Abstract
To study the prevalence of chronic suppurative otitis media among school children in Belagavi, rural area of South India. A community based descriptive cross sectional survey was conducted in 7 schools of rural areas of Belagavi district in Karnataka over a period of 2 months between 15th July and 15th September 2018. A survey demographic data collection was done on 694 school children aged between 6 and 14 years attending these schools. A detailed history and otoscopic examination was done in the school premises. Data received from the study was entered and statistical analysis was done. CSOM was present in 36 (5.2%) out of 694 students examined among which 22 (6.8%) of them lived in families with overcrowding. H/o cleaning the ear with various materials was given by 27 (7.4%) of them. 29 (9.3%) of them had recurrent respiratory tract infection, 7 students had active disease. The prevalence of CSOM in this study is relatively lower in this part of the rural South India. There is a higher prevalence of safe disease with central perforation than unsafe disease. Recurrent respiratory tract infections and history of cleaning of ear were the predictors of CSOM among school children. There is a need for better knowledge of illness and screening programme for early detection and management.
Keywords: Chronic suppurative otitis media, Prevalence, Children, Belagavi
Introduction
Chronic suppurative otitis media (CSOM) is one of the most common diseases of the middle ear particularly in childhood [1]. It is a common health problem in a developing country like India especially in the lower socio economic status. Overcrowding, poor hygiene and housing conditions, poor nutrition, frequent upper respiratory tract infections are some of the risk factors contributing to the condition [2, 3].
CSOM is characterised by persistent ear discharge through a perforated tympanic membrane for more than 2 weeks [4]. It is one of the leading causes of preventable disabling hearing impairment leading to poor scholastic performance, delayed speech and language development and poor cognition. The global burden of CSOM varies between 1 and 46%, A prevalence of 4% or greater indicates a public health problem that needs urgent attention [5]. Over 90% of the burden is borne by countries in the South-east Asia and Western Pacific regions, Africa, and several ethnic minorities in the Pacific rim. CSOM is uncommon in the Americas, Europe, the Middle East, and Australia [6].
With this background this study was undertaken to find out the prevalence of CSOM, its association with age, sex and other potential contributing factors among school going children in Belagavi, rural area of South India.
Materials and Methods
A community based descriptive cross sectional survey was conducted in 7 schools of Belagavi over a period of 2 months between 15th July and 15th September 2018. All 7 schools were located in rural areas of Belagavi district (Hukkeri, Sankeshwar, Itagi) in Karnataka, South India. Ethical clearance was obtained from local institutional ethical committee.
Assent was obtained from class teachers and school headmaster as the students examined were below 18 years of age. A survey demographic data collection using questionnaire was done on 694 school going children aged between 6 and 14 years attending these schools. Sample size (N) was 694 by universal sampling technique where all the students present in the school premises at that time were examined. Exclusion criteria was none. Students were asked about their age, parents education status, parents occupation, living conditions like total income of family, number of family members and number of rooms at home. They were also asked about history of recurrent respiratory tract infection and its frequency, history of cleaning the ear using various objects like ear buds, match stick, hair pin, pen, pencil, key etc.
A detailed history and otoscopic examination was done in the school premises. Those students with wax in the ear were either cleaned and examined there only or prescribed wax dissolving agents. Aural toileting was done and students were re examined after 5 days in school premises. Those with history of ear discharge and permanent perforation of tympanic membrane were diagnosed as cases of CSOM. Further they were classified as tubotympanic type if perforation was in pars tensa and atticoantral type if perforation was in pars flaccida or if retraction pocket, cholesteatoma was present. Data received from the study was entered, expressed in proportions and was analyzed using Chi square test. p < 0.05 was considered as statistically significant. Statistical analysis was done using statistical package for social sciences (SPSS) software version 20.0.
Results
Out of 694 students examined CSOM was present among 36 (5.2%) students. 29 of them had tubotympanic type of disease and 7 of them had atticoantral disease (Figs. 1, 2). Out of 36 students, 19 (5.1%) were boys and 17 (5.3%) were girls. 31 out of 36 (4.5%) students were above or of 11 years of age.
Fig. 1.
