Abstract
Squamous chronic otitis media (COM) implies formation of a retraction pocket (inactive form) or frank cholesteatoma (active form) in pars tensa or pars flaccida of tympanic membrane. A retraction pocket or frank cholesteatoma are believed to occur due to tubal dysfunction. The present study was undertaken to investigate the pattern of mastoid pneumatisation and Eustachian dysfunction by dynamic slow motion videoendoscopy (DSVE) in cases of both, active and inactive type of squamous chronic otitis media (COM). 52 patients (65 ears) comprising of twenty-six ears with pars flaccida squamous disease and 39 ears with Pars Tensa squamous disease were enrolled for the study. DSVE findings, in terms of grade and type of Eustachian dysfunction were noted. Mastoid pneumatization pattern on CT-scans, and peroperative status of mastoid pneumatisation, especially contracted mastoid with anteriorly placed sigmoid sinus or low lying dura were also recorded for every case while performing tympano-mastoidectomy. Primary sclerotic/diploic type of mastoid pneumatisation pattern and Eustachian dysfunction were found to have inverse relationship in the cases of squamous otitis media. Eustachian dysfunction, diagnosed on DSVE, had significant association with both pars flaccida (P = 0.0001) and pars tensa disease (P = 0.0007). Primary sclerotic or diploic mastoid were found to be more common in ears with pars flaccida squamous disease than pars tensa COM (46.15% vs. 38.46%, P < 0.05).
Keywords: Squamous otitis media, Dynamic slow motion endoscopy, Eustachian tube function, Mastoid pneumatisation, Mastoid sclerosis
Introduction
Squamous Chronic Otitis media (COM) can manifest in passive (retraction pocket) or active form (frank cholesteatoma formation). It could involve Pars flaccida or Posterosuperior portion of pars tensa. Both Pars flaccida and Pars Tensa cholesteatomas begin as retraction pockets [1, 2]. A retraction pocket is believed to occur due to tubal dysfunction, leading to negative middle ear pressure and finally may result in frank cholesteatoma [3, 4].
Other important association that has been observed is that pars flaccida retraction pocket/cholesteatoma are more common in poorly pneumatized mastoids and the severity of retraction has been shown to have direct relationship with the degree of mastoid pneumatization. Well pneumatized mastoids usually show normal pars flaccida [5]. Mastoid pneumatisation plays the role of passive middle ear pressure buffer and hence ears with sclerotic type of mastoids are at a risk of developing complications like retraction pockets, ossicular necrosis and retraction pocket cholesteatoma [5]. Other studies have found cholesteatoma in ears with well –pneumatized mastoids [6].
It is still not clear whether primary sclerosis or secondary sclerosis is associated with cholesteatoma. Most cases of otitis media have secondary sclerosis, due to new bone formation [7]. With the hypothesis that primary sclerosis, is genetically determined, and associated with contracted mastoid, may have an etiological role in squamous otitis media, whereas secondary sclerosis, observed in both squamosal and mucosal disease is a result, and not the cause, of otitis media or Eustachian dysfunction, we undertook this study to find out the incidence of primary sclerosis/contracted mastoid versus Eustachian dysfunction in cases of squamous otitis media of primary acquired type. This is probably first such correlative study.
Materials and methods
This was a prospective cross-sectional study, carried out at a rural tertiary centre of central India, between August 2012 and June 2016. All the patients diagnosed as squamous otitis media of primary type, that is involving pars flaccida or postero-superior quadrant of pars tensa and who gave consent, were enrolled for the study, after approval of “Institutional ethics committee”. The cases comprised of, both inactive squamous otitis media (retraction pocket, where fundus of the retraction could be seen) and active squamous otitis media (frank cholesteatoma or deep pocket where fundus could not be seen) involving either pars flaccida or pars tensa. Patients with pars tensa marginal or subtotal perforations with cholesteatoma (secondary acquired cholesteatoma) and totally adhesive tympanic membranes were excluded. The methodology is shown in the flow chart (Fig. 1). Otoscopy and otomicroscopy was done to confirm the ear findings and middle ear disease was classified using the classification adapted from Browning. Dynamic slow motion video-endoscopy was done in each case to document functional or mechanical type of Eustachian dysfunction. 30° rigid Karl Storz nasal endoscope of 4 mm diameter Endoscope was introduced along the floor of the nasal cavity after anaesthetizing the nasal cavity with local anaesthetic agent in the form of 4% xylocaine soaked cotton pledgets, with patient in supine position. Transnasal endoscopic examination of the nasopharyngeal opening of ET during rest, swallowing and yawning was carried out to study its dilatory movements and recorded with the help of scopydoc recording software and analysed in slow motion. Eustachian function Grading was done. Grades 0 and 1 were considered as normal whereas Grades 2 (A and B) and Grade 3 (A, B and Patulous) were considered as dysfunctional [8, 9]. Radiological investigations in the form of High Resolution Computed Tomography (HRCT) Scan were done in each case. Mastoid pneumatization pattern on CT-Scans along with peroperative status of mastoid pneumatisation, especially contracted mastoid with anteriorly placed sigmoid sinus or low lying dura, were noted during tympano-mastoidectomy and correlated with Eustachian function (Figs. 2, 3a–c).
