stressors is recognized to be a determinant of subsequent health status. Based on the Lazarus and Folkman's model, coping is defined as “constantly changing cognitive and behavioral efforts to manage specific external and/or internal demands that are appraised as taxing or exceeding the resources of a person” [12].
This systematic review paper presents a synthesis of the findings from quantitative studies that explored relationships among psychosocial determinants of health and coping in adult men and women with type 2 diabetes. The research question that guided this systematic review was; What is the current knowledge, based on quantitative studies, on relationships among known psychosocial determinants of health and coping in adults with type 2 diabetes?
This systematic review builds on foundational conceptual work and serves as the next layer of knowledge discovery in a program of research focused on enhancing knowledge and improving the care of persons who are diagnosed with type 2 diabetes. In the summer of 2017, a new nursing concept, “taking on a life-altering change” [13], was explicated using a 10-phase systematic sequential process described by Liehr & Smith [14,15]. Nurses care for patients who are in the midst of experiencing a transition from life as normal to life being very different as they confront new health diagnoses or challenges. This new concept is rooted in nursing practice, was derived from a practice story of a life-altering change, and specifies a conceptual domain for knowledge development from the disciplinary perspective of Nursing [16]. Three core qualities were determined to be essential to defining the concept of “taking on a life-altering change” as a rhythmical transcendent journey of experiencing ups and downs on the way to acceptance.
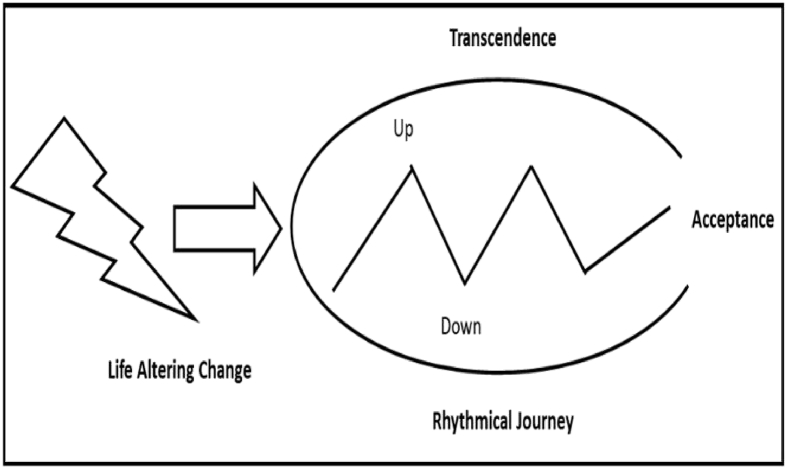
The 10-step process for concept development included exploration of the concept, “taking on a life-altering change” in the context of an existing theory and Pamela Reed's Theory of Self-Transcendence was chosen [17]. Reed's theory has three core concepts of vulnerability, self-transcendence, and well-being. When exploring “Taking on a life-altering change” in the context of Reed's theory, the vulnerability was viewed through the lens being diagnosed with type 2 diabetes. Self-transcendence was viewed as a capacity to expand self-boundaries which included intrapersonal (greater awareness of one's values), interpersonal (relating to others and one's environment), temporal (integrating time, past and future in a way that it has meaning for the present), and transpersonal (to connect with dimensions beyond the world). Reed's theory describes well-being as a sense of feeling whole and healthy. Well-being was viewed as feeling whole and healthy again by moving to acceptance of the life-altering change, type 2 diabetes (Fig. 1).
Fig. 1.
Model of life altering change.
2. Methods
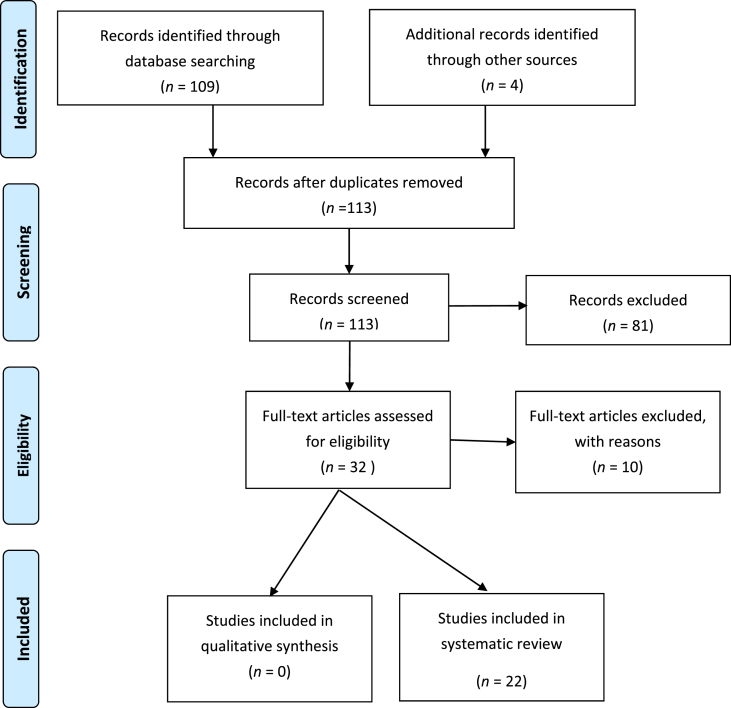
The literature search protocol was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [18,19].
2.1. Eligibility criteria
To be included in the literature synthesis, research reports had to meet the following inclusion criteria: quantitative study design, published in English language, study sample including adults with type 2 diabetes, and a reliable and valid measure of an identified psychosocial factor relative to coping. Quantitative studies were excluded if they only included the following; people in the sample with type 1 diabetes mellitus, insulin use in type 1 diabetes mellitus (insulin use in type 2 diabetes only if included if relevant to adults with type 2 diabetes), one gender, family/spousal coping, qualitative design, and mixed methods design.
2.2. Information sources
Databases searched included: Academic Search Complete, CINAHL with Full Text, ERIC, Health and Psychosocial Instruments (Hapi), Health Source: Nursing/Academic Edition, Medline, PsycARTICLES, PsycINFO, and Social Work Abstracts.
