Abstract
Tympanoplasty is surgical reconstruction of tympano-ossicular system and includes—Canalplasty, Meatoplasty, Myringoplasty and Ossiculoplasty. To analyse and compare the intraoperative and postoperative aspects and the outcomes of conventional postauricular microscopic tympanoplasty and permeatal endoscopic tympanoplasty this study was conducted on 50 patients undergoing type I tympanoplasty (25 patients divided into two groups; group A—microscopic tympanoplasty and group B—endoscopic tympanoplasty). Advantages, disadvantages and results were compared between the two groups. Success rates and hearing improvement were comparable in both groups while intraoperative ease, postoperative morbidity and operative time was seen superior in endoscopic group. Although, endoscopic technique being minimally invasive yet has disadvantages such as single handed difficult instrumentation, frequent cleaning of scope and thus a steep learning curve. In conclusion permeatal endoscopic tympanoplasty can be considered as a good alternative to the conventional microscopic tympanoplasty.
Keywords: Permeatal endoscopic tympanoplasty, Minimally invasive tympanoplasty, Type I tympanoplasty
Introduction
“Chronic otitis media” is any structural change in the middle ear system associated with a permanent defect in the tympanic membrane (TM) [1]. Tympanoplasty is a surgical reconstruction of tympano-ossicular system and includes—Canalplasty, Meatoplasty, Myringoplasty and Ossiculoplasty [2].
Conventional microscopic tympanoplasty with a postauricular incision remains the most effective procedure for patients with chronic otitis media, especially in cases of anterior or large tympanic membrane perforation as well as anterior bony overhang.
Endaural and transcanal approaches are also used during myringoplasty and tympanoplasty. Recently, transcanal endoscopic approach has become quite popular [3]. Minimally invasive otologic surgery has recently been developed along with endoscopic techniques.
Advantages of permeatal endoscopic ear surgery compared to the conventional microscopic surgery include avoiding endaural vertical and postauricular incisions in securing the surgical view. Endoscopically the typical transcanal approach is possible by elevating tympanomeatal flap. This avoids other unnecessary incisions and soft tissue dissections.
The endoscopic approach also provides better visualization of hidden areas in the middle ear cavity including the anterior–posterior epitympanic spaces, sinus tympani, facial recess and hypotympanum.
In this study we evaluated and compared the results in terms of hearing outcome, operative time and graft success rate in patients who underwent either endoscopic or conventional microscopic tympanoplasty. The aim was to find out the clinical benefits of permeatal endoscopic tympanoplasty in comparison to the conventional microscopic surgery by postauricular approach.
Aims and Objectives
To compare the hearing outcomes preoperative, and postoperative at 1, 3 and 6 months.
To compare graft uptake rate, operative time and postoperative morbidity between the two groups.
Methodology
Study Area
The present study was conducted in the Department of Otorhinolaryngology at Sri Aurobindo Institute of Medical Sciences, Indore (M.P.).
Study Design
A prospective, randomized, comparative study.
Time Frame to Address the Study
The study was conducted between November 2015 and August 2017.
Study Population
All patients presenting to the Department of Otorhinolaryngology, Sri Aurobindo Institute of Medical Sciences, Indore (M.P.) with complaints of decreased hearing and ear discharge between the age 18–60 years during the study period formed the study population.
Sample Size
We have included 25 patients per group. The convenient sampling technique was used for the present study.
Grouping
The patients fulfilling all the inclusion criteria and none of the exclusion criteria willing to provide their voluntary consent for participation in the study, were further divided into two groups of 25 patients each using Lottery System.
Group A (n = 25) Patients of this group underwent microscopic tympanoplasty
Group B (n = 25) Patients of this group underwent endoscopic tympanoplasty
Type 1 tympanoplasty using underlay technique was done in all patients.
Inclusion Criteria
Patient presenting with complaints of decreased hearing and ear discharge.
Age group—18–60 years of either gender
Pure conductive hearing loss [< 40 dBHL by (PTA)], irrespective of size of perforation.
Safe COM.
Patient and/or his/her legally acceptable representative willing to provide their voluntary written informed consent form for participation in the study
Exclusion Criteria
Conductive hearing loss (> 40 dBHL).
Age group (< 18 & > 60 years).
Uncooperative patients.
Mixed hearing loss.
Marginal perforation.
Patients unfit for surgery
Cases with recurrence.
Unsafe COM.
