Abstract
Nurses are at the forefront of providing healthcare services to individuals of all age groups and with varying medical conditions. Aside from the critical knowledge and technical skills from nursing science, advancement in technology has assisted nurses in delivering quality nursing care by streamlining workflow processes and ensuring that data can easily be retrieved or modified. Electronic health records dramatically changed the landscape of the healthcare practice by providing an electronic means to store data and for healthcare professionals to retrieve and manipulate health information in a secured and collaborative environment. But with the nature of data being stored in the electronic health records, nurses still need to organize and process these data into relevant information, knowledge or wisdom so they can provide better holistic care to patients. This discussion paper details the role of content management systems in addressing nursing workflow by providing a mechanism for nurses to be developers themselves, and not just users or consumers of health innovative technologies. By using content management systems as platform for application development, nurses or other healthcare professionals, may be able to address problems with internal workflow without having to incur huge amounts in software development, or having to extensively learn programming languages.
Keywords: Content management system, Electronic health records, Software, Health personnel, Nursing informatics, Programming languages, Workflow
What is known?
-
•
Data management is a crucial aspect of healthcare innovations. Clinical data provide a holistic and collaborative understanding of the clinical condition, and the management of patient care.
-
•
Implementations and deployments of electronic medical records have been vast, particularly in developed countries. The electronic medical record, however, can be thought of as a repository of patient data. Human cognitive perception is still needed to provide meaning to the data stored in the electronic records.
What is new?
-
•
Content management systems can be used when storing synthesized data based on human understanding. Focusing on transforming these stored electronic clinical data into information, knowledge and wisdom is part of data utilization to provide safe and effective patient care.
1. Nurse and the EHR
The evolution of the profession of nursing does not only depend on how nursing as a science evolves, but how interrelated or interdependent fields of study progress as well. Nurses owe their knowledge in pathology and physiology from discoveries made by scientists in the medical sciences, and from nurses engaged in the field of pathophysiological research, as with those nurse scientists working in the areas of symptoms management, diabetes management and genetic research. The expansion in the knowledgebase in computer, information and cognitive sciences paved the way for nursing informatics to be realized as a crucial field for nurses, either as fundamental tool for beginning nurses or as a specialty field for nurse informaticians.
The electronic health record (EHR) is a product of interdepartmental and interdisciplinary collaboration to address a common concern in the healthcare industry - how to store, retrieve and manipulate patient data in a secured and collaborative environment. There are glaring differences between fully implementing a basic EHR compared to no implementation or not fully implemented. In a setting where there is no basic EHR or if the EHR is not fully implemented, vital patient information tend to get lost during change of shift reports. There is greater possibility that patient safety and quality of care could be compromised. Nurses were also found not confident enough in assessing patient’s readiness for discharge. In places where there is full implementation of basic EHR, there was enhanced or more efficient nursing care, and better coordination of care and patient safety [1].
Aside from storing clinical information for later retrieval, current electronic medical records have add-on features. An integrated clinical decision support system (CDSS) based on intuitive data entry forms could allow data input parameters to be patterned based on the CDSS architecture to address both acute and chronic health conditions [2]. Patient access to personal health record (PHR) is crucial, and some EHR integrate PHR within their system. Among the three configurations of a PHR - standalone, tethered, integrated - researchers have found that only the integrated approach has the true transformative potential when it comes to patients being able to manage their own health. Having a PHR module within the EHR improves the quality and portability of patient information; enables real-time communication between patient and provider; and improves patient knowledge on health [3]. Content templating, such as physician progress and unit reports, may be available in some EHR’s. These templating modules assist healthcare providers in accessing pertinent information that is vital to provision of patient care.
The impact of EHR integration in the hospital system is a significant one, particularly to nurses caring for patients at the bedside. There was a change on how nurses spent time in certain activities, such as the amount of time interacting with computers; though the impact was uniformly dispersed among other activities. The duration and frequency of activities done by nurses were not adversely changed by the introduction of additional healthcare innovations. There was also no significant change in the time spent by nurses with their patients, verbally interacting with them, as the nurses try to integrate the change in workflow to accommodate health information systems in their normal routine [4]. This says a great deal about the flexibility of nurses when it comes to adapting to changes in the workflow system. By balancing their use of computers and patient care, nurses could reap the benefit of the integration of health information technology into the field of healthcare.
