Abstract
The first step of the UNAIDS/WHO 90-90-90 targets to encourage early diagnosis with treatment for the control of HIV-1 epidemic is to achieve 90% HIV-1 diagnosis in infected individuals. In Japan, approximately 30% of newly reported cases have been annually identified by AIDS onset, implying that substantial numbers of HIV-1-infected individuals remain undiagnosed. However, the proportion of undiagnosed cases has not yet been determined. In the present study, the proportion of recent HIV-1 infections to newly-diagnosed cases was determined from 2006 to 2015 using a recent infection assay for three metropolitan areas in Japan: Tokyo, Osaka, and Fukuoka. Estimated median periods between infection and diagnosis were 1.0, 1.8, and 2.9 years for Tokyo, Osaka, and Fukuoka, respectively. Estimation of annual HIV-1 incidence by a back-calculation method using these data as well as HIV/AIDS national surveillance data indicated proportions of undiagnosed to new HIV-1 infections from 2006 to 2015 to be 18% in Tokyo, 22% in Osaka, 38% in Fukuoka, and 28% in Japan. This is the first report estimating HIV-1 incidence in Japan using a serological biomarker in combination with national HIV/AIDS surveillance data.
Keywords: HIV-1, AIDS, Incidence, Surveillance, Early diagnosis, Japan
1. Introduction
Early diagnosis with treatment is important in the control of the HIV-1 epidemic. Several studies have reported that undiagnosed individuals account for the majority of HIV-1 transmissions (Hall et al., 2012). One of the UNAIDS/WHO 90-90-90 targets (MacCarthy et al., 2015) is to achieve 90% HIV-1 diagnosis in infected individuals. Estimation of HIV-1 diagnosis frequency is crucial for developing strategies to reduce the number of new HIV-1 infections.
HIV/AIDS surveillance in Japan began in 1984, and the current system of national surveillance has been conducted under the Infectious Diseases Control Law since April 1999 (AIDS Surveillance Committee, 2016). Approximately 1300–1600 newly diagnosed HIV/AIDS cases have been reported annually for the past ten years. Notably, approximately 30% of newly reported cases were identified by AIDS onset, implying the existence of a substantial number of undiagnosed HIV-1-infected individuals in Japan. A definitive method for estimating HIV-1 incidence has not yet been established (Iwamoto et al., 2017).
Several approaches have been used to estimate national HIV-1 incidence (Wand et al., 2009, van Sighem et al., 2015, Pharris et al., 2016). Selecting the optimum method is challenging, especially in countries with low HIV-1 prevalence, as large, long-term studies are required for robust statistical analyses. UNAIDS/WHO has recently identified methodologies for estimating HIV-1 incidence, primarily using case-based surveillance (UNAIDS/WHO working group on Global HIV/AIDS and STI surveillance, 2011, UNAIDS/WHO working group on Global HIV/AIDS and SIT surveillance, 2017). Most of these methods adopt back-calculation approaches (Brookmeyer and Gail, 1994) and some incorporate biomarkers such as CD4+ T cell counts. HIV-1 recent infection assays were initially developed in the 1990s based on changes in HIV-1-specific antibody avidity during the course of infection (Janssen et al., 1998). Recently, HIV-1 recent infection assays with improved accuracy have been used to estimate national HIV-1 incidence (UNAIDS/WHO working group on Global HIV/AIDS and STI surveillance, 2011, UNAIDS/WHO working group on Global HIV/AIDS and SIT surveillance, 2017, Hall et al., 2008, Parekh et al., 2004, Duong et al., 2012).
In this study, a recent infection assay in addition to HIV/AIDS national surveillance data was used to estimate HIV-1 incidence from 2006 to 2015 in Japan. We investigated the proportion of recent infections to newly diagnosed cases in three metropolitan areas: Tokyo, Osaka, and Fukuoka prefectures, which cumulatively represent approximately half of the reported HIV-1 infections in Japan. We then estimated the number of new HIV-1 infections from 2006 to 2015 in Japan by a modified back-calculation method using serological and HIV/AIDS national surveillance data.
