Abstract
The aim of the study was to re- evaluate the current bacteriological profile of chronic suppurative otitis media and to know their antibiotic sensitivity pattern to commonly used antibiotics. To provide a guideline for empirical antibiotic therapy when culture facilities are not available. Observational study. Patients who presented to Ear, Nose and Throat department with chronic or recurrent ear discharge and on clinical examination found to have actively discharging ears were selected. Patients who did not receive antimicrobial therapy (topical or systemic) for the last 7 days were included. Out of the 106 ear swabs processed, bacterial growth was found in 100 samples (94.33%), while 6 samples (5.66%) showed no growth. The results revealed Pseudomonas aeruginosa as the most isolated bacteria (49%), followed by Staphylococcus aureus (18%). Antibiotic susceptibility—Pseudomonas aeruginosa was sensitive to Cefoperazone–Sulbactam (96%), Imipenem (82%), Piperacillin–Tazobactam (82%), Amikacin in 82% and Gentamicin (76%). It was found that Pseudomonas was sensitive to Ciprofloxacin in only 57% of the cases. Staphylococcus aureus isolates were sensitive to Vancomycin in 90%, Gentamicin in 81%, Clindamycin in 72%, and Erythromycin in 45%. It was found that 100% of the isolates were resistant to Ciprofloxacin. Our findings highlight the importance of continuous and periodic evaluation of microbiological pattern and antibiotic sensitivity of isolates in chronic suppurative otitis media patients to decrease the potential risk of complications by early institution of appropriate treatment.
Keywords: Chronic suppurative otitis media, Pseudomonas aeruginosa, Staphylococcus aureus, Antibiotic sensitivity
Introduction
Chronic suppurative otitis media (CSOM) is an infection of the middle ear cleft lasting for 12 weeks and beyond [1]. It is a major health problem in developing countries causing serious local damage and threatening complications [2]. The prevalence accounts for 72/1000 people [3].
In chronic infections, Proteus mirabilis, Pseudomonas aeruginosa, and enterococcus are often seen. Factors which increase virulence of bacteria include: Biofilm formation, Beta lactamase production, Metalloprotease production, Colony swarming, Lipopolysacharide, motility, capsule formation [3].
The indiscriminate, haphazard, and half-hearted use of antibiotics and poor follow up have resulted in persistence of low grade infections and antibiotic resistance [3].
The aim of the study is to re-evaluate the current bacteriological profile of CSOM and the sensitivity pattern to most of the currently available antibiotics in our environment [1].
Materials and Methods
We conducted a prospective study for a period of 6 months (January 2018–June 2018) in a tertiary care hospital of Mysuru, India. The study was approved by our Institutional Ethical Committee. Written informed consent (signed by patient or parent/guardian) was obtained from all patients.
Inclusion criteria was patients presenting with chronic or recurrent ear discharge for more than 12 weeks, and on clinical examination found to have discharging ears. Patients who did not receive antimicrobial therapy (topical or systemic) for the last 7 days were included.
Aural swabs were used to collect ear discharges, under illumination, by swabbing the discharging ears with a sterile cotton swab after dry mopping the discharge in the external ear to avoid contamination of the middle ear samples. The samples were immediately sent to the hospital’s microbiology laboratory without delay and samples were inoculated onto Mac Conkey agar (MCA), Blood Agar (BA), and chocolate agar plates. MCA and BA plates were inoculated aerobically at 37 °C for 27–48 h.
Organisms were identified using standard procedures [2]. Antimicrobial sensitivity testing for aerobic isolates was carried out by Kirby Bauer disc diffusion method on Muller Hinton agar. Results were interpreted in accordance with central laboratory standards institute guidelines [2].
Results
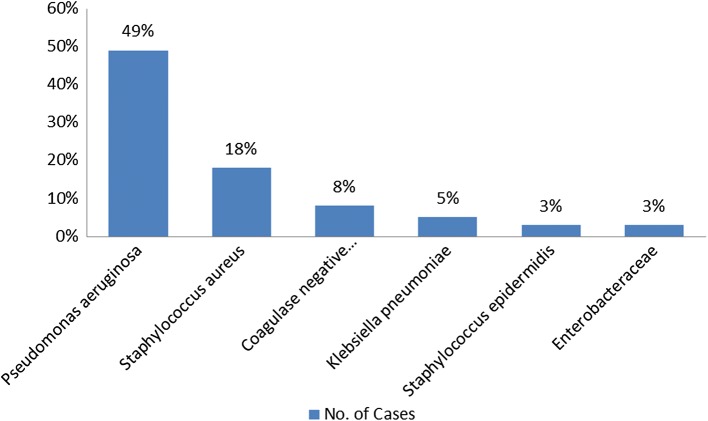
Out of 106 cases studied, 67 (63.20%) were males and 39 (36.79%) were females, giving a male to female ratio of 1.6:1. Higher incidence of CSOM was seen in age group of 19–45 years (52%) and it decreases as the age increases. In our study, we found the incidence of CSOM above 45 years of age to be 10%. Out of the 106 ear swabs processed, bacterial growth was found in 100 samples (94.33%), while 6 samples (5.66%) showed no growth. The results revealed Pseudomonas aeruginosa as the most commonly isolated bacteria (49) (49%), followed by Staphylococcus aureus 18 (18%). Other organisms isolated were coagulase negative Staphylococcus aureus (8%), Klebsiella pneumoniae (5%), Staphylococcus epidermidis (3%) and Enterobacteriacea (3%) (Fig. 1).