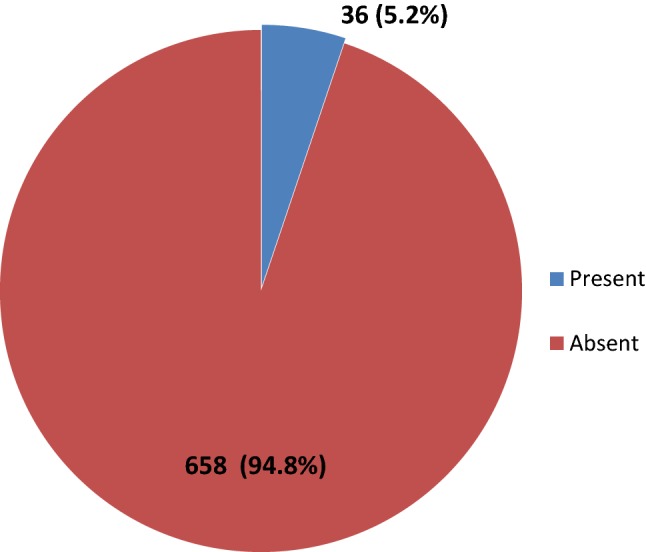
Prevalence of CSOM in study participants
Fig. 2.
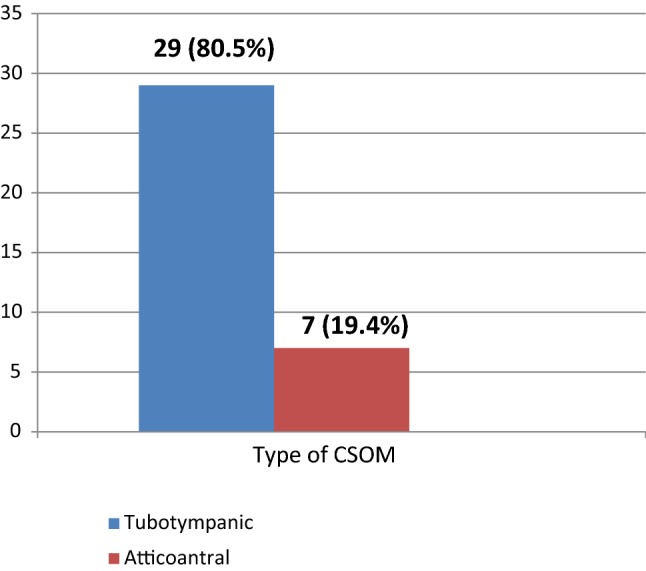
Prevalence of type of CSOM in study participants
Mothers of 12 (7.2%) students and fathers of 6 (5.4%) students with CSOM were illiterate.
Out of 36 students with CSOM 22 (6.8%) of them lived in families with overcrowding.
Among children with CSOM 27 (7.4%) of them gave h/o cleaning the ear with various instruments like ear buds, hair pin, match stick, pen, pencil, key etc. and 29 (9.3%) of them had recurrent respiratory tract infection both of which are statistically significant.(p < 0.05).
All the students diagnosed as cases of CSOM gave h/o ear discharge in the past and 7 (19.4%) of them had active disease (Tables 1, 2, 3).
Table 1.
Demographic characteristics of study participants (N = 694)
| Demographic profile | Characteristic | N (%) |
|---|---|---|
| Gender | Boys | 372 (53.6) |
| Girls | 322 (46.3) | |
| Age (in years) | ≤ 10 | 49 (7) |
| ≥ 11 | 643 (92.6) | |
| Mothers education | Illiterate | 166 (23.9) |
| Literate | 527 (75.9) | |
| Father’s education | Illiterate | 116 (16.7) |
| Literate | 578 (83.2) |
Table 2.
Association of demographic characteristics with CSOM
| Demographic characteristics | CSOM present (%) | CSOM absent (%) | Chi square value | p value |
|---|---|---|---|---|
| Gender | ||||
| Boys | 19 (5.1) | 353 (94.9) | 0.10 | 0.919 |
| Girls | 17 (5.3) | 305 (94.7) | ||
| Age (in years) | ||||
| ≤ 10 | 5 (9.8) | 46 (90.2) | 1.48 | 0.22 |
| ≥ 11 | 31 (4.9) | 612 (95.1) | ||
| Mother’s education | ||||
| Illiterate | 12 (7.2) | 154 (92.8) | 2.16 | 0.14 |
| Literate | 23 (4.4) | 504 (95.6) | ||
| Father’s education | ||||
| Illiterate | 6 (5.4) | 110 (94.6) | 0.001 | 0.90 |
| Literate | 30 (5.2) | 548 (94.8) | ||
Table 3.
