Abstract
Objective:
To describe national, state-specific, and sociodemographic trends in diagnoses of depressive disorders recorded during delivery hospitalizations.
Methods:
Data were analyzed from the National Inpatient Sample (2000–2015) and 31 publically available State Inpatient Databases (2000–2015) of the Healthcare Cost and Utilization Project. Delivery Hospitalizations were identified by using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic and procedure codes for obstetric delivery. Depressive disorders were identified from ICD-9-CM diagnoses codes classified as depressive disorders in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (291.89, 292.84, 293.83, 296.2–296.26, 296.3–296.36, 300.4, and 311). Prevalence rates and average annual rate change were calculated nationally and across 28 states with at least 3 years of data and age, payer source, and race or ethnicity.
Results:
The U.S. rate of depressive disorders recorded during delivery hospitalizations increased from 4.1 diagnoses per 1,000 hospitalizations in 2000 to 28.7 in 2015. Rates significantly increased in 27 of the 28 states. Recent (2014–2015) rates were lowest in Hawaii and Nevada (<14/1,000) and highest in Vermont, Minnesota, Oregon, and Wisconsin (>49/1,000). Rates in 2015 were highest among those aged 35 years or older, public insurance recipients, and non-Hispanic white women (>31/1,000). The highest annual rate increases were in Vermont and Maine (≥3.8/1,000). Non-Hispanic white women, those ≥ 35 years of age, and public insurance recipients showed the highest annual rate increases during 2000–2015 (≥1.7 per 1,000).
Conclusion:
During 2000–2015, rates of depressive disorders recorded during delivery hospitalizations increased nationally, in 27 states with available data, and across all sociodemographic categories.
Precis
From 2000–2015, rates of depressive disorders recorded during delivery hospitalizations increased nationally across age, insurance, and race or ethnicity categories.
Introduction
Depression is one of the most common disorders during pregnancy and the postpartum period, with a prevalence ranging from 8.5%–12.9%.1,2 Depression during pregnancy is associated with an increased risk of poor maternal self-care, inadequate nutrition,3 obstetric complications,4–6 preterm labor,4,6,7 substance use,8 lower initiation and duration of breastfeeding,9 poor maternal-fetal attachment,10 and postpartum and chronic depression.11 Maternal depression can affect a child’s mental and motor development, temperament, self-regulation, self-esteem, and behavior;12 these detrimental effects can last into adolescence.13,14 In extreme cases, depression during pregnancy and the postpartum period can contribute to maternal mortality.15
There is growing recognition that maternal mental health is an important issue. The 21st Century Cures Act of 2016 authorized appropriations for federal grants to establish, expand, or maintain culturally competent state-based programs to screen and treat women who are pregnant or postpartum with depression.16 Given this recent focus, it is important to establish a baseline trend of depressive disorder diagnoses amongst pregnant women, prior to this legislation. Whether U.S. rates of depressive disorders recorded during delivery hospitalization have changed over time, or whether they vary by state or sociodemographic characteristics, has not been documented previously. Of population-based studies examining race or ethnicity and self-report depressive symptoms during pregnancy, results are inconclusive.17,18 Thus, we aim to describe U.S. rates of depressive disorders recorded during delivery hospitalizations, and also how patterns differ by state and socioeconomic factors, such as age, race or ethnicity, and type of insurance, from 2000 to 2015.
Methods
Data were analyzed from the National Inpatient Sample (2000–2015) and the State Inpatient Databases (2000–2015) of the Healthcare Cost and Utilization Project, Agency for Healthcare Research and Quality from 2000 through the third quarter of 2015.19 The fourth quarter of 2015 is excluded because of the transition to the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) Codes. The Healthcare Cost and Utilization Project contains the largest collection of longitudinal hospital care data derived from administrative data. The database includes all listed diagnoses and procedures, discharge status, patient demographics, and charges for all patients, regardless of payer. These data are frequently used to document mental health diagnoses20,21 and have undergone quality control measures.19 The National Inpatient Sample was used for all national analyses, including those by sociodemographic factors. This dataset approximates a 20% stratified sample of all patients discharged from U.S. community hospitals. Survey-specific analysis techniques were used to account for clustering, stratification, and weighting, making the National Inpatient Sample nationally representative. The State Inpatient Databases were used for all state-specific analyses. This dataset includes census data from states that agree to release public use data, which includes 31 states in this analysis. No survey-specific analysis techniques are required when using the State Inpatient Databases.