The design of clinical systems should address particular workflow and must be done on a continuous and iterative approach based on identified needs. A crucial module in any electronic health record system is the computerized provider order entry or CPOE. Benefits of CPOE include readable and understandable physician orders, the ability of systems to be accessed remotely, and reduced order turnaround times [5]. A study conducted revealed the CPOE can affect clinical work. It can cause interaction difficulties between computer systems and users. It can cause changes in the dynamics of clinical workflow. It may also address only a subcomponent of the totality of the workflow for various clinical personnel. CPOE modules may diminish awareness of the clinical situation. And lastly, in terms of organizational operation, a poorly designed CPOE could ultimately mirror the quality of internal policies and procedures [6].
Health information systems (HIS) are information technology systems applied to healthcare with four crucial functions: (1) to generate data, (2) to compile or aggregate data, (3) to analyze and synthesize data, and (4) to communicate and use data [7]. Healthcare institutions use HIS’s in gathering, synthesizing and storing data, and in the exchange of information in the decision-making phase at various sectors of healthcare service to promote quality [8]. These systems are built to streamline the workflow processes in the hospital or any healthcare setting.
A crucial element in the success of HIS implementation is acceptance by users, particularly nurses. No matter how advanced the system is or its associated modules or peripherals, if there is poor acceptance by users, problems in usability can occur. Education and training play a vital role in introducing new information systems to frontline personnel. Before, during and after HIS go-live implementation, nurse informaticians have the role of assisting nurses assimilate into the new workflow environment, and to gather necessary feedbacks to help improve the overall EHR experience. Time is also an important element when it comes to acceptance. A study revealed that nurses in the intensive care unit were more accepting of the EHR system at twelve (12) months compared to three (3) months after EHR implementation [9].
The integration of information technology innovations in healthcare does not only bring benefits to the organization. Sometimes, a change in the status quo could also usher in disruptive change on the negative side. Though nurses perceived the retrievability of data as one of the strengths of the electronic medical record, other nurses observed the lack of relevance in documentation as one of the barriers [10]. A field study of hospitals in Saudi Arabia highlighted six (6) main categories of barriers to the implementation of health information systems: human, professional, technical, organizational, financial, and legal or regulatory barriers. Of the six identified main categories, human and financial barriers are the two prominent categories of barriers to successful EMR implementation [11]. Before deploying any EMR system, the implementing institution must assess the readiness of its personnel and the impact the system will have in the different healthcare professionals. If the overall cost of EMR deployment is burdensome for the organization, if it does not have the determination and concrete policies on deploying an EMR system, or if it does not have the technical capabilities to implement the system, it is unlikely that the organization would deploy an EMR system. Due diligence must be exercised to make sure the chosen EMR system adheres to laws and implementing rules and regulations of a particular state or country. No matter how advanced the EMR system is, if it does not follow legal or regulatory requirements, the implementing institution may choose to delay deployment of an EMR system, or make the necessary modifications to the system - that could cost more.
Gathering feedback from users of health information systems is a crucial part of health information technology implementation. The integration of electronic medical records in the workflow of nurses may cause disturbance in daily routine. It is imperative that nurses be included in the design of health information systems since nurses form bulk of the clinical personnel in the hospital, and any disruption in the nursing workflow could ultimately affect individualized care and patient safety. It has been shown that the implementation of health information systems has a negative impact on nurses when the system is not adequately designed. Nurses should be involved in software design aspect so that the core and intricacy of nursing does not disappear in the system architecture [12,13].
To highlight the importance of gathering feedbacks from or including nurses in the software development process, a technology company in Hong Kong devised an electronic nursing information system for use by nurses in the operating theater. The information system was designed using free and open source software components. This means the source code is readily available, and can have features extended based on the needs of nurses. The operating theater information system utilized Joomla as the content management system (CMS). The Joomla system designed used MySQL for database management, PHP as web application programming language, and Linux as operating system. The main objective of the electronic nursing information system is to eliminate human error in documenting instrument count related to illegible handwriting or records that are unaccounted for [14]. This nursing information system deployment clearly illustrates the potential of CMSs to enhance nursing clinical workflow.
