Abstract
Introduction and Hypothesis
Vulvodynia is chronic debilitating burning vulvar pain or pain on contact. Although women who suffer from vulvodynia are more likely than others to experience co-morbid interstitial cystitis (IC) and urinary tract infections (UTIs), few studies have explored whether women with vulvodynia experience adverse urinary symptoms (LUTS) in the absence of urological pain.
Methods
211 participants with and 226 participants without clinically-confirmed vulvodynia completed the Pelvic Pain and Urgency/frequency (PUF) questionnaire and were scored using all questions, and then a subset of questions relating only to their current frequency and bother of urination during day and night, and the frequency, severity and bother of urgency after voiding. Total, symptom, and bother scores were compared in women with and without vulvodynia, and regression models estimated adjusted odds ratios, and 95% confidence intervals for the various LUTS symptoms.
Results
As expected, 40% of women with vulvodynia met criteria for IC (PUF>12) compared to 2% without vulvodynia. After excluding questions related to bladder or vulvovaginal pain, women with vulvodynia, compared to those without, were skewed toward higher PUF scores, including being 2.4 times more likely to report usually or always bothered by night time voiding (95% CI 1.22–4.74), and 18 times more likely to report moderate/severe urgency after urination (95% CI 5.48– 64.12).
Conclusions
Women with vulvodynia are substantially more likely to report voiding dysfunction and symptoms of urgency than women with no history of vulvar pain. These findings are independent of comorbid Interstitial Cystitis or history of urinary tract infections.
Keywords: Vulvodynia, lower urinary tract symptoms, risk factors, retrospective study
Brief Summary:
Women with vulvodynia compared to controls are substantially more likely to report voiding dysfunction and symptoms of urgency independent of comorbid interstitial cystitis.
Introduction
Vulvodynia is a chronic condition characterized by debilitating vulvar discomfort due to burning pain or pain on contact that occurs in the absence of clinically visible pathological findings or identifiable disorders [1,2]. This condition is highly prevalent in the general population, with recent research suggesting that by age 40, 8% of women may have experienced unexplained vulvar pain for a period of at least 3 months or longer during their lifetime [3]. We also know that less than 50% of patients seek treatment, and those that do are often misdiagnosed due to inconsistent diagnostic criteria and disorder classification [4].
Women who suffer from vulvodynia are more likely than others to experience co-morbid interstitial cystitis (IC) [5] and urinary tract infections (UTI) [6,7]. However, there is little evidence in the scientific literature that women with vulvodynia experience other lower urinary tract symptoms (LUTS) in the absence of IC and UTI history. The primary objective of this study is to determine whether women with vulvodynia, compared to women without, differed in their self-reported history of daytime and nighttime urination frequency, urgency after urination, and severity and bother associated with urgency experiences.
Materials and Methods
The University of Minnesota and Boston University Institutional Review Board approved this study. Written consent has been obtained from all participants. Data for this analysis were originally collected as part of a case-control study to explore etiological predictors of vulvodynia, and its methods have been published elsewhere [8]. Briefly, approximately 30,000 women 18–40 years of age who were part of the administrative database of a large health care network that represents approximately 27% of the population in the Minneapolis/St. Paul metropolitan area, were initially screened through self-administered surveys to determine the presence of vulvar pain symptoms. These women were seen at one of approximately 40 outpatient community health clinics for any reason between March, 2010 and October, 2013. In a separate analysis we compared the demographic characteristics of this sample to census based data and found strong representation [9]. Upon review of the screener questionnaire, women likely to meet the International Society for the Study of Vulvovaginal Diseases (ISSVD) criteria for vulvodynia were invited to participate in a clinical visit to confirm the diagnosis.