2.3. Electronic search strategy and study selection process
An advanced search was conducted using the following keywords and Boolean operators: Psychology (subject term) (Medline MeSH term 2017 for psychosocial factors) AND adaptation, psychological (subject term) (Medline MeSH term 2017 for coping) AND Diabetes Mellitus, Type 2 (subject term) AND Coping (field not specified because limited it to 10 articles) (CINHAL Heading for coping). The initial search yielded 141 articles. The search was then limited to the English language (132 articles) and by age group to all adult 19+ (109 articles). Four additional articles were discovered on Google search. Joanna Briggs Institute and Cochrane databases were also searched for recently published systematic reviews, but none were identified.
After screening articles by eligibility by reading titles, abstracts, and full papers as needed to establish, 22 published reports were established as meeting eligibility criteria and these articles. Fig. 2 illustrates the selection for inclusion process(Fig. 2).
Fig. 2.
Flow Diagram showing selection of studies for inclusion.
2.4. Data abstraction
The included 22 published manuscripts were critiqued by each of the coauthors to develop a synthesis of meaningful findings of psychosocial factors and coping in persons with type 2 diabetes. Studies critiques were detailed and included querying the manuscripts for commonalities or differences in use of conceptual or theoretical frameworks to guide the studies, methods used to operationalize psychosocial factors and coping, overall study design and methods used to describe relationships among psychosocial factors and coping, inclusion of interventions aimed to enhance coping in persons with type 2 diabetes, commonalities and differences in findings for the relationships among psychosocial factors and coping in persons with type 2 diabetes.
3. Results
3.1. Geographical distribution of studies
A total of twenty-two published articles are included; twenty primary reports of quantitative research studies published between 1996 and 2018, one meta-analysis [20] and one systematic review [21]. The included articles reflect a global perspective on coping with type 2 diabetes as they include two reports each from Canada [9,22], Iran [23,24], Sweden [11,25] and the United States [7,20,21,26,27]. One report each was generated from KwaZulu-Natal South Africa [28], Jordan [29], Taiwan [30], Poland [31], Norway [10], Mexico [32], China [33], Portugal [3], Japan [34], Netherlands [35], and Croatia [36]. The majority of the included studies used descriptive research designs. Table 1 presents a summary of each included article including authors, year of publication, and location of study, the purpose of study, study design, sample size, data collection, instrument, and results.
Table 1.
Literature review table.
| Study | Design and sample | Study details | Outcome assessment | Findings |
|---|---|---|---|---|
| Pipernik-Okanovic et al.(1996) [36] | A longitudinal study with 71 newly diagnosed type 2 diabetes | Fifteen days after diagnosis patients evaluated their feelings and perceptions toward type 2 diabetes. Group 1 (n = 36) Absence of negative emotional reaction and reported ability to cope. Group 2 (n = 17) Negative emotional reactions, but also reported ability to cope. Group 3 (n = 18) Negative emotional reactions (inability to cope). |
Social and emotional factors subscales of the diabetes care profile. HbA1c at 1-year follow-up |
HbA1c measures differed with better HbA1c measures in group 1 and poorest measures in group 3. (P < 0.05) Perceived coping abilities were better in higher educated persons and with those with more familial support. The healthier the patient coped correlated with the HbA1c. |
| Sandén-Eriksson (2000) [25] | A longitudinal study with 88 participants (50 men and 39 women newly diagnosed with type 2 diabetes mellitus) | Patients were asked about their self-assessed worries about their health and the health of others of the same age as compared to them. | Sense of Coherence-13 | Strong positive correlation between low levels of HbA1c and high levels of active management and emotional acceptance of diabetes. |
| Macrodimitris, & Endler (2001) [22] | A cross-sectional study of 115 adults (65 women and 50 men diagnosed with type 3 diabetes mellitus within 6 months prior) | Mailed a consent form and questionnaire packet to examine the relationship of coping strategies and perceived control to psycho-logical and physio-logical adjustment in adults with type 2 diabetes. | Coping with Health Injuries and Problems Scale; Event Perception Measure Endler Multi-dimensional Anxiety Scale-State Subscale; Center for Epidemiological Studies Depression Scale (CES-D) |
Emotional preoccupation and palliative coping were positively correlated with depression and anxiety. Emotional preoccupation coping mediated the relationships between perceived control and depression and perceived control and anxiety. |
| Koopmanschap (2002) [35] | A cross-sectional study of 4189 in five of eight European countries | The study examined patient perspective of the impact of type 2 diabetes mellitus. | Euroqol 5 Dimensions Quality of Life(EQ-5D) |
Patients reported depression and anxiety generally more often in diabetics. Type 2 diabetics report reduction of family functional and social life. The results predicted a poorer health-related quality of life by multivariate analysis in order of importance: gender (female), complications, treatment type, age, obesity, and hyperglycemia. |
| Coelho et al.(2003) [3] | A cross-sectional study of 123 type 2 diabetic patients and 124 non-type 2 diabetic patients | The participants were given two instruments to examine the relationship between coping style and perceived quality of life in patients with non-insulin dependent diabetes mellitus. | Coping Responses Inventory-Adult Form; Nottingham Health Profile |
A greater proportion of diabetic patients used avoidance coping styles, which overall where related to worse quality of life. Diabetic patients regard diabetes and changes in lifestyle as a threat. |
| Gåfvels & Wändell (2006) [11] | A cross sectional study of 232 participants (121 men and 111 women) | The General Coping Questionnaire was administered to assess and compare coping strategies in men and women with type 2 diabetes and their relationship to their demographic, medical, socio-economic, and psychosocial situation. | General Coping Questionnaire | Gender differences for the coping strategies resignation, protest, and isolation were higher in women. |
| Nakahara et al.(2006) [34] | A longitudinal prospective design on 256 participants (193 men and 63 women) | Obtained baseline psycho-social factors then developed a causal model of HbA1c at 6 months after assessment. The reliability of the model was investigated with HbA1c at 12 months. Repeated measures and structural equation Modeling. Assessment of the causal relation-ships between psycho-social factors and glycemic control. |
Summary of Diabetes Self-Care Activities Scale; Problem Areas in Diabetes Scale; Multidimensional Diabetes Questionnaire; Life- and Health-Related Questionnaire; Profile of Mood States (POMS) |