Narrow canal
Patient and/or his/her legally acceptable representative not willing to provide their voluntary written informed consent form for participation in the study
Outcome Parameters
The following parameters were evaluated:
Graft take up rate
Audiological improvement
Operative time
Outcome Success End-Point
Successful graft take up was defined as having no residual perforation, atelectasis or lateralisation
In each case, the pre and post operative pure tone audiometry air bone gap (PTA–ABG) was evaluated and pure tone average improvement was noted.
Outcome Failures
Graft failures (residual perforation, lateralisation)
Reperforation
Methodology
After identifying the prospective patients for the study, the study procedures, risks/benefits, type of procedure, anesthesia, grouping, etc. were explained to the patient and/or his/her legally acceptable representative in detail and after obtaining their voluntary written informed consent for participation in the study, the study related procedures were initiated.
In all the patients, history and clinical ENT and head and neck examination was done including tuning fork tests, X-ray mastoid and PTA. Antibiotics were given prior to admission to dry the ear, if discharging. Ear was kept dry for at least 6 weeks. Examination under microscope was done in each case. Any septic foci in nose or throat were treated. In all the patients it was confirmed that the Eustachian tube function was normal. Preoperatively pure tone audiometry was done in each patient and patient with pure conductive hearing loss < 40 dBHL was selected irrespective of size of perforation. All routine investigations were done. Then all the patients were subjected to type I tympanoplasty in local anaesthesia or general anaesthesia.
Microscopic Tympanoplasty
In tympanoplasty performed via a postauricular approach with microscope, firstly local infilteration was done with lignocaine 2% with adrenaline in post auricular region and all four quadrants of ear. Painting and draping done. In all cases post aural (William Wilde’s) incision was given.
Postauricular incision was made approximately 1 cm behind the postauricular crease. A large temporalis fascia graft (or tragal cartilage/perichondrium) was harvested, cleaned of residual muscle, and placed on a ceramic block to allow drying. A T-shaped incision is made in the periosteum overlying the mastoid. The periosteum was elevated and moved anteriorly into the ear canal. The canal skin and periosteum was elevated using a duckbill elevator or round knife. A self-retaining retractor was placed to retract the canal skin and the ear forward. The canal incision is designed to create a laterally based canal skin flap or vascular strip. The horizontal incision is cut first approximately 2–5 mm lateral to the annulus from the 12 to the 8 O’clock position (right ear). The vertical incisions were made next. The margins of the perforations were refreshed. The undersurface of the tympanic membrane was then abraded with a round knife to increase adhesion to the graft. A tympanomeatal flap was then elevated anteriorly. The status of the middle ear was then inspected for disease. The ossicles were gently manipulated with a Rosen needle to evaluate for mobility. The round window reflex was inspected at this time. The eustachian tube and middle ear were then packed with Gelfoam. The fascia graft (or tragal cartilage/perichondrium) was shaped to the proper size needed for the perforation. It was then carefully tucked into position under the anterior tympanic membrane remnant and onto the posterior canal wall. The annulus was placed back into position posteriorly and the vascular strip carefully moved into its anatomic place. Antibiotic soaked Gelfoam was placed over the drum remnant, graft, and vascular strip and the external canal. The postauricular incision was closed subcutaneously with absorbable suture and steri-strips or staples were applied to the skin. A mastoid dressing was placed to provide light pressure and protection.
Endoscopic Tympanoplasty
In endoscopic tympanoplasty rigid endoscope of 4 mm in diameter, 0° and 18 cm in length was used. The ear canal was cleaned and inspected. First, the perforation and status of middle ear mucosa were examined. Local anesthetic, including epinephrine at a concentration of 1/100,000, was injected into the four quadrants of the outer ear canal. Tara bichi sutures were applied to pinna. The margins of the perforations were refreshed. The undersurface of the tympanic membrane was then abraded with a round knife to increase adhesion to the graft. A tympanomeatal flap was then elevated anteriorly. The status of the middle ear was then inspected for disease (Fig. 1). The ossicles were gently manipulated with a Rosen needle to evaluate for mobility. The round window reflex was inspected at this time. The eustachian tube and middle ear was then packed with Gelfoam. The tragal cartilage graft and perichondrium was harvested. It was then carefully tucked into position under the anterior tympanic membrane remnant and onto the posterior canal wall. The annulus was placed back into position posteriorly and the vascular strip was carefully moved into its anatomic place. Antibiotic soaked Gelfoam was placed over the drum remnant, graft, and vascular strip and the external canal. Tragal sutures applied. A small dressing was applied.