2. Methods
2.1. HIV/AIDS national surveillance
The Japanese HIV/AIDS national surveillance program (AIDS Surveillance Committee, 2016) annually collects and classifies the total number of HIV/AIDS diagnosed cases into two mutually exclusive categories: (1) “HIV cases” - infection diagnosed prior to AIDS onset and (2) “AIDS cases” - infection diagnosed following the onset of AIDS indicator diseases defined within the Infectious Diseases Control Law in Japan. An HIV-infected individual once registered as an “HIV case” is not registered as an “AIDS case” even if the individual subsequently develops AIDS. Data on CD4 counts for HIV cases at diagnosis are unavailable.
2.2. Laboratory testing
This study was approved by the ethical committee of the National Institute of Infectious Diseases, Japan (approval number: 719; on September 13, 2016). Specimens were anonymous and residual diagnostic material from subjects who provided written consent for HIV testing. Blood samples were obtained from individuals who visited local health centers for voluntary counseling and testing and found to be HIV-1 positive in Tokyo, Osaka, and Fukuoka from 2006 to 2015. Specimens were screened using the following immunoassays: GENEDIA HIV-1/2 MIXT PA (FUJIREBIO Inc.), ESPLINE HIV-Ag/Ab (FUJIREBIO Inc.), Dainascreen HIV-1/-2 (Alere Medical), ARCHITECT HIV Ag/Ab Combo Assay (Abbott Japan), Genscreen ULTRA HIV Ag-AB (Bio-Rad), and Enzygnost HIV Integral II (Siemens Healthcare). Reactive samples were confirmed by western blot (WB; NEW LAV Blot [Bio-Rad]). Samples that were reactive by screening test and negative by WB were further tested with a nucleic acid amplification test (NAT) for determination of HIV-1 infection. Seropositive samples (i.e., positive by WB) were assessed for HIV-1 recent infection assay using the BED HIV-1 Incidence EIA/HIV-1 LAg-Avidity EIA (Sedia BioSciences) according to the manufacturer's instructions (Hall et al., 2008, Parekh et al., 2004, Duong et al., 2012). Samples used for recent infection assay were obtained from HIV cases (i.e., ART-naive and prior to AIDS onset) only. Recent infection was defined as: (i) seronegative and NAT-positive or (ii) seropositive and HIV-1 recent infection assay-positive.
2.3. Estimation of HIV-1 incidence
A modified back-calculation Ottawa/Sydney model (Wand et al., 2009, UNAIDS/WHO working group on Global HIV/AIDS and SIT surveillance, 2017) was used for estimation of HIV-1 incidence by introducing parameters obtained from the HIV-1 recent infection assay and the HIV/AIDS national surveillance data. First, we built a sub-model for HIV diagnosis kinetics to estimate the distribution of the period between HIV-1 infection and diagnosis before AIDS onset as an exponential function. The proportion of undiagnosed (Survivor [Sh]) to HIV-1-infected individuals is given by: Sh(t) = exp−λt (λ: a constant number). Because the HIV-1 recent infection assay defines those infected with HIV-1 for less than half a year as recently-infected (Duong et al., 2012), coefficient λ was calculated using the following formula: Sh(0.5) = 1 − “proportion of recent infections (mean from 2006 to 2015)” = exp−0.5λ. The proportion of individuals diagnosed at x years after infection was given by fh(x) = Sh(x) − Sh(x + 1). Second, we built a sub-model for AIDS onset kinetics to estimate the period between HIV-1 infection and AIDS onset in the absence of laboratory diagnosis. Adopting the Weibull distribution with median time to AIDS onset of 6.5 years (Wand et al., 2009, Brookmeyer and Gail, 1994, Collaborative Group on AIDS Incubation and HIV Survival, including the CASCADE EU Concerted Action, 2000), the proportion of individuals without AIDS to HIV-1-infected undiagnosed individuals at x years after infection was given by Sa(x) = exp(−0.1014x2.08). The proportion of individuals developing AIDS at x years after infection was determined from fa(x) = Sa(x) − Sa(x + 1) (Wand et al., 2009). Third, we built a model for HIV/AIDS diagnosis kinetics by combining the above two sub-models. The probability of diagnosis at x years after HIV-1 infection was given by f(x) = m × fh(x) + (1 − m) × fa(x). The mixing constant, m, was defined as the mean proportion of HIV cases to the annual reported total HIV/AIDS cases in the national surveillance data with 1 − m being the mean ratio of AIDS cases to total HIV/AIDS cases. Introducing the data obtained from the HIV-1 recent infection assay and the HIV/AIDS national surveillance into the above formulae, HIV-1 incidence for individual years was calculated on the source code written in R language. Data were optimized by the quasi-Newton method as described before (Wand et al., 2009). Sensitivity analysis to address the uncertainty of HIV-1 incidence estimation was conducted by varying recent infection proportions and AIDS ratios within 95% confidence interval on the measured proportions/ratios (Wand et al., 2009, van Sighem et al., 2015).