Fig. 1.
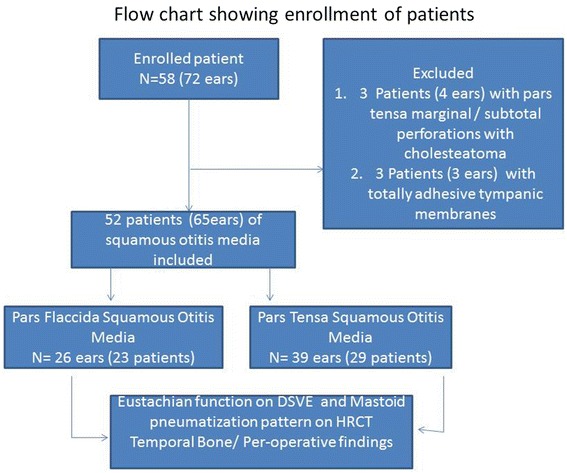
Flow chart
Fig. 2.
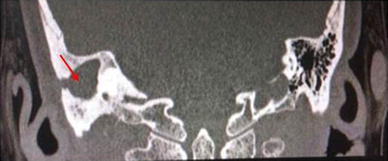
Coronal section of high resolution computed tomography (HRCT) scan of temporal bone, showing well pneumatized mastoid on left side and right mastoid showing secondary sclerosis with soft tissue density lesion (red arrow)
Fig. 3.
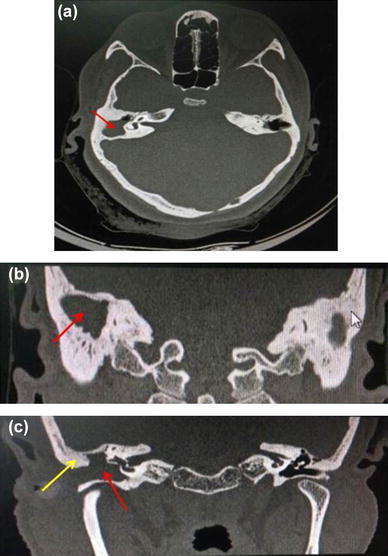
Bilateral primary sclerotic mastoid. a Axial section of HRCTscan of temporal bone showing soft tissue density of cholesteatoma (red arrow) on right side. b, c Coronal sections showing bilateral primary sclerotic mastoid pneumatisation with soft tissue density lesion (red arrow) filling attic and mesotypanum causing destruction of scutum (yellow arrow)
Results
A total of 52 patients of squamous otitis media were studied. Most of the patients (42.32%) were in the age group of 16–30 years and 27 patients (51.92%) were males (Table 1). Among 52 patients, 65 ears with squamous type of COM were studied, out of which, 26 ears (23 patients) had Pars Flaccida Squamous Otitis Media and 39 ears (29 patients) had Pars Tensa Squamous Otitis Media (Table 2). Simultaneous bilateral disease was more common in Pars Tensa disease in 24.2% of patients, as compared to Pars Flaccida disease in 13%. Pars Flaccida Squamous OM (Inactive and Active) was slightly more common on right side in 13 out of 23 patients (56.5%). Pars Tensa Squamous OM (Inactive and Active) was more common on left side in 13 out of 29 patients (44.8%) (Table 3).
Table 1.
Baseline characteristics
| Number of patients | Percentage | |
|---|---|---|
| Age in years | ||
| 1–15 | 8 | 15.38 |
| 16–30 | 22 | 42.32 |
| 31–45 | 20 | 38.46 |
| 46–60 | 1 | 1.92 |
| 61–75 | 1 | 1.92 |
| Total | 52 | 100.00 |
| Mean ± SD | 28.18 ± 12.23 (10–70 years) | |
| Sex | ||
| Male | 27 | 51.92 |
| Female | 25 | 48.08 |
| Total | 52 | 100.00 |
Table 2.
