Abstract
Objectives
Several recent large-scale studies have indicated a prospective association between job strain and coronary heart disease, stroke and diabetes. Job strain is also associated with poorer mental health, a risk factor for cardiometabolic disease. This study investigates the prospective relationships between change in job strain, poor mental health and cardiometabolic disease, and whether poor mental health is a potential mediator of the relationship between job strain and cardiometabolic disease.
Methods
We used data from five cohort studies from Australia, Finland, Sweden and UK, including 47 757 men and women. Data on job strain across two measurements 1–5 years apart (time 1 (T1)–time 2 (T2)) were used to define increase or decrease in job strain. Poor mental health (symptoms in the top 25% of the distribution of the scales) at T2 was considered a potential mediator in relation to incident cardiometabolic disease, including cardiovascular disease and diabetes, following T2 for a mean of 5–18 years.
Results
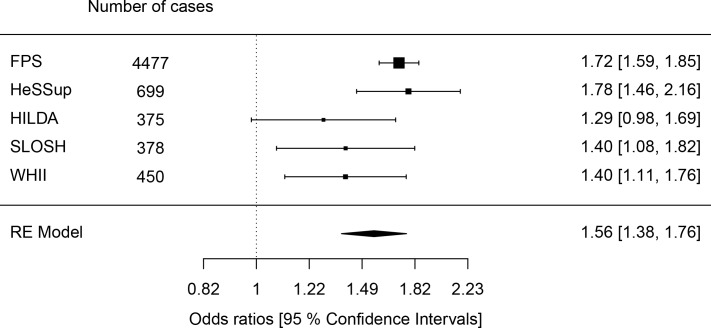
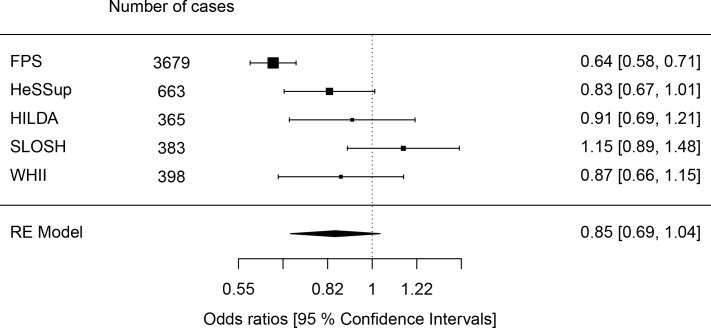
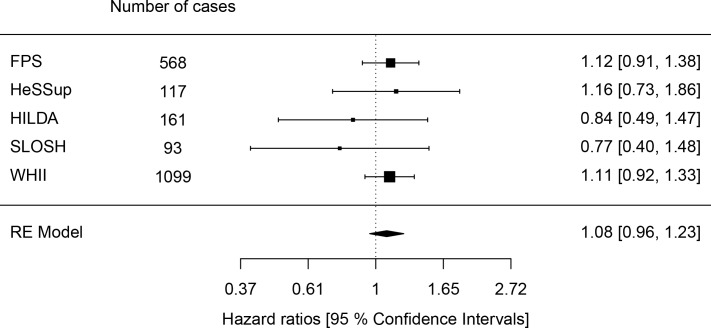
An increase in job strain was associated with poor mental health (HR 1.56, 95% CI 1.38 to 1.76), and a decrease in job strain was associated with lower risk in women (HR 0.70, 95% CI 0.60–0.84). However, no clear association was observed between poor mental health and incident cardiometabolic disease (HR 1.08, 95% CI 0.96–1.23), nor between increase (HR 1.01, 95% CI 0.90–1.14) and decrease (HR 1.08, 95% CI 0.96–1.22) in job strain and cardiometabolic disease.
Conclusions
The results did not support that change in job strain is a risk factor for cardiometabolic disease and yielded no support for poor mental health as a mediator.
Keywords: mental health, cardiovascular, diabetes mellitus, stress, meta-analysis
Key messages.
What is already known about this subject?
Job strain (a combination of high demands and low control at work) has been found a risk factor for both poor mental health and cardiometabolic disease, including cardiovascular disease and diabetes.
Poor mental health also appears to be a risk factor for cardiometabolic disease.
However, whether poor mental health is a mediator in the pathway from job strain to cardiometabolic disease has not been tested longitudinally.
What are the new findings?
This study showed that an increase in job strain is associated with risk of poor mental health supporting a temporal precedence of job strain and a causal association.
However, no clear associations were observed between change in job strain and cardiometabolic disease, or between poor mental health and cardiometabolic disease.
Hence, the study yielded no support for poor mental health as a mediator in the relationship between job strain and cardiometabolic disease.
How might this impact on policy or clinical practice in the foreseeable future?
The findings suggest that interventions targeting mental health may not be an effective alternative to preventing any effects of job strain on cardiometabolic disease, but support continued policy and practice targeting the psychosocial work environment for mental health promotion.
