Abstract
Background
Choledocholithiasis is an endemic condition in the world. Although rare, foreign body migration with biliary complications needs to be considered in the differential diagnosis for patients presenting with typical symptoms even many years after cholecystectomy, EPCP, war-wound, foreign body ingestion or any other particular history before. It is of great clinical value as the present review may offer some help when dealing with choledocholithiasis caused by foreign bodies.
Case presentation
We reported a case of choledocholithiasis caused by fishbone from choledochoduodenal anastomosis regurgitation. Moreover, we showed up all the instances of choledocholithiasis caused by foreign bodies published until June 2018 and wrote the world’s first literature review of foreign bodies in the bile duct of 144 cases. The findings from this case suggest that the migration of fishbone can cause various consequences, one of these, as we reported here, is as a core of gallstone and a cause of choledocholithiasis.
Conclusion
The literature review declared the choledocholithiasis caused by foreign bodies prefer the wrinkly and mainly comes from three parts: postoperative complications, foreign body ingestion, and post-war complications such as bullet injury and shrapnel wound. The Jonckheere-Terpstra test indicated the ERCP was currently the treatment of choice. It is a very singular case of choledocholithiasis caused by fishbone, and the present review is the first one concerning choledocholithiasis caused by foreign bodies all over the world.
Keywords: Choledocholithiasis, Common bile duct, Foreign body, Fishbone
Background
The incidence of gallstones is about 15% [1], and the incidence of bile-duct stones accounts for approximately 20% of all gallstones [2]. The calculus in the common bile duct (CBD) may originate from the bile duct system, known as the primary choledocholithiasis. The stones may also have been caused by the decline of stones in the gallbladder, and therefore it is called the secondary choledocholithiasis. The secondary choledocholithiasis is located in the distal of the CBD, which can cause biliary obstruction and infection. Secondary choledocholithiasis is usually considered as an extra-cystic complication of the gallbladder stones, but there are a few exceptions. For example, this paper expounded the case that fishbone entered the CBD through duodenal regurgitation. Choledocholithiasis caused by the foreign body is very rare. There hasn’t been related report about the incidence so far. Choledocholithiasis is mainly manifested as abdominal pain, fever, chills, and jaundice. However, choledocholithiasis caused by the foreign body may present some specific clinical symptoms according to the nature of the foreign body, such as nausea, vomiting, and melena [3, 4]. Primary choledocholithiasis is usually considered to be caused by the translocation of the stones from gall bladder or intrahepatic duct. Nevertheless, patients with secondary choledocholithiasis often have a history of cholecystectomy, EPCP, war-wound, foreign body ingestion, or other particular histories, which need to be paid great attention when diagnosing. The primary treatments for choledocholithiasis are surgery and ERCP currently, and a relatively small proportion of people adopted the methods of conservative treatment [5–7], PTC [8–12] and ESWL [13]. Herein, we report a case of choledocholithiasis caused by fishbone and review all the case reports of choledocholithiasis produced by foreign bodies. A retrospective analysis of the characteristics of the patient population, source of foreign body, clinical manifestation, treatment, and the outcome was conducted. To our knowledge, the present review was the first one concerning choledocholithiasis caused by foreign bodies and may offer some help when dealing with the peculiar secondary choledocholithiasis.
Case presentation
A 69-year-old Chinese woman with a 6-month history of remittent fever, chilling, jaundice, myalgia, fatigue, and mild headache without abdominal pain was referred to our department. The patient had undergone a BillrothII subtotal gastrectomy for the duodenal ulcer with stenosis 14 years before and cholecystectomy, T-tube choledochostomy and choledochoduodenostomy due to CBD inflammatory stenosis 10 years before. There was no tenderness in her abdomen during admission.
Blood investigations showed marked impaired liver function of TBIL 19.5 umol/L, ALT 102 U/L and AST 214 U/L. Markers of inflammation were shown to be elevated in patients, such as WBC 15.38 × 10^9/L, NEU% 88.3, procalcitonin (PCT) 4.40 ng/ml (range, 0–0.05). CA19–9 was elevated at 56.52 U/ml (range, 0–27). Ultrasonographic examination of the biliary tract showed choledocholithiasis (4.4 cm × 2.0 cm) with dilatation of intrahepatic and extrahepatic bile duct (Fig. 1a). Of note, the outer layer of the stone was hyperechoic while the inner layer was hypoechoic. The strange phenomenon suggested that calculi may be made of two components at least. Then the patient underwent the upper abdominal enhanced computed tomography (CT), and the results revealed the muddy stone in intrahepatic bile duct with dilatation and pneumatosis and showed post-subtotal gastrectomy feature. However, the most critical finding which CT revealed was a strip of hyperdense inside the CBD, which was 4.0*2.5 cm with CT values about 57HU (Fig. 1b, c). It was worth mentioning that the patient didn’t have any past medical history about stents implantation. We diagnosed choledocholithiasis with acute obstructive cholangitis initially. However, we still didn’t know the essence of the hyperdense hidden in the bile duct.
Fig. 1.
Exploration and truth of the long high-density shadow. a Abdominal ultrasonography view of the biliary tract shows choledocholithiasis (4.4 cm × 2.0 cm) with dilatation of intrahepatic and extrahepatic bile duct. b Plain CT scan image reveals a strip of hyperdense inside the CBD. c Coronal CT view of the long high-density shadow. d The photographs of the excised specimen showed a sharp linear fishbone
To prevent the patient from getting worse, we recommended ERC or PTC or surgery as a choice to the patient and her family. As the success ratio of ERC or PTC was decreased due to the large size of the choledocholithiasis and the surgery history, which increased the difficulty of ERC and PTC, the patients and her family chose to perform the surgery. Under general anesthesia, laparoscopic common bile duct exploration (LCBDE) was performed on June 19, 2017. The gallbladder had been removed before, and postoperative adhesion of abdominal cavity was severe. After removed the adhesion, the dilated CBD with a diameter of 2.5 cm was revealed. A small incision was made into the CBD on the upper margin of the duodenum. Intraoperative choledochoscope revealed the massive sandy stone in the CBD.
What’s more, a considerable stone about 4.0 cm × 2.0 cm with irregular shape adhered severely to the adjacent structures. The stone was extracted with a retrieval balloon and basket catheter. When we checked out the calculi removed from the bile duct, unexpectedly the stone was broken down, and we found a fishbone inside. The mass with a strip of hyperdense revealed by CT scan was a fishbone, which migrated into the CBD (Fig. 1d). The patient was uneventful when discharged on the eighth postoperative day, and without recurrence until 21 months after the operation (Additional file 1).