Psychosocial factors including social support, diabetes-related distress, daily burden, and emotion-focused coping influenced HbA1c indirectly through self-efficacy. |
| Duangdao & Roesch (2008) [20] | A meta-analysis of 21 primary studies consisting of 3381 people with diabetes | Summarization of relationships between coping dimensions (avoidance, emotion-focused, and problem-focused and indices of adjustment (depression, anxiety, glycemic control) in individuals with diabetes. | Studies had to meet four criteria for inclusion for the meta-analysis: presence of coping variable, outcome variable of adjustment (psychosocial or physical), diagnosed with diabetes, and relevant statistical information presented in the article. | Problem-focused coping was associated with better overall adjustment. Coping methods aimed at moderating stressors and negative situations improve psychological health. |
| Zhang et al.(2009) [33] | A pilot study of a cross-sectional study of 304 participants (121 men and 183 women) participants diagnosed with type 2 diabetes according to World Health Organization criteria for at least 1 year | Assessment of possible interactive effects of coping styles and psychological stress on depression and anxiety symptoms in Chinese patients with type 2 diabetes. | Psychological stress measured with scales originally developed by Leung et al. and Lin and Zhang. Medical Cope Questionnaire; The Hospital Anxiety and Depression Scale |
Physiological stress might directly increase the risk of anxiety and depression symptoms and the effects of psychosocial stress on anxiety and depression symptoms are moderated by coping styles used by Chinese patients with type 2 diabetes. |
| Garay-Sevilla et al. (2011) [32] | A cross-sectional study of 210 (51 men and 159 women) from two institutes in Mexico | Exploration of diverse psychosocial factors on adherence to treatment in patients with type 2 diabetes. | Adherence to treatment questionnaire; Jalowiec Coping Scale; Social Support Questionnaire; Belief in Conventional Medicine; questionnaire on perception of the burden of treatment cost on family finances. |
Male diabetic patients had better adherence to medication, better social support, and higher rates for supportive coping styles. Female diabetic patients had lower social support than males. |
| Shah et al.(2012) [7] | A cross-sectional study of 201 participants (76 men and 125 women) participants | Examined relationships among diabetes-related distress, appraisal, coping and depressive symptoms in patients with type 2 diabetes using Transactional Model of Stress and Coping by Lazarus and Folkman. | Diabetes-relates stress; Cognitive appraisal; The Diabetes Coping Measure; Zung Self-rating Depression Scale |
Path analysis suggests that patients who have greater diabetes-related stress or greater depressive symptoms have a negative appraisal of their diabetes. This is associated with greater use of avoidance as coping. |
| Karlsen et al. (2012) [10] | A cross sectional study of 425 Norwegian adults from five Norwegian countries strategically selected to represent Norwegian regions (urban/rural) | Examined the degree in which clinical indicators, coping styles, and perceived support from healthcare professional and family are related to diabetes-related distress. | Demographic data questionnaire; Problem Areas in Diabetes (PAID); COPE Inventory; One subscale of WAYS of Coping Questionnaire |
64% of participants reported self-blame when facing distress. Diabetes distress influenced by psychosocial variables such as coping style and perceived support. Interventions based on psychosocial approaches may primarily influence distress |
| Smalls et al.(2011) [26] | A cross-sectional study at two adult primary care clinics in southeastern United States who had an appointment between June and August 2010 (117 men and 261 women) | Examined the emotional approach to coping on diabetes outcomes. | Demographic data Coping measure eight-item emotion approach scale allowing evaluation of emotional processing and emotional expression. Diabetes Knowledge Questionnaire; Morisky adherence score (self-report tool to assess medication adherence); 11-item summary of Diabetes Self-Care Activities (SDSCA) |
Significant correlations between emotional coping and self-care behaviors. Coping through an emotional approach is significantly associated with behaviors that lead to positive diabetes outcomes. |
| Thorpe et al.(2013) [21] | Systematic review of 129 articles published August 2006–April 2011 | Summarization of recent literature on approaches to supporting healthy coping diabetes in two specific areas: impact of different approaches to diabetes treatment on healthy coping and effectiveness of interventions specifically designed to support healthy coping. | Articles included reported the effects of either a diabetes treatment or healthy coping intervention on at least one psychosocial or quality of life outcome. Type 1 or Type Diabetes Mellitus. Research component |
Findings include a growing appreciation from medical and research communities of the complex relationships between diabetes treatment, psychosocial factors, and metabolic control. Healthy coping interventions including diabetes self-management, education, support groups, problem-solving approaches, and coping skills interventions for improving outcomes. Cognitive behavioral therapy and collaborative care for treating depression. |
| Kalka (2014) [31] | Prospective, cross-sectional, descriptive study of 87 participants (42 persons with type 2 diabetes and 45 healthy persons) | Comparison of quality of life, symptoms of depression, and strategies of coping with stress among middle aged type 2 diabetes. | World Health Organization Quality of Life Instrument; Beck Depression Inventory; Coping Inventory for Stressful Situations; The Proactive Coping Inventory |
Individuals with type 2 diabetes had lower global perceived quality of life satisfaction with health and physical domain and intensity of depressive symptoms were higher. Persons with diabetes use an emotion-oriented style of coping. Healthy participants use avoidance-oriented style of coping. |
| Shayeghian et al. (2015) [23] | Prospective, cross-sectional study of 100 participants (40 men and 60 women) | Exploration of the role of coping styles and social support in the relationship between self-care activities and glycated hemoglobin in patients with type 2 diabetes. | Diabetes Self-Care Activities; Multidimensional Scale of Perceived Social Support Scale; Brief COPE |
Significant relationships of glycated hemoglobin with self-care activities, coping styles, and social support. Lower HgA1C correlates with higher incidence of self-care activities, positive coping styles, and greater social support. |
| Shamsalinia et al.(2015) [24] | Cross-sectional, correlational study of 150 participants | An investigation of the level of hope (as the psychosocial factor) and its relationship with religious coping among type 2 diabetes patients. | Herth Hope Index; Short form of religious coping |