Introduction
Work-related stress, one of the major contemporary challenges, can be defined in different ways influenced by different theoretical perspectives. Job strain, which refers to a combination of high demands and low control at work according to the job–demand–control model,1 is one of the most commonly studied indicators of work stress. Several recent large-scale studies have indicated that job strain is associated with a moderately elevated risk of coronary heart disease (CHD)2 and stroke.3 Job strain also appears to be a risk factor for type 2 diabetes,4 but not, for example, cancer,5 asthma6 or chronic obstructive lung disease,7 suggesting that job strain may have some specificity with regard to cardiometabolic disease.8
Meta-analyses suggest that job strain is also associated with poorer mental health, particularly depression.9 10 Poor mental health, especially depression, is also associated with a range of cardiometabolic disorders.11 The relationship between depression and cardiometabolic disease may be bidirectional,12 but some studies suggest that depression is a stronger risk factor, for example, for diabetes than diabetes is for depression.13 14
There are a number of possible pathways through which works stress may be linked to cardiometabolic disease, including psychological health. However, very little is still known about this plausible mediating mechanism.8 15
The objective of the present study was to assess whether, and to what extent, poor mental health is an intermediate variable in the relationship between job strain and cardiometabolic disease (cardiovascular disease (CVD) and diabetes), focusing on change in job strain using repeated measures from several cohort studies mimicking an intervention setting.
Methods
Design and material
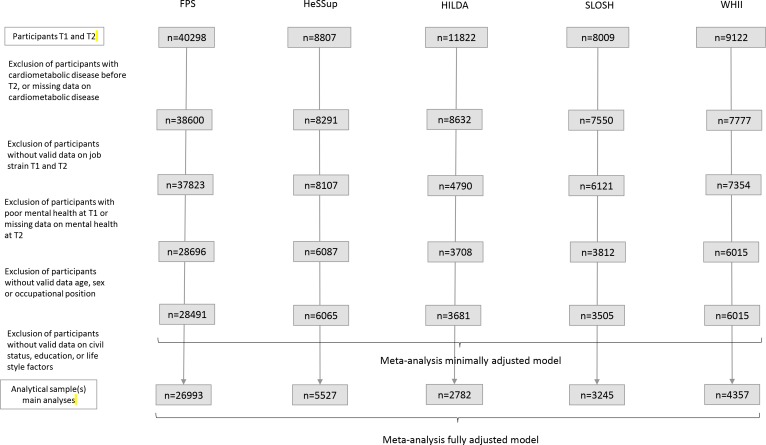
We used data from five large well-characterised occupational cohorts: the Finnish Public Sector (FPS) study, the Health and Social Support (HeSSup) study from Finland, the Household, Income and Labour Dynamics in Australia (HILDA) study, the Swedish Longitudinal Occupational Survey of Health (SLOSH) study and the Whitehall II (WHII) study from UK. The cohort studies are further described in the Appendix. All studies have repeatedly collected self-reported questionnaire data, which have been complemented with data from administrative sources. We retrieved baseline (time 1 (T1)) data of job demands and control and from a second time point (time 2 (T2)) from all studies, 1–5 years later depending on the cohort, to study change in job strain. The potential mediator, poor mental health, was assessed at T2 and new-onset cardiometabolic disease (CVD or diabetes) after T2 (with follow-up on average 5–18 years). The design is illustrated in online supplementary figure 1. For the analyses, individuals with CVD or diabetes up to T2 were excluded, people with poor mental health T1, as well as self-employed individuals and those with missing data on exposure, mediator or covariates, yielding a total study sample of 47 757 individuals for analyses (see more figure 1).
Figure 1.
A flowchart describing the selection of study subjects for the main analyses based on minimally or fully adjusted models. FPS, Finnish Public Sector; HeSSUP, Health and Social Support; HILDA, Household, Income and Labour Dynamics in Australia; SLOSH, Swedish Longitudinal Occupational Survey of Health; T1, time 1; T2, time 2; WHII, Whitehall II.
oemed-2018-105595supp001.pdf (440.8KB, pdf)
Job strain
Data on job demands and control were assessed at T1 and T2. The complete demand and control scales based on the job demand–control model were used in SLOSH (based on the Demand–Control Questionnaire), while partial scales were used in FPS, HeSSup (based on the Job Content Questionnaire) and WHII (based on the Demand–Control Questionnaire).16 The included partial scales have been shown to have a high correlation with the complete scales.16 In HILDA, similar scales for demands (based on 4 items) and control (based on 11 items) were used. First, job strain was defined using the subtraction approach (difference between demands and control) at T1 and T2.17 Second, to identify changes greater than the mimimal detectable change, we calculated a relative change index, considering the difference between T1 and T2 job strain scores, and the SD of the measure at baseline and reliability of the measure.18 19 The reliability was assumed to be 0.90 (the test–retest correlation for control observed in WHII).18 Finally, we divided the participants into three categories with (1) increasing job strain (relative change index of 1.96 or higher), (2) decreasing job strain (reliable change index −1.96 or lower) and (3) no change in job strain (reliable change index >−1.96 and <1.96, used as reference).18
Poor mental health
Symptoms of poor mental health were assessed by the participant-completed questionnaires at T1 and T2. The General Health Questionnaire (GHQ) was used in FPS and WHII.20 Beck Depression Inventory (BDI) was used in HeSSup.21 Both GHQ and BDI have been found useful for detecting depressive disorders in the general population.22 In HILDA, the Mental Health Inventory-5 was used, a five-item subscale of the general health measure 36-Item Short Form Survey,23 which has been found psychometrically comparable to GHQ-12.24 In SLOSH, a brief subscale of the Symptom Checklist-90 (SCL-90) was employed (labelled the six item Symptom Checklist-Core Depression Scale (SCL-CD6)).25 The SCL-90 has also been found to have properties similar to those of the GHQ-12 for psychiatric screening.26 The composite scale scores were dichotomised in accordance with previous research, categorising people above the top 25% of the distribution in each study as having poor mental health.27 This definition of poor mental health was used for comparability between studies.