Literature review
We reported an unusual case of fishbone-induced choledocholithiasis. In this case, the patient’s Oddi sphincter had lost function due to choledochoduodenostomy before, and the fishbone was able to pass through the choledochoduodenal anastomosis and migrate into the CBD. The fishbone acted as a core to form a mixed stone, with cholesterol as its main component ultimately.
It was secluded that the foreign body was hidden in the bile duct. These clinical manifestations always presented a diagnostic dilemma. This case’s only diagnostic clue was linear and sharp calcification within the mass. However, it was hard to connect the linear calcification to the accidentally ingested fishbone because the CBD was isolated from the digestive tract in principle. Thus, identification and removal of the fishbone as soon as possible are essential.
On the other hand, the hidden foreign body in the CBD is rare and can lead to complications which include foreign body related biliary stones. Most cases have been reported as case reports. This study reviews cases of foreign body migration reported in the literature. Method searches and reviews of the literature from “PubMed” search engines using the keywords “foreign body case” and “bile duct” were carried out. Three hundred ninety-seven papers were identified, but details for only 144 cases were available for the present study [3–133]. We specified a protocol for the inclusion of the literature. First of all, the foreign body doesn’t belong to the human body or isn’t a parasite. Secondly, foreign body causes diseases with abnormal migration. Thirdly, the foreign body was hidden in the CBD.
The median age at diagnosed as stones caused by foreign body was 62 years old (range 5 to 91 years). The senior people (range 41 to 80 years) were too fragile to prevent the foreign body from migrating. There was no statistical significance between the genders (the male made up 47.92% versus female 51.39%).
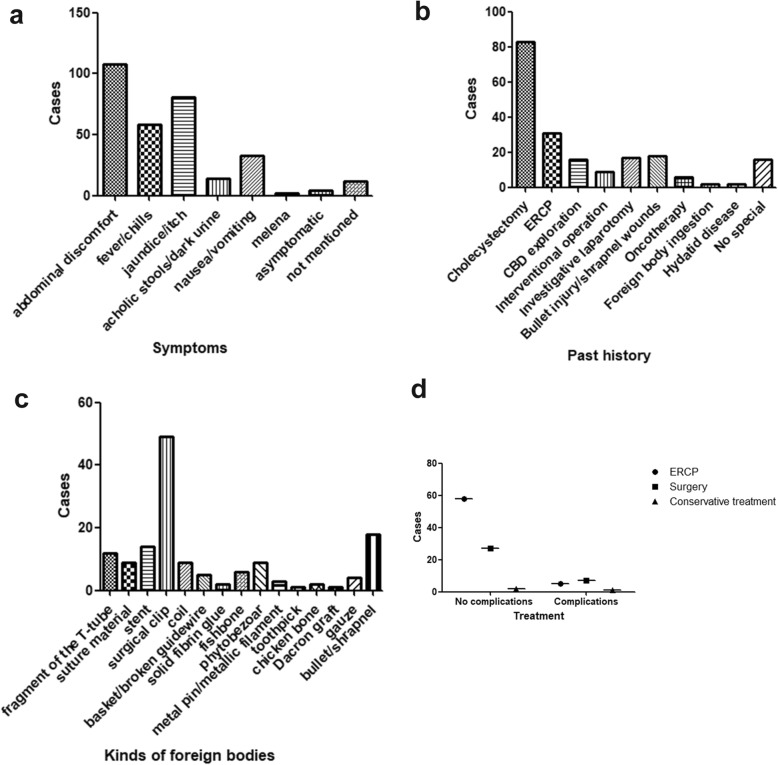
Details of the clinical presentations and past medical history were depicted in Table 1. The most common clinical presentations were abdominal pain, fever/chills, and jaundice (Fig. 2a). Most of these patients had suffered cholecystectomy, and ERCP, followed by bullet injury or shrapnel wounds in third place before the foreign body induced choledocholithiasis (Fig. 2b).
Table 1.
Details of the clinical presentations and past medical history (n = 144)
| Details | N (%) |
|---|---|
| Clinical Symptoms | |
| Abdominal discomfort or abdominal pain | 108 (75.0%) |
| Fever/chills | 58 (40.3%) |
| Jaundice/itch | 81 (56.3%) |
| Acholic stools/dark urine | 14 (9.7%) |
| Nausea/vomiting | 33 (22.9%) |
| Melena | 2 (1.4%) |
| Asymptomatic | 4 (2.8%) |
| Not mentioned | 12 (8.3%) |
| Past Medical History | |
| Cholecystectomy | 83 (57.6%) |
| ERCP (with sphincterotomy/Stenting) | 31 (21.5%) |
| Common bile duct surgery | 16 (11.1%) |
| Embolization/interventional operation | 9 (6.3%) |
| Investigative laparotomy/abdominal surgery | 17 (11.8%) |
| Bullet injury/shrapnel wounds | 18 (12.5%) |
| Surgery/radiotherapy for carcinoma | 6 (4.2%) |
| Foreign body ingestion | 2 (1.4%) |
| Hydatid disease | 2 (1.4%) |
| No special | 16 (11.1%) |
Fig. 2.
Description of CBD foreign body in the literature review. a The different manifestations of foreign body migration patients. b The patients’ history. c Different kinds of foreign bodies. d The different ways to remove the foreign body
There are different kinds of foreign bodies (Fig. 2c). The postoperative complications were the most common cause. The surgical clips (49 accounts for 34.0%), stents (14 accounts for 9.7%) and the fragment of the T-tube (12 accounts for 8.3%) were the most CBD foreign body. There was another kind of foreign body that would pass through the human digestive tract and migrated to the CBD, which included the phytobezoar (9 accounts for 6.3%), fishbone (6 accounts for 4.2%), metal pin (3 accounts for 2.1%), chicken bone (2 accounts for 1.4%)and toothpick (1 accounts for 0.7%). The third significant categories included the debris of bullet or shrapnel (18 accounts for 12.5%).