Distribution of type of middle ear disease (n = 65 ears)
| Diagnosis | Frequency (no. of ears) | Percentage | |
|---|---|---|---|
| (Squamous) pars flaccida COM | Inactive (squamous) pars flaccida COM (retraction) | 3 | 4.62 |
| Active (squamous) pars flaccida COM (with cholesteatoma) | 23 | 35.38 | |
| Total | Pars flaccida squamous COM (inactive and active) | 26 | 40 |
| (Squamous) pars tensa COM | Inactive (squamous) pars tensa COM (retraction) | 21 | 32.31 |
| Active (squamous) pars tensa COM (with cholesteatoma) | 18 | 27.69 | |
| Total | Pars tensa squamous COM (inactive and active) | 39 | 60 |
| Total | 65 | 100.00 |
Table 3.
Laterality of different type of middle ear disease (N = 52 pts, 65 ears)
| Diagnosis | Frequency (no. of ears) | Total no. of patients (N) | Right | Left | Bilateral | Associated with other type of disease in contralateral ear |
|---|---|---|---|---|---|---|
| Inactive (squamous) pars flaccida COM (retraction) | 3 | 2 | 1 | – | 1 | – |
| Active (squamous) pars flaccida COM (with cholesteatoma) | 23 | 21 | 12 | 6 | 2 | 1 (on left side) associated with inactive pars tensa squamous COM on right side |
| Total pars flaccida squamous COM (Inactive and Active) | 23 | 13 (56.5%) | 7 (6 + 1) (30.4%) | 3 (13%) | ||
| Inactive (squamous) pars tensa COM (retraction) | 21 | 13 | 4 | 4 | 5 | – |
| Active (squamous) pars tensa COM (with cholesteatoma) | 18 | 16 | 3 | 9 | 2 | 2 (on right side) associated with inactive squamous pars tensa COM on left side |
| Total pars tensa squamous COM (inactive and active) | 29 | 9 (7 + 2) (31%) | 13 (44.8%) | 7 (24.2%) | ||
| Total | 65 | 52 | 22 | 20 | 10 |
In cases of Pars Flaccida squamous otitis media (Active and inactive), 10 (38.5%) had normal Eustachian function on DSVE whereas 16 (61.5%) were diagnosed to have Eustachian dysfunction on DSVE {X2 20.49, P = 0.0001, S}. In cases of Pars Tensa squamous otitis media (Active and inactive), 15 (38.5%) had normal Eustachian function on DSVE whereas 24 (61.5%) were diagnosed to have Eustachian dysfunction on DSVE {X2 11.52, P = 0.0007, S} (Table 4; Fig. 4). Thus, Eustachian dysfunction, diagnosed on DSVE, had significant association with both pars flaccida (P = 0.0001) and pars tensa disease (P = 0.0007).
Table 4.
Correlation between Eustachian dysfunction by DSVE and type of middle ear disease
| Type of disease | Diagnosis | Normal ET function on DSVE (percentage) | Eustachian dysfunction on DSVE (percentage) | Total | X2-value |
|---|---|---|---|---|---|
| Pars flaccida squamous disease | Inactive (squamous) pars flaccida COM (retraction) | 2 (66.67%) | 1 (33.33%) | 3 | 20.49 P = 0.0001, S |
| Active (squamous) pars flaccida COM(with cholesteatoma) | 8 (34.8%) | 15 (65.2%) | 23 | ||
| Total | Squamous pars flaccida COM | 10 (38.5%) | 16 (61.5%) | 26 | |
| Pars tensa squamous disease | Inactive (squamous) pars tensa COM (retraction) | 8 (38.1%) | 13 (61.9%) | 21 | 11.52 P = 0.0007, S |
| Active (squamous) pars tensa COM (with cholesteatoma) | 7 (38.9%) | 11 (61.1%) | 18 | ||
| Total | Squamous pars tensa COM | 15 (38.5%) | 24 (61.5%) | 39 | |
| Total (ears) | 25 | 40 | 65 |
Fig. 4.