Development of hope was found with positive religious coping, marital status, and social support. A negative relationship was found between hope and age (older adults) and hope and negative religious coping. |
| Burns et al. (2016) [9] | Prospective, longitudinal study (data collected over 2 years) n = 1742 (888 men and 854 women) This study was compared to data from CS studies. |
Expansion upon the existing literature by examining prospective associations between coping strategies and mental health outcomes. | Coping strategies were measured at baseline; Mental health conditions assessed at each point with self-report symptom measures; The Coping Inventory for Stressful Situations; PHQ-9 questionnaire; Generalized Anxiety Disorder-7; Diabetes Distress Scale |
Cross-sectional results differed from prospective results. Only emotion-oriented coping appears to play a role in the development of depressive symptoms (anxiety, depression, and diabetes related distress). Interventions targeting specific coping strategies might alleviate mental health problems in patients with type 2 diabetes. |
| Al-Amer et al.(2016) [29] | Cross-sectional, descriptive study of 220 participants (115 women and 105 men) who attended the Endocrinology Clinic, Jordan University Hospital | Examined relationships between self-care activities and illness perception, depression, social support, religiosity and spiritual coping, and self-efficacy among patients with type 2 diabetes | Brief Illness Perception Questionnaire; Patients' Health Questionnaire 9; ENRICH Social Support Instrument; Religious and Spiritual Coping Subscales; Diabetes Management Self-Efficacy Scale; Summary of Diabetes Self-Care Activities |
Depression symptoms were ubiquitous among the study sample. Structural Equation Model showed a direct relationship between self-efficacy and self-care activities. Programs that enhance self-care leads to better outcomes when considering psychosocial factors (illness perception, depressive symptoms, self-efficacy, social support, and religiosity and spiritual coping). |
| Huang et al. (2016) [30] | Cross-sectional, descriptive, correlational study of 241 (126 men and 115 women) adults with type 2 diabetes from an outpatient department in an urban hospital in southern Taiwan | Examined the direct and indirect relationships among demographic variables, disease characteristics, coping style, health related quality of life, and depressive symptoms | Demographic information; Modified WAYS of Coping Checklist; The Center for Epidemiological Studies Depression Scale; Short Form 36 Health Survey |
Patients which rely more on active and minimizing coping styles might reduce their depressive symptoms. Coping styles mediate relationships between the stressors of disease characteristic and demographic variables and health-related quality of life. |
| Ramkisson et al. (2017) [28] | Cross-sectional study of 401 (243 females and 158 men) participants on public and private facilities on the north coast of KwaZulu-Natal, South Africa | Explored whether patients with poor perceived social support have lower levels of well-being and coping than patients with good social support. | The Diabetes Care Profile; The General Health Questionnaire; Social Support Questionnaire; WHO-5 Well-being index |
There is an inverse relationship between social support and coping. An increase in social support is associated with a decrease in emotional distress |
| Whitebird et al. (2018) [27] | One-arm pilot intervention study. n = 31 analyzed (21 females and 10 males) 38 consented (5 withdrew prior to intervention, 1 withdrew during intervention, and 1 lost to follow-up) |
Examined whether a community-based mindfulness-based stress reduction (MBSR) program can improve diabetes management by improving HgA1C and decrease diabetes-related distress and improve anxiety and depression in people with type 2 diabetes. | Short-Form-12 Health Survey (SF-12); Patient Health Questionnaire (PHQ9); State-Trait Anxiety Inventory (STAI); Perceived Stress Scale (PSS); Coping Strategies Inventory (CSI-SF); Medical Outcomes Study (MOS) Social Support Survey; Self-Compassion Scale (SCS-SF); the Problems Areas in Diabetes (PAID); Diabetes Empowerment Scale (DES) |
Completion of MBSR program showed significant improvement in diabetes-related distress, psychosocial self-efficacy, and glucose control. |
3.2. Theoretical and conceptual frameworks employed in study designs
Nine studies described the use of guiding theoretical or conceptual frameworks. Sandén-Eriksson applied Sense of Coherence by Antonovsky [25] and Al-Amer et al. employed Social Cognitive Theory [29]. The remaining seven studies [7,9,10,20,22,26,30] foundational work by Lazarus and Folkman to include Cognitive Theory of Stress and Coping, the definition of coping, and scales derived from the Transactional Model of Stress and Coping Theory [12].
3.3. Operationalizing psychosocial factors and coping in persons with type 2 diabetes
There were commonalities in the included studies when critiqued to identify instruments used to operationalize both psychosocial factors and coping. A common instrument used to measure psychosocial factors was the Problems Areas in Diabetes (PAID) which is a 20-item measure of emotional distress that is specific to diabetes. Internal reliability for all 20 items is reported to be 0.30 or higher and Cronbach's α was 0.95 for the total scale. Concurrent and discriminant validity is well documented [37]. Common coping measures included in the studies were COPE Inventory [10], Ways of Coping Questionnaire (WAYS) [10], modified Ways of Coping Checklist [30], Brief COPE [23], Coping Inventory for Stressful Situations (CISS) [31], and Jalowiec Coping Scale [32]. All six of these instruments have well-documented reliability and validity and measure coping as conceptually described by Lazarus and Folkman in their early work of stress and coping with the TMSC [12].
3.4. Meta-analysis on coping dimensions in persons with type 2 diabetes
Data from twenty-two primary studies to examine the relations among coping dimensions of avoidance, approach, emotion-focused, and problem-focused to measures of adjustment which included scores of depression, anxiety, and overall glycemic control [20]. Differences were identified between those who used approach or problem-focused coping when compared to other coping dimensions. Approach and problem-focused coping were linked to improved overall adjustment. More importantly, this rigorous meta-analysis reported a sizable effect size between emotional-based coping and psychological outcomes. It was an unanticipated finding that emotion-based coping was inversely related to psychological outcomes of anxiety and depression. There was no correlation between avoidance coping and depression or anxiety. It was concluded that taking on the diagnosis of diabetes in a direct way can lead to improved health outcomes. Further, coping methods aimed at addressing negative feelings and stressors commonly associated with diabetes management would have the potential to improve psychological health in persons with type 2 diabetes [20].