2. Data-information-knowledge-wisdom Continuum
Information management forms a vital part of the nursing workflow. Even before the introduction of health information technology innovations, such as the electronic medical records, nurses have been keeping record of care rendered to patients, clinical assessments, procedures done and medications administered through chart entries. A summary of patient care can also be found in the nursing kardex which is a tool used by nurses to condense healthcare information necessary for patient care. The need to organize and synthesize data to produce relevant information or knowledge is crucial in the nurse’s decision making process.
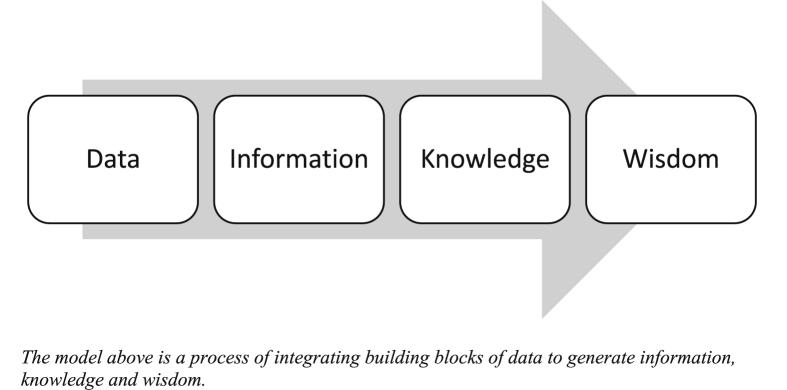
The Data-Information-Knowledge-Wisdom (DIKW) Continuum is a concept of synthesizing data to have meaningful information to produce the knowledge necessary to have the right wisdom to make informed clinical decisions with regards to patient care. Data is the most fundamental and discrete element of the DIKW model, and is produced either through manual or automated methods of observation. Information happens when meaning is attached to organized and processed data, and is created by integrating various data points to form a meaningful depiction of the situation. When information is further organized and processed, knowledge is produced. Knowledge is a body of meaningful information composed of discrete data so that relations and interactions are defined and operationalized, and is generally influenced by assumptions and norms of a particular field of practice. When the nurse has the sufficient knowledgebase, the nurse can now use this knowledge in making clinical decisions with regards to patient care. Wisdom is the utilization of the knowledge acquired from meaningful information to clinical judgment, and is related to the nurse’s capacity to make informed clinical judgment based on the knowledge the nurse has accumulated [[15], [16], [17]] (see Fig. 1).
Fig. 1.
The Data-Information-Knowledge-Wisdom model.
One of the important features of most electronic medical records is the ability to layout patient care summary based on information stored in the database. Assessment data, such as blood pressure, heart rate and temperature, can be further combined with medication administration data, such as the medication name and dosage, to build information and knowledge on how an individual patient’s body would react to a particular drug at a specified dose. This could then aid the physician in developing wisdom on how to manage the patient’s blood pressure on an individualized basis. For nurses, this could provide wisdom to reinforce the need for evaluating the patient before and after intervention, since even though the blood pressure and heart rate can be affected by anti-hypertensive medications, the nurse must first assess whether changes in heart rate from baseline could have been caused by an increase in body temperature [18,19].
The patient care summary is generally an electronic template where needed patient information is summarized. An electronic patient care summary is similar to the nursing kardex where nurses can browse through patient information without having to go through modules or sections of the health information system. Templating of patient care information or summary is a process of transforming data stored in the electronic medical record into relevant information or knowledge needed to provide quality nursing care. However, in order for the patient care summary template or module to be useful to nurses, the template and its content should be relevant to the workflow of nurses. If the summary does not provide enough cognitive support to nurses - as with templates designed solely for physicians, or if the layout is inadequate, inflexible and does not display evident information, or assist nurses encode information, the chances of the patient summary being used in actual clinical setting would be slim [20].