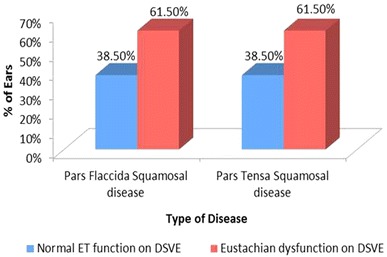
Graph showing correlation between Eustachian dysfunction by DSVE and type of middle ear disease
In cases of Pars Flaccida squamous otitis media (Active and inactive), 12 (46.15%) had primary sclerotic/diploic and contracted mastoid pneumatization pattern confirmed by peroperative condition of mastoid air cells and anteriorly placed sigmoid sinus or low lying dura whereas 14 (53.85%) were found to have secondary sclerosis in well-pneumatized mastoid {X2 = 1.28, P = 0.25, NS}. In cases of Pars Tensa squamous otitis media (Active and inactive), 15 (38.46%) had primary sclerotic/diploic and contracted mastoid pneumatization pattern whereas 24 (61.54%) had secondary sclerosis in pneumatized mastoid {X2 = 11.52, P = 0.0007, S} (Table 5; Fig. 5). Primary sclerotic/diploic mastoid were found to be more common in ears with pars flaccida squamous OM than pars tensa OM (46.15% vs. 38.46%). When the pattern of mastoid pneumatization and Eustachian function on DSVE, were analysed by Fisher’s Exact test, Primary sclerotic type of mastoid pneumatization pattern and Eustachian dysfunction were found to have significant inverse relationship in the cases of squamous otitis media with P value of < 0.05 (Table 6; Fig. 6).
Table 5.
Correlation between mastoid pneumatization and type of middle ear disease
| Diagnosis | Primary sclerotic/diploic and contracted mastoid(percentage) | Secondary sclerosis in well-pneumatized mastoid) (percentage) | Total | X2-value | |
|---|---|---|---|---|---|
| Pars flaccida squamous disease | Inactive (squamous) pars flaccida com (retraction) | 2 (66.7%) | 1 (33.3%) | 3 | 1.28 P = 0.25, NS |
| Active (squamous) pars flaccida COM (with cholesteatoma) | 10 (43.5%) | 13 (56.5%) | 23 | ||
| Total | Pars flaccida squamous COM (inactive and active) | 12 (46.15%) | 14 (53.85%) | 26 | |
| Pars tensa squamous disease | Inactive (squamous) pars tensa COM (retraction) | 8 (38.1%) | 13 (61.9%) | 21 | 11.52 P = 0.0007, S |
| Active (squamous) pars tensa COM (with cholesteatoma) | 7 (38.9%) | 11 (61.1%) | 18 | ||
| Total | Pars tensa squamous COM (inactive and active) | 15 (38.46%) | 24 (61.54%) | 39 | |
| Grand total | 27 (41.54%) | 38 (58.46%) | 65 | 8.00 P = 0.004, S |
Fig. 5.
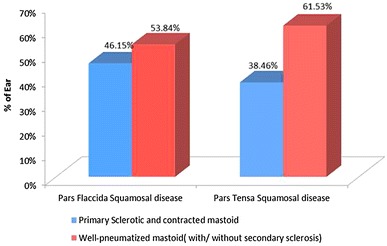
Graph showing correlation between mastoid pneumatization and type of middle ear disease
Table 6.
Correlation between presence of mastoid pneumatization and Eustachian dysfunction by DSVE in cases of chronic otitis media
| Primary sclerotic/diploic and contracted mastoid (percentage) | Secondary sclerosis in well-pneumatized mastoid (percentage) | Total | |
|---|---|---|---|
| Normal ET function on DSVE (percentage) | 25 (92.59%) | 0 (0%) | 25 |
| Eustachian dysfunction on DSVE | 2 (7.40%) | 38 (100%) | 40 |
| Total | 27 | 38 | 65 |
| Fisher’s exact test | 0.0001, S, P < 0.05 | ||
Fig. 6.
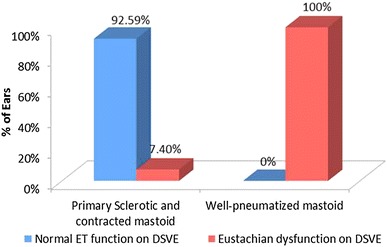
Graph showing correlation between presence of mastoid pneumatization and Eustachian dysfunction by DSVE in cases of chronic otitis media
Discussion
This study suggests that Eustachian tube dysfunction and sclerotic mastoid pneumatization pattern are independent etiological factors for squamous otitis media as they were found to have inverse relationship in patients of COM. We found both types of Eustachian dysfunction, namely of mechanical and functional type [8, 9]. If Eustachian function was found to be good on DSVE and a patient had squamous otitis media, we observed high likelihood of finding a low-lying dura or an ante-posed sigmoid sinus while doing mastoid surgery. In all patients with squamous otitis media in our study, who had good Eustachian function pre-operatively, we found poor mastoid pneumatization bilaterally (primary sclerosis/diploic) and per-operatively, the sigmoid sinus was found to be anteriorly placed.