3. Results
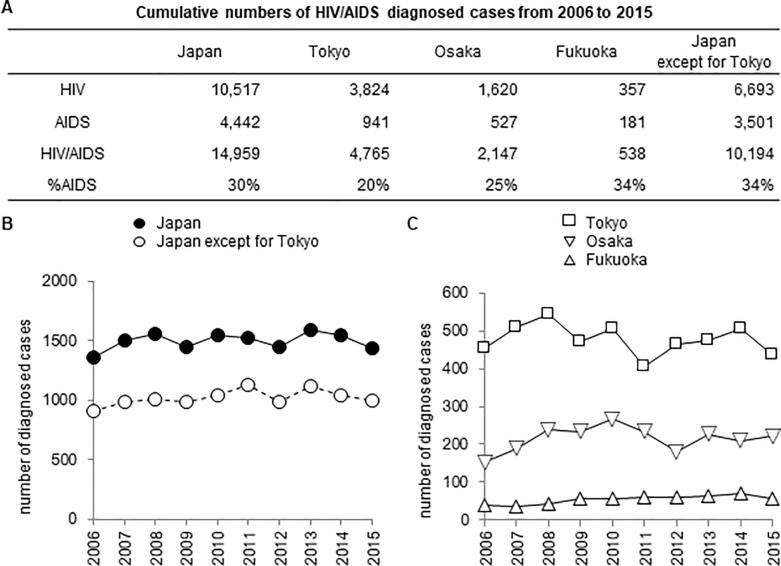
The number of annually reported HIV/AIDS cases in Japan was relatively constant, ranging from 1358 to 1590 since 2006 (Fig. 1). A total of 14,959 HIV-positive cases (10,517 HIV [9906 male; 611 female] and 4442 AIDS [4161 male; 281 female]) were reported from 2006 to 2015. Men who have sex with men and heterosexual males accounted for 63% (9481/14,959) and 18% (2649/14,959) of cases, respectively. The majority of HIV cases were in the 20–40 year age range (86%), while most AIDS cases were in the 30–50 year range (78%). Tokyo, Osaka, and Fukuoka prefectures had 4765, 2147, and 538 HIV/AIDS cases, respectively, cumulatively representing 50% (7450/14,959) of newly diagnosed HIV-1 infections in Japan.
Fig. 1.
Trends in HIV/AIDS cases diagnosed in Japan from 2006 to 2015. (A) Cumulative numbers of HIV/AIDS diagnosed cases from 2006 to 2015 in Japan, Tokyo, Osaka, Fukuoka, and Japan without Tokyo prefecture (Japan except for Tokyo). (B) and (C) Changes in annual HIV/AIDS diagnosed cases in Japan (closed circles), Japan except for Tokyo (open circles), Tokyo (open squares), Osaka (open reverse triangles), and Fukuoka (open triangles). Data were obtained from the HIV/AIDS national surveillance report (AIDS Surveillance Committee, 2016). HIV: cases diagnosed with HIV infection prior to AIDS onset; AIDS: cases diagnosed after AIDS onset; %AIDS: frequency of AIDS to the sum of HIV and AIDS.
Approximately 30% of newly reported HIV/AIDS cases were detected by AIDS onset. The percentage of AIDS cases to total annual HIV/AIDS cases during 2006–2015 was different among prefectures and lower in Tokyo (mean: 19.8% [95% CI: 18.5–21.1]) compared with those in Osaka (24.3% [21.8–26.9]) and in Fukuoka (33.5% [29.5–37.3]). The proportion of AIDS cases to total HIV/AIDS cases in Japan other than Tokyo (“Japan except for Tokyo”) was most similar to that in Fukuoka (Fig. 1A).