Another area where nurses could benefit from electronic templating is shift reports or bedside rounds. The exchange of information from the ongoing to the incoming shift is vital in providing continuity of patient care. Reports should not be lengthy narratives, but be concise and should capture the overall patient condition - outlining relevant events that took place and plan of care. The Situation-Background-Assessment-Recommendation (SBAR) protocol is a format that nurses use to present information when conducting bedside rounds. Using this method, nurses are able to provide a more directed and efficient way of communication. With a standardized electronic template tailored for nursing workflow, there is reduction in time spent for change-of-shift reports, decreased end-of-shift overtime, and a more homogenized process of information exchange. There is also enhancement in the quality of information and fulfillment with the process among staff members. The use of electronic templating or information layout is an integral processes of synthesizing data from the EHR. Nurses working at the bedside are in a strategic position to influence change that could benefit hospital operations and clinical practice [21,22].
The institution may decide to adopt an interdisciplinary or interdepartmental approach in preparing an electronic template module for patient care summary based on the available features of the electronic medical record. Although there may be variation on the type of patient care templating system for nurses and physicians, some informational needs of nurses overlap with that of physicians. Creating an information layout that will address both the concerns of nurses and physicians means there is conformity in the patient care summary and the overall direction of the plan of care. Examples of overlapping informational needs are brief history of present admission, plan for discharge, medication regimen and contemplated surgical intervention. Doing so may boost the consistency of data shared during change of shift, facilitate the formulation of mutuality, and promote communication among disciplines [23].
3. Content management systems
Templating of patient care summary can be built as a module on the electronic medical record - either as custom built for the institution or shipped with the system using a predefined layout. A custom built solution is tailored to the specific needs of the organization, but may incur additional expense in planning, development, implementation, and future modifications. A patient care summary module integrated with the system would have a predefined layout, and may not allow customization based on identified needs of the hospital. This is where the CMS can be a solution to address nursing workflow.
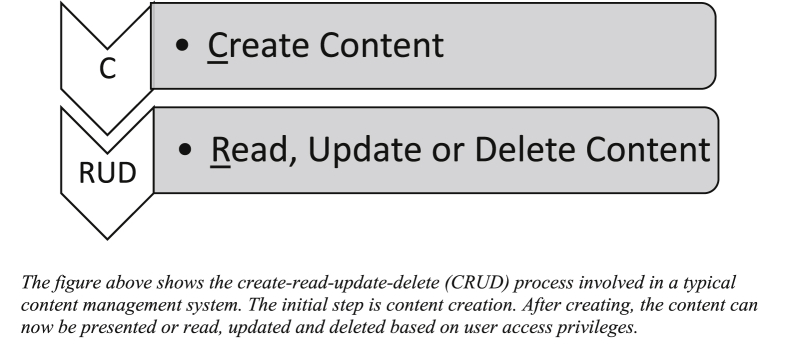
CMSs are information technology systems that allow access, creation, modification and deletion of content based on established access roles. These systems also allow users to expand layout and functionality using plugin and theme architectures. A CMS has a more complex architecture than application frameworks that would allow non-programmers to design and build web applications without a solid background in coding. Applications built using CMSs, however, may not be that flexible, extensible or scalable than when using application frameworks (see Fig. 2).
Fig. 2.
Content management system.
Of the various open source CMSs available, the three popular ones are WordPress, Drupal and Joomla. WordPress is the most popular CMS with the greatest install base, the highest number of searches in the Google search engine, and ranks high among CMS users when it comes to ease of use. Features and functionalities of WordPress-based applications can be extended using a variety of plugins available in the plugins directory. The presentation layout or template is also readily modifiable using themes in the theme directory [24]. For nurse developers with knowledge in PHP Hypertext Preprocessor (PHP) - the programming language of WordPress - they can alter the functionality and template presentation of the web applications that they are building at the code level, giving them more flexibility and creativity in integrating feature-rich modules.
WordPress started as a blogging platform that eventually expanded into a fully featured CMS and application development platform, particularly for non-programmers. Being an open source project and with the ease of use and extensibility offered by the CMS through its theme and plugin architecture, the Open Nursing Information System or Open-NIS Project was created to promote the use of CMSs , specifically WordPress and WordPress-based CMSs, such as ClassicPress, in the field of healthcare technology innovation. By providing open standards on how content management systems can be applied in the context of health information technology, the Open-NIS Project aims to promote and inspire nurses to become developers of nursing workflow systems, and be part of addressing nursing workflow issues in their respective healthcare organizations [25].