3.5. Systematic review on coping in persons with type 2 diabetes
The most recent systematic review on coping in persons with type 2 diabetes was reported in 2013 and included 129 study reports [21]. In this review, it was concluded that healthy coping is related to several psychosocial outcomes: depression, anxiety disorder, perceived stress, diabetes-specific distress, positive attitudes and beliefs about the illness and treatment, positive relationships with others, and health-related quality of life. Findings included a growing appreciation from medical and research communities of the complex relationships between diabetes treatment, psychosocial factors, and metabolic control. The most significant findings from this literature review are the identification of potential interventions aimed at improving coping and subsequent health outcomes. It was concluded the diabetes education programs and support groups do benefit patients with an enhanced perception of support. Interventions that employed problem solving or cognitive restructuring techniques resulted in improve psychosocial adjustment. Healthy coping interventions including diabetes self-management programs, diabetes education, support groups, problem-solving approaches, and coping skills interventions; all resulted in some improvement in outcomes. For persons with type 2 diabetes and comorbid depression, cognitive behavioral therapy and collaborative care were effective for diminishing depressive symptoms [21].
3.6. Mindfulness-based stress reduction intervention study
A one-arm pilot study was conducted to investigate the mindfulness-based intervention on diabetes-related distress, psychosocial self-efficacy, glucose control, depression, anxiety, coping, self-compassion, and social support [27]. The program consisted of eight weeks (2.5 h each week) and included four types of mediation; sitting, standing, walking, and supine. Impact of the mindfulness intervention was assessed using surveys and blood samples at baseline and post-intervention. Completion of the mindfulness-based stress reduction (MBSR) program showed significant improvement in diabetes-related distress, psychosocial self-efficacy, and glucose control. In addition, participants reported improvement in depression, anxiety, stress, coping, self-compassion, and social support [27].
3.7. Empirical evidence from the literature
The co-authors categorized the synthesis of empirical evidence from the included manuscripts into 4 categories; psychosocial factors and social support, positive coping, negative coping, and gender differences. These categories were conceived after critique and in-depth discussion of commonalities and differences in study findings.
3.7.1. Psychosocial factors: social support and hope
Perceived coping abilities were better for persons with more familial support [36] and it was reported that an inverse relationship exists between social support and emotional distress, those with increased social support reported diminished emotional distress [28]. Increased social support was linked to improved glycemic control [23]. One study identified hope as an important psychosocial factor to study in persons with type 2 diabetes [24]., Nakahara et al. explored the causal relationships between psychosocial factors including social support and glycemic control through structural equation modeling. They described that social support had an indirect effect on glycemic control through its influence or relationship with self-efficacy [34].
3.7.2. Positive coping
For this review, positive coping-was viewed as a positive emotion or action-based response to diabetes and defined as an effective coping style that directly impacts better health benefits by lower glycosylated hemoglobin levels in patients with type 2 diabetes [23]. Examples of effective coping styles are active coping, planning, positive reframing, and acceptance. Positive coping contributes to better health outcomes [23]. Problem-focused coping was determined to moderate stressors and negative situations [20], coping through an emotional approach led to positive diabetes outcomes [26], and positive coping was inversely correlated with HbA1c [23]. The positive emotion of hope was reported as being related to positive religious coping, marital status, and social support [24]. In addition, a positive emotional state has the potential to increase self-efficacy and may lead to positive health outcomes [34]. Finally, the included systematic review concluded that healthy coping strategies of diabetes self-management, education, support groups, problem solving skills were all beneficial to health outcomes [21].
3.7.3. Negative coping
Negative coping is defined as an emotion-focused coping strategy that increases anxiety and depression symptoms. Emotional preoccupation, which focuses on an emotional response on the illness and palliative coping to lessen the unpleasantness of the illness was correlated with depression and anxiety [22]. Negative coping leads to diabetes being viewed as a threat which is a contributor to a worse quality of life [3]. Negative coping styles are reported to be significantly linked to increased anxiety and depression [33]. In addition, negative religious coping was associated with a negative relationship of hope in older adults with type 2 diabetes [24] and results from a path analysis demonstrate that avoidance coping leads to greater diabetes-related distress and depression symptoms [7].
3.7.4. Gender differences in coping with type 2 diabetes
Four studies addressed gender differences in coping with type 2 diabetes. Women with type 2 diabetes reported lower social support than men which is problematic since social support has been linked to worse outcomes. Gender differences for the coping strategies of resignation, protest, and isolation (based on the General Coping Questionnaire) were higher in women which is also problematic because they are determined to be negative coping styles. Further, poorer health-related quality of life has been reported in women with type 2 diabetes [35] and a second study reported that both diabetic and non-diabetic women had a poorer quality of life when compared to men [3]. One study reported that men reported higher rates for supportive coping styles [32](Table 1).
4. Discussion
Most included studies used Lazarus and Folkman's definition of coping and study instruments that were derived from the Transactional Model of Stress and Coping Theory [12]. The model can serve as an appropriate guiding framework for the study of coping because it details the interacting subjectivities of appraisal of illness as a stressor, emotional experience, and cognitive adaptation, viewing coping as being influenced by emotional regulation [12]. The model could be adopted for the study of coping in persons with type 2 diabetes by researchers who seek to maintain consistency in an approach to the problem of ineffective coping. The inclusion of the basic concepts of human adaptation in the model allows researchers to consider that, in the experience of illness, human beings will be appraising the stressor, responding with and moderating emotional and problem-focused coping mechanisms, and seeking effective coping by revising goals and coping strategies to self-manage and improve outcomes.
This synthesis highlights that both social support and hope are important for coping with type 2 diabetes. Knowing that social support is linked to decreased emotional distress and improved health outcomes in persons with type 2 diabetes are congruent with current literature. A very recent report on older adults indicates that the inclusion of planning to enhance social support is essential to diminishing depressive symptoms in older adults with type 2 diabetes [38]. Higher levels of social inclusion have been reported as predictive of lower levels of blood glucose and low-density lipoprotein [39], and it has been reported that low social support is linked to shorter leukocyte telomere length which is a predictor for higher rates of cellular aging [40]. In addition, since it is now known that the trajectory of social support is predictive of functional disability in adults with type 2 diabetes [41], the logical conclusion can be drawn that social support is integral to coping and should be included in future studies designed to build knowledge on coping in adults with type 2 diabetes. The findings of the review and their congruence with most recent literature make it critical to understand how facilitating social support could be integrated into coping interventions.