To choose the best way to remove the foreign body from the CBD, we selected the valid data about the treatment and follow-up. After we made a non-parametric test to compare the outcome about ERCP, surgery and conservative treatment, the Jonckheere-Terpstra test found a significant statistical difference(P = 0.044) and indicated the ERCP was the best way to extract the foreign body while the surgery was chasing closely behind (Fig. 2d). Only a relatively small proportion of people used the methods of conservative treatment [5–7], PTC [8–12] and ESWL [13]. The vast majority of victims (92 accounts for 63.89%) recovered uneventfully and were perfectly well at the follow-up clinical examination, but for others the CBD foreign body migration was an omen of misfortune and disaster, it pushed through victims with long-term problems or complications, such as pancreatitis [27], recurrence of cholesterol stones [90, 92], bile leak [90, 99, 127], subhepatic abscess [127], even death [80, 81].
Discussion and conclusion
Overall, the foreign body migration in the bile duct is rare. However, it is likely that the actual incidence of foreign body migration with resultant biliary complications is underestimated. It’s possible that additional publications, especially in the non-English journals, non-indexed, might have been missed. What’s more, cases of the foreign body hidden in the bile duct might have gone unreported or have been included as part of other types of publications.
In conclusion, although rare, foreign body migration with biliary complications need to be considered in the differential diagnosis for patients presenting with typical symptoms even many years after cholecystectomy, EPCP, war-wound, foreign body ingestion or any other particular history before. The clinical manifestations are similar to that of primary or secondary cholesterol choledocholithiasis, and ERCP is currently the treatment of choice.
This literature review was the first paper concerning on choledocholithiasis caused by foreign bodies and intended to give some suggestions about the differential diagnosis, and the options of treatment for the foreign body migrated to the CBD.
Supplementary information
Additional file 1. Timeline of the case.
Acknowledgements
We thank the patient for her cooperation.
Abbreviations
- CBD
Common bile duct
- CT
Computer tomography
- ERCP
Endoscopic retrograde cholangiopancreatography
- ESWL
Extracorporeal shock wave lithotripsy
- LCBDE
Laparoscopic common bile duct exploration
- PTC
Percutaneous transhepatic cholangio
Authors’ contributions
+MY and BWH are contributed equally to this work. MY and BWH conceived and designed the whole project. YL, YN, ZZ, and SL collected and analyzed the data. BWH interpretation of data and drafted the article. MY gave critical revision of the article for relevant intellectual content. BHH had ensured the questions related to the accuracy and integrity of any part of the work. All authors have read and approved the manuscript.
Funding
This study was sponsored by grants from the Guangdong Provincial Science and Technology Plan projects (No.2016A030313769), National Natural Science Foundation of China (No.81672475), Guangzhou Science and Technology Plan of Scientific Research Projects (No.201707010323).
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Ethics approval and consent to participate
This article is a retrospective study and does not contain any studies with human subjects performed by any of the authors. So, the ethical approval was not necessary, and the Guangdong Provincial People’s Hospital medical ethics committee can offer an exempt ethical statement in support.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Min Yu and Bowen Huang contributed equally to this work.
Contributor Information
Min Yu, Email: yuminzhongda@163.com.
Bowen Huang, Email: huangbowenjack@qq.com.
Ye Lin, Email: forestleaves@126.com.
Yuxue Nie, Email: snowynie@sina.com.
Zixuan Zhou, Email: jay1995jay@sohu.com.
Shanshan Liu, Email: Doctorjane1962@sohu.com.
Baohua Hou, Email: hbh1000@126.com.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12876-019-1088-8.
References
- 1.Verhart JE, Khare M, Hill M, et al. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology. 1999;117:632–639. doi: 10.1016/S0016-5085(99)70456-7. [DOI] [PubMed] [Google Scholar]
- 2.Ponsioen CY. Diagnosis, Differential Diagnosis, and epidemiology of primary Sclerosing cholangitis. Dig Dis. 2015;33(Suppl 2):134–139. doi: 10.1159/000440823. [DOI] [PubMed] [Google Scholar]
- 3.Kusters PJ, Keulen ET, Peters FP. Duodenal perforation following bile duct endoprosthesis placement. Endoscopy. 2014;46(Suppl 1 UCTN):E646–E647. doi: 10.1055/s-0034-1390849. [DOI] [PubMed] [Google Scholar]
- 4.Elewaut A, De Vos M, Huble F, et al. Unusual migration of a straight Amsterdam-type endoprosthesis for bile duct stones. Am J Gastroenterol. 1989;84:674–676. [PubMed] [Google Scholar]
- 5.Barai V, Hedawoo J, Changole S. Forgotten CBD stent (102 months) with stone-stent complex: a case report. Int J Surg Case Rep. 2017;30:162–164. doi: 10.1016/j.ijscr.2016.11.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Girotra M, Dang SM, Rego R. Endoscopic removal of migrated vascular embolic material from the common bile duct: multi-modality approach (with video) Dig Endosc. 2014;26:492–493. doi: 10.1111/den.12237. [DOI] [PubMed] [Google Scholar]