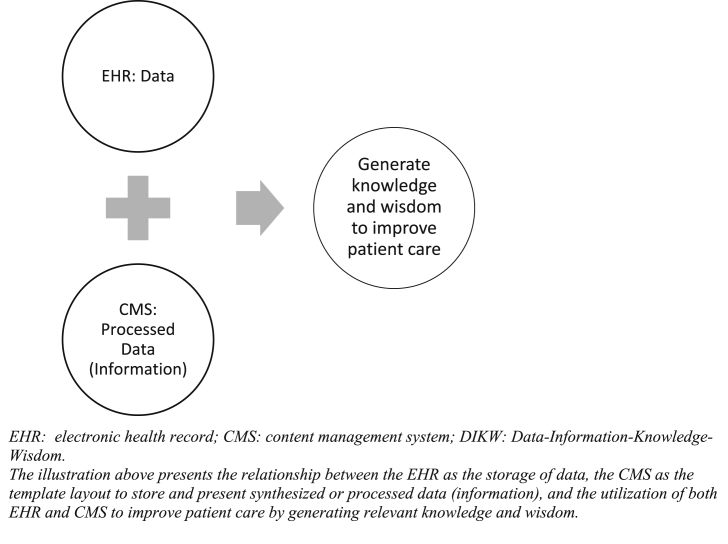
CMSs can be used in conjunction with electronic medical records. The CMSs can serve to augment functionalities of data handling to address nursing workflow efficiency, particularly those lacking in the electronic medical record system in terms of built-in features or customizability. Since the prominent function of an electronic health record system is to store data and make data available for retrieval and reporting, its purpose is to address the data section of the DIKW framework. CMSs could address the information, knowledge and wisdom sections of the model by storing and presenting information or data that has already been organized and synthesized by the nurse. This is analogous to how the nursing kardex was designed. The nursing kardex was not designed to replace nurse’s notes, medication administration records or nursing care plans, nor is it part of the permanent record of the patient. Its main purpose is to augment nursing workflow by providing patient care summary that is relevant to how provision of care is done in a particular ward or unit [26]. In the same way, electronic medical records may not fully address the needs of nurses for the synthesis and transmission of information that is aligned to how processes and procedures are done in the organization or in a particular unit. This is where the value of CMSs comes in. This has been shown outside the realm of healthcare information technology, such as libraries and research institutes that also utilize WordPress and Joomla in managing data internally [27,28] (see Fig. 3).
Fig. 3.
Content management and DIKW.
4. Nurse as a developer
Nurses, as part of the healthcare force, are users or consumers of healthcare information technology innovations. These innovations have been beneficial in making workflow as efficient as possible by digitizing the storage of data and providing ease in the retrieval and manipulation of needed healthcare information. It is also interesting to view nurses as developers of health technology innovations as well, not just users of healthcare systems. Being at the forefront of patient care, nurses are valuable assets in determining how organizations can improve efficiency in the workplace.
Though a background in programming may be required to develop complex modules for electronic medical record systems, the requirement for developing applications using CMSs is not that focused on programming itself but on theme and plugin architecture - specific to a particular CMS - that is needed to modify layout and functionalities. Knowledge in coding would definitely be beneficial since the nurse developer will be able to extend the functionalities to a much greater extent than if the nurse does not have sufficient knowledge in programming. The most important aspect is to collaborate with the information technology or IT department to review the application with regards to security, and compatibility or interoperability with deployed information technology systems.
The security of an application is crucial when designing health-related programs. Whether the application built by the nurse developer was done using programming skills or with the aid of a CMS or an application-building platform, it is imperative that security code review be done, either through manual or automated means. With manual security code review, the nurse developer needs to be knowledgeable in the programming language the application was written since the review would entail browsing through program source code to detect possible vulnerabilities. This is also true with automated code review since results from automated code review would still need manual examination of code snippets to verify whether the result is a false positive or false negative based on the code functionality and security measures taken in place [29].