The analytical sample of interest, delivery hospitalizations, was identified from the 2000–2015 data files by using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic and procedure codes pertaining to obstetric delivery.22 The outcome of interest, depressive disorder, was identified from ICD-9-CM diagnoses codes classified as depressive disorders in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (Substance or Medication-Induced Depressive Disorder: 291.89, 292.84, Depressive Disorder Due to Another Medical Condition: 293.83, Major Depressive Disorder, single or recurrent episode: 296.2–296.26, 296.3–296.36, Persistent Depressive Disorder [Dysthymia]: 300.4, and Other Specified or Unspecified Depressive Disorder: 311). Premenstrual Dysphoric Disorder (625.4) was not included given our sample of interest, delivery hospitalizations.23 Given the nature of hospital discharge data, we were unable to identify what screening methods or assessments were used to identify these depressive disorders. Other covariates of interest were sociodemographic factors like age, payer source, and race or ethnicity. For payer source, ‘public’ includes Medicaid and Medicare, although Medicare recipients made up less than 2% of this category, and ‘other’ includes Worker’s Compensation, Tricare, Title V, and other government programs.19
National and state-specific prevalence rates and 95% confidence intervals of depressive disorders recorded per 1,000 delivery hospitalizations during 2000–2015 were calculated for each year nationally and across sociodemographic factors (age, payer source, and race or ethnicity) and states. Joinpoint version 4.6 was used to select linear models, by way of permutation tests, to determine the average annual rate change over the study period. For this analysis, we did not allow for any joinpoints, or change in trends, between years. Average annual rate changes were only calculated for the 27 states with at least 3 years of data and significant linear trends. A statistically significant change indicates that the annual rate change is different from zero, or that the trend is significantly decreasing or increasing over time. Joinpoint was also used to perform pairwise comparisons to determine whether trends significantly differed across categories of each sociodemographic factor. P-values less than 0.05 were considered statistically significant. Institutional Review Board approval was not needed as this analysis was not considered human subjects research because of the use of publically available de-identified data.
Results
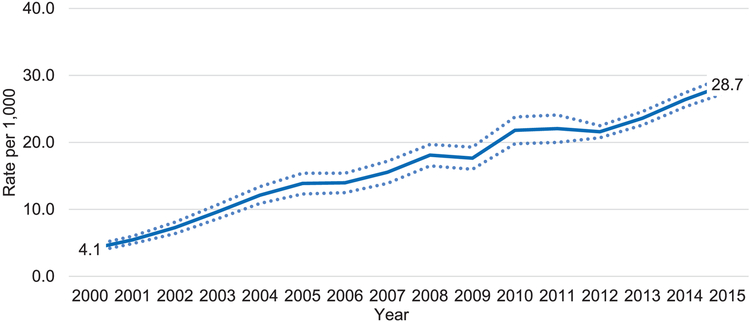
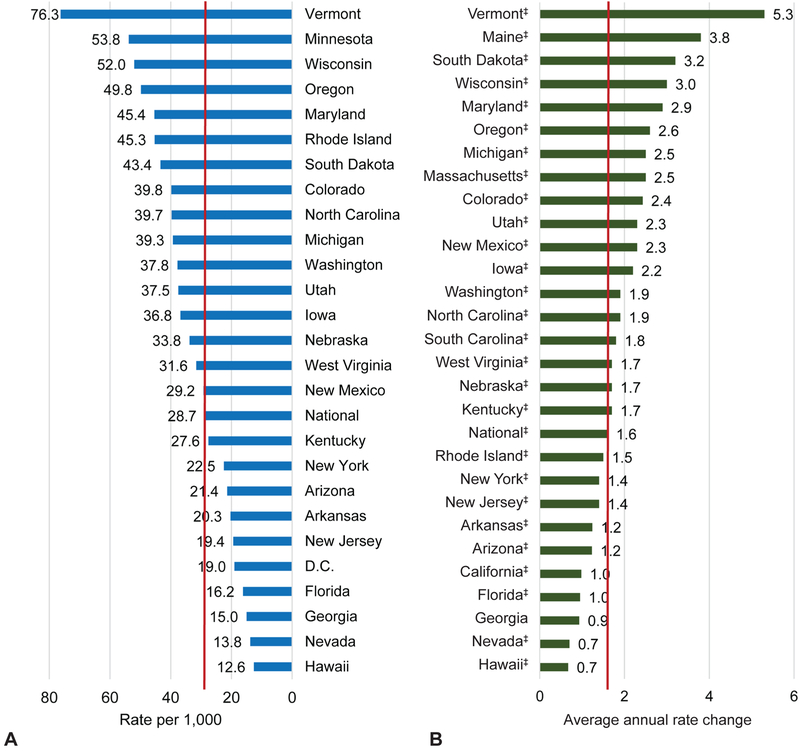
Analyses using the National Inpatient Sample revealed that U.S. rates of depressive disorders recorded during delivery hospitalizations increased from 4.1 diagnoses per 1,000 delivery hospitalizations in 2000 to 28.7 in 2015 (Figure 1; Table 1). This represents a 7-fold increase in the rate and an average rate increase of 1.6/1,000 each year during 2000 to 2015. State-specific analyses using the State Inpatient Databases revealed that rates of depressive disorders recorded during delivery hospitalizations varied by state (Table 2; Appendix 1 [Appendix 1 is available online at http://links.lww.com/xxx]); 2014–2015 diagnosis rates were lowest in Hawaii and Nevada (<14/1,000) and highest in Vermont, Minnesota, Wisconsin, and Oregon (>49/1,000). During the study period, there were significant increases in the rate of depressive disorders recorded during delivery hospitalizations for 27 of the 28 states with at least 3 years of data. Georgia was the only state where a linear trend was not significantly fit for the data (P = 0.4). Rates increased the slowest in Hawaii and Nevada with average increases of 0.7/1,000 each year. Rates increased the fastest in Vermont and Maine, both of which showed average increases of at least 3.8/1,000 each year (Figure 2).