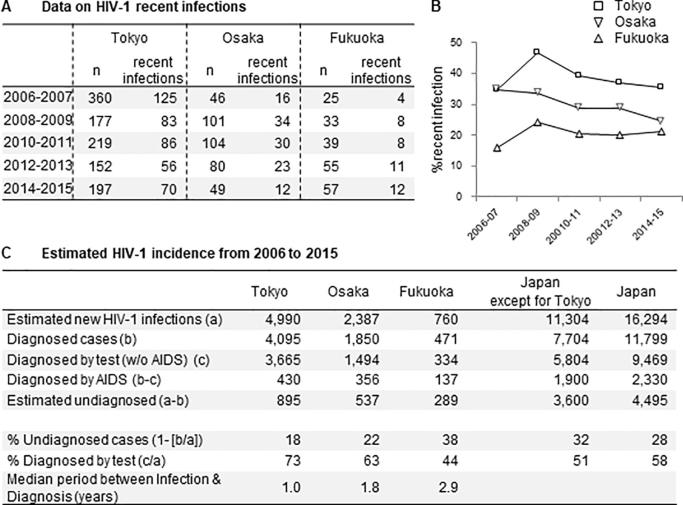
The proportions of recent infections in Tokyo, Osaka, and Fukuoka from 2006 to 2015 (Fig. 2A) were different among the prefectures and higher in Tokyo (mean: 38.6% [95% CI: 32.5–44.8]) compared with those in Osaka (30.1% [24.9–35.3]) and in Fukuoka (20.4% [16.7–24.0]). There was no clear temporal change in the proportion of recent infections in Tokyo and Fukuoka, but Osaka showed a decreasing trend over the ten-year study period (Fig. 2B).
Fig. 2.
Early diagnosis frequency and estimated HIV-1 incidence from 2006 to 2015. (A) Data on HIV-1 recent infection frequency in Tokyo, Osaka, and Fukuoka. (B) Temporal changes in the frequency of recent infections over time. (C) Estimated HIV-1 incidence from 2006 to 2015 and undiagnosed cases at the end of 2015 in Tokyo, Osaka, Fukuoka, Japan except for Tokyo, and Japan. HIV-1 incidence in Tokyo, Osaka, and Fukuoka was estimated using data from the HIV-1 recent infection assay and the HIV/AIDS national surveillance. HIV-1 incidence in Japan except for Tokyo was estimated by applying the early diagnosis frequency from Fukuoka. Estimated cases in Japan are the sum of the cases in Tokyo and in Japan except for Tokyo.
HIV-1 incidence analysis based on a back-calculation model utilizing the data from recent infection proportions and national surveillance estimated that 4990 (range obtained from sensitivity analysis: 4964–5001) individuals in Tokyo, 2387 (2364–2404) in Osaka, and 760 (652–782) in Fukuoka were newly infected with HIV-1 from 2006 to 2015, with 895 (785–1017) individuals (18%) in Tokyo, 537 (467–622) (22%) in Osaka, and 289 (188–337) (38%) in Fukuoka remaining undiagnosed at the end of 2015 (Fig. 2C). Thus, 4095 (82%), 1850 (78%), and 471 (62%) cases in Tokyo, Osaka, and Fukuoka, respectively, were diagnosed by the end of 2015, of whom 3665 (73%) [Tokyo], 1494 (63%) [Osaka], and 334 (44%) [Fukuoka] were diagnosed prior to AIDS onset. Estimates of median period from infection to diagnosis were 1.0 (IQR: 0.4–2.8), 1.8 (0.8–4.2), and 2.9 (1.1–6.2) years in Tokyo, Osaka, and Fukuoka, respectively.
Based on the proportion of AIDS cases to total HIV infections being comparable between Fukuoka and Japan without Tokyo prefecture (“Japan except for Tokyo”) (Fig. 1A), we estimated HIV-1 incidence in Japan except for Tokyo by applying the recent infection proportion from Fukuoka to determine λ in a sub-model for HIV diagnosis kinetics (Fig. 2C). Finally, we estimated national HIV-1 incidence from 2006 to 2015 by adding the estimates from “Tokyo” and “Japan except for Tokyo” (Fig. 2C). The incidence model estimated that 16,294 (15,949–16,414) individuals were newly infected between 2006 and 2015 in Japan; of these, 4495 (4093–5201) individuals (28%) remained undiagnosed, and 11,799 (72%) were diagnosed with HIV-1 infection by the end of 2015, with 9469 (58%) diagnosed by laboratory testing before AIDS onset.