Data encryption is the process of obscuring plain text data using an encryption algorithm and key to encrypt information, and using the same key to decrypt the cipher text to present the actual data. Sensitive personal information must be encrypted. Thus, the nurse developer must programmatically devise encryption methods to protect healthcare-related data in case of a breach. In the Philippines, Section 28 (Guidelines for Technical Security Measures) sub-section “g” of the Implementing Rules and Regulations of the Data Privacy Act of 2012 states that personal data in storage and in transit must be encrypted [30]. This is a concrete example of administrative and legislative measures in the Association of Southeast Asian Nations (ASEAN) region to protect personal information through data encryption.
An example of a healthcare application that nurses can delve into is undergraduate and graduate health education. A simple web application patterned from a blogging platform can serve as an electronic portfolio where faculty and professors would be able to follow through the student’s progress from his blog entries. This is a basic usage of a CMS, but can have a huge impact in terms of determining student’s understanding of the concepts being taught and skills acquired while in internship or residency, like health assessment, nursing care plans and relevant literature reviews [31,32].
Another area of interest would be personal health records and self-management among patients with chronic conditions, such as diabetes and hypertension. Healthcare applications can be designed by nurses using CMSs that will address monitoring of patient’s blood glucose levels and blood pressure, and the ability to connect with their primary health care physicians or nurse practitioners so the providers can be alerted as well with abnormal fluctuations in glucose or blood pressure levels. However, there is a need to design personal health record systems based on identified and perceived needs, and attitude of individuals. Policies should also be in place to empower individuals so that better quality data can be obtained and improve the overall health literacy [33].
Clinical decision support systems can be integrated in nursing healthcare applications, such as when designing a personal health record system for diabetic patients whose insulin coverage is based on a particular sliding scale set in place by the primary healthcare physician or diabetes specialist. The platform could serve as data repository for blood glucose levels and insulin coverage. The concept of clinical decision support for diabetic patients during office visits has been described [34]. This same paradigm can be applied in a personal health record system where the physician and patient are seen as collaborators in promoting healthcare.
The area of healthcare application development for nurses is broad and an expanding realm, and is only limited by the nurse developer’s imagination. Nurses have problems and concerns in the workplace specific to efficiency in workflow. Nurses have the power to be problem solvers themselves and become nurse developers who can address these needs, using CMSs, as forefront healthcare providers.
5. Conclusion
Nurses are at the frontline of healthcare delivery service. They encounter varying and numerous workflow problems on a daily basis. They can become excellent healthcare innovators to address potential problems in their routine by adopting available and appropriate technology resources. By expanding their skillset into CMSs and information technology development as a whole, nurses have at their disposal a wide array of tools to build modern technological solutions to address difficulties that could affect patient care or nursing workflow. However, with the availability of technological tools, nurse developers should be knowledgeable and responsible on how to properly integrate or implement these advancements into their current information technology systems, in coordination with the information technology department. This collaboration would make sure the health information technology solution uses appropriate technologies to capture needed healthcare information.
Nurse developers can also work independently to build application platforms or software-as-a-service infrastructures to improve the quality of patient care and nursing service. Being an independent creator of health information technology solutions, the use of CMSs would allow rapid application development to achieve a minimum viable product needed to test whether the innovative idea is sound and feasible. CMSss and low or no-code application development platforms are widely available for nurse developers who are interested in developing database-driven applications. However, the nurse developer must still be able to examine the application at the programming code level, particularly during security code review, to show credibility and elicit confidence from users. Nurse developers should be mindful when handling patient or user information by adhering to information technology best practices, such as security code review and data encryption of sensitive personal information - whether in storage or in transit, to protect healthcare data.