Figure 1.
U.S. national prevalence rate* and 95% confidence interval† of depressive disorders recorded per 1,000 hospitalizations Nationwide Inpatient Sample, Healthcare Cost and Utilization Project, 2000–−2015.‡ The solid blue line represents the prevalence rate and the dotted blue lines represent the 95% confidence intervals. *Prevalence rate numerator consisted of depressive disorder International Classification of Diseases-9-Clinical Modification codes (291.89, 292.84, 293.83, 296.2–296.26, 296.3–296.36, 300.4, and 311), prevalence rate denominator consisted of delivery hospitalization discharges. †Confidence intervals are based on unweighted data. ‡Rates are for 2000 through the third quarter of 2015.
Table 1.
National Case Counts and 95% Confidence Intervals (CI) of Depressive Disorders* Recorded at Delivery Hospitalization by Year; National Inpatient Database, Healthcare Cost and Utilization Project, 2000–2015
| Year | N (95% CI) |
|---|---|
| 2000 | 16,055 (14,150 – 18,081) |
| 2001 | 20,999 (18,843 – 23,073) |
| 2002 | 29,045 (25,488 – 32,258) |
| 2003 | 37,919 (33,804 – 42,058) |
| 2004 | 49,496 (44,493 – 54,698) |
| 2005 | 56,306 (49,893 – 62,468) |
| 2006 | 57,731 (51,626 – 63,603) |
| 2007 | 68,080 (60,847 – 75,293) |
| 2008 | 73,349 (66,858 – 79,825) |
| 2009 | 69,650 (63,113 – 76,131) |
| 2010 | 81,063 (73,613 – 88,485) |
| 2011 | 81,044 (73,466 – 88,526) |
| 2012 | 81,360 (77,964 – 84,743) |
| 2013 | 88,375 (84,564 – 92,048) |
| 2014 | 100,290 (96,182 – 104,165) |
| 2015† | 82,086 (78,654 – 85,518) |
Consists of depressive disorder ICD-9-CM codes (291.89, 292.84, 293.83, 296.2–296.26, 296.3–296.36, 300.4, and 311)
Case counts are only for the first three quarters of 2015 and are not representative of the entire year
Table 2.
Case Counts of Depressive Disorders* Recorded at Delivery Hospitalizations, by State and Year; State Inpatient Databases, Healthcare Cost and Utilization Project, 2000–2015
| State | 00 | 01 | 02 | 03 | 04 | 05 | 06 | 07 | 08 | 09 | 10 | 11 | 12 | 13 | 14 | 15† |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Arizona | 218 | 324 | 495 | 686 | 887 | 962 | 1,067 | 1,058 | 1,236 | 1,225 | 1,333 | 1,436 | 1,440 | 1,564 | 1,676 | 1,299 |
| Arkansas | --- | --- | --- | --- | 204 | 316 | 449 | 404 | 372 | 522 | 505 | 516 | 549 | 650 | 740 | --- |
| California | 1,187 | 1,613 | --- | 2,748 | 3,463 | 4,037 | 4,241 | 4,757 | 5,058 | 5,400 | 6,171 | 6,817 | --- | --- | --- | --- |
| Colorado | 307 | 553 | 825 | 976 | 1,245 | 1,444 | 1,582 | 1,706 | 1,930 | 2,033 | 2,092 | 2,242 | 1,940 | 2,092 | 2,321 | 1,891 |
| D.C. | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | 233 | 268 | --- |
| Florida | 559 | 845 | 1,110 | 1,438 | 1,926 | 2,052 | 2,352 | 2,479 | 2,642 | 2,742 | 2,815 | 2,874 | 2,807 | 2,943 | 3,422 | --- |
| Georgia | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | 1,658 | 1,594 | 1,893 | --- |
| Hawaii | 43 | 61 | 62 | 106 | 109 | 105 | 140 | 98 | 148 | 166 | 172 | 211 | 149 | 198 | 191 | --- |