- 7.Onghena T, Vereecken L, Van den Dwey K, et al. Common bile duct foreign body: an unusual case. Surg Laparosc Endosc. 1992;2:8–10. [PubMed] [Google Scholar]
- 8.Carballo RL, Ruiz MI, Jimenez AR, et al. Hepatic abscesses secondary to a foreign body in the common bile duct. Rev Esp Enferm Dig. 2017;109:658. doi: 10.17235/reed.2017.4873/2017. [DOI] [PubMed] [Google Scholar]
- 9.Stephens M, Ruddle A, Young WT. An unusual complication of a dropped clip during laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2010;20:e103–e104. doi: 10.1097/SLE.0b013e3181df9b56. [DOI] [PubMed] [Google Scholar]
- 10.Kaji H, Asano N, Tamura H, et al. Common bile duct stone caused by a fish bone: report of a case. Surg Today. 2004;34:268–271. doi: 10.1007/s00595-003-2670-8. [DOI] [PubMed] [Google Scholar]
- 11.Yoshizumi T, Ikeda T, Shimizu T, et al. Clip migration causes choledocholithiasis after laparoscopic cholecystectomy. Surg Endosc. 2000;14:1188. doi: 10.1007/s04640040030. [DOI] [PubMed] [Google Scholar]
- 12.O’Regan PF, Shanahan F, Lennon JR, et al. Successful endoscopic removal of a common bile duct foreign body. Endoscopy. 1982;14:26–27. doi: 10.1055/s-2007-1021568. [DOI] [PubMed] [Google Scholar]
- 13.Hearne SE, Stump DL. Endoscopic removal of prolene sutures from the common bile duct during endoscopic retrograde cholangiography. Gastrointest Endosc. 1990;36:301–303. doi: 10.1016/S0016-5107(90)71030-9. [DOI] [PubMed] [Google Scholar]
- 14.Sakakida T, Sato H, Doi T, et al. A bile duct stone formation around a fish bone as a Nidus after Pancreatoduodenectomy. Case Rep Gastroenterol. 2018;12:69–75. doi: 10.1159/000486191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zaafouri H, Hasnaoui A, Essghaeir S, et al. Ascending cholangitis secondary to migrated embolization coil of gastroduodenal artery pseudo-aneurysm a case report. BMC Surg. 2017;17:30. doi: 10.1186/s12893-017-0227-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Connell JL, Rosalki SB. Shrapnel biliary calculus; a case report. Br J Surg. 1954;42:218–219. doi: 10.1002/bjs.18004217217. [DOI] [PubMed] [Google Scholar]
- 17.Hurt RL. Penetrating chest wound with lodgement of the foreign body in the common bileduct; case report. Br J Surg. 1947;34:429. doi: 10.1002/bjs.18003413620. [DOI] [PubMed] [Google Scholar]
- 18.Brunaldi VO, Brunaldi MO, Masagao R, et al. Toothpick inside the common bile duct: a case report and literature review. Case Rep Med. 2017;2017:1–4. doi: 10.1155/2017/5846290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ribeiro I, Pinho R, Proenca L, et al. A strange finding in the common bile duct. Gastroenterol Hepatol. 2016;39:531–532. doi: 10.1016/j.gastrohep.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Bent CK, Wright L, Dong PR. “Coildocholithiasis”-common bile duct obstruction secondary to migration of right hepatic artery Pseudoaneurysm coils. J Vasc Interv Radiol. 2016;27:1741–1743. doi: 10.1016/j.jvir.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 21.Patil U, Dhonde A. Endoscopic management of an unusual foreign body in the bile duct. Gastrointest Endosc. 2016;83:1288–1289. doi: 10.1016/j.gie.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 22.Albert JG. “Cutting the wire” as a troubleshooter for a Dormia basket impacted in the common bile duct. Gastrointest Endosc. 2016;83:465. doi: 10.1016/j.gie.2015.08.018. [DOI] [PubMed] [Google Scholar]
- 23.Yang YL, Zhang C, Zhang HW, et al. Common bile duct injury by fibrin glue: report of a rare complication. World J Gastroenterol. 2015;21:2854–2857. doi: 10.3748/wjg.v21.i9.2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Upwanshi MH, Shaikh ST, Ghetla SR, et al. De novo Choledocholithiasis in retained common bile duct stent. J Clin Diagn Res. 2015;9:D17–D18. doi: 10.7860/JCDR/2015/13889.6478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sormaz IC, Keskin M, Sonmez RE, et al. Obstructive jaundice secondary to endoclip migration into common bile duct after laparoscopic cholecystectomy. Minerva Chir. 2015;70:381–383. [PubMed] [Google Scholar]
- 26.Hong T, Xu XQ, He XD, et al. Choledochoduodenal fistula caused by migration of endoclip after laparoscopic cholecystectomy. World J Gastroenterol. 2014;20:4827–4829. doi: 10.3748/wjg.v20.i16.4827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghalim F, Alatawi A, Leblanc S, et al. Endoscopic retrograde cholangioscopic removal of migrated vascular coils from the common bile duct. Clin Res Hepatol Gastroenterol. 2014;38:e31–e32. doi: 10.1016/j.clinre.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 28.Fernandez-Urien I, Marra-Lopez C, Jimenez J. A rare cause of biliary colics. Gastroenterology. 2014;147:e9–10. doi: 10.1053/j.gastro.2014.05.033. [DOI] [PubMed] [Google Scholar]
- 29.Garcia-Gallont R, Velasquez JS, Duarte W. Surgical removal of a severed Dormia basket from the bile duct. Endoscopy. 2014;46(Suppl 1 UCTN):E20–E21. doi: 10.1055/s-0033-1344829. [DOI] [PubMed] [Google Scholar]
- 30.Ray S, Bhattacharya SP. Endoclip migration into the common bile duct with stone formation: a rare complication after laparoscopic cholecystectomy. JSLS. 2013;17:330–332. doi: 10.4293/108680813X13654754534350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zapatier JA, Jani P, Pimentel R, et al. Pancreatic stent migration into the bile duct causing cholangitis. Endoscopy. 2013;45(Suppl 2):E324–E325. doi: 10.1055/s-0033-1344773. [DOI] [PubMed] [Google Scholar]