Of the 1,398 women with vulvar pain symptoms invited, 350 completed their examination and 234 were clinically confirmed as meeting the diagnostic criteria for vulvodynia. There were no important differences in demographic characteristics (age, race, and marital status) or reproductive history (age at menarche, cycle regularity, and history of oral contraceptive use) among those who agreed and did not agree to participate in the clinical evaluation based on their screener questionnaire responses. A randomly selected woman from the same pool of those screened with no history of vulvar discomfort was selected as unexposed and assigned a reference age identical to the age at first onset of vulvar pain in the matched woman with vulvodynia. Of 2,287 women invited with no history of vulvar pain, 251 agreed and 234 were clinically confirmed as having no ongoing or past history of vulvar pain. For this analysis, we excluded 7 women with vulvodynia who reported a history of interstitial cystitis, and 15 women with and 4 women without vulvodynia who had missing information on urinary tract infection or the Pelvic Pain and Urgency/Frequency (PUF) questionnaire [10], resulting in 212 women with vulvodynia and 230 without vulvodynia for these analyses. All women enrolled had no active genitourinary infections at the time of their clinical visit, and if parous, being at least 1-year postpartum. Women were asked to refrain from introducing anything into their vaginas for 48 hours before the clinical visit.
All participants completed a background and medical history questionnaire by telephone that covered demographic characteristics, sexual and reproductive history, and personal medical history. In addition, all women participated in a telephone-administered Structured Clinical Interview for DSM-IV (SCID). Primary outcomes of interest in this analysis were lower urinary tract symptoms, measured through the Pelvic Pain and Urgency/frequency (PUF) questionnaire [10]. The original PUF symptoms score was calculated by summing up items 1, 2, 3a, 4, 4a, 5 and 5a (see Table 1). The original PUF bother score was calculated by summing up items 2a, 3b, 4b and 5b. The original PUF total score was calculated by summing up PUF symptoms and bother scores. Since items 3a, 3b, 4, 4a and 4b overlap with the diagnostic criteria for vulvodynia, we then created new PUF scores restricting on urinary symptoms by omitting responses to questions 3a, 3b, 4, 4a and 4b.
Table 1.
Pelvic Pain and Urinary/Frequency (PUF) Patient Symptoms Scale
| Questions | Point Scales | ||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |
| 1. How many times do you go to the bathroom during the day (times/day)? | 3-6 | 7-10 | 11-14 | 15-19 | 20+ |
| 2. How many times do you go to the bathroom at night (times/night)? | 0 | 1 | 2 | 3 | 4+ |
| 2a. If you get up at night to go to the bathroom, does it bother you? | Never | Occasionally | Usually | Always | |
| 3a. Do you now or have you ever had pain or symptoms during or after sexual intercourse? | Never | Occasionally | Usually | Always | |
| 3b. Has pain or urgency ever made you avoid sexual intercourse? | Never | Occasionally | Usually | Always | |
| 4. Do you have pain associated with your bladder or in your pelvis (vagina, labia, lower abdomen, urethra, perineum)? | Never | Occasionally | Usually | Always | |
| 4a. If you have pain is it usually… | Mild | Moderate | Severe | ||
| 4b. Does your pain bother you? | Never | Occasionally | Usually | Always | |
| 5. Do you still have urgency after going to the bathroom? | Never | Occasionally | Usually | Always | |
| 5a. If you have urgency, is it usually… | Mild | Moderate | Severe | ||
| 5b. Does your urgency bother you? | Never | Occasionally | Usually | Always | |
Statistical analysis
The analyses were based on 442 participants in which all outcomes and primary covariates were successfully obtained. Body mass index (BMI) categories were defined as <18.5 kg/m2 for underweight, ≥18.5 to <25.0 kg/m2 for normal, ≥25.0 to <30.0 kg/m2 for overweight and ≥30.0 kg/m2 for obese according to guidelines from the National Heart, Lung, and Blood Institute [11]. Gynecological conditions included cervical polyps, uterine fibroids, endometriosis, cervicitis, abnormal pap smear, a biopsy of cervix for examination & diagnosis, removal of all or part of an ovary, polycystic ovary syndrome, ovarian cysts, amenorrhea, hysterectomy and tubal ligation.
Gynecological infections included Gonorrhea, genital warts, bacterial vaginosis, trichomoniasis, pelvic inflammatory disease (PID), chlamydia, genital herpes, and urinary tract infection (UTI). Participant age at first gynecological condition/infection diagnosis was then compared to their age at first experience of vulvar pain to determine whether the condition/infection happened before the first onset of vulvodynia (or the reference age among unexposed participants). Smoking history was determined by whether the participants ever smoked 100 cigarettes in their lifetime, and if yes, additional categories were created based on cut-off values derived from tertiles of the average number of cigarettes smoked per day in all women. History of childhood abuse was defined as experience of any physical or sexual abuse through age 11 based on a detailed assessment previously described [12]. In general, the term “antecedent” was defined as exposures reported before age at first onset of vulvodynia, or the reference age among women without vulvodynia.