Association of various risk factors with CSOM
| Risk factors for CSOM | CSOM present (%) | CSOM absent (%) | Chi square value | p value |
|---|---|---|---|---|
| Overcrowding | ||||
| Present | 22 (6.8) | 302 (93.2) | 3.17 | 0.075 |
| Absent | 14 (3.8) | 356 (96.2) | ||
| H/o respiratory tract infection | ||||
| Present | 29 (9.3) | 282 (90.7) | 19.61 | < 0.0001* |
| Absent | 7 (1.8) | 376 (98.2) | ||
| H/o ear cleaning | ||||
| Present | 27 (7.4) | 339 (92.6) | 7.55 | 0.006* |
| Absent | 9 (2.7) | 319 (97.3) | ||
| H/o ear discharge | ||||
| Present | 31 (100) | 0 (0) | 593.10 | < 0.0001* |
| Absent | 5 (0.7) | 658 (99.3) | ||
*p values are statistically significant as p < 0.05
Discussion
CSOM is a common disease to come across in day to day ENT practice. It is associated with permanent changes of middle ear and structural abnormality of pars tensa or pars flaccida that occurs due to inadequately treated acute otitis media, eustachian tube dysfunction, negative middle ear pressure or chronic otitis media with effusion [7, 8].
The present study was a cross sectional study conducted in 7 different schools on 694 students. The prevalence of CSOM in this study is 5.2% which is less than the prevalence reports of CSOM in other parts of Indian subcontinent. No significant difference was present in its prevalence with respect to age and gender of students.
A study conducted by Parvez et al. [9] at Aligarh, Uttar Pradesh on 610 children estimated the overall prevalence of CSOM to be 6.1% which was found to be 7% in rural area and 1.8% in urban area. Studies in China by Chen et al. [10] have reported prevalence of 9.82%. The prevalence of CSOM was found to be 6% in a study conducted by Rupa et al. [11] in Tamil Nadu while Verma et al. [12] in Haryana have estimated the prevalence of CSOM to be 15.3% which is much higher than that of present study. Two studies in developing country like Bangladesh also reported prevalence of 5.2% and 7.3% among school going children [13, 14].
Of the 36 students with CSOM, 29 (80.5%) of them had mucosal disease and 7 (19.4%) of them had atticoantral disease which means there is a higher prevalence of safe disease than unsafe disease. An institutional study by Kumari et al. [15] conducted in Hyderabad, Telangana showed high prevalence of squamosal disease (47.3%) when compared to mucosal type (18.5%). Another study by Basak et al. [8] in West Bengal reported the prevalence of tubotympanic disease to be 86% and of atticoantral type 14%.
Though parental illiteracy, overcrowding and poor socioeconomic status has been identified as the independent risk factors for CSOM this study could not establish any correlation between the same. Some studies have shown significant association of CSOM between nutritional status of child and standard of living index [9]. Improvement in housing, hygiene and nutrition condition was found to halve the prevalence of CSOM in Maori children between 1978 and 1987 [16].
In this study a strong association was found to be present between CSOM and h/o recurrent respiratory tract infections and h/o cleaning of ear with various objects. This is in accordance to the result described by Kumari et al. [15] in their study that occurrence of nasal/nasopharyngeal disorders such as sinusitis and tonsillopharyngitis was high in CSOM. A study by Muftah et al. [17] also identified recurrent respiratory tract infections of more than three times per year has been identified as the independent risk factor of CSOM.
Conclusion
CSOM is still a prevalent pathology in a developing country like India. It is a matter of serious concern with regard to long term affects like early communication, language development and educational progress.
At present the scenario has improved due to better health care services and good access to health facilities.
There is a need for better knowledge of the illness, better ear care and screening programme for early detection and management of CSOM.
Compliance with Ethical Standards
Conflict of interest
Shama A. Bellad, Avinash Kavi, R. S. Mudhol declare that we have no cConflict of interest.