| Iowa | 194 | 202 | 324 | 456 | 631 | 652 | 688 | 846 | 829 | 928 | 967 | 1,136 | 1,080 | 1,236 | 1,295 | 1,058 |
| Kentucky | 165 | 218 | 306 | 459 | 588 | 620 | 651 | 660 | 812 | 1,041 | 1,094 | 1,160 | 1,220 | 1,260 | 1,390 | 1,064 |
| Maine | 198 | 272 | 360 | 543 | --- | --- | 576 | 685 | 709 | 763 | 692 | 647 | 690 | --- | --- | --- |
| Maryland | 352 | 559 | 816 | 992 | 1,380 | 1,624 | 1,961 | 2,158 | 2,216 | 2,295 | 2,554 | 2,617 | 2,662 | 2,735 | 3,060 | --- |
| Massachusetts | 772 | 909 | 1,200 | 1,454 | 1,649 | 1,765 | 1,956 | 2,185 | 2,088 | 2,360 | 2,603 | 2,856 | 2,661 | 2,822 | --- | --- |
| Michigan | 636 | 772 | 1,148 | 1,387 | 1,825 | 2,404 | 2,615 | 2,710 | 2,982 | 3,154 | 3,233 | 3,388 | 3,352 | 3,928 | 4,333 | --- |
| Minnesota | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | 3,398 | 2,695 |
| Mississippi | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | 301 | 316 | --- | --- | --- | --- |
| Nebraska | --- | 134 | 218 | 337 | 293 | 293 | 361 | 418 | 527 | 597 | 605 | 648 | 553 | 726 | 775 | 657 |
| Nevada | --- | --- | 72 | 116 | 164 | 173 | 211 | 226 | 238 | 255 | 262 | 304 | 290 | 279 | 465 | --- |
| New Jersey | 340 | 385 | 562 | 746 | 897 | 1,023 | 1,249 | 1,746 | 2,051 | 1,815 | 1,887 | 1,752 | 1,605 | 1,821 | 1,917 | --- |
| New Mexico | --- | --- | --- | --- | --- | --- | --- | --- | 416 | 501 | 518 | 640 | 618 | 635 | 669 | --- |
| New York | 873 | 1,122 | 1,548 | 2,054 | 2,444 | 2,743 | 3,104 | 3,287 | 3,790 | 3,820 | 4,356 | 4,708 | 4,488 | 4,572 | 5,154 | --- |
| North Carolina | 503 | 707 | 1,009 | 1,432 | 1,736 | 1,883 | 2,181 | 2,152 | 2,284 | 2,462 | 2,589 | 2,716 | 2,802 | 3,223 | 4,061 | 3,385 |
| Oregon | 336 | 525 | 666 | 730 | 875 | 944 | 987 | 1,124 | 1,335 | 1,372 | 1,487 | 1,569 | 1,661 | 1,706 | 2,120 | --- |
| Rhode Island | --- | --- | 338 | 338 | 403 | 453 | 415 | 432 | 431 | 378 | 437 | 564 | 466 | 431 | 503 | --- |
| South Carolina | 183 | 235 | 360 | 495 | 595 | 630 | 674 | 733 | 968 | 1,138 | 1,358 | 1,395 | 1,361 | 1,469 | --- | --- |
| South Dakota | --- | --- | --- | --- | --- | --- | --- | 237 | 245 | 330 | 324 | 368 | 394 | 451 | 509 | --- |
| Utah | 234 | 348 | 567 | 716 | 883 | 876 | 932 | 1,114 | 1,346 | 1,578 | 1,503 | 1,595 | 1,555 | 1,798 | 1,856 | --- |
| Vermont | --- | 52 | 51 | 69 | 111 | 156 | 186 | 290 | 249 | 265 | 313 | 277 | 301 | 400 | 421 | --- |
| Washington | 436 | 534 | 724 | 879 | 1,007 | 1,018 | 1,198 | 1,296 | 1,507 | 1,816 | 1,885 | 2,001 | 2,046 | 2,456 | 3,006 | --- |
| West Virginia | 101 | 151 | 175 | 233 | 272 | 340 | 406 | 452 | 403 | 439 | 456 | 418 | 544 | 591 | 631 | --- |
| Wisconsin | 505 | 650 | 862 | 1,258 | 1,566 | 1,759 | 1,998 | 2,257 | 2,325 | 2,396 | 2,613 | 2,709 | 2,517 | 2,755 | 3,147 | 2,501 |
--- Data not available
Consists of depressive disorder ICD-9-CM codes (291.89, 292.84, 293.83, 296.2–296.26, 296.3–296.36, 300.4, and 311)
Case counts shown are only for the first three quarters of 2015 and are not representative of the entire year
Figure 2.