Cardiometabolic disease
As an outcome variable, we focused on incident cardiometabolic diseases, including CVD (comprising CHD and cerebrovascular disease) and diabetes, from self-reported or administrative data sources following T2 to end of study (which varied between the cohorts). Any main diagnosis in hospital registers coded I20.0, I20.1 or I21-25 in the International Classification of Disease (ICD)-10 or 410–414 in ICD-9 or ICD-8, or any main cause of death coded I20-25 in ICD-10 or 410–414 in ICD-9 were used to indicate CHD. The corresponding codes for cerebrovascular disease were I60-69 (ICD-10), and 430–438 (ICD-8 and ICD-9). In HILDA, where no administrative data were available, we used self-reported doctor-diagnosed heart disease or circulatory disease. Diabetes was ascertained from hospital and death records (a main or side diagnoses of E11 in ICD-10, or 250 in ICD-8 and ICD9), from medication, and/or from self-reports or glucose intolerance test. In FPS, HeSSup and SLOSH, a combination of data from hospital/death registers, drug registers (any prescriptimetabolon record of A10X, A10A and A10B according to the Anatomical Classification System) and self-reports were used. In WHII, a combination of self-reports and glucose intolerance test was used, while only self-reported information was available in HILDA.
Covariates
A directed acyclic graph was construed to aid in the selection of confounders to include in the models (see online supplementary figure 1). All studies included information on possible confounders such as sex, age, civil status, socioeconomic status (SES) and/or education, lifestyle factors, and certain chronic disorders. Two groups of civil status were used: married/cohabiting and single. SES was categorised into low, intermediate and high based on occupational position according to employer records (FPS), self-reported job titles (SLOSH and HILDA) or civil service employment grade (WHII).28 Manual workers such as labourers and elementary and service workers were regarded as having low SES, while those with advanced or intermediate occupations, such as clericals and sales, were classified with intermediate SES, and professionals and managers were regarded as having high SES. In HeSSup occupational position was based on educational level. In all other studies, educational level was further categorised into three groups corresponding to primary, secondary and postsecondary education based on self-reports. The lifestyle factors included obesity (body mass index of 30 or more according the WHO recommendations), physical inactivity, risky alcohol drinking (high vs low weekly consumption) and current smoking (yes or no) from the participant-completed questionnaires. These factors were largely defined according to previous studies, in which 21 units or more (women) or 28 units or more of weekly alcohol consumption were defined as high alcohol consumption, and very little, moderate or vigorous, or no physical leisure time activity or exercise was defined as physical inactivity.29 30 In SLOSH, consuming six or more drinks per occasion was additionally considered as risky drinking. These factors measured at T1 were considered confounders, while lifestyle factors measured at T2 were regarded as possible mediators and were left out of the analyses. Data on other diseases, including musculoskeletal problems, chronic obstructive pulmonary disease and cancer at T1, ascertained from administrative sources, were also considered but were not used in the final analyses due to large heterogeneity in measurements between studies.
Data analyses
To assess the potential mediating role of poor mental health, we first estimated the association between increase and decrease in job strain and poor mental health with logistic regression and then between poor mental health and incident cardiometabolic disease using Cox proportional hazard regression. We also assessed the association between increase or decrease in job strain and cardiometabolic disease using Cox regression. Second, we performed causal mediation analyses, using a mediation macro developed by Valeri and Vanderweele31 based on the counterfactual framework. The macro calculates the total effect and the natural and indirect effects. The natural direct effect is the contrast between the counterfactual outcome if the individuals were exposed (experienced change in job strain) and the counterfactual outcome if the same individuals were unexposed (experienced no change in job strain), with the mediator assuming whatever value it would have taken when unexposed. The natural indirect effects are the contrast, given exposure, between the counterfactual outcome if the mediator assumed whatever value it would have taken when exposed and the counterfactual outcome if the mediator assumed whatever value it would have taken when unexposed.32 For the mediator, a logistic regression was specified, and for the outcome, a Cox proportional hazard models was applied. The follow-up time for cardiometabolic diseases started from T2 and ended at the time of event, death, end of study or last time of information available on cardiometabolic disease, whichever came first. We first fitted minimally adjusted models, including age, sex and occupational position, followed by additional adjustment for education (except in HeSSup), civil status and health behaviours, including smoking, risky drinking and physical inactivity, as well as obesity (fully adjusted model). In sensitivity analyses, we included those with poor mental health at baseline and adjusted for poor mental health at baseline in the models. We also assessed if the results were influenced by the length of follow-up for incident cardiometabolic disease using data from the WHII study and stratified for sex. The analyses were first conducted separately for all cohorts then pooled using meta-analytic techniques using the metafor package in R.33 Since the different studies were not equal in terms of method and characteristics, random effects meta-analyses was preferred, which assumed different true effects across cohorts.
Results
Of the 47 757 individuals with valid data on cardiometabolic disease (contributing with 395 453 person-years at risk), about 14%–18% experienced increase in job strain, while 15%–20% experienced a decrease in job strain.
Some characteristics of the samples from the respective cohorts are presented in table 1. The distribution of most sociodemographic characteristics was relatively similar across the study samples. At baseline (T1), the mean age of the participants ranged between 44 and 49. However, the proportion of women differed between the studies, with a high proportion in FPS and a low proportion in WHII. A higher proportion of the HILDA participants had high SES position compared with the other cohorts. Moreover, a lower proportion reported risky alcohol consumption in the SLOSH study.