- 32.Bartos D, Bartos A, Acalovschi I, et al. Biliary plastic stent as a matrix core for lithogenesis in the common bile duct: a rare cause of jaundice. J Gastrointestin Liver Dis. 2012;21:427–429. [PubMed] [Google Scholar]
- 33.Rowe D, Nikfarjam M. Cystic duct clip migration into the common bile duct. Indian J Gastroenterol. 2012;31:86. doi: 10.1007/s12664-011-0155-z. [DOI] [PubMed] [Google Scholar]
- 34.AlGhamdi HS, Saeed MA, AlTamimi AR, et al. Endoscopic extraction of vascular embolization coils that have migrated into the biliary tract in a liver transplant recipient. Dig Endosc. 2012;24:462–465. doi: 10.1111/j.1443-1661.2012.01307.x. [DOI] [PubMed] [Google Scholar]
- 35.Dias R, Dharmaratne P. Ingested foreign body in the common bile duct. J Indian Assoc Pediatr Surg. 2012;17:31–32. doi: 10.4103/0971-9261.91085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sajith KG, Dutta AK, Joseph AJ, et al. Tombstone of surgical clip in common bile duct. Trop Gastroenterol. 2012;33:67–69. doi: 10.7869/tg.2012.12. [DOI] [PubMed] [Google Scholar]
- 37.Bhandari V, Singh M, Vyas HG, et al. Diagnostic dilemma in an unusual case of common bile duct obstruction. Gut Liver. 2011;5:245–247. doi: 10.5009/gnl.2011.5.2.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gonzalez FJ, Dominguez E, Lede A, et al. Migration of vessel clip into the common bile duct and late formation of choledocholithiasis after laparoscopic cholecystectomy. Am J Surg. 2011;202:e41–e43. doi: 10.1016/j.amjsurg.2010.08.011. [DOI] [PubMed] [Google Scholar]
- 39.Gorman DR, Hutson WR. Successful endoscopic removal of metal vascular coils from the biliary tree. Dig Liver Dis. 2011;43:e27. doi: 10.1016/j.dld.2011.05.023. [DOI] [PubMed] [Google Scholar]
- 40.Altun R, Yildirim AE, Ocal S, et al. Coil migration into the common bile duct as a cause of cholangitis. Endoscopy. 2011;43(Suppl 2 UCTN):E33. doi: 10.1055/s-0030-1256024. [DOI] [PubMed] [Google Scholar]
- 41.Martos M, Cosme A, Bujanda L, et al. Obstructive jaundice for biliary mold due to foreign body. Rev Esp Enferm Dig. 2011;103:36–37. [PubMed] [Google Scholar]
- 42.Lee SL, Kim HK, Cho YS. Acute obstructive cholangitis due to foreign body in the common bile duct. Migrated endoclip. Gastroenterology. 2010;139:e3–e4. doi: 10.1053/j.gastro.2009.10.065. [DOI] [PubMed] [Google Scholar]
- 43.Ransibrahmanakul K, Hasyagar C, Prindiville T. Removal of bile duct foreign body by using spyglass and spybite. Clin Gastroenterol Hepatol. 2010;8:e9. doi: 10.1016/j.cgh.2009.08.033. [DOI] [PubMed] [Google Scholar]
- 44.Teicher EJ, Sandhu RS, Dangleben DA, et al. Common duct obstruction by shotgun bullet fragment as a cause of cholangitis. Am Surg. 2010;76:780–782. [PubMed] [Google Scholar]
- 45.Somi MH, Rezaeifar P. Shrapnel splinter in the common bile duct. Arch Iran Med. 2010;13:53–56. [PubMed] [Google Scholar]
- 46.Das K, Basu K, Ray S, et al. Suture material in the common bile duct causing recurrent post-cholecystectomy pain. Endoscopy. 2010;42(Suppl 2):E258. doi: 10.1055/s-0030-1255655. [DOI] [PubMed] [Google Scholar]
- 47.Dokas S, Kalampakas A, Delivorias P, et al. Removal of a large stone growing around and encasing a plastic biliary stent: respect the ductal axis. Dig Liver Dis. 2009;41:319–321. doi: 10.1016/j.dld.2007.10.014. [DOI] [PubMed] [Google Scholar]
- 48.Bansal VK, Misra MC, Bhowate P, et al. Laparoscopic management of common bile duct “Stentolith”. Trop Gastroenterol. 2009;30:95–96. [PubMed] [Google Scholar]
- 49.Goshi T, Okamura S, Takeuchi H, et al. Migrated endoclip and stone formation after cholecystectomy: a case treated by endoscopic sphincterotomy. Intern Med. 2009;48:2015–2017. doi: 10.2169/internalmedicine.48.2634. [DOI] [PubMed] [Google Scholar]
- 50.Hoffman A, Kiesslich R, Galle PR, et al. A 9-year retained T-tube fragment encased within a stone as a rare cause of jaundice. Z Gastroenterol. 2008;46:700. doi: 10.1055/s-2007-963720. [DOI] [PubMed] [Google Scholar]
- 51.Kim KH, Jang BI, Kim TN. A common bile duct stone formed by suture material after open cholecystectomy. Korean J Intern Med. 2007;22:279–282. doi: 10.3904/kjim.2007.22.4.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tsujino T, Sugawara Y, Kawabe T, et al. Foreign body (suture thread) in the bile duct after living donor liver transplantation. Liver Transpl. 2007;13:1065–1066. doi: 10.1002/lt.21139. [DOI] [PubMed] [Google Scholar]
- 53.Steffen M, Kronsbein H, Wesche L. Metal clip as a nidus for formation of common bile duct stone following laparascopic cholecystectomy. Z Gastroenterol. 2007;45:317–319. doi: 10.1055/s-2007-962982. [DOI] [PubMed] [Google Scholar]
- 54.Dolay K, Alis H, Soylu A, et al. Migrated endoclip and stone formation after cholecystectomy: a new danger of acute pancreatitis. World J Gastroenterol. 2007;13:6446–6448. doi: 10.3748/wjg.v13.i47.6446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li ZS, Liao Z. A simple method to remove an embedded self-expandable metallic stent with a balloon. Endoscopy. 2007;39(Suppl 1):E233–E234. doi: 10.1055/s-2007-966582. [DOI] [PubMed] [Google Scholar]
- 56.Mangiavillano B, Masci E. An obstructive, proximally migrated plastic biliary stent extracted with a "modified" Seldinger technique and a polypectomy snare. Endoscopy. 2007;39(Suppl 1):E256. doi: 10.1055/s-2007-966478. [DOI] [PubMed] [Google Scholar]