A state-specific comparison of depressive disorders recorded per 1,000 delivery hospitalizations: (A) prevalence rate*, 2014–2015† and (B) average annual rate change, 2000–2015. Data from state inpatient databases, Healthcare Cost and Utilization Project. Red line notes national value. *Prevalence rate numerator consisted of depressive disorder International Classification of Diseases-9-Clinical Modification codes (291.89, 292.84, 293.83, 296.2–296.26, 296.3–296.36, 300.4, and 311), prevalence rate denominator consisted of delivery hospitalization discharges. †Rates for Arizona, Colorado, Iowa, Kentucky, Minnesota, Nebraska, North Carolina, and Wisconsin are 2015, the remainder are 2014. ‡Significant at P<.05.
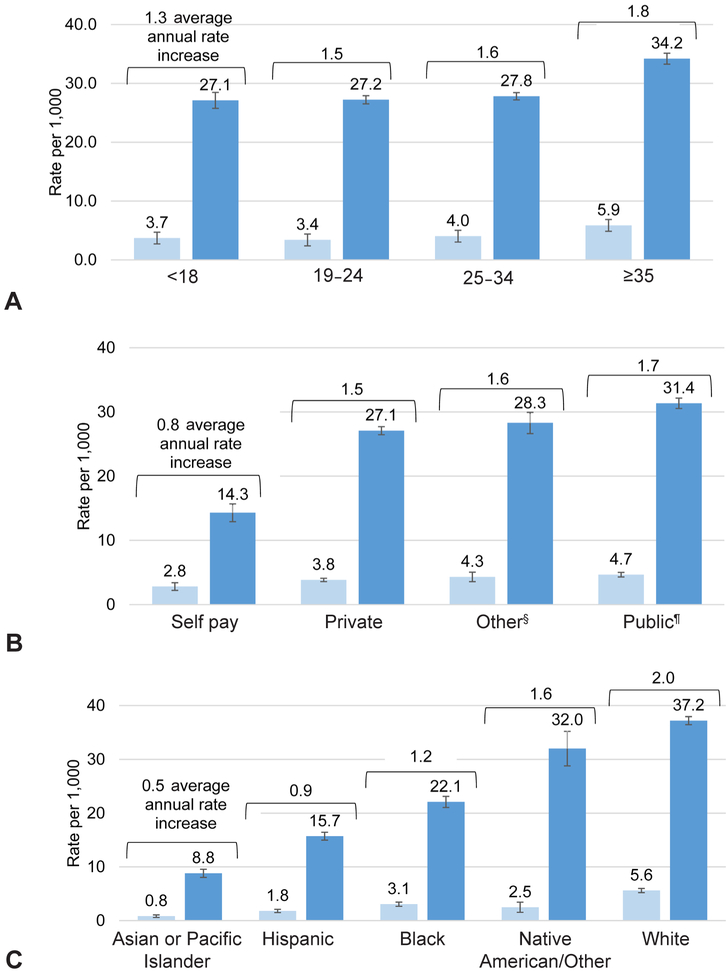
Additional analyses using the National Inpatient Sample revealed that rates of depressive disorders recorded during delivery hospitalizations varied across age, payer source, and race or ethnicity, but increased significantly among all groups. Rates in 2000 ranged from 3.4 per 1,000 among women aged 19–24 years to 5.9 among women aged 35 years or older. Rates in 2015 ranged from 27.1 per 1,000 among women aged 18 years or younger to 34.2 among women aged 35 years or older (Figure 3). Rates increased the fastest during 2000–2015 among women aged 35 years and older (1.8/1,000 per year), and pairwise comparisons showed that the annual rate increases were significantly different amongst all age groups (P’s < 0.05). Rates in 2000 ranged from 2.8 per 1,000 among self-paying women to 4.7 among publicly insured deliveries. Rates in 2015 ranged from 14.3 per 1,000 among self-paying women to 31.4 among publically insured deliveries (Figure 3). Rates increased the fastest during 2000–2015 among publically insured deliveries (1.7/1,000 per year), and pairwise comparisons showed that the annual rate increases were significantly different between public and private and between self-pay and all other groups (P’s <0.05; Figure 3). By race or ethnicity, rates in 2000 ranged from 0.8 per 1,000 among Asian or Pacific Islander women to 5.6 among non-Hispanic white women. Rates in 2015 ranged from 8.8 per 1,000 among Asian or Pacific Islander women to 37.2 among non-Hispanic white women (Figure 3). Rates increased the fastest over time among non-Hispanic white women (2.0/1,000 per year), and pairwise comparisons showed that the annual rate increases were significantly different amongst all race and ethnicity groups. (P’s <0.05; Figure 3).
Figure 3.