Conflicts of interest
None.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2019.09.012.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Kutney-Lee A., Kelly D. The effect of hospital electronic health record adoption on nurse-assessed quality of care and patient safety. J Nurs Adm. 2011 Nov;41(11) doi: 10.1097/NNA.0b013e3182346e4b. 466-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schnipper J.L., Linder J.A., Palchuk M.B., Einbinder J.S., Qi Li, Postilnik A., Middleton B. “Smart Forms” in an electronic medical record: documentation-based clinical decision support to improve disease management. J Am Med Inform Assoc. 2008 Jul;15(4):513–523. doi: 10.1197/jamia.M2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Detmer D, Bloomrosen M, Raymond B, Tang P. Integrated personal health records: transformative tools for consumer-centric care. BMC Med Inf Decis Mak. 2008 Oct 6;8(45) doi: 10.1186/1472-6947-8-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cornell P., Riordan M., Herrin-Griffith D. Transforming nursing workflow, Part 2: the impact of technology on nurse activities. J Nurs Adm: J Nurs Adm. 2010 Oct;40(10):432–439. doi: 10.1097/NNA.0b013e3181f2eb3f. [DOI] [PubMed] [Google Scholar]
- 5.Niazkhani Z., Pirnejad H., Berg M., Aarts J. The impact of computerized provider order entry systems on inpatient clinical workflow: a literature review. J Am Med Inform Assoc. 2009 Jul 1;16(4):539–549. doi: 10.1197/jamia.M2419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Campbell E.M., Guappone K.P., Sittig D.F. Computerized provider order entry adoption: implications for clinical workflow. J Gen Intern Med. 2009 Jan;24(1):21–26. doi: 10.1007/s11606-008-0857-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO) June 2008. Toolkit on monitoring health systems strengthening: health information systems. [Google Scholar]
- 8.Yazdi-Feyzabadi V., Emami M., Mehrolhassani M.H. Health information system in primary health care: the challenges and barriers from local providers’ perspective of an area in Iran. Int J Prev Med. 2015 Jul 6;6:57. doi: 10.4103/2008-7802.160056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carayon P., Cartmill R., Blosky M.A., Brown R., Hackenberg M., Hoonakker P., Hundt A.S., Norfolk E., Wetterneck T.B., Walker J.M. ICU nurses’ acceptance of electronic health records. J Am Med Inform Assoc. 2011 Nov 1;18(6):812–819. doi: 10.1136/amiajnl-2010-000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carrington J.M., Effken J.A. Strengths and limitations of the electronic health record for documenting clinical events. Comput Inf Nurs. 2011 June;29(6):360–367. doi: 10.1097/NCN.0b013e3181fc4139. [DOI] [PubMed] [Google Scholar]
- 11.Khalifa M. Barriers to health information systems and electronic medical records implementation: a field study of Saudi Arabian hospitals. Procedia Comput Sci. 2013;21:335–342. [Google Scholar]
- 12.Househ M., Ahmad A., Alshaikh A., Alsuweed F. Patient safety perspectives: the impact of CPOE on nursing workflow. Stud Health Technol Inform. 2013 Jan 01;183:367–371. [PubMed] [Google Scholar]
- 13.Stevenson J.E., Nilsson G.C., Petersson G.I., Johansson P.E. Nurses’ experience of using electronic patient records in everyday practice in acute/inpatient ward settings: a literature review. Health Inf J. 2010 Mar 1;16(1):63–72. doi: 10.1177/1460458209345901. [DOI] [PubMed] [Google Scholar]
- 14.Vesta Technology & System Ltd [Internet] Hong Kong: vesta technology & system ltd; [cited 2019 sep 15] http://www.vesta-technology.com/electronic-nursing-information-system/ Available from.