- 57.Kim TO, Lee SH, Kim GH, et al. Common bile duct stone caused by a phytobezoar. Gastrointest Endosc. 2006;63:324. doi: 10.1016/j.gie.2005.09.037. [DOI] [PubMed] [Google Scholar]
- 58.Aloysius MM, Zaitoun AM, Goddard WP, et al. EUS-guided core biopsy for pseudopapillary tumor of the pancreas. Gastrointest Endosc. 2006;63:155–156. doi: 10.1016/j.gie.2005.06.059. [DOI] [PubMed] [Google Scholar]
- 59.Cimsit B, Keskin M, Ozden I, et al. Obstructive jaundice due to a textiloma mimicking a common bile duct stone. J Hepato-Biliary-Pancreat Surg. 2006;13:172–173. doi: 10.1007/s00534-005-1022-z. [DOI] [PubMed] [Google Scholar]
- 60.Alsulaiman R, Barkun J, Barkun A. Surgical clip migration into the common bile duct after orthotopic liver transplantation. Gastrointest Endosc. 2006;64:833–834. doi: 10.1016/j.gie.2006.04.016. [DOI] [PubMed] [Google Scholar]
- 61.Turaga KK, Amirlac B, Davis RE, Yousef K, Richards A, Fitzgibbons RJ., Jr Cholangitis after coil embolization of an iatrogenic hepatic artery Pseudoaneurysm: unusual case report. Surg Laparosc Endosc Percutan Tech. 2006;16:36–38. doi: 10.1097/01.sle.0000202189.65160.ef. [DOI] [PubMed] [Google Scholar]
- 62.Moghaddam JA, Amini M, Adibnejad S. Development of bile duct bezoars following cholecystectomy caused by choledochoduodenal fistula formation: a case report. BMC Gastroenterol. 2006;6:1. doi: 10.1186/1471-230X-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zuber-Jerger I, Kullmann F. Prevention of food bezoar in the common bile duct by endoscopic stenting. Dig Liver Dis. 2006;38:529–530. doi: 10.1016/j.dld.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 64.Mouzas IA, Petrakis I, Vardas E, et al. Bile leakage presenting as acute abdomen due to a stone created around a migrated surgical clip. Med Sci Monit. 2005;11:S16–S18. [PubMed] [Google Scholar]
- 65.Kamona A, Mansour A, Qandeel M, et al. Biliary obstruction secondary to combat-related foreign bodies: report of two cases. Abdom Imaging. 2005;30:748–749. doi: 10.1007/s00261-005-0325-5. [DOI] [PubMed] [Google Scholar]
- 66.Sandroussi C, Lemech LD, Grunewald B, et al. Late complication following coil embolization of a biliary leak. ANZ J Surg. 2005;75:614–615. doi: 10.1111/j.1445-2197.2005.03444.x. [DOI] [PubMed] [Google Scholar]
- 67.Chong VH, Yim HB, Lim CC. Clip-induced biliary stone. Singap Med J. 2004;45:533–535. [PubMed] [Google Scholar]
- 68.Kim YH, Kim YJ, Park WK, et al. Fish bone as a nidus for stone formation in the common bile duct: report of two cases. Korean J Radiol. 2004;5:210–213. doi: 10.3348/kjr.2004.5.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Dell’Abate P, Del RP, Soliani P, et al. Choledocholithiasis caused by migration of a surgical clip after video laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2003;13:203–204. doi: 10.1089/109264203766207753. [DOI] [PubMed] [Google Scholar]
- 70.Eguchi S, Matsuo S, Hidaka M, et al. Impaction of a shrapnel splinter in the common bile duct after migrating from the right thoracic cavity: report of a case. Surg Today. 2002;32:383–385. doi: 10.1007/s005950200058. [DOI] [PubMed] [Google Scholar]
- 71.Lindstrom E, Ohlsson B, Robertson F, et al. Pin within a bile duct stone. Gastrointest Endosc. 2002;55:912. doi: 10.1067/mge.2002.123905. [DOI] [PubMed] [Google Scholar]
- 72.Haq A, Morris J, Goddard C, et al. Delayed cholangitis resulting from a retained T-tube fragment encased within a stone: a rare complication. Surg Endosc. 2002;16:714. doi: 10.1007/s00464-001-4235-5. [DOI] [PubMed] [Google Scholar]
- 73.Tsumura H, Ichikawa T, Kagawa T, et al. Failure of endoscopic removal of common bile duct stones due to endo-clip migration following laparoscopic cholecystectomy. J Hepato-Biliary-Pancreat Surg. 2002;9:274–277. doi: 10.1007/s005340200032. [DOI] [PubMed] [Google Scholar]
- 74.Froehlich F, Nussbaumer F, Worreth M. Broken T-tube branch causing bile duct stone. Gastrointest Endosc. 2001;54:494–495. doi: 10.1067/mge.2001.117960. [DOI] [PubMed] [Google Scholar]
- 75.Matsumoto H, Ikeda E, Mitsunaga S, et al. Choledochal stenosis and lithiasis caused by penetration and migration of surgical metal clips. J Hepato-Biliary-Pancreat Surg. 2000;7:603–605. doi: 10.1007/s005340070011. [DOI] [PubMed] [Google Scholar]
- 76.Baldota S, Breach C, Murtuza B, et al. Chicken bone injury of the common bile duct. J R Soc Med. 2000;93:84. doi: 10.1177/014107680009300213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bayar S, Saxena R, Salem RR. Foreign body reaction to a metal clip causing a benign bile duct stricture 16 years after open cholecystectomy: report of a case. Surg Today. 2000;30:534–536. doi: 10.1007/s005950070122. [DOI] [PubMed] [Google Scholar]
- 78.Hatzidakis AA, Karampekios S, Tsetis D, et al. Percutaneous foreign body retrieval through the biliary tract with the Nitinol goose-neck snare. Eur Radiol. 2000;10:1355. doi: 10.1007/s003309900285. [DOI] [PubMed] [Google Scholar]
- 79.Ng WT, Kong CK, Lee WM. Migration of three endoclips following laparoscopic cholecystectomy. J R Coll Surg Edinb. 1999;44:200–202. [PubMed] [Google Scholar]
- 80.Alberts MS, Fenoglio M, Ratzer E. Recurrent common bile duct stones containing metallic clips following laparoscopic common bile duct exploration. J Laparoendosc Adv Surg Tech A. 1999;9:441–444. doi: 10.1089/lap.1999.9.441. [DOI] [PubMed] [Google Scholar]
- 81.Simmons TC, Essilfie W, Fleming A. Obstructive jaundice occurring 40 months after gunshot wound to the left thoraco-abdomen. Gastrointest Endosc. 1998;48:423–425. doi: 10.1016/S0016-5107(98)70017-3. [DOI] [PubMed] [Google Scholar]