Prevalence rates,* 95% confidence intervals,† and average annual percent change in the rate of depressive disorders recorded during delivery hospitalizations by sociodemographic characteristics: (A) age at admission, (B) payer source, and (C) race–ethnicity. Data from the Nationwide Inpatient Sample, Healthcare Cost and Utilization Project, 2000–2015.‡ Light blue bars indicate the year 2000; dark blue bars indicate the year 2015. *Prevalence rate numerator consisted of depressive disorder ICD-9-CM codes (291.89, 292.84, 293.83, 296.2–296.26, 296.3–296.36, 300.4, and 311), prevalence rate denominator consisted of delivery hospitalization discharges. †Confidence intervals are based off of unweighted data. ‡Rates are for 2000 through the third quarter of 2015. §Includes Worker’s Compensation, Tricare, Title V, and other government programs. ¶Includes Medicaid and Medicare (<2%).
Discussion
Results from this report show that national rates of depressive disorders recorded during delivery hospitalizations increased significantly from 4.1 per 1,000 hospitalizations in 2000 to 28.7 in 2015, an average increase of 1.6 diagnoses per 1,000 each year. The most recent systematic reviews estimating the national prevalence of depression during pregnancy date back to 2005;1,2 the current report provides the most updated estimates available for depressive disorder recorded at delivery hospitalization. Among the 28 states with at least 3 years of data, 27 showed significant increases in rates of depressive disorders recorded during delivery hospitalizations during 2000–2015. Recent rates (2015) were highest in deliveries to women identified as 35 years or older, publically insured, and non-Hispanic white. Consistent with the literature,18 women receiving public insurance during pregnancy showed the highest rates of depression diagnoses at delivery. This finding is also consistent with the United States Preventive Services Task Force’s acknowledgement of lower socioeconomic status as a risk factor for depression.24 Because screening and diagnosing practices may differ by sociodemographic factors, differences in rates across these factors may reflect variability in identification of depression, rather than inherent risk of depression. For example, non-Hispanic white women are more likely to be screened for depression at delivery than non-Hispanic Black women,25 potentially inflating rates of depression amongst non-Hispanic white women.
Increasing trends in depressive disorders recorded during delivery hospitalization in this report may help to explain previously documented decreasing rates of self-reported postpartum depressive symptoms from 2004 to 2012.17 Increasing diagnoses at delivery from 2000 to 2015 may have resulted in an increase in treatment during the postpartum period and, in turn, a decrease in self-reported postpartum depressive symptoms. In many cases, pregnancy can be an opportunity for frequent care and monitoring by a health care provider, providing an ideal opportunity for the detection of depressive symptoms and if applicable, the documentation of a diagnosis, and the provision of treatment options through their clinic or referral.26 In the absence of active case identification strategies, most women with perinatal depression may neither seek nor receive help,27 thus, the American College of Obstetricians and Gynecologists, the United States Preventive Services Task Force’s, and The Council on Patient Safety in Women’s Health recommend universal screening for depression in pregnant and postpartum women.24,26,28 Given that screening is not universally practiced, depressive symptoms are commonly undiagnosed27,29 and our estimates are most likely underestimated.
This analysis documents baseline trends prior to 2016 legislation aimed at improving perinatal depression screening and treatment.16 State efforts to improve depression education and screening practices may be associated with differences in rates of diagnosed depressive disorders. A study of New Jersey data during 2009–2010 found that approximately 90% of women were screened for depression at delivery following a 2006 mandate requiring depression screening at hospital delivery.25 However, this may not be the case in all states and the overall impact of legislation on perinatal depression treatment outcomes remains unclear.30 Increasing trends in this report could be a result of more cases, better recognition of depression, or improved diagnoses following screening and assessment. Future analyses documenting rates post-legislation and incorporating multiple data sources with varying forms of depression ascertainment would complement this analysis and allow for a better understanding of the burden of depression in pregnant women.
Results of our study are subject to several limitations. First, the nature of the data used affects the generalizability of the results. Data do not include deliveries outside of the hospital; however, those births represent only 1.5% of all US births.31 Not all hospitals participated; however, at least 80% of National Center for Health Statistics births are represented for each state. Not all states provided data to the public-use State Inpatient databases, and amongst those that did, not all had data for every year in the study period. Second, estimates are most likely underestimates because screening for depression is not universally practiced. In addition, because many women deliver without a prenatal care record,32 depressive disorders recorded in other points during the pregnancy may not be documented on the delivery encounter for hospital discharge data. Third, analyses were dependent on ICD-CM coding, which may vary by hospital and state, and which may contribute to underestimated rates as ICD-CM codes are for billing and depressive disorders may not be documented. Depression screening and diagnosis are not typically included in reimbursed global obstetric payments, and providers may be less likely to document these ICD-CM codes because there is limited to no financial benefit from billing.33 We are also unable to determine what type of screener was used to identify and document the depressive disorders, so we are unable to comment on the sensitivity of these diagnoses. However, these data are frequently used to identify mental health diagnoses.20,21
Findings from this first state-based analysis of rates of depressive disorders recorded during hospitalization can help states understand the overall burden of depression among women at delivery. During 2000–2015, rates of depressive disorders recorded at delivery hospitalization increased significantly across the nation and in 27 states, and differed across age, insurance type, and race or ethnicity.