4. Discussion
In the present study, the HIV-1 recent infection assay was used to evaluate early diagnosis proportions during 2006 to 2015 when annually reported HIV/AIDS cases were relatively constant. Tokyo and Osaka were initially selected for analysis due to their high number of reported cases. Additionally, we selected Fukuoka prefecture, based on the proportion of AIDS cases to total HIV/AIDS cases being similar to that in “Japan except for Tokyo”. No increase in the proportion of recent infections was observed during the study period, indicating no improvement in early diagnosis in these prefectures.
We estimated HIV-1 incidence from 2006 to 2015 in three metropolitan areas using a modified back-calculation Ottawa/Sydney model, which can make maximal use of data from recent infections, cases diagnosed in the asymptomatic phase, and those diagnosed by AIDS onset (Wand et al., 2009). HIV-1 incidence was determined separately for “Tokyo” and “Japan except for Tokyo”, to estimate HIV-1 incidence for the whole of Japan. The model estimates that 4495 cases of those infected with HIV-1 during 2006–2015 in Japan remained undiagnosed. The cumulative number of reported HIV/AIDS cases (including mortality) was approximately 26,000 at the end of 2015. Thus, the undiagnosed percent is estimated to be more than 15% (4495/[4495 + 26,000]), implying that the first target of the UNAIDS 90-90-90 strategy has not been achieved in Japan. Furthermore, our results indicate that only 58% of HIV-1 infections were diagnosed before AIDS onset, suggesting that public health strategies promoting early diagnosis need to be strengthened in Japan.
We used mean values of recent infection proportions and ratios of HIV cases (diagnosed with HIV-1 infection prior to AIDS) to total annual HIV/AIDS cases from 2006 to 2015 to determine λ and m for estimation of HIV-1 incidence, respectively, because there was no clear temporal change in the proportions and ratios, although Osaka showed a decreasing trend of recent infection proportions. If clear changes in the proportions or ratios in the next ten years occur, values in individual years will need to be applied to determine λ or m for more accurate HIV-1 incidence estimation.
Limitations of our study include not testing all HIV cases by the HIV-1 recent infection assay and using Fukuoka as a surrogate for “Japan except for Tokyo”. However, based on the comparability between the proportion of AIDS cases for Fukuoka and “Japan except for Tokyo” and the logistical difficulties in obtaining sufficient data on recent infection for all prefectures, this could be a reasonable strategy. Further studies in other regions of Japan could lead to a more accurate estimate of HIV-1 incidence in Japan.
5. Conclusion
This is the first report estimating HIV-1 incidence in Japan using a serological biomarker in combination with National HIV/AIDS surveillance data and applying a modified back-calculation method. The estimation indicates that only 58% of HIV-1 infections were diagnosed before AIDS onset. Our findings could inform the care cascade HIV-1 prevention strategies and contribute to promoting national programs aimed at early diagnosis and treatment.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
We thank Kazuhiko Kano and Teiichiro Shiino for their help in calculation/estimation of HIV-1 incidence. Gratitude is also expressed to Phillip Renzullo for helpful discussions on the manuscript.
Funding statement
This work was supported by the Ministry of Health, Labor, and Welfare (MHLW) of Japan (Health and Labor Sciences Research Grants [H29-AIDS-Ippan-005, H26-AIDS-Seisaku-Ippan-002, and H28-Shinko-Gyosei-Ippan-006]) and by Japan Agency for Medical Research and Development (AMED) under Grant Numbers JP18fk0410011, JP18fk0410003, JP18fk0108049, JP18jk0210002, and JP18kk0205011.
References
- AIDS Surveillance Committee, Ministry of Health, Labor and Welfare, Japan. 2016. Annual AIDS Occurrence Report 2016 (in Japanese). http://api-net.jfap.or.jp/status/.