Table 1.
Characteristics of the samples by cohort
| FPS | HeSSup | HILDA | SLOSH | WHII | Mean or proportion pooled across cohorts | |
| Eligible for analyses on cardiometabolic disease | 28 491 | 6065 | 3681 | 3505 | 6015 | |
| Person-years (mean follow-up time in years) | 191 829.9 (6.7) | 54 315.4 (9.0) | 23 636.0 (6.4) | 17 766.5 (5.1) | 107 904.7 (17.9) | 7.3* |
| Number of cases (rate per 1000 person-years) | 616 (3.2) | 122 (2.3) | 161 (6.8) | 108 (6.1) | 1512 (14.0) | |
| Number (%) of participants experiencing increase in job strain, T1–T2 | 5015 (18) | 839 (14) | 520 (14) | 544 (16) | 1087 (18) | 16† |
| Number (%) of participants experiencing no major change in job strain, T1–T2 | 19 295 (68) | 4020 (66) | 2552 (69) | 2249 (64) | 3973 (66) | 67† |
| Number (%) of participants experiencing decrease in job strain, T1–T2 | 4181 (15) | 1206 (20) | 609 (17) | 712 (20) | 955 (16) | 17† |
| Number (%) of participants with poor mental health | 5245 (18) | 915 (15) | 445 (12) | 515 (15) | 740 (12) | 14† |
| Number of women (%) | 23 032 (81) | 3437 (57) | 1765 (48) | 1919 (55) | 1801 (30) | 55† |
| Mean age, T1 (SD) | 47.1 (8.6) | 44.3 (9.4) | 40.0 (12.8) | 49.2 (9.5) | 44.8 (6.0) | 45.4 |
| Number (%) of participants according to socioeconomic status, T1 | ||||||
| Low | 5121 (18) | 2487 (41) | 923 (25) | 1116 (32) | 1985 (33) | 29† |
| Intermediate | 15 454 (54) | 2235 (37) | 993 (27) | 1630 (47) | 2941 (49) | 42† |
| High | 7916 (28) | 1343 (22) | 1765 (48) | 759 (22) | 1089 (18) | 27† |
| Number (%) of participants with obesity, T1‡ | 2780 (10) | 474 (8) | 674 (18) | 343 (10) | 374 (6) | 10† |
| Number (%) of participants with physical inactivity, T1‡ | 4831 (17) | 1045 (17) | 702 (19) | 571 (16) | 1437 (25) | 19† |
| Number (%) of participants with high alcohol consumption, T1‡ | 3557 (13) | 782 (13) | 389 (14) | 142 (4) | 914 (15) | 11† |
| Number (%) of participants smoking, T1‡ | 4712 (17) | 1211 (22) | 711 (19) | 465 (13) | 915 (15) | 17† |
*Test for heterogeneity showed p<0.001.
†The proportions were pooled through meta-analyses using metaphor with logit transformation to increase the probability of a normal distribution suitable for estimation of summary proportions. Tests for heterogeneity showed p<0.001.
‡Missing values: obesity (FPS n=569, HeSSup n=27, HILDA n=0, SLOSH n=41 and WHII n=8), physical inactivity (FPS n=263, HeSSup n=26, HILDA n=1, SLOSH n=12 and WHII n=183), alcohol consumption (FPS n=65, HeSSup n=1, HILDA n=897, SLOSH n=235 and WHII n=50) and smoking (FPS n=604, HeSSup n=490, HILDA n=5, SLOSH n=7 and WHII n=5).
FPS, Finnish Public Sector; HILDA, Household, Income and Labour Dynamics in Australia; HeSSUP, Health and Social Support; SLOSH, Swedish Longitudinal Occupational Survey of Health; T1, time 1; T2, time 2; WHII, Whitehall II.
Relationship between job strain and poor mental health
Logistic regression analyses indicated that an increase in job strain between T1 and T2 was associated with higher risk of poor mental health at T2. The pooled OR across cohorts was 1.56, with a 95% CI of 1.38 to 1.76 (figure 2) when adjusting for sex, age, occupational position, civil status, education and lifestyle factors. A decrease in job strain tended to be associated with a lower risk of poor mental health (OR 0.85, 95% CI 0.69 to 1.04; see figure 3). The heterogeneity was modest with regard to increase in job strain (I2 53%) but high for decrease in job strain (I2 78%). These associations were found in most cohorts, and the estimates were similar in models adjusting only for sex, age and occupational position (online supplementary figure 2-3). Similar estimates were also obtained in sensitivity analyses alternatively adjusting for poor mental health at baseline (online supplementary figure 4-5). The association between increase in job strain and poor mental health was similar among men and women (online supplementary figure 6-7), but differed slightly between men and women experiencing a decrease in job strain. The results indicated that job strain was associated with a lower risk of poor mental health among women (online supplementary figure 8-9).
Figure 2.
Results from logistic regression analyses assessing the relationship between increase in job strain between T1 and T2 and poor mental health T2, adjusting for sex, age, occupational position, civil status, education, obesity, physical inactivity, risky drinking, smoking, and poor mental health. FPS=the Finnish Public Sector Study, HeSSup=the Health and Social Support study, HILDA=the Household, Income and Labour Dynamics in Australia, SLOSH=the Swedish Longitudinal Occupational Survey of Health, WHII=the Whitehall II study, RE=random effect (pooled estimate across cohorts). FPS, Finnish Public Sector; HeSSUP, Health and Social Support; HILDA, Household, Income and Labour Dynamics in Australia; SLOSH, Swedish Longitudinal Occupational Survey of Health; WHII, Whitehall II; RE, random effect.