Supplementary Material
Financial Disclosure
Nancy Byatt receives grant funding from the National Institute of Health (R41 MH113381) and the Centers for Disease Control and Prevention (U01DP006093) for projects related to perinatal depression. Dr. Byatt receives salary and funding support from Massachusetts Department of Mental Health via the Massachusetts Child Psychiatry Access Program for Moms (MCPAP for Moms). Dr. Byatt is the founding and current statewide Medical Director of MCPAP for Moms. Dr. Byatt is also the Executive Director of Lifeline4Moms. Dr. Byatt is a member of the American College of Obstetricians and Gynecologists’ Expert Work Group on Maternal Mental Health. She has served on the Perinatal Depression Advisory Board for the Janssen Disease Interception Accelerator Program, the Physician Advisory Board for Sage Therapeutics, and is a Council Member of the Gerson Lehrman Group. She has also received speaking honoraria from and serves a consultant for Sage Therapeutics or their agents and Ovia Health. Dr. Byatt has also received honoraria from Medscape and Miller Medical Communications. Tiffany A. Moore Simas receives grant funding from the National Institute of Health (R41 MH113381) and the Centers for Disease Control and Prevention (U01DP006093) for projects related to perinatal depression. Dr. Moore Simas receives a stipend from the Massachusetts Department of Mental Health via Beacon for her role as Engagement Director of the Massachusetts Child Psychiatry Access Program for Moms (MCPAP for Moms). Dr. Moore Simas is Medical Director of Lifeline4Moms; she co-directs the American College of Obstetricians and Gynecologists’ Expert Work Group on Maternal Mental Health and was a member of the Council on Patient Safety in Women’s Health Care’s task force for creation of the maternal mental health patient safety bundle and co-author on the associated commentary. Dr. Moore Simas has served on ad hoc Physician Advisory Boards for Sage Therapeutics, has received speaking honoraria, and serves as a consultant on observational studies and a systematic review. Dr. Moore Simas serves as a consultant to Ovia Health, has received compensation for reviewing a perinatal depression case for McGraw Hill, and has received speaking honoraria from Miller Medical Communications. The other authors did not report any potential conflicts of interest.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily reflect the official position of the CDC.
A list of states participating in the State Inpatient Databases, Healthcare cost and Utilization Project, Agency for Healthcare Research and Quality is available at www.hcup-us.ahrq.gov/hcupdatapartners.jsp.
Presented as a poster session at the World Psychiatric Association Epidemiology and Public Health Section meeting: Emerging Mental Health Challenges Across the Globe, May 2–4, New York City, NY.
Peer Review History
Received January 2, 2019. Received in revised form March 7, 2019. Accepted March 21, 2019. Peer reviews are available at http://links.lww.com/xxx.
References
- 1.Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, et al. Perinatal depression: prevalence, screening accuracy, and screening outcomes. AHRQ Evidence Report Summaries 2005:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol 2005;106:1071–83. [DOI] [PubMed] [Google Scholar]
- 3.Zuckerman B, Amaro H, Bauchner H, Cabral H. Depressive symptoms during pregnancy: Relationship to poor health behaviors. Am J Obstet Gynec 1989;160:1107–11. [DOI] [PubMed] [Google Scholar]
- 4.Chung TKH, Lau TK, Yip ASK, Chiu HFK, Lee DTS. Antepartum depressive symptomatology is associated with adverse obstetric and neonatal outcomes. Psychosom Med 2001;63:830–4. [DOI] [PubMed] [Google Scholar]
- 5.Kurki T, Hiilesmaa V, Raitasalo R, Mattila H, Ylikorkala O. Depression and anxiety in early pregnancy and risk for preeclampsia. Obstet Gynecol 2000;95:487–90. [DOI] [PubMed] [Google Scholar]
- 6.Alder J, Fink N, Bitzer J, Hosli I, Holzgreve W. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med 2007;20:189–209. [DOI] [PubMed] [Google Scholar]
- 7.Dayan J, Creveuil C, Marks MN, Conroy S, Herlicoviez M, Dreyfus M, et al. Prenatal depression, prenatal anxiety, and spontaneous preterm birth: A prospective cohort study among women with early and regular care. Psychosom Med 2006;68:938–46. [DOI] [PubMed] [Google Scholar]