- Brookmeyer R., Gail M.H. AIDS Epidemiology: A Quantitive Approach. Oxford University Press; New York: 1994. Generalized back-calculation: extension to account for nonstationary incubation distributions; p. 219. [Google Scholar]
- Collaborative Group on AIDS Incubation and HIV Survival, including the CASCADE EU Concerted Action Time from HIV-1 seroconversion to AIDS and death before widespread use of highly-active antiretroviral therapy: a collaborative re-analysis. Lancet. 2000;355:1131–1137. [PubMed] [Google Scholar]
- Duong Y.T., Qiu M., De A.K., Jackson K., Dobbs T., Kim A.A., Nkengasong J.N., Parekh B.S. Detection of recent HIV-1 infection using a new limiting-antigen avidity assay: potential for HIV-1 incidence estimates and avidity maturation studies. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0033328. e33328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall H.I., Song R., Rhodes P., Prejean J., An Q., Lee L.M., Karon J., Brookmeyer R., Kaplan E.H., McKenna M.T., Janssen R.S., HIV Incidence Surveillance Group Estimation of HIV incidence in the United States. JAMA. 2008;300:520–529. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall H.I., Holtgrave D.R., Maulsby C. HIV transmission rates from persons living with HIV who are aware and unaware of their infection. AIDS. 2012;26:893–896. doi: 10.1097/QAD.0b013e328351f73f. [DOI] [PubMed] [Google Scholar]
- Iwamoto A., Taira R., Yokomaku Y., Koibuchi T., Rahman M., Izumin Y., Tadokoro K. The HIV cascade in Japan: Japanese perspectives. PLoS One. 2017;12 doi: 10.1371/journal.pone.0174360. e0174360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen R.S., Satten G.A., Stramer S.L., Rawal B.D., O’Brien T.R., Weiblen B.J., Hecht F.M., Jack N., Cleghorn F.R., Kahn J.O., Chesney M.A., Busch M.P. New testing strategy to detect early HIV-1 infection for use in incidence estimates and for clinical and prevention purposes. JAMA. 1998;280:42–48. doi: 10.1001/jama.280.1.42. [DOI] [PubMed] [Google Scholar]
- MacCarthy S., Hoffmann M., Ferguson L., Nunn A., Irvin R., Bangsberg D., Gruskin S., Dourado I. The HIV care cascade: models, measures and moving forward. J. Int. AIDS Soc. 2015;18:193–195. doi: 10.7448/IAS.18.1.19395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parekh B.S., Kennedy M.S., Dobbs T., Pau C.P., Byers R., Green T., Hu D.J., Vanichseni S., Young N.L., Choopanya K., Mastro T.D., McDougal J.S. Quantitative detection of increasing HIV type 1 antibodies after seroconversion: a simple assay for detecting recent HIV infection and estimating incidence. AIDS Res. Hum. Retroviruses. 2004;18:295–307. doi: 10.1089/088922202753472874. [DOI] [PubMed] [Google Scholar]
- Pharris A., Quinten C., Noori T., Amato-Gauci A.J., van Sighem A., the ECDC HIV/AIDS Surveillance and Dublin Declaration Monitoring Networks Estimating HIV incidence and number of undiagnosed individuals living with HIV in the European Union/ European Economic area, 2015. Euro Surveill. 2016;21:30417. doi: 10.2807/1560-7917.ES.2016.21.48.30417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS/WHO working group on Global HIV/AIDS and SIT surveillance, 2017. Estimating HIV-1 incidence using HIV case surveillance. WHO. https://www.who.int/hiv/pub/meetingreports/estimating-hiv-incidence-using-case-surveillance/en/.
- UNAIDS/WHO working group on Global HIV/AIDS and STI surveillance, 2011. When and how to use assays for recent infection to estimate HIV incidence at a population level. WHO. https://apps.who.int/iris/handle/10665/44612.
- van Sighem A.V., Nakagawa F., Angelis D.D., Quinten C., Bezemer D., De Coul O.E., Egger M., de Wolf Frank, Fraser C., Phillips A. Estimating HIV incidence, time to diagnosis, and the undiagnosed HIV epidemic using routine surveillance data. Epidemiology. 2015;25:653–660. doi: 10.1097/EDE.0000000000000324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wand L., Wilson D., Yan P., Gonnermann A., McDonald A., Kaldor J., Law M. Characterizing trends in HIV infection among men who have sex with men in Australia by birth cohorts: results from a modified back-projection method. J. Int. AIDS Soc. 2009;12:19. doi: 10.1186/1758-2652-12-19. [DOI] [PMC free article] [PubMed] [Google Scholar]