- 82.Loveday EJ. A migrating biliary wallstent: an unusual complication. Clin Radiol. 1997;52:246. doi: 10.1016/S0009-9260(97)80286-3. [DOI] [PubMed] [Google Scholar]
- 83.Pescatore P, Meier-Willersen HJ, Manegold BC. A severe complication of the new self-expanding spiral nitinol biliary stent. Endoscopy. 1997;29:413–415. doi: 10.1055/s-2007-1004226. [DOI] [PubMed] [Google Scholar]
- 84.Cetta F, Lombardo F, Baldi C. Clip migration within the common duct after laparoscopic cholecystectomy a case of transient acute pancreatitis in the absence of a source. Endoscopy. 1997;29:S59–S60. doi: 10.1055/s-2007-1004338. [DOI] [PubMed] [Google Scholar]
- 85.Muhammad SR, Gatehouse D. Removal of a retained T-tube from the common bile duct. J Pak Med Assoc. 1997;47:194–195. [PubMed] [Google Scholar]
- 86.Schutz SM, Chinea C, Friedrichs P. Successful endoscopic removal of a severed, impacted Dormia basket. Am J Gastroenterol. 1997;92:679–681. [PubMed] [Google Scholar]
- 87.Bradfield H, Granke D. Surgical clip as a nidus for a common bile duct stone: radiographic demonstration. Abdom Imaging. 1997;22:293–294. doi: 10.1007/s002619900192. [DOI] [PubMed] [Google Scholar]
- 88.Shibata S, Okumichi T, Kimura A, et al. A case of choledocholithiasis with an endoclip nidus, 6 months after laparoscopic cholecystectomy. Surg Endosc. 1996;10:1097–1098. doi: 10.1007/s004649900249. [DOI] [PubMed] [Google Scholar]
- 89.Brogdon BG, Neuffer FH, Siner JR. Choledochal ‘clipoliths’ after cholecystectomy. South Med J. 1996;89:1111–1113. doi: 10.1097/00007611-199611000-00020. [DOI] [PubMed] [Google Scholar]
- 90.Savader SJ, Brodkin J, Osterman FJ. In situ formation of a loop snare for retrieval of a foreign body without a free end. Cardiovasc Intervent Radiol. 1996;19:298–301. doi: 10.1007/BF02577656. [DOI] [PubMed] [Google Scholar]
- 91.Entel RJ, Peebles MW. Migratory surgical clip in the common bile duct: CT diagnosis. Abdom Imaging. 1996;21:329–330. doi: 10.1007/s002619900074. [DOI] [PubMed] [Google Scholar]
- 92.Silvis SE, Meier PB, Nelson DB. The use of a wire mesh stent in treating biliary obstruction caused by shrapnel. Gastrointest Endosc. 1996;44:741–746. doi: 10.1016/S0016-5107(96)70066-4. [DOI] [PubMed] [Google Scholar]
- 93.Lamotte M, Kockx M, Hautekeete M, et al. Biliary phytobezoar: a medical curiosity. Am J Gastroenterol. 1995;90:1346–1348. [PubMed] [Google Scholar]
- 94.Tsai CC, Mo LR, Lin RC, et al. Delayed spontaneous migration of Gianturco-Rosch metallic stent from the biliary tree. Eur J Radiol. 1995;20:221–223. doi: 10.1016/0720-048X(95)00658-D. [DOI] [PubMed] [Google Scholar]
- 95.Martinez J, Combs W, Brady PG. Surgical clips as a nidus for biliary stone formation: diagnosis and therapy. Am J Gastroenterol. 1995;90:1521–1524. [PubMed] [Google Scholar]
- 96.Rizzo J, Tripodi J, Gold B, et al. Surgical clips as a nidus for stone formation in the common bile duct. J Clin Gastroenterol. 1995;21:169–171. doi: 10.1097/00004836-199509000-00022. [DOI] [PubMed] [Google Scholar]
- 97.Szanto I, Gamal EM, Banai J, et al. Common bile duct stone formation induced by tomato skin following endoscopic sphincterotomy. Endoscopy. 1994;26:712. doi: 10.1055/s-2007-1009077. [DOI] [PubMed] [Google Scholar]
- 98.Thors H, Gudjonsson H, Oddsson E, et al. Endoscopic retrieval of a biliary T-tube remnant. Gastrointest Endosc. 1994;40:241–242. doi: 10.1016/S0016-5107(94)70179-2. [DOI] [PubMed] [Google Scholar]
- 99.Uomo G, Manes G, Laccetti M, et al. Necrotizing acute pancreatitis due to a common bile duct foreign body. Am J Gastroenterol. 1994;89:1109–1110. [PubMed] [Google Scholar]
- 100.Benakis P, Nicolakis D, Triantafillidis JK. Successful endoscopic removal of part of a T-tube from the common bile duct. Endoscopy. 1994;26:756. doi: 10.1055/s-2007-1009097. [DOI] [PubMed] [Google Scholar]
- 101.Sato T, Denno R, Yuyama Y, et al. Unusual complications caused by endo-clip migration following a laparoscopic cholecystectomy: report of a case. Surg Today. 1994;24:360–362. doi: 10.1007/BF02348568. [DOI] [PubMed] [Google Scholar]
- 102.Kelly MD, Hugh TB. Cherry stalk in the common bile duct. Aust N Z J Surg. 1993;63:571–574. doi: 10.1111/j.1445-2197.1993.tb00457.x. [DOI] [PubMed] [Google Scholar]
- 103.Arnaud JP, Bergamaschi R. Migration and slipping of metal clips after celioscopic cholecystectomy. Surg Laparosc Endosc. 1993;3:487–488. [PubMed] [Google Scholar]
- 104.Mansvelt B, Harb J, Farkas B, et al. “Clip-stone” filiation within the biliary tract. HPB Surg. 1993;6:185–188. doi: 10.1155/1993/35965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wu WC, Katon RM, JH MA. Endoscopic management of common bile duct stones resulting from metallic surgical clips (eat's eye calculi) Gastrointest Endosc. 1993;39:712–715. doi: 10.1016/S0016-5107(93)70231-X. [DOI] [PubMed] [Google Scholar]
- 106.Cetta F, Lombardo F, Rossi S. Large foreign body as a nidus for a common duct stone in a patient without spontaneous biliary enteric fistula or previous abdominal surgery. HPB Surg. 1993;6:235–242. doi: 10.1155/1993/51546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Gay P, Gaddie D. Perforation of the stomach by fish bone producing delayed transient obstructive jaundice. Aust N Z J Surg. 1993;63:826–827. doi: 10.1111/j.1445-2197.1993.tb00352.x. [DOI] [PubMed] [Google Scholar]