Figure 3.
Results from logistic regression analyses assessing the relationship between decrease in job strain between T1 and T2 and poor mental health T2, adjusting for sex, age, occupational position, civil status, education, obesity, physical inactivity, risky drinking, smoking, and poor mental health. FPS=the Finnish Public Sector Study, HeSSup=the Health and Social Support study, HILDA=the Household, Income and Labour Dynamics in Australia, SLOSH=the Swedish Longitudinal Occupational Survey of Health, WHII=the Whitehall II study, RE=random effect (pooled estimate across cohorts) . FPS, Finnish Public Sector; HeSSUP, Health and Social Support; HILDA, Household, Income and Labour Dynamics in Australia; SLOSH, Swedish Longitudinal Occupational Survey of Health; WHII, Whitehall II; RE, random effect.
Relationship between poor mental health and cardiometabolic disease
Cox regression analyses indicated a weak association between poor mental health and incident CVD, but the pooled risk estimate was not statistically significant. The pooled minimally adjusted HR across cohorts was 1.10 (95% CI 0.98 to 1.23; see online Supplementary figure 10), and the fully adjusted risk estimate remained similar (HR 1.08, 95% CI 0.96 to 1.23; figure 4). None of the cohort-specific estimates were statistically significant in the separate analyses. There was no heterogeneity between studies (I2 0%) and no major differences between men and women (online supplementary figure 11-12). Similar estimates were also obtained in sensitivity analyses alternatively adjusting for poor mental health at baseline (online supplementary figure 13). A shorter follow-up time in the WHII study, until phase 5 instead of phase 9, also yielded similar results although slightly weaker risk estimate (data not shown).
Figure 4.
Results from Cox regression analyses assessing relationship between poor mental health T2 and incident cardiometabolic disease, adjusting for sex, age, occupational position, civil status, education, obesity, physical inactivity, risky drinking, smoking, as well as job strain FPS=the Finnish Public Sector Study, HeSSup=the Health and Social Support study, HILDA=the Household, Income and Labour Dynamics in Australia, SLOSH=the Swedish Longitudinal Occupational Survey of Health, WHII=the Whitehall II study, RE=random effect (pooled estimate across cohorts). FPS, Finnish Public Sector; HeSSUP, Health and Social Support; HILDA, Household, Income and Labour Dynamics in Australia; SLOSH, Swedish Longitudinal Occupational Survey of Health; WHII, Whitehall II; RE, random effect.
Relationship between job strain and cardiometabolic disease and the role of poor mental health as potential mediator
Finally, the analyses showed no clear total effect of increase in job strain on cardiometabolic disease (online supplementary figure 14), and no heterogeneity between cohorts was noted (I2 0%). The pooled HR was 1.01 (95% CI 0.90 to 1.14). Although no heterogeneity was observed, there was a statistically significant association between increase in job strain and cardiometabolic disease in the SLOSH data (HR 1.78, 95% CI 1.06 to 3.00). The results were relatively similar in minimally adjusted models (data not shown) and in sensitivity analyses including people with prior poor mental health alternatively adjusting for baseline mental health (online supplementary figure 15), but showing a weaker HR in SLOSH. The results were also supported in the causal mediation analyses (online supplementary table 1).
No association with cardiometabolic disease was observed in corresponding analyses of decrease in job strain (HR 1.08, 95% CI 0.96 to 1.22; online supplementary figure 16-17). Moreover, no differences between men and women were observed in analyses of increase and decrease in job strain in relation to cardiometabolic disease. A shorter follow-up time in the WHII study, until phase 5 instead of phase 9, also yielded similar results although slightly weaker risk estimate (data not shown).
Discussion
The results of the present study indicated that an increase in job strain was especially associated with poor mental health. Poor mental health, however, was not clearly associated with later cardiometabolic disease, and no significant association was observed between increase or decrease in job strain and cardiometabolic disease, indicating that they key criteria for mediation were not fulfilled.
Although previous work has suggested a prospective relationship between job strain and depressive symptoms and clinical depression,9 34 few earlier studies have examined change in job strain in relation to depression/depressive symptoms. The results of the present study are in line with results from several of the earlier studies examining change in job strain over time, for example, with those of Burns et al 35, who showed that moving into strain was associated with mental health, and those of Wang et al indicating an increased risk of major depression.36 Wang et al also noted a lower risk of major depression among people going from high strain to low strain, comparable with that of people with repeated low strain, which is in keeping with our findings. Together these studies strengthen the plausibility of a causal relation between job strain and poor mental health by indicating that a change in job strain may be followed by a change in mental health.