Fig. 1.

Microcopic intraoperative view of middle ear
Postoperative Management
In microscopic tympanoplasty, mastoid dressing was done immediately after operation and kept for 7 days postoperatively. Patient was kept on intravenous antibiotic for 2 days after which he/she is discharged on oral antibiotics.
In endoscopic tympanoplasty a small dressing was applied over canal removed after 7 days. Patient was discharged the same day or next day on oral antibiotics.
In both the groups, patient was called on seventh postoperative day for suture removal. After dressing removal, topical antibiotics drops were prescribed for 15 days.
Follow-Up
Follow up was done after one month, third month and sixth month from the day of operation. Patient was asked for subjective improvement in hearing which was done using pure tone audiometry (PTA) and air–bone gap (ABG) and any postoperative complications were watched carefully. The audiometric evaluation was done at 1 month, 3 months and 6 months in every patient irrespective of graft take-up (Fig. 2).
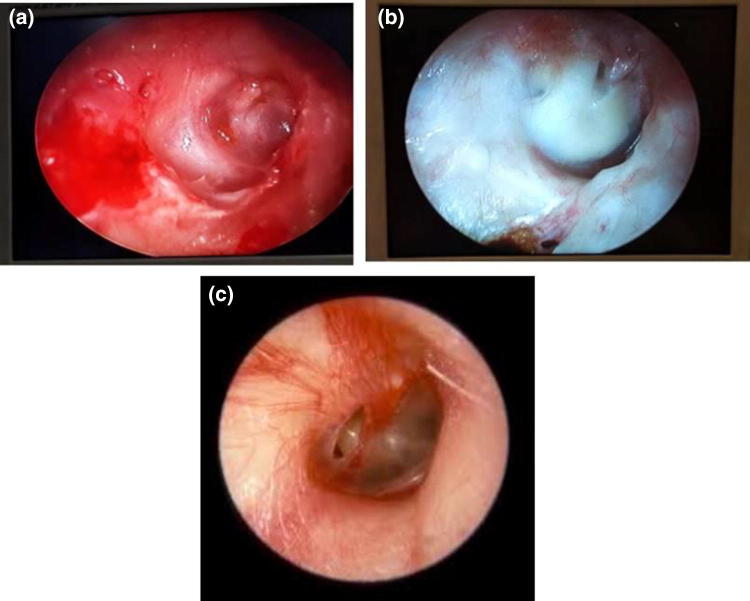
Fig. 2.
Post operative (follow-up) pictures of tympanic membrane; a microscopic, b endoscopic, c residual perforation
Data Collection Method
The data was collected in the customized proforma designed for the study purpose.
Statistical Analysis
The data was initially entered into the customized proforma and then transferred to Microsoft Excel for analysis. Online statistical software were used for calculating the p values. Comparison of mean between the two groups was done using unpaired ‘t’ test. A p value of < 0.05 was taken as statistically significant.
Financial Inputs and Funding
Both the procedures are routinely conducted in our institute. All the charges for the surgical procedure and management of the condition were borne by the patients as per the norms laid down by the institution. But no additional tests/procedures/investigations were done for the specific purpose of the study. Hence, there was no financial implications either on the patient or the institution. Also, all the study related expenses were borne by the investigator herself. This study was neither funded nor sponsored by institution or company.
Ethical Considerations
The protocol of the study was initially submitted to the Ethics Committee of our institute. After getting their approval for the study, the study was initiated in the institution. Also before enrolling any patient into the study, a written voluntary informed consent was taken from the patient and/or his/her legally acceptable representative for participation in the study. This consent was in addition to the regular consents obtained for the surgical management of the condition as per the norms laid down by the institution.
Results and discussion
There were 48% males and 52% females in the microscopic approach group, while there were 52% males and 48% females in the endoscopic approach group. In microscopic approach group, it was observed that in 22 patients (88%), graft uptake is good while in 3 patients (12%) residual perforation was present. In permeatal endoscopic approach group, it was observed that in 21 patients (84%), graft uptake was good while in 4 patients (16%) residual perforation was present. There was residual perforation in 12% cases in microscopic versus 16% in endoscopic approach groups which was statistically not significant (Chi square value = 0.166, p = 0.684) (Table 1). This result is similar to that of study by Raj and Meher [4] where the rate of graft survival was 90% in patients undergoing endoscopic myringoplasty, and 85% in those undergoing microscopic myringoplasty.
Table 1.