- 15.McGonigle D., Mastrian K.G. fourth ed. Jones & Bartlett Learning; Burlington, MA: 2017. Nursing informatics and the foundation of knowledge. [Google Scholar]
- 16.Mansfield J.A., Schuerer D., Burke K. The future role of the registered nurse in patient safety and quality. In: Kelly P., Vottero B., Christie-McAulifee C.A., editors. Introduction to quality and safety education for nurses: core competencies for nursing leadership and management. Springer Publishing Company, LLC; New York, NY: 2018. pp. 467–500. [Google Scholar]
- 17.Yoost B.L., Crawford L.R. Elsevier, Inc; St. Louis, MO: 2016. Fundamentals of nursing: active learning for collaborative practice. [Google Scholar]
- 18.Davies P., Maconochie I. The relationship between body temperature, heart rate and respiratory rate in children. Emerg Med J. 2009 Sep;26(9):641–643. doi: 10.1136/emj.2008.061598. [DOI] [PubMed] [Google Scholar]
- 19.Jensen M.M., Brabrand M. The relationship between body temperature, heart rate and respiratory rate in acute patients at admission to a medical care unit. Scand J Trauma Resusc Emerg Med. 2015;23(Suppl 1):A12. [Google Scholar]
- 20.Staggers N., Clark L., Blaz J.W., Kapsandoy S. Why patient summaries in electronic health records do not provide the cognitive support necessary for nurses’ handoffs on medical and surgical units: insights from interviews and observations. Health Inf J. 2011 Sep 01;17(3):209–223. doi: 10.1177/1460458211405809. [DOI] [PubMed] [Google Scholar]
- 21.Cornell P., Gervis M.T., Yates L., Vardaman J.M. Impact of SBAR on nurse shift reports and staff rounding. Medsurg Nurs. 2014 Sep/Oct;23(5):334–342. [PubMed] [Google Scholar]
- 22.Nelson B.A., Massey R. Implementing an electronic change-of-shift report using Transforming Care at the bedside processes and methods. J Nurs Adm. 2010 April;40(4):162–168. doi: 10.1097/NNA.0b013e3181d40dfc. [DOI] [PubMed] [Google Scholar]
- 23.Collins S.A., Stein D.M., Vawdrey D.K., Stetson P.D., Bakken S. Content overlap in nurse and physician handoff artifacts and the potential role of electronic health records: a systematic review. J Biomed Inform. 2011 August;44(4):704–712. doi: 10.1016/j.jbi.2011.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farooq A., Javed F., Hussain M., Abbas T., Hussain A. Open source content management systems: a canvass. Int J Multidiscip Sci Eng. 2012 Oct;3(10):38–43. [Google Scholar]
- 25.Ang R.J. WordPress as a platform for nursing informatics. Can J Nurs Inf. 2018 Sep 21;13(3) [Google Scholar]
- 26.Timby B.K. ninth ed. Lippincott Williams & Wilkins; Philadelphia, PA: 2009. Fundamental nursing skills and concepts. [Google Scholar]
- 27.Jones K.M.L., Farrington P.A. American Library Association; Chicago, IL: 2013. Learning from libraries that use WordPress: content-management system best practices and case studies. [Google Scholar]
- 28.Cao Xiang, Yu Wenhua. International conference on management and service science. 2010. Using content management system Joomla! to build a website for research institute needs. 2010 Aug 24-26; Wuhan, China. [Google Scholar]
- 29.OWASP Code Review Guide Table of Contents [Internet] Open web application security project (OWASP) https://www.owasp.org/index.php/OWASP_Code_Review_Guide_Table_of_Contents Last modified: 9 September 2010 [cited 2019 Jun 10]. Available from:
- 30.Implementing Rules and Regulations of Republic Act No 10173, known as the “Data Privacy Act of 2012” [Internet] Philippines: national privacy commission, Republic of the Philippines; 2016 aug 24 [cited 2019 jun 10] https://www.privacy.gov.ph/implementing-rules-and-regulations-of-republic-act-no-10173-known-as-the-data-privacy-act-of-2012/ Available from.
- 31.Avila J, Sostmann K, Breckwoldt J, Peters H. Evaluation of the free, open source software WordPress as electronic portfolio system in undergraduate medical education. BMC Med Educ. 2016 Jun 3;16 doi: 10.1186/s12909-016-0678-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sheriff M.R., JU Weerasinghe, Ponnamperuma G. Use of a blog as a tracking tool for student-supervisor interaction in a Biomedical Informatics course: future portfolios. Sri Lanka J Bio Med Inf. 2012;3(3):101–105. [Google Scholar]
- 33.Greenhalgh T, Hinder S, Stramer K, Bratan T, Russell J. Adoption, non-adoption, and abandonment of a personal electronic health record: case study of HealthSpace. BMJ. 2010 Nov 17;341:c5814 doi: 10.1136/bmj.c5814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.O’Connor P.J., Sperl-Hillen J.M., Rush W.A., Johnson P.E., Amundson G.H., Asche S.E., Ekstrom H.L., Gilmer T.P. Impact of electronic health record clinical decision support on diabetes care: a randomized trial. Ann Fam Med. 2011 Jan 1;9(1):12–21. doi: 10.1370/afm.1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.