Fig. 1.
Spectrum of bacterial isolates in chronic suppurative otitis media
Antibiotic susceptibility
In our study, Pseudomonas Aeruginosa was sensitive to Cefoperazone–Sulbactam combination (96%), Intermediate in 1%, resistant in 3%. Isolates were sensitive to Ciprofloxacin (57%), intermediate in 14%, resistant in 28%. Isolates were sensitive to Gentamicin (76%) and resistant in 24%. Pseudomonas aeruginosa was sensitive to Imipenem (82%) intermediate in 3%, resistant in 14%, sensitive to Piperacillin–Tazobactam (82%),intermediate in 14%, resistant in 3%, sensitive to Amikacin in 82%, resistant to the same in 18% (Table 1).
Table 1.
Antibiotic Sensitivity patterns of Pseudomonas aeruginosa in chronic suppurative otitis media
| Antibiotic Class | Antibiotic | Sensitive (%) | Intermediate (%) | Resistant (%) |
|---|---|---|---|---|
| Cephalosporin | Cefoperazone + Sulbactam | 96 | 1 | 3 |
| Aminoglycoside |
Amikacin Gentamycin |
82 76 |
0 0 |
18 24 |
| Carbapenem | Imipenem | 82 | 3 | 14 |
| Penicillins | Piperacillin/Tazobactam | 82 | 14 | 3 |
| Fluoroquinolones | Ciprofloxacin | 57 | 14 | 28 |
Staphylococcus aureus isolates were sensitive to Erythromycin (45%), intermediate in 10%, resistant in 45%. Isolates were sensitive to Gentamicin in 81%, resistant in 18%. Staphylococcus aureus was sensitive to Clindamycin in 72%,resistant in 27%. Isolates were sensitive to Vancomycin in 90%, resistant in10% (Table 2). It was also found that 100% of the Staphylococcus aureus isolates were resistant to Ciprofloxacin.
Table 2.
Antibiotic Sensitivity patterns of Staphylococcus aureus in chronic suppurative otitis media
| Antibiotic class | Antibiotic | Sensitive (%) | Intermediate (%) | Resistant (%) |
|---|---|---|---|---|
| Aminoglycosides | Gentamicin | 81 | 0 | 18 |
| Glycopeptide antibiotic | Vancomycin | 90 | 0 | 10 |
| Lincomycin antibiotic | Clindamycin | 72 | 0 | 27 |
| Fluoroquinolones | Ciprofloxacin | 0 | 0 | 100 |
| Macrolide antibiotic | Erythromycin | 45 | 10 | 45 |
Discussion
CSOM is a major public health problem and India is one of the countries with a high prevalence rate. It is a persistent disease with great risk of irreversible complications. CSOM is an important cause of preventable hearing loss particularly in the developing world [2]. It is calculated that about 13.8–36.2% of the people have hearing impairment due to CSOM [3].
The mucopus removed from ears with active COM is rarely sterile. Early, microbiological diagnosis ensures prompt and effective treatment to avoid complications. Microbiology cultures yield many organisms and these vary depending on climate, patient population and whether antibiotics have or have not been recently used. The proportion of different organisms isolated vary from study to study, but Proteus species and Pseudomonas aeruginosa most frequently predominate. Pseudomonas is ubiquitous in our physical environment and has a predilection for moist areas. It is thought to infect tissues first by adherence to epithelial cells by means of pili or fimbriae. Deb et al. in their study, found the most common bacteria isolated to be Escherchia coli (20.75%0, and Staph. Aureus (20.75%), followed by Proteus (16.98%) [5]. Samanth et al. in their study found Staphylococcus aureus to be the most commonly isolated organism (35%). Our study showed the most commonly isolated organism to be Pseudomonas aeruginosa (49%). This correlates with a similar study done by Kazeem et al. which showed Pseudomonas aeruginosa to be the commonly isolated organism (31.5%), followed by Staphylococcus aureus (23.2%). The predominance of Gram negative aerobes indicates that the source of the infection is not the nasopharynx, which doesn’t contain these organisms. Scott Brown [4] in our study, Staphylococcus epidermidis was isolated in 3% of cases which was probably a contaminant of external auditory canal skin.
The widespread use of antibiotics has precipitated the emergence of multiple resistant strains of bacteria which can produce both primary and post operative infection. Hence, in vitro antibiotic sensitivity pattern is very important for the clinician to plan a general outline of treatment for a patient with a chronically discharging ear [3].