Distribution of postoperative condition of tympanic membrane: I (intact) P (perforation)
| Condition of tympanic membrane | Group A | Group B | ||
|---|---|---|---|---|
| No. | % | No. | % | |
| Intact | 22 | 88.0 | 21 | 84.0 |
| Perforation | 3 | 12.0 | 4 | 16.0 |
| Total | 25 | 100.0 | 25 | 100.0 |
The comparison of pure tone audiometry between the microscopic approach group and endoscopic approach group at preoperative, 1 month postoperative, 3 months postoperative and 6 months postoperative was found to be statistically not significant (preoperative p = 0.520; 1 month postoperative p = 0.787, 3 months postoperative p = 0.610 and 6 months postoperative p = 0.783), showing a comparable findings between the two groups. The improvement in pure tone audiometry between the two groups was found to be statistically comparable (9.46 ± 5.41 in microscopic approach group vs. 8.29 ± 5.37 in endoscopic approach group), p = 0.446 (Table 2).
Table 2.
Comparison of pure tone audiometry between the two groups
| Group A (Mean ± SD) (dBHL) | Group B (Mean ± SD) (dBHL) | ‘t’ value | p value | |
|---|---|---|---|---|
| Preoperative | 32.33 ± 4.44 | 31.56 ± 3.97 | 0.65 | 0.520, NS |
| 1 month postoperative | 23.68 ± 4.21 | 23.36 ± 4.14 | 0.27 | 0.787, NS |
| 3 months postoperative | 23.34 ± 4.72 | 24.00 ± 4.26 | 0.51 | 0.610, NS |
| 6 months postoperative | 22.86 ± 5.15 | 23.26 ± 5.07 | 0.28 | 0.783, NS |
Similarly the comparison of air–bone gap between the microscopic approach group and endoscopic approach group at preoperative, 1 month postoperative, 3 months postoperative and 6 months postoperative was found to be statistically not significant (preoperative p = 0.216; 1 month postoperative p = 0.987, 3 months postoperative p = 0.733 and 6 months postoperative p = 0.643), showing a comparable findings between the two groups. The improvement in air–bone gap between the two groups was found to be statistically comparable (6.51 ± 2.65 in microscopic approach group vs. 6.09 ± 4.10 in endoscopic approach group), p = 0.673 (Table 3).
Table 3.
Comparison of ABG between the two groups
| Group A (Mean ± SD) (dBHL) | Group B (Mean ± SD) (dBHL) | ‘t’ value | p value | |
|---|---|---|---|---|
| Preoperative | 15.96 ± 1.89 | 16.62 ± 1.81 | 1.26 | 0.216, NS |
| 1 month postoperative | 10.00 ± 2.93 | 9.98 ± 2.69 | 0.02 | 0.987, NS |
| 3 months postoperative | 9.52 ± 2.79 | 9.80 ± 2.98 | 0.34 | 0.733, NS |
| 6 months postoperative | 9.45 ± 2.82 | 9.86 ± 3.43 | 0.47 | 0.643, NS |
The mean operative time was higher in microscopic approach in comparison to the endoscopic approach group (83.8 ± 22.7 min vs. 63.2 ± 13.6 min), which was statistically significant (t value = − 3.90, p = 0.000) (Table 4) as in the study of Ghaffar et al. [5] where mean operation time was found to be 62.85 min in patients undergoing endoscopic tympanoplasty.
Table 4.
Distribution of patients according to operative time
| Operative time (min) | Group A | Group B | ||
|---|---|---|---|---|
| No. | % | No. | % | |
| 31–60 min | 6 | 24.0 | 13 | 52.0 |
| 61–90 min | 8 | 32.0 | 12 | 48.0 |
| 61–90 min | 11 | 44.0 | 0 | 0.0 |
| Total | 25 | 100.0 | 25 | 100.0 |
The mean postoperative hospital stay in microscopic approach group was 2.96 ± 0.93 days while in endoscopic approach group was 1.24 ± 0.43 days, which was significantly higher in the microscopic approach group (p < 0.001) (Table 5). Patel et al. also reported lower hospital stay in endoscopic tympanoplasty [2].
Table 5.
Distribution of patients according to postoperative hospital stay
| Postoperative hospital stay (days) | Group A | Group B | ||
|---|---|---|---|---|
| No. | % | No. | % | |
| 1 day | 0 | 0.0 | 19 | 76.0 |
| 2 days | 4 | 16.0 | 6 | 24.0 |
| 3 days | 18 | 72.0 | 0 | 0.0 |
| 4 days | 3 | 12.0 | 0 | 0.0 |
| Total | 25 | 100.0 | 25 | 100.0 |
In a study Huang et al. [6] performed type 1 tympanoplasty in 50 patients by microscopic approach and in another 50 patients by endoscopic approach. Similar hearing recovery and rate of perforation closure were found between the two patient groups.