The knowledge about positive and negative coping and appraisal of diabetes as a challenge or threat is important in understanding the influence of positive coping and the detriment of negative coping. Understanding how a person copes is key to effective treatment planning. It has been reported that if persons with diabetes can receive intervention that facilitates the appraisal of type 2 diabetes as a challenge rather than a threat, then they may be able to, in a sense, rise to the challenge and meet the demands of the illness [1]. The mindfulness intervention reviewed in this paper [27] has the potential to engage persons with type 2 diabetes in mindfulness which could lead to a reappraisal of the illness or open-mindedness to embrace comprehensive care.
Interventions that build self-efficacy also have the potential for success. One strategy may be to work to build self-efficacy in persons with type 2 diabetes [29,34] since self-efficacy contributed to positive outcomes. It is possible that persons with higher self-efficacy will think differently about their experience of illness and be more prepared or motivated to engage in positive coping strategies and health behaviors. One recent study reported that self-efficacy is essential to autonomous motivation in eating behaviors in persons with type 1 diabetes so it could be inferred that interventions targeting enhanced self-efficacy in persons with type 2 diabetes could also result in enhanced motivation and improved adherence to dietary restrictions which are essential to glucose control [42].
The findings related to gender differences in this review are important. It may be that women with type 2 diabetes have ineffective coping and need more support and gender-specific interventions. Understanding how men and women respond differently to illness is key to designing effective interventions. This review identified a significant gap in the literature as there were no studies of gender differences in many countries, including the United States, yet it is known that sex is an important biological variable to consider [43].
The study findings are congruous with the foundational work on the concept, “Taking on a life-altering change is a rhythmical journey of experiencing ups and downs on the way to acceptance.” Embedded in the concept there is a cognitive aspect missing on how persons with diabetes view this life-altering change. This could reflect the psychosocial factors associated with the illness.
4.1. Implications for future research
There is a general lack in the literature when seeking to understand the differences in coping based on age. For example, there are no studies that differentiated coping differences for young adults, mid-life adults, older adults, and old-old adults. This is important because adults in these age groups are undergoing different challenges and human developmental processes as they live with the life-altering change of type 2 diabetes. It is necessary to understand these differences because younger adults diagnosed with a chronic illness will likely need adequate coping strategies that endure for many years.
Future studies are needed to address the gender difference in coping with type 2 diabetes. These studies could consider that gender response to illness have varied perspectives including physiological, psychological, emotional, behavioral, and social responses. Knowing that gender differences exist in coping, studies are needed that incorporate sex as a biological variable [43], recognizing that differences in coping exist between men and women, and gender precise interventions for copying may be needed in adults with type 2 diabetes.
Studies that seek to understand coping with type 2 diabetes in the context of culture are needed so that culturally competent interventions could be developed [44]. The experience of illness is inevitably linked to the experience of culture. Since culture often drives the food we eat, how we exercise, our health-seeking behavior, and our support needs and system; studies that build knowledge about coping with type 2 diabetes in varied cultures are needed. Knowing the illness in the context of the cultural healthcare system would also inform the future potential for scalability and sustainability of interventions.
It is imperative that future studies are designed to consistently include important factors that are relative to coping such as marital status, socioeconomic status, living situation, and educational level [45]. Consistency of inclusion of key factors known to be influential to coping will enhance the potential to build knowledge and develop effective interventions.
The findings of this literature synthesis indicate that there is a general gap in the advancement of the complexity of the design of studies which is problematic. In order to continue to build evidence on the topic of coping in persons with type 2 diabetes, studies are needed that reflect careful intervention design and testing, and subsequent comparative effectiveness trials are needed. The general lack of experimental randomized controlled trials that include interventions aimed at enhancing coping in persons with type 2 diabetes makes it difficult to translate findings to clinical practice. Comparative effective studies could help providers decide on which intervention is potentially most effective for enhancing coping in specified populations. Future studies that include a mindfulness component are warranted based on the findings presented in this review. Finally, there is a lack of complex designs such as SMART designs that could sequentially work with study populations to analyze which interventions work for specific groups, what dose of intervention is needed, and what combinations of interventions work for persons with varying characteristics.
4.2. Strengths and limitations
It is a strength of this synthesis that it was conducted with rigor and adherence to the PRISMA guidelines. The results of the synthesis are logically presented based on careful critiques of the included studies. It is also a strength that the included research studies are geographically dispersed because it gives the reader a general picture of the global challenges of coping with diabetes.
The results of this synthesis are limited to include only logical inferences from included studies and it is acknowledged that not all studies were designed to include the known factors that are influential to coping such as marital status, socioeconomic status, and living situation. It is also a limitation in this literature that the majority of the included quantitative studies of adults with type 2 diabetes were descriptive in design and used convenience samples which limit the generalizability of findings. Further, there were limitations in drawing inferences about interventions since intervention studies were limited in number. The broad geographic base of the studies does limit drawing conclusions about any specific culture or healthcare system.
5. Conclusion
Type 2 diabetes is a chronic disease that imposes adjustments in the patient's lifestyle and behaviors and is linked to poor health outcomes. Overall acceptance and management of type 2 diabetes are influenced by an individual appraisal of the illness and individual coping responses. Knowing that coping strategies differ by gender and that they are linked to psychosocial factors of hope, self-efficacy, anxiety, depressive symptoms, and diabetes-related distress informs the design of future studies of coping in persons with type 2 diabetes. The current gaps in the literature related to age, gender, culture, and available interventions make it imperative that interventions be developed, evaluated, and compared for translation to implementation studies and clinical care guidelines.
Author contributions
McCoy and Theeke conceived the study and were instrumental in the design of the study and participated in the critiquing of literature and manuscript writing. McCoy held primary responsibility for the development of the manuscript lead author. Theeke provided significant writing on each section of the manuscript and participated in the revision process as the manuscript was being reviewed. McCoy takes responsibility for the paper as a whole as it is foundational to a developing program of research with the selected population.
Conflicts of interest
None.