Shatz and Sade, pointed out that the position of the sigmoid sinus is genetically determined and there is statistically significant difference between the position of sigmoid sinus in sclerotic mastoids of patients and pneumatized mastoids of controls [10]. However, Lee et al. [7] found no difference in the sigmoid sinus type in comparison between sclerotic and pneumatic mastoids. We propose that former series represents cases with primary sclerosis, which are genetically determined and have anteriorly placed sigmoid sinus, whereas latter series represents secondary sclerosis in pneumatized mastoids with no change in position of sigmoid sinus. We observed that in cases with primary sclerosis, the landmarks were anteriorly placed and it could be an etiological factor for squamous otitis media in our patients, as Eustachian function was good in these cases. Small mastoid volume acted as a contributing factor and is genetically determined. In cases with secondary sclerosis, position of sigmoid sinus was not forward and such cases had well-pneumatized mastoids genetically but developed sclerosis due to Eustachian dysfunction or otitis media. In our study, all the patients with normally placed landmarks per-operatively, were found to have Eustachian dysfunction on DSVE and this may be a possible cause of secondary sclerosis as well as squamosal otitis media. Lee et al. [7] also observed that sclerosis does not change the location of landmarks, especially the sigmoid sinus. So, secondary sclerosis, which is a result of Eustachian dysfunction or chronic otitis, as in cases of mucosal disease, has no implication in causation of squamous otitis media. Secondary sclerosis can be confirmed per-operatively by the presence of normally placed sigmoid sinus. However, primary sclerosis with contracted mastoid, which is genetically determined and bilaterally present, may contribute to squamous otitis media by affecting the mastoid buffer.
Ears with poorly pneumatized mastoids, lack the buffering action on middle ear pressure and hence, have a tendency to develop a negative gas balance, with persistent high negative pressure and resultant chronic sequelae. Sade studied the buffering action of mastoid pneumatisation on middle ear pressure and found that it fluctuates only up to 8 mm H2O in average pneumatic ears (10 cm2), whereas it is as high as 80 mm H2O, in ears with sclerotic mastoids. This leads to retraction of the pars flaccida (PF), which lacks the organized middle fibrous layer, and is the first reaction to a middle ear (ME) negative pressure in adults. Once a negative pressure sets in, various other mechanisms may also act as pressure buffers by reducing the middle ear volume. These include retraction of the pars tensa, mucosal oedema or middle ear exudate. In our study, pars flaccida squamous disease was slightly more common than pars tensa disease in ears with primary sclerosis or diploid type of pneumatisation pattern. Postero-superior retraction pockets of pars tensa can also occur in ears with poorly pneumatised mastoids (primary sclerotic or diploic) with normal Eustachian function.
Toros et al. [11] correlated mastoid pneumatisation pattern with Korner’s septum and found no association between them. We feel that Korner’s septum may be an etiological factor for COM by decreasing the mastoid buffer in cases of well- pneumatized mastoid as the presence of the septum decreases the ventilating air volume of antrum and middle ear. In one of the patients, we encountered a Korner’s septum with well-pneumatized mastoid associated with squamous otitis media.
Studies have shown that well pneumatized mastoids with a volume of 6 cm2 and above, function as pressure buffer and such ears rarely develop negative pressure or chronic ear disease [12]. In our study, we found that gross Eustachian dysfunction, even in the presence of good pneumatisation could result in both pars flaccida and pars tensa type of squamous otitis media of primary acquired type, being more common in latter type. In most cases of squamous disease, we found mechanical dysfunction due to some underlying nasal pathology such as severe septal deviation, adenoid hypertrophy or uncontrolled allergic rhinitis. This has implications from management point of view. In inactive squamous disease and limited cholesteatoma, nasal pathology should be addressed in the form of medical or surgical management. The number of cases of inactive squamous otitis media were less in our study as the cases with mechanical dysfunction of Eustachian tube on DSVE were first treated for their nasal, paranasal or nasopharyngeal conditions and their retractions responded. Tympanomastoidectomy was offered only when primary sclerotic mastoid pneumatisation pattern was found on CT-Scan with good Eustachian function or in patients who refused for any nasal surgery in spite of Eustachian dysfunction due to septal deviation. The limitation of our study was small sample size of inactive disease. More studies are needed to confirm this.