- 8.Ross LE, Dennis C-L. The prevalence of postpartum depression among women with substance use, an abuse history, or chronic illness: a systematic review. J Womens Health 2009;18:475–86. [DOI] [PubMed] [Google Scholar]
- 9.Grigoriadis S, VonderPorten EH, Mamisashvili L, Tomlinson G, Dennis CL, Koren G, et al. The impact of maternal depression during pregnancy on perinatal outcomes: a systematic review and meta-analysis. J Clin Psychiatry 2013;74:e321–41. [DOI] [PubMed] [Google Scholar]
- 10.Lindgren K Relationships among maternal–fetal attachment, prenatal depression, and health practices in pregnancy. Res Nurs Health 2001;24:203–17. [DOI] [PubMed] [Google Scholar]
- 11.Najman J, Plotnikova M, Williams G, Alati R, Mamun AA, Scott J, et al. Trajectories of maternal depression: a 27-year population-based prospective study. Epidemiol Psychiatr Sci 2017;26:79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wisner KL, Chambers C, Sit DY. Postpartum depression: A major public health problem. JAMA 2006;296:2616–8. [DOI] [PubMed] [Google Scholar]
- 13.Murray L, Arteche A, Fearon P, Halligan S, Goodyer I, Cooper P. Maternal postnatal depression and the development of depression in offspring Up to 16 years of age. J Am Acad Child Adolesc Psychiatry 2011;50:460–70. [DOI] [PubMed] [Google Scholar]
- 14.Murray L, Arteche A, Fearon P, Halligan S, Croudace T, Cooper P. The effects of maternal postnatal depression and child sex on academic performance at age 16 years: A developmental approach. J Child Psychol Psychiatry 2010;51:1150–9. [DOI] [PubMed] [Google Scholar]
- 15.Building US Capacity to Review and Prevent Maternal Deaths. Report from nine maternal mortality review committees. 2018. [Google Scholar]
- 16.21st Century Cures Act. H.R. 34, 114th Congress. (2016).
- 17.Ko JY, Rockhill KM, Tong VT, Morrow B, Farr SL. Trends in Postpartum Depressive Symptoms - 27 States, 2004, 2008, and 2012. MMWR Morb Mortal Wkly Rep 2017;66:153–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. Am J Obstet Gynecol 2010;202:5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Databases HCUP. Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 1999–2014. [PubMed] [Google Scholar]
- 20.Bennett AC, Gibson C, Rohan AM, Howland JF, Rankin KM. Mental Health and Substance Use-Related Hospitalizations Among Women of Reproductive Age in Illinois and Wisconsin. Public Health Rep (Washington, DC: 1974) 2019;134:17–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heslin KC, Elixhauser A, Steiner CA. Hospitalizations Involving Mental and Substance Use Disorders Among Adults, 2012: Statistical Brief #191. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. [PubMed] [Google Scholar]
- 22.Kuklina EV, Whiteman MK, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J 2008;12:469–77. [DOI] [PubMed] [Google Scholar]
- 23.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.) Arlington, VA: Author; 2013. [Google Scholar]
- 24.AL Siuand the USPSTF. Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA 2016;315:380–7. [DOI] [PubMed] [Google Scholar]
- 25.Farr SL, Denk CE, Dahms EW, Dietz PM. Evaluating universal education and screening for postpartum depression using population-based data. J Womens Health 2014;23:657–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 757: Screening for Perinatal Depression. Obstet Gynecol 2018;132:e208–e12. [DOI] [PubMed] [Google Scholar]
- 27.Milgrom J, Gemmill AW. Screening for perinatal depression. Best Pract Res Clin Obstet Gynaecol 2014;28:13–23. [DOI] [PubMed] [Google Scholar]
- 28.Council on Patient’s Safety in Women’s Health Care. Maternal Mental Health: Perinatal Depression and Anxiety. Patient Safety Bundle 2016. [Google Scholar]
- 29.Ko JY, Farr SL, Dietz PM, Robbins CL. Depression and treatment among U.S. pregnant and nonpregnant women of reproductive age, 2005–2009. J Womens Health 2012;21:830–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rhodes AM, Segre LS. Perinatal depression: a review of US legislation and law. Arch Womens Ment Health 2013;16:259–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hamilton BE, Martin JA, Osterman MJ, Curtin SC, Mathews T. Births: final data for 2014. 2015. [PubMed] [Google Scholar]
- 32.Miller DW, Jr., Yeast JD, Evans RL. Missing prenatal records at a birth center: a communication problem quantified. AMIA Annu Symp Proc 2005;2005:535–9. [PMC free article] [PubMed] [Google Scholar]
- 33.Ballard D Simplify Coding by Knowing what is Packaged into Obstetrics Care. American Academy of Professional Coders 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.