Acknowledgement
Jonas Nurse Scholar Cohort 2018–2020 has received scholarship money that was matched by WVU as financial support for graduate school as I work on my PhD.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2019.09.003.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Carpenter R., Theeke L., Mallow J., Theeke E., Gilleland D. Relationships among distress, appraisal, self-management behaviors, and psychosocial factors in a sample of rural appalachian adults with type 2 diabetes. Online J Rural Nurs Health Care. 2017;17(2):34–64. [Google Scholar]
- 2.Disease DoHPaC . 2019. Statistics about the population of West Virginia, West Virginia behavioral risk factor surveillance system [internet]. West Virginia department of health and human resources bureau for public health. [Statistics about the population of West Virginia]https://dhhr.wv.gov/hpcd/data_reports/Pages/Fast-Facts.aspx Available from: [Google Scholar]
- 3.Coelho R., Amorim I., Prata J. Coping styles and quality of life in patients with non-insulin-dependent diabetes mellitus. Psychosomatics. 2003;44(4):312–318. doi: 10.1176/appi.psy.44.4.312. [DOI] [PubMed] [Google Scholar]
- 4.Lee K.S., Park K.W. Social determinants of association among diabetes mellitus, visual impairment and hearing loss in a middle-aged or old population: artificial-neural-network analysis of the Korean longitudinal study of aging (2014-2016) Geriatrics (Basel) 2019;4(1):1–12. doi: 10.3390/geriatrics4010030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rad G.S., Bakht L.A., Feizi A., Mohebi S. Importance of social support in diabetes care. J Educ Health Promot. 2013;2:62. doi: 10.4103/2277-9531.120864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anderson R.J., Freeland K.E., Clouse R.E., Lustman P.J. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 7.Shah B.M., Gupchup G.V., Borrego M.E., Raisch D.W., Knapp K.K. Depressive symptoms in patients with type 2 diabetes mellitus: do stress and coping matter? Stress Health. 2012;28(2):111–122. doi: 10.1002/smi.1410. [DOI] [PubMed] [Google Scholar]
- 8.Smith K.J., Beland M., Clyde M., Gariepy G., Page V., Badawi G. Association of diabetes with anxiety: a systematic review and meta-analysis. J Psychosom Res. 2013;74(2):89–99. doi: 10.1016/j.jpsychores.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 9.Burns R.J., Deschenes S.S., Schmitz N. Associations between coping strategies and mental health in individuals with type 2 diabetes: prospective analyses. Health Psychol. 2016;35(1):78–86. doi: 10.1037/hea0000250. [DOI] [PubMed] [Google Scholar]
- 10.Karlsen B., Oftedal B., Bru E. The relationship between clinical indicators, coping styles, perceived support and diabetes-related distress among adults with type 2 diabetes. J Adv Nurs. 2012;68(2):391–401. doi: 10.1111/j.1365-2648.2011.05751.x. [DOI] [PubMed] [Google Scholar]
- 11.Gåfvels C., Wändell P.E. Coping strategies in men and women with type 2 diabetes in Swedish primary care. Diabetes Res Clin Pract. 2006;71(3):280–289. doi: 10.1016/j.diabres.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Lazarus R., Folkman S. Springer Publishing Company; New York, NY: 1984. Stress, appraisal, and coping. [Google Scholar]
- 13.McCoy M., editor. 2019; Cleveland, OH. nursing.case.edu/nursing-theory. Case Western Reserve University; 2019. Taking on a life altering change: a developing concept. Nursing theory: a 50-year perspective past and future. [Google Scholar]
- 14.Liehr P., Smith M.J. Story inquiry: a method for research. Arch Psychiatr Nurs. 2007;21(2):2. doi: 10.1016/j.apnu.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 15.LIehr P.R., Smith M.J. Springer Publishing company; New York, NY: 2014. Concept building for research. Middle range theory for nursing. [Google Scholar]
- 16.Newman M.A., Sime A.M., Corcoran-Perry S.A. The focus of the discipline of nursing. Adv Nurs Sci. 1991;14(1):1–6. doi: 10.1097/00012272-199109000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Reed P.G. Theory of self-transcendence. In: Smith M.J., Liehr P., editors. Middle range theory for nursing. 3 ed. Springer Publishing; New York, NY: 2014. [Google Scholar]
- 18.Swartz M.K. The PRISMA statement: a guideline for systematic reviews and meta-analysis. J Pediatr Health Care. 2011;25:1–2. doi: 10.1016/j.pedhc.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Tam W.W.S., Khalechelvam P. Endorsement of PRISMA statement and quality of systematic reviews and meta-analyses published in nursing journals: a cross-sectional study. BMJ Open. 2017 Feb 7;7(2):1–8. doi: 10.1136/bmjopen-2016-013905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duangdao K.M., Roesch S.C. Coping with diabetes in adulthood: a meta-analysis. J Behav Med. 2008;31(4):291–300. doi: 10.1007/s10865-008-9155-6. [DOI] [PubMed] [Google Scholar]
- 21.Thorpe C.T., Fahey L.E., Johnson H., Deshpande M., Thorpe J.M., Fisher E.B. Facilitating healthy coping in patients with diabetes: a systematic review. Diabetes Educat. 2013;39(1):33–52. doi: 10.1177/0145721712464400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Macrodimitris S.D., Endler N.S. Coping, control, and adjustment in type 2 diabetes. Health Psychol. 2001;20(3):208–216. [PubMed] [Google Scholar]
- 23.Shayeghian Z., Aguilar-Vafaie M.E., Besharat M.A., Amiri P., Parvin M., Gillani K.R. Self-care activities and glycated hemoglobin in Iranian patients with type 2 diabetes: can coping styles and social support have a buffering role? Psychol Health. 2015;30(2):153–164. doi: 10.1080/08870446.2014.951651. [DOI] [PubMed] [Google Scholar]