Conclusion
We conclude that both Eustachian dysfunction and reduced mastoid pneumatisation pattern of primary sclerotic/diploic type can independently result in persistent negative middle ear pressure and lead to the causation of chronic otitis media of squamous type.
When Eustachian dysfunction is found and the disease is in inactive/early stage, we should address the cause of dysfunction first. Cases with primary sclerotic/diploic mastoid pneumatisation pattern but normal Eustachian function mostly require inside–out approach mastoidectomy for disease clearance and ventilation, as the mastoid is found to be contracted.
Compliance with Ethical Standards
Conflict of interest
The authors declares that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Sudhoff H, Tos M. Pathogenesis of attic cholesteatoma: clinical and immunohistochemical support for combination of retraction theory and proliferation theory. Am J Otol. 2000;21(6):786–792. [PubMed] [Google Scholar]
- 2.Sudhoff H, Tos M. Pathogenesis of sinus cholesteatoma. Eur Arch Otorhinolaryngol. 2007;264(10):1137–1143. doi: 10.1007/s00405-007-0340-y. [DOI] [PubMed] [Google Scholar]
- 3.Welkoborsky HJ. Current concepts of the pathogenesis of acquired middle ear cholesteatoma. Laryngorhinootologie. 2011;90(1):38–48. doi: 10.1055/s-0030-1268464. [DOI] [PubMed] [Google Scholar]
- 4.Maniu A, Harabagiu O, Perde Schrepler M, Cătană A, Fănuţă B, Mogoantă CA. Molecular biology of cholesteatoma. Rom J Morphol Embryol. 2014;55(1):7–13. [PubMed] [Google Scholar]
- 5.Sadé J, Fuchs C, Luntz M. The pars flaccida middle ear pressure and mastoid pneumatization index. Acta Otolaryngol. 1996;116(2):284–287. doi: 10.3109/00016489609137842. [DOI] [PubMed] [Google Scholar]
- 6.Iqbal IZ, Watson C. A study of mastoid pneumatisation and the presence of cholesteatoma in 393 patients. J Laryngol Otol. 2016;130(1):66–68. doi: 10.1017/S0022215115003047. [DOI] [PubMed] [Google Scholar]
- 7.Lee DH, Jung MK, Yoo YH, Seo JH. Analysis of unilateral sclerotic temporal bone: How does the sclerosis change the mastoid pneumatization morphologically in the temporal bone? Surg Radiol Anat. 2008;30(3):221–227. doi: 10.1007/s00276-008-0310-0. [DOI] [PubMed] [Google Scholar]
- 8.Jain S, Gupta M, Singh P. Dynamic video endoscopy in Eustachian tube dysfunction: is it better than impedance audiometry. Innov J Med Health Sci. 2016;6(3):88–92. [Google Scholar]
- 9.Gupta M, Jain S, Gaurkar S, Deshmukh PT. Role of dynamic slow motion video endoscopy in etiological correlation between eustachian dysfunction and chronic otitis media: a case-control study. Indian J Otol. 2015;21:19–24. doi: 10.4103/0971-7749.152853. [DOI] [Google Scholar]
- 10.Shatz A, Sadé J. Correlation between mastoid pneumatization and position of the lateral sinus. Ann Otol Rhinol Laryngol. 1990;99(2 Pt 1):142–145. doi: 10.1177/000348949009900213. [DOI] [PubMed] [Google Scholar]
- 11.Toros SZ, Karaca CT, Habeşoğlu TE, Noşeri H, Ertugay CK, Naiboğlu B, Egeli E. Is there a relation between mastoid aeration and Körner’s septum? Eur Arch Otorhinolaryngol. 2010;267(10):1523–1526. doi: 10.1007/s00405-010-1277-0. [DOI] [PubMed] [Google Scholar]
- 12.Sadé J, Fuchs C. Secretory otitis media in adults: II. The role of mastoid pneumatization as a prognostic factor. Ann Otol Rhinol Laryngol. 1997;106(1):37–40. doi: 10.1177/000348949710600107. [DOI] [PubMed] [Google Scholar]