However, with regard to mental health and cardiometabolic disease, our results showed only weak excess risk estimates for cardiometabolic disease that did not reach statistical significance. This is contrary to some of the previous literature suggesting that depression or poor mental health more generally increases the risk of CVD and diabetes.12–14 A recent study, on the other hand, indicated that the association between psychological distress and ischaemic heart disease was largely due to confounding by health behaviours and functional limitations and argued that reverse causality may explain a significant proportion of the association.37 In this study, reverse causality is unlikely, when it comes to mental health and cardiometabolic disease, since cardiometabolic disease was only assessed after the measurement of mental health. This may be an explanation for the weak associations. The exclusion of poor mental health at T1 may also play a role. More work may be needed to determine the role of poor mental health as a risk factor for cardiometabolic disease. In contrast with some earlier work, we also observed no clear overall relationship between increase/decrease in job strain and CVD or diabetes.2–4 However, findings about whether job strain causes CVD have been partly inconsistent.15 One review noted an increased risk only among studies with a long follow-up (10 years or more), and it is possible that the follow-up time was too short in some of the cohorts included in this study to detect an association. Moreover, compared with many previous studies in the field, we focused on change in job strain, and the results are therefore not directly comparable with many earlier studies. In the present study, we applied a design based on repeated measures that may better account for intraindividual variation, reduce bias due to regression to the mean and elucidate the temporal order with regard to relief of job strain and poor mental health.38 It should be noted though that repeated exposure to job strain was thereby not considered, although it may be associated with an increased risk 0f cardiometabolic disease and may explain the lack of relationship with cardiometabolic disease in this study. To our knowledge, this is also the first longitudinal study to examine the entire pathway from job strain to cardiometabolic disease through some indicator of mental health. The lack of clear association between job strain and cardiometabolic disease and between poor mental health and cardiometabolic disease, however, did not give support to the mediating role of poor mental health in the present study.
Apart from using repeated measures, other strengths of the present study include the prospective design and the large sample of individuals. This allowed us to examine the prospective association between job strain and cardiometabolic disease and the potential pathway through poor mental health with sufficient power. We also used a combination of self-reported and register data, which is a strength, as self-reports may give rise to bias due to common method variance. Common method bias may, however, be an issue influencing the results of associations between job strain and mental health. The dropout due to missing data on covariates was generally limited, hence imputation was not considered.
There are also some other limitations of the study that should be acknowledged. The included cohorts differed to some extent with regard to study population, measurements, time lag between measurements and follow-up. While some studies included only public sector employees, other cohorts were more representative of the total working populations. Furthermore, the measurement of the mediator especially differed between several cohorts, with some scales specifically assessing depressive symptoms and others assessing more general distress, which may explain some of the heterogeneity in results. Only more considerable changes were considered as an increase or increase in job strain, while those with small changes in job strain scores were considered unchanged. Potential misclassification of exposure could lead to a dilution of the risk estimates. The reference group moreover included people with stable/recurrent job strain, which may not be the optimal comparison. Moreover, the results mimic an intervention, provided the assumption of consistency is met (meaning that there are no different versions of the exposure that are differently associated with the potential outcome). We also used a slightly wider definition for CVDs than in previous studies2 4 to increase the power for the analyses. This has some potential drawbacks. Job strain and mental health, for example, are not necessarily associated with all the included diagnostic codes, such as haemorrhagic stroke diluting the main association. With regard to confounding, health behaviours may be another main pathway through which job strain may influence cardiometabolic disease. Possible confounding by time-varying health behaviours is difficult to rule out. However, we were able to control for health behaviours at baseline, which generally did not affect the results considerably. Possibly important unmeasured factors such as childhood factors, life events, diet and biological factors were, however, not available and may have contributed to residual confounding. It is possible that time stable characteristics, such as genetics and personality, partly account for the job strain–mental health relationship,39 40 and reverse causation cannot be ruled out. Future studies on the role of mental health may hence be needed to confirm or refute our findings.
In conclusion, this study gave no clear support for a prospective association between poor mental health and cardiometabolic disease and between change in job strain and cardiometabolic disease, and hence yielded no support for poor mental health as a mediator.
Acknowledgments
We thank all participants in the Finnish Public Sector (FPS), Health and Social Support (HeSSUP), Household, Income and Labour Dynamics in Australia (HILDA), Swedish Longitudinal Occupational Survey of Health (SLOSH) and Whitehall II (WHII) study. We would also thank Statistics Sweden for carrying out the data collection, data managers of the SLOSH study, WHII researchers and support staff for making the study possible. We thank the Finnish Work Environment fund for supporting FPS, the Academy of Finland for supporting HeSSup, the Australian Government Department of Social Services for supporting HILDA and the Swedish Research Council for Health, Working Life and Welfare, as well as the Swedish Research Council, for supporting SLOSH. Finally, we thank the UK Medical Research Council (MR/K013351/1 and G0902037), the British Heart Foundation (RG/13/2/30098) and the US National Institutes of Health (R01HL36310 and R01AG013196), which supported the collection of data in the WHII Study.
Footnotes
Contributors: All authors contributed to the conception and design of the study, interpretation of data and critical revision of the manuscript for important intellectual content; gave approval of the version to be published; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. LMH, JV, SS, MK and HW contributed to data acquisition, and LMH and JP contributed to the analysis of data for the work. LMH drafted the paper. JP had full access to data from FPS and HeSSup. LMH had full access to individual participant data from HILDA, SLOSH and WHII and takes responsibility for the integrity of the unpublished data and the accuracy of the data analysis.
Funding: The study was financially supported by the NordForsk, the Nordic Programme on Health and Welfare (grant number 75021). MK was also supported by the Medical Research Council (K013351). The funders had no role in the design or in the collection, analysis, interpretation of data, writing of the report or decision to submit the article for publication. This paper uses unit record data from the Household, Income and Labour Dynamics in Australia (HILDA) Survey. The HILDA Project is initiated and funded by the Australian Government Department of Social Services (DSS) and is managed by the Melbourne Institute of Applied Economic and Social Research (Melbourne Institute). The findings and views reported in this paper, however, are those of the authors and should not be attributed to either DSS or the Melbourne Institute.