Similarly in the study of Patel et al. [7], mean time of endoscopic and microscopic tympanoplasty operations was found to be 75 min and 90 min, respectively. They reported very similar graft success rates in patients undergoing endoscopic and microscopic tympanoplasty.
In microscopic approach group, the preoperative mean air bone gap (PTA–ABGs) significantly declined 6 months postoperatively from 15.96 ± 1.89 dBHL to 9.45 ± 2.80 dBHL while in endoscopic approach group from 16.62 ± 1.81 dBHL to 9.86 ± 3.43 dBHL (Table 3). The mean improvement in air bone gap (PTA–ABGs) in microscopic group is 6.51 ± 2.65 dBHL while in endoscopic group it is 6.09 ± 4.10. In microscopic approach group, the preoperative mean hearing loss (PTA) significantly declined 6 months postoperatively from 32.33 ± 4.44 dBHL to 22.86 ± 5.15 dBHL and in endoscopic approach group from 31.56 ± 3.97 dBHL to 23.26 ± 5.07 dB (Table 2). The mean improvement in hearing loss in microscopic group is 9.46 ± 5.41 dBHL while in endoscopic group it is 8.29 ± 5.37 dBHL. In microscopic approach group the mean operative time is found 83.8 ± 22.7 min while in endoscopic group it is 63.2 ± 13.6 min (Table 4).
Thus, the postoperative hearing improvement and the success rate are comparable in two groups but operative time and morbidity (size of the dressing and postoperative hospital stay) also the cosmetic outcome are inferior in microscopic than endoscopic group.
Conclusion
We found that endoscopic and microscopic tympanoplasty have similar degree of graft uptake and hearing improvement. Whereas, less postoperative morbidity, shorter operation time, better view of middle ear intraoperatively and better cosmesis is seen with permeatal endoscopic technique. But, endoscopic technique has its disadvantages such as single handed difficult instrumentation, frequent cleaning of scope and thus a steep learning curve. Thus we conclude that endoscopic tympanoplasty can be considered as a good alternative to the conventional postaural microscopic tympanoplasty.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bedajit RK, Mallik P, Kumar P, Devi HP, Sudhiranjan T, Singh OP, et al. Endoscopic transcanal mastoidectomy with tympanoplasty. Natl J Otorhinolaryngol Head Neck Surg. 2015;3(2):10–11. [Google Scholar]
- 2.Patel J, Aiyer RG, Gajjar Y, Gupta R, Raval J, Suthar PP. Endoscopic tympanoplasty versus microscopic tympanoplasty in tubotympanic CSOM: a comparative study of 44 cases. Int J Res Med Sci. 2015;3(8):1953–1957. doi: 10.18203/2320-6012.ijrms20150307. [DOI] [Google Scholar]
- 3.Akyigit A, Sakallioglu O, Karlidag T. Endoscopic tympanoplasty. J Otol. 2017;12(2):62–67. doi: 10.1016/j.joto.2017.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raj A, Meher R. Endoscopic transcanal myringoplasty E A study. Indian J Otolaryngol Head Neck Surg. 2001;53(1):47–49. doi: 10.1007/BF02910979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghaffar S, Ikram M, Zia S, Raza A. Incorporating the endoscopeinto middle ear surgery. Ear Nose Throat J. 2006;85:593–596. doi: 10.1177/014556130608500911. [DOI] [PubMed] [Google Scholar]
- 6.Huang T-Y, Ho K-Y, Wang L-F, Chien C-Y, Wang H-M. A comparative study of endoscopic and microscopic approach type 1 tympanoplasty for simple Chronic Otitis media. J Inter Adv Otol. 2016;12(1):28–31. doi: 10.5152/iao.2015.1011. [DOI] [PubMed] [Google Scholar]
- 7.Patel J, Aiyer RG, Gajjar Y, Gupta R, Raval J, Suthar PP. Endoscopic tympanoplasty vs microscopic tympanoplasty In tubotympaniccsom: a comparative study of 44 cases. Int J Res Med Sci. 2015;3(8):1953–1957. doi: 10.18203/2320-6012.ijrms20150307. [DOI] [Google Scholar]