In the present study, patients of different age groups presenting with complaints of ear discharge were selected (106). Aural swabs were collected in sterile test tubes, with sterile cotton swabs, under direct illumination. Culture was done in the microbiology laboratory of the hospital using standard procedures. Antibiotic sensitivity to commonly used antibiotics was done using Kirby Bauer disc diffusion method on Muller Hinton agar and results were interpreted.
A study conducted by Deb et al. showed Ciprofloxacin to be effective in eradicating majority of gram negative bacteria in which it was tested [5]. Prakash et al. in their study, found that Pseudomonas aeruginosa was sensitive to Amikacin, Gentamicin and Ciprofloxacin [2]. In our study, Pseudomonas aeruginosa isolates were found to be sensitive to Cefoperazone–Sulbactam combination (96%), to Piperacillin–Tazobactam (82%), to Amikacin in 82%, to Imipenem in 82% and to Ciprofloxacin in 57%. This result is parallel with the results of study conducted by Mofatteh et al. which showed Pseudomonas aeruginosa sensitive to Imipenem (100%), Ciprofloxacin (93.7%), and Amikacin (93.7%) [6]. Our results also showed Staphylococcus aureus sensitive to Vancomycin in 90%, to Gentamicin in 81%, to Clindamycin in 72%, and to Erythromycin in 45%. This is similar to results obtained by Samanth et al. which found Staphylococcus aureus sensitive to Vancomycin (100%), to Gentamycin (100%), and to Erythromycin in 62% [3].
Our study showed that, of the Staphylococcus aureus isolates obtained, 100% were resistant to Ciprofloxacin. This is however in contrast with the results obtained by Mofatteh et al. which showed Staphylococcus aureus with only resistance of 13% to Ciprofloxacin. [6] This may be due to indiscriminate use of Ciprofloxacin ear drops.
Overall, our study showed significant difference in isolates and antimicrobial susceptibility patterns in CSOM patients compared to previous studies conducted. The variation may be related to differences in geography, local antimicrobial prescribing practices and the prevalence of resistant bacterial strains.
The limitation of our study is that we did not study the anaerobic bacterial profile in chronic suppurative Otitis media.
Conclusion
With the development and widespread use of antibiotics, the types of pathogenic micro-organisms and their resistance to antibiotics have changed. Continuous and periodic evaluation of microbiological pattern and antibiotic sensitivity of isolates is necessary to decrease potential risk of complications by early institution of appropriate treatment. Our findings highlight the importance of Pseudomonas aeruginosa and Staphylococcus aureus as the most common causative agent for chronic suppurative Otitis media. Antibiotic sensitivity pattern revealed sensitivity to antibiotics like Cefoperazone–Sulbactam, followed by Imipenem, Piperacillin–Tazobactam, Vancomycin, Gentamicin.
Another significant finding was that Pseudomonas aeruginosa was sensitive to Ciprofloxacin in only 57% of cases and Staphylococcus aureus was resistant to Ciprofloxacin in 100% of the cases.
Compliance with Ethical Standards
Conflict of interest
All the authors declare they have no conflicts of interest and have not received any funding.
Informed Consent
Informed consent was obtained from all individual participants in the study.
Ethical Approval
All procedures performed in the study were in accordance with the ethical standards of the institution.
References
- 1.Kazeem MJ, Aiyeleso R. Current bacteriological profile of chronic suppurative otitis media in a tertiary facility of Northern Nigeria. Indian J Otol. 2016;22:157–161. doi: 10.4103/0971-7749.187979. [DOI] [Google Scholar]
- 2.Prakash R, Juval D, Negi V, Pal S, Adekhandi S, et al. Microbiology of Chronic Suppurative Otitis media in a Tertiary Care setup of Uttarkhand state. India. N Am J Med Sci. 2013;5(4):282–287. doi: 10.4103/1947-2714.110436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samanth TU, Jha SG, Sinha V, Dadhich S. Bacteriology and drug susceptibility in chronic suppurative otitis media in Ear, Nose and Throat outpatient and inpatient department of tertiary care hospital, Bhavnagar, Indian. J Otol. 2017;23:252–255. [Google Scholar]
- 4.Scott Brown WG. Otorhinolaryngology, head and neck surgery. 6. Boca Raton: CRC press; 1996. [Google Scholar]
- 5.Deb T, Ray D. A study of the Bacteriological Profile of Chronic Suppurative Otitis Media in Agartala. Indian J Otolaryngol Head Neck Surg. 2012;64(4):326–329. doi: 10.1007/s12070-011-0323-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mofatteh MR, Shahabian Moghaddam F, Yousefi M, et al. A study of bacterial pathogens and antibiotic susceptibility patterns in chronic suppurative otitis media. The journal of Laryngology and Otology. 2018;132:41–45. doi: 10.1017/S0022215117002249. [DOI] [PubMed] [Google Scholar]