Competing interests: None.
Patient consent for publication: Not required.
Ethics approval: Ethical approval was given for each cohort in each country from relevant ethical committees/boards. The Finnish Public Sector study was approved by the ethics committee of the Finnish Institute of Occupational Health (60/13/03/00/2011), and Health and Social Support study was approved by the concurrent joint ethics committee of the University of Turku and the Turku University Central Hospital. The Household, Income and Labour Dynamics in Australia study was approved by both the human research ethics committee of University of Melbourne and the ethics committee of the Australian Institute of Health and Welfare. The Swedish Longitudinal Occupational Survey of Health was approved by the Regional Research Ethics Board in Stockholm (2006/158-31, 2008/240-32, 2008/1808-32, 2010/0145-32, 2012/373-31/5, 2013/2173-32 and 2015/2187-32). The Whitehall II study was approved by the University College London Medical School committee on the ethics of human research. Informed consent was obtained for all participants.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available.
References
- 1. Karasek R, Theorell T. Healthy work: stress, productivity, and the reconstruction of working life. New York: Basic Books, 1990. [Google Scholar]
- 2. Kivimäki M, Nyberg ST, Batty GD, et al. Job strain as a risk factor for coronary heart disease: a collaborative meta-analysis of individual participant data. Lancet 2012;380:1491–7. 10.1016/S0140-6736(12)60994-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fransson EI, Nyberg ST, Heikkilä K, et al. Job strain and the risk of stroke: an individual-participant data meta-analysis. Stroke 2015;46:557–9. 10.1161/STROKEAHA.114.008019 [DOI] [PubMed] [Google Scholar]
- 4. Nyberg ST, Fransson EI, Heikkilä K, et al. Job strain as a risk factor for type 2 diabetes: a pooled analysis of 124,808 men and women. Diabetes Care 2014;37:2268–75. 10.2337/dc13-2936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Heikkilä K, Nyberg ST, Theorell T, et al. Work stress and risk of cancer: meta-analysis of 5700 incident cancer events in 116,000 European men and women. BMJ 2013;346:f165 10.1136/bmj.f165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Heikkilä K, Madsen IEH, Nyberg ST, et al. Job strain and the risk of severe asthma exacerbations: a meta-analysis of individual-participant data from 100 000 European men and women. Allergy 2014;69:775–83. 10.1111/all.12381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Heikkilä K, Madsen IEH, Nyberg ST, et al. Job strain and COPD exacerbations: an individual-participant meta-analysis. Eur Respir J 2014;44:247–51. 10.1183/09031936.00205113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kivimäki M, Kawachi I. Work stress as a risk factor for cardiovascular disease. Curr Cardiol Rep 2015;17:630 10.1007/s11886-015-0630-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Theorell T, Hammarström A, Aronsson G, et al. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health 2015;15:738 10.1186/s12889-015-1954-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Netterstrøm B, Conrad N, Bech P, et al. The relation between work-related psychosocial factors and the development of depression. Epidemiol Rev 2008;30:118–32. 10.1093/epirev/mxn004 [DOI] [PubMed] [Google Scholar]
- 11. Scott KM. Depression, anxiety and incident cardiometabolic diseases. Curr Opin Psychiatry 2014;27:289–93. 10.1097/YCO.0000000000000067 [DOI] [PubMed] [Google Scholar]
- 12. Whooley MA, Wong JM. Depression and cardiovascular disorders. Annu Rev Clin Psychol 2013;9:327–54. 10.1146/annurev-clinpsy-050212-185526 [DOI] [PubMed] [Google Scholar]
- 13. Mezuk B, Eaton WW, Albrecht S, et al. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care 2008;31:2383–90. 10.2337/dc08-0985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hasan SS, Mamun AA, Clavarino AM, et al. Incidence and risk of depression associated with diabetes in adults: evidence from longitudinal studies. Community Ment Health J 2015;51:204–10. 10.1007/s10597-014-9744-5 [DOI] [PubMed] [Google Scholar]
- 15. Sara JD, Prasad M, Eleid MF, et al. Association between Work‐Related stress and coronary heart disease: a review of prospective studies through the job strain, Effort‐Reward balance, and organizational justice models. J Am Heart Assoc 2018;7:e008073 10.1161/JAHA.117.008073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Fransson EI, Nyberg ST, Heikkilä K, et al. Comparison of alternative versions of the job demand-control scales in 17 European cohort studies: the IPD-Work Consortium. BMC Public Health 2012;12:62 10.1186/1471-2458-12-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Courvoisier DS, Perneger TV. Validation of alternative formulations of job strain. J Occup Health 2010;52:5–13. 10.1539/joh.L9084 [DOI] [PubMed] [Google Scholar]
- 18. Smith P, Beaton D. Measuring change in psychosocial working conditions: methodological issues to consider when data are collected at baseline and one follow-up time point. Occup Environ Med 2008;65:288–96. quiz 95-6 10.1136/oem.2006.032144 [DOI] [PubMed] [Google Scholar]