- 24.Shamsalinia A., Pourghaznein T., Parsa M. The relationship between hope and religious coping among patients with type 2 diabetes. Glob J Health Sci. 2015;8(1):208. doi: 10.5539/gjhs.v8n1p208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanden-Eriksson B. Coping with type-2 diabetes: the role of sense of coherence compared with active management. J Adv Nurs. 2000;31(6):1393–1397. doi: 10.1046/j.1365-2648.2000.01410.x. [DOI] [PubMed] [Google Scholar]
- 26.Smalls B.L., Walker R.J., Hernandez-Tejada M.A., Campbell J.A., Davis K.S., Egede L.E. Associations between coping, diabetes knowledge, medication adherence and self-care behaviors in adults with type 2 diabetes. Gen Hosp Psychiatry. 2012;34(4):385–389. doi: 10.1016/j.genhosppsych.2012.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whitebird R.R., Kreitzer M.J., Vazquez-Benitez G., Enstad C.J. Reducing diabetes distress and improving self-management with mindfulness. Soc Work Health Care. 2018;57(1):48–65. doi: 10.1080/00981389.2017.1388898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramkisson S., Pillay B.J., Sibanda W. Social support and coping in adults with type 2 diabetes. Afr J Prim Health Care Fam Med. 2017;9(1):e1–e8. doi: 10.4102/phcfm.v9i1.1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Al-Amer R., Ramjan L., Glew P., Randall S., Salamonson Y. Self-efficacy, depression, and self-care activities in adult Jordanians with type 2 diabetes: the role of illness perception. Issues Ment Health Nurs. 2016;37(10):744–755. doi: 10.1080/01612840.2016.1208692. [DOI] [PubMed] [Google Scholar]
- 30.Huang C.Y., Lai H.L., Lu Y.C., Chen W.K., Chi S.C., Lu C.Y. Risk factors and coping style affect health outcomes in adults with type 2 diabetes. Biol Res Nurs. 2016;18(1):82–89. doi: 10.1177/1099800415569845. [DOI] [PubMed] [Google Scholar]
- 31.Kalka D. The quality of life, symptoms of depression and coping with stress among individuals with type 2 diabetes - preliminary study. Psychiatr Pol. 2014;48(5):931–940. doi: 10.12740/pp/22868. [DOI] [PubMed] [Google Scholar]
- 32.Garay-Sevilla M.E., Porras J.S., Malacara J.M. Coping strategies and adherence to treatment in patients with type 2 diabetes mellitus. Rev Investig Clin. 2011;63(2):155–161. [PubMed] [Google Scholar]
- 33.Zhang C.X., Tse L.A., Ye X.Q., Lin F.Y., Chen Y.M., Chen W.Q. Moderating effects of coping styles on anxiety and depressive symptoms caused by psychological stress in Chinese patients with Type 2 diabetes. Diabet Med. 2009;26(12):1282–1288. doi: 10.1111/j.1464-5491.2009.02840.x. [DOI] [PubMed] [Google Scholar]
- 34.Nakahara R., Yoshiuchi K., Kumano H., Hara Y., Suematsu H., Kuboki T. Prospective study on influence of psychosocial factors on glycemic control in Japanese patients with type 2 diabetes. Psychosomatics. 2006;47(3):240–246. doi: 10.1176/appi.psy.47.3.240. [DOI] [PubMed] [Google Scholar]
- 35.Koopmanschap M., Board C.-A. Coping with Type II diabetes: the patient's perspective. Diabetologia. 2002;45(7):S18–S22. doi: 10.1007/s00125-002-0861-2. [DOI] [PubMed] [Google Scholar]
- 36.Pipernik-Okanovic M., Roglic G., Metelko Z. Emotional adjustment and metabolic control in newly diagnosed diabetic persons. Diabetes Res Clin Pract. 1996;34(2):99–105. doi: 10.1016/s0168-8227(96)01342-3. [DOI] [PubMed] [Google Scholar]
- 37.Welch G.W., Jacobson A.M., Polonsky W.H. The problem areas in diabetes scale. An evaluation of its clinical utility. Diabetes Care. 1997;20(5):760–766. doi: 10.2337/diacare.20.5.760. [DOI] [PubMed] [Google Scholar]
- 38.Kong L.N., Zhu W.F., He S., Yao Y., Yang L. Relationships among social support, coping strategy, and depressive symptoms in older adults with diabetes. J Gerontol Nurs. 2019;45(4):40–46. doi: 10.3928/00989134-20190305-03. [DOI] [PubMed] [Google Scholar]
- 39.Floyd K., Veksler A.E., McEwan B., Hesse C., Boren J.P., Dinsmore D.R. Social inclusion predicts lower blood glucose and low-density lipoproteins in healthy adults. Health Commun. 2017;32(8):1039–1042. doi: 10.1080/10410236.2016.1196423. [DOI] [PubMed] [Google Scholar]
- 40.Carroll J.E., Diez Roux A.V., Fitzpatrick A.L., Seeman T. Low social support is associated with shorter leukocyte telomere length in late life: multi-ethnic study of atherosclerosis. Psychosom Med. 2013;75(2):171–177. doi: 10.1097/PSY.0b013e31828233bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Levy M., Deschenes S.S., Burns R.J., Elgendy R., Schmitz N. Trajectories of social support in adults with type 2 diabetes: associations with depressive symptoms and functional disability. Int J Geriatr Psychiatry. 2019;34(3):480–487. doi: 10.1002/gps.5042. [DOI] [PubMed] [Google Scholar]
- 42.Eisenberg M.H., Lipsky L.M., Dempster K.W., Liu A., Nansel T.R. I should but I can't: controlled motivation and self-efficacy are related to disordered eating behaviors in adolescents with type 1 diabetes. J Adolesc Health. 2016;59(5):537–542. doi: 10.1016/j.jadohealth.2016.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clayton J.A. Applying the new SABV (sex as a biological variable) policy to research and clinical care. Physiol Behav. 2018;187:2–5. doi: 10.1016/j.physbeh.2017.08.012. [DOI] [PubMed] [Google Scholar]
- 44.Zeh P., Cannaby A.M., Sandhu H.K., Warwick J., Sturt J.A. A cross-sectional survey of general practice health workers' perceptions of their provision of culturally competent services to ethnic minority people with diabetes. Prim Care Diabetes. 2018;12(6):501–509. doi: 10.1016/j.pcd.2018.07.016. [DOI] [PubMed] [Google Scholar]
- 45.Hankonen N., Absetz P., Haukkala A., Uutela A. Socioeconomic status and psychosocial mechanisms of lifestyle change in a type 2 diabetes prevention trial. Ann Behav Med. 2009;38(2):160–165. doi: 10.1007/s12160-009-9144-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.