- 108.Raoul JL, Bretagne JF, Siproudhis L, et al. Cystic duct clip migration into the common bile duct: a complication of laparoscopic cholecystectomy treated by endoscopic biliary sphincterotomy. Gastrointest Endosc. 1992;38:608–611. doi: 10.1016/S0016-5107(92)70531-8. [DOI] [PubMed] [Google Scholar]
- 109.Matsuura T, Kanisawa Y, Sato T, et al. Migration of "endo-clips" into common bile-duct after laparoscopic cholecystectomy. Lancet. 1992;340:306. doi: 10.1016/0140-6736(92)92394-U. [DOI] [PubMed] [Google Scholar]
- 110.Ghazanfari K, Gollapudi PR, Konicek FJ, et al. Surgical clip as a nidus for common bile duct stone formation and successful endoscopic therapy. Gastrointest Endosc. 1992;38:611–613. doi: 10.1016/S0016-5107(92)70532-X. [DOI] [PubMed] [Google Scholar]
- 111.Mitchell R, Kerr R, Barton J, et al. Biliary obstruction secondary to shrapnel. Am J Gastroenterol. 1991;86:1531–1534. [PubMed] [Google Scholar]
- 112.David X, Bories P, Parelon G, et al. Acute pancreatitis induced by “herbs of Provence”. Lancet. 1991;337:311. doi: 10.1016/0140-6736(91)90934-H. [DOI] [PubMed] [Google Scholar]
- 113.Cardin F, Fritsch J, Aubert A, et al. Two-stage endoscopic removal of a foreign body from the common bile duct. Surg Endosc. 1991;5:94–95. doi: 10.1007/BF00316846. [DOI] [PubMed] [Google Scholar]
- 114.Goh PM, Sim EK, Isaac JR. Endoscopic extraction of a proximally migrated Amsterdam-type biliary endoprosthesis. Gastrointest Endosc. 1990;36:539–540. doi: 10.1016/S0016-5107(90)71143-1. [DOI] [PubMed] [Google Scholar]
- 115.Banez VP, Leung JW, Lau WY. Endoscopic management of an unusual intrabiliary foreign body. Br J Surg. 1990;77:882. doi: 10.1002/bjs.1800770812. [DOI] [PubMed] [Google Scholar]
- 116.Sakai P, Ishioka S, Zambrano M, et al. Endoscopic removal of an atypical common bile duct foreign body. Endoscopy. 1990;22:93. doi: 10.1055/s-2007-1012806. [DOI] [PubMed] [Google Scholar]
- 117.Janson JA, Cotton PB. Endoscopic treatment of a bile duct stone containing a surgical staple. HPB Surg. 1990;3:67–71. doi: 10.1155/1990/53506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Merrett M, Desmond P. Removal of impacted endoscopic basket and stone from the common bile duct by extracorporeal shock waves. Endoscopy. 1990;22:92. doi: 10.1055/s-2007-1012805. [DOI] [PubMed] [Google Scholar]
- 119.Ormann W. A thread as a nidus of a common bile duct calculus--findings during endoscopic lithotripsy. Endoscopy. 1989;21:191–192. doi: 10.1055/s-2007-1012940. [DOI] [PubMed] [Google Scholar]
- 120.Niebuhr H, Nowak H, Tichbi E. A grenade splinter as the cause of cholangitis and icterus. Dtsch Med Wochenschr. 1989;114:1283–1285. doi: 10.1055/s-2008-1066754. [DOI] [PubMed] [Google Scholar]
- 121.Davis M, Hart B, Kleinman R. Obstructive jaundice from open vessel clip. Gastrointest Radiol. 1988;13:259–260. doi: 10.1007/BF01889075. [DOI] [PubMed] [Google Scholar]
- 122.Orda R, Leviav A, Ratan I. Common bile duct stone caused by a foreign body. J Clin Gastroenterol. 1986;8:466–468. doi: 10.1097/00004836-198608000-00018. [DOI] [PubMed] [Google Scholar]
- 123.Danzi JT. Two cases of acute pancreatitis due to a foreign body. Gastrointest Endosc. 1986;32:360–361. doi: 10.1016/S0016-5107(86)71888-9. [DOI] [PubMed] [Google Scholar]
- 124.Rudiger E, Weiss E, Schludermann W. Postoperative complications of gallbladder stones. Endoscopy. 1985;17:85. doi: 10.1055/s-2007-1018466. [DOI] [PubMed] [Google Scholar]
- 125.Siegel JH. Biliary bezoar: the sump syndrome and choledochoenterostomy. Endoscopy. 1982;14:238. doi: 10.1055/s-2007-1021630. [DOI] [PubMed] [Google Scholar]
- 126.Edwards FH, Davies RS. Late post-traumatic obstructive jaundice secondary to a biliary tract foreign body. J Trauma. 1982;22:336–338. doi: 10.1097/00005373-198204000-00015. [DOI] [PubMed] [Google Scholar]
- 127.Brutvan FM, Kampschroer BH, Parker HW. Vessel clip as a nidus for formation of common bile duct stone. Gastrointest Endosc. 1982;28:222–223. doi: 10.1016/S0016-5107(82)73080-9. [DOI] [PubMed] [Google Scholar]
- 128.Klein E, Schneebaum S, Feuchtwanger MM, et al. Shell splinter in the common bile duct: a rare cause of obstructive jaundice. Am J Surg. 1981;141:376–377. doi: 10.1016/0002-9610(81)90200-2. [DOI] [PubMed] [Google Scholar]
- 129.Rao BK, Lieberman LM. Intermittent common bile duct obstruction at ampulla of Vater due to chicken bone impaction: diagnosis by hepatobiliary imaging. Clin Nucl Med. 1981;6:59–61. doi: 10.1097/00003072-198102000-00003. [DOI] [PubMed] [Google Scholar]
- 130.Prinz RA, Pickleman J. Common bile duct obstruction associated with a dacron H-graft portacaval shunt. Arch Surg. 1978;113:333–335. doi: 10.1001/archsurg.1978.01370150105027. [DOI] [PubMed] [Google Scholar]
- 131.Weithofer G, Blazek Z, Warm K, et al. Spontaneous expulsion of a migrating infantry missile impacted in the duodenum and the common bile duct, 32 years after wounding. Endoscopy. 1977;9:106–109. doi: 10.1055/s-0028-1098501. [DOI] [PubMed] [Google Scholar]
- 132.Rhomberg HP, Judmair G, Bodner E. Grenade splinter causing biliary colic. Lancet. 1977;1:201. doi: 10.1016/S0140-6736(77)91810-4. [DOI] [PubMed] [Google Scholar]
- 133.Krontiris A, Tsironis A. Common duct obstruction by a bullet compression cap: a rare case. Ann Surg. 1962;156:303–306. doi: 10.1097/00000658-196208000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Timeline of the case.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.