- 19. Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol 1991;59:12–19. 10.1037/0022-006X.59.1.12 [DOI] [PubMed] [Google Scholar]
- 20. Goldberg DP, Blackwell B. Psychiatric illness in general practice. A detailed study using a new method of case identification. Br Med J 1970;1:439–43. 10.1136/bmj.2.5707.439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561–71. 10.1001/archpsyc.1961.01710120031004 [DOI] [PubMed] [Google Scholar]
- 22. Aalto A-M, Elovainio M, Kivimäki M, et al. The Beck depression inventory and general health questionnaire as measures of depression in the general population: a validation study using the composite international diagnostic interview as the gold standard. Psychiatry Res 2012;197:163–71. 10.1016/j.psychres.2011.09.008 [DOI] [PubMed] [Google Scholar]
- 23. Ware JE, Snow KK, Kosinski M, et al. SF-36® health survey manual and interpretation guide. Boston: New England Medical Center, The Health Institute, 1993. [Google Scholar]
- 24. McCabe CJ, Thomas KJ, Brazier JE, et al. Measuring the mental health status of a population: a comparison of the GHQ-12 and the SF-36 (MHI-5). Br J Psychiatry 1996;169:517–21. 10.1192/bjp.169.4.516 [DOI] [PubMed] [Google Scholar]
- 25. Magnusson Hanson LL, Westerlund H, Leineweber C, et al. The symptom Checklist-core depression (SCL-CD6) scale: psychometric properties of a brief six item scale for the assessment of depression. Scand J Public Health 2014;42:82–8. 10.1177/1403494813500591 [DOI] [PubMed] [Google Scholar]
- 26. Holi MM, Marttunen M, Aalberg V. Comparison of the GHQ-36, the GHQ-12 and the SCL-90 as psychiatric screening instruments in the Finnish population. Nord J Psychiatry 2003;57:233–8. 10.1080/08039480310001418 [DOI] [PubMed] [Google Scholar]
- 27. Wittchen H-U, Jacobi F. Size and burden of mental disorders in Europe--a critical review and appraisal of 27 studies. Eur Neuropsychopharmacol 2005;15:357–76. 10.1016/j.euroneuro.2005.04.012 [DOI] [PubMed] [Google Scholar]
- 28. Marmot MG, Smith GD, Stansfeld S, et al. Health inequalities among British civil servants: the Whitehall II study. Lancet 1991;337:1387–93. 10.1016/0140-6736(91)93068-K [DOI] [PubMed] [Google Scholar]
- 29. Fransson EI, Heikkilä K, Nyberg ST, et al. Job strain as a risk factor for leisure-time physical inactivity: an individual-participant meta-analysis of up to 170,000 men and women: the IPD-Work Consortium. Am J Epidemiol 2012;176:1078–89. 10.1093/aje/kws336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kivimäki M, Nyberg ST, Fransson EI, et al. Associations of job strain and lifestyle risk factors with risk of coronary artery disease: a meta-analysis of individual participant data. CMAJ 2013;185:763–9. 10.1503/cmaj.121735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods 2013;18:137–50. 10.1037/a0031034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Richiardi L, Bellocco R, Zugna D. Mediation analysis in epidemiology: methods, interpretation and bias. Int J Epidemiol 2013;42:1511–9. 10.1093/ije/dyt127 [DOI] [PubMed] [Google Scholar]
- 33. Viechtbauer W. Conducting Meta-Analyses in R with the metafor Package. J Stat Softw 2010;36:1–48. 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- 34. Madsen IEH, Nyberg ST, Magnusson Hanson LL, et al. Job strain as a risk factor for clinical depression: systematic review and meta-analysis with additional individual participant data. Psychol Med 2017;47:1342–56. 10.1017/S003329171600355X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Burns RA, Butterworth P, Anstey KJ. An examination of the long-term impact of job strain on mental health and wellbeing over a 12-year period. Soc Psychiatry Psychiatr Epidemiol 2016;51:725–33. doi: 10.1007/s00127-016-1192-9. [Epub ahead of print:13 Feb 2016]. [DOI] [PubMed] [Google Scholar]
- 36. Wang J, Schmitz N, Dewa C, et al. Changes in perceived job strain and the risk of major depression: results from a population-based longitudinal study. Am J Epidemiol 2009;169:1085–91. 10.1093/aje/kwp037 [DOI] [PubMed] [Google Scholar]
- 37. Welsh J, Korda RJ, Joshy G, et al. Psychological distress and ischaemic heart disease: cause or consequence? Evidence from a large prospective cohort study. J Epidemiol Community Health 2017;71:jech-2017-209535–89. 10.1136/jech-2017-209535 [DOI] [PubMed] [Google Scholar]
- 38. Moran AE, Liu K. Invited commentary: quantifying the added value of repeated measurements. Am J Epidemiol 2017;186:908–9. 10.1093/aje/kwx146 [DOI] [PubMed] [Google Scholar]
- 39. Oshio T, Tsutsumi A, Inoue A. Do time-invariant confounders explain away the association between job stress and workers' mental health? Evidence from Japanese occupational panel data. Soc Sci Med 2015;126:138–44. 10.1016/j.socscimed.2014.12.021 [DOI] [PubMed] [Google Scholar]
- 40. Milner A, Krnjack L, LaMontagne AD. Psychosocial job quality and mental health among young workers: a fixed-effects regression analysis using 13 waves of annual data. Scand J Work Environ Health 2017;43:50–8. 10.5271/sjweh.3608 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
oemed-2018-105595supp001.pdf (440.8KB, pdf)