Ethical Approval
The study has been approved by the institutional ethics committee and the study has been performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
As the study participants are below 18 years of age and not eligible to give consent, assent was obtained from class teacher and the school headmaster.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kong K, Coates HL. Natural history, definitions, risk factors and burden of otitis media. Med J Aust. 2009;191(Suppl9):S39–S43. doi: 10.5694/j.1326-5377.2009.tb02925.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thakur SK, Singh SK, Acharya R, Anwar A, Ghimire N. Sociodemographic profile and the associated factors of chronic otitis media in rural areas of eastern Nepal. Int J Otorhinolaryngol Head Neck Surg. 2017;3:222–227. doi: 10.18203/issn.2454-5929.ijohns20170905. [DOI] [Google Scholar]
- 3.Hunt L, Mulwafu W, Knott V, et al. Prevalence of paediatric chronic suppurative otitis media and hearing impairment in rural Malawi: a cross-sectional survey. PLoS One. 2017;12(12):e0188950. doi: 10.1371/journal.pone.0188950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith AW, Hatcher J, Mackenzie IJ, Thompson S, Bal I, Macharia I, et al. Randomised controlled trial of treatment of chronic suppurative otitis media in Kenyan school children. Lancet. 1996;348(9035):1128–1133. doi: 10.1016/S0140-6736(96)09388-9. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization (1996) Prevention of hearing impairment from chronic otitis media. In: Report of a WHO/CIBA foundation workshop, held at The CIBA Foundation. World Health Organization, London, U.K., pp 19–21
- 6.Acuin J. Chronic suppurative otitis media-Burden of illness and management options. Geneva: World Health Organization; 2004. [Google Scholar]
- 7.Vikram BK, Khaja N, Udayashankar SG, et al. Clinico-epidemiological study of complicated and uncomplicated chronic suppurative otitis media. J Laryngol Otol. 2008;122:442–446. doi: 10.1017/S0022215107000278. [DOI] [PubMed] [Google Scholar]
- 8.Basak B, Gayen GC, Das M, et al. Demographic profile of CSOM in a rural tertiary care hospital. IOSR J Pharm. 2014;4(6):43–46. [Google Scholar]
- 9.Parvez A, Khan Z, Hashmi SF, Khan MS. A cross sectional study of chronic suppurative otitis media and its associated factors among primary school children in rural and urban areas of Aligarh, India. Int J Commun Med Public Health. 2016;3:2150–2154. doi: 10.18203/2394-6040.ijcmph20162561. [DOI] [Google Scholar]
- 10.Chen CH, Lin CJ, Hwang YH, et al. Epidemiology of otitis media in Chinese children. Clin Otolaryngol Allied Sci. 2003;28(5):442–445. doi: 10.1046/j.1365-2273.2003.00741.x. [DOI] [PubMed] [Google Scholar]
- 11.Rupa V, Jacob A, Joseph A, et al. CSOM: prevalence and practices among rural south indian children. Int J Pediatr Otorhinolaryngol. 2003;48(3):217–221. doi: 10.1016/S0165-5876(99)00034-8. [DOI] [PubMed] [Google Scholar]
- 12.Verma AK, et al. Epidemiology of CSOM and deafness in a rural area and developing an intervention strategy. Indian J Pediatr. 1995;62(6):725–729. doi: 10.1007/BF02825128. [DOI] [PubMed] [Google Scholar]
- 13.Shaheen MM, Raquib A, Ahmad SM. Indian J Otolaryngol Head Neck Surg. 2012;64:36. doi: 10.1007/s12070-011-0150-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kamal N, Joarder AH, Chowdhury AA, Khan AW. Prevalence of chronic suppurative otitis media among the children living in two selected slums of Dhaka City. Bangladesh Med Res Counc Bull. 2004;30(3):95–104. [PubMed] [Google Scholar]
- 15.Kumari MS, Madhavi J, Krishna NB, Meghanadh KR, Jyothy A. Prevalence and associated risk factors of otitis media and its subtypes in South Indian population. Egypt J Ear Nose Throat Allied Sci. 2016;17:57–62. doi: 10.1016/j.ejenta.2016.04.001. [DOI] [Google Scholar]
- 16.Giles M, Asher I. Prevalence and natural history of otitis media with perforation in Maori school children. J Laryngol Otol. 1991;105:257–260. doi: 10.1017/S0022215100115555. [DOI] [PubMed] [Google Scholar]
- 17.Muftah S, Mackenzie I, Faragher B, Brabin B. Prevalence of chronic suppurative otitis media (CSOM) and associated hearing impairment among school-aged children in Yemen. Oman Med J. 2015;30(5):358. doi: 10.5001/omj.2015.72. [DOI] [PMC free article] [PubMed] [Google Scholar]