Descriptive analyses were performed on key demographic, personal, and medical history characteristics, stratified by vulvodynia status. The distributions of both original and restricted PUF symptoms, bother and total scores by vulvodynia status were also presented, in numbers and histograms.
We conducted regression analyses on specific PUF questionnaire items that do not overlap with the diagnostic criteria for vulvodynia. We included in these analyses frequency of urination during the day (Q1) and night (Q20), and the amount of bother reported by subjects during night time voiding (Q2a). We also included urgency after going to the bathroom (Q5), the severity of that urgency (Q5a), and to what degree the urgency bothered the participant (Q5b). Multinomial and logistic regression models were used to estimate both crude and adjusted odds ratios, and 95% confidence intervals for frequency of daytime & nighttime voiding, bother due to nighttime voiding, urgency, severity & bother after going to the bathroom. For both multinomial and logistic regression models, a forward selection approach with 10% criterion (change-in-estimate method) was used for model selection, in addition to predetermined confounders based on prior studies published in this area. The potential confounders were current age, use of sleeping medication, smoking history, antecedent anxiety and history of UTI. Indicator variables were included to represent missing data categories of the covariates in the descriptive table.
Results
Women with vulvodynia were on average 2 years younger, more likely to be nulligravid (53.3% vs. 41.3%), have a history of UTIs prior to the reference age (44.8% vs. 28.7%), report the use of sleeping medications at night (12.7% vs. 3.1%), a history of anxiety prior to first onset of vulvar pain (41.5% vs. 25.7%), and greater frequency of self-reported yeast infections compared to a comparable time period among women with no history of vulvodynia (Table 2).
Table 2.
Demographic characteristics by vulvodynia status, n=442
| Vulvodynia Status | ||
|---|---|---|
| Characteristics | Yes (N=212) | No (N=230) |
| Current age, years, means (SD) | 28.9 (±5.2) | 31.4 (±5.1) |
| Hispanic or Latina, n (%) | ||
| Yes | 11 (5.2) | 8 (3.5) |
| No | 199 (93.9) | 218 (94.8) |
| Missing | 2 (0.9) | 4 (1.7) |
| BMI Categories, n (%) | ||
| Underweight | 8 (3.8) | 5 (2.2) |
| Normal | 108 (50.9) | 122 (53.0) |
| Overweight | 58 (27.4) | 41 (17.8) |
| Obese | 36 (17.0) | 59 (25.7) |
| Missing | 2 (0.9) | 3 (1.3) |
| Number of Pregnancy, n (%) | ||
| Never Pregnant | 113 (53.3) | 95 (41.3) |
| 1-2 times | 64 (30.2) | 86 (37.4) |
| 3 times or more | 35 (16.5) | 48 (20.9) |
| Missing | 0 (0.0) | 1 (0.4) |
| Use of barrier contraception device (i.e. diaphragm, sponge or cervical cap), n (%) | ||
| Yes | 13 (6.1) | 13 (5.7) |
| No | 199 (93.9) | 217 (94.4) |
| Yeast Infection, n (%) | ||
| Yes, before reference age | 20 (9.4) | 36 (15.7) |
| Yes, only after reference age | 73 (34.4) | 81 (35.2) |
| Yes, both | 79 (37.3) | 51 (22.2) |
| No | 39 (18.4) | 60 (26.1) |
| Missing | 1 (0.5) | 2 (0.9) |
| Number of Gynecologic conditions, before reference age, n (%) | ||
| 0 | 146 (68.9) | 172 (74.8) |
| 1 | 35 (16.5) | 26 (11.3) |
| 2 | 19 (9.0) | 24 (10.4) |
| 3 or more | 12 (5.7) | 8 (3.5) |
| Number of Gynecologic infections, before reference age, n (%) | ||
| 0 | 101 (47.6) | 147 (63.9) |
| 1 | 93 (43.9) | 61 (26.5) |
| 2 or more | 18 (8.5) | 22 (9.6) |
| UTI Infection, n (%) | ||
| 1st onset prior to reference age | 95 (44.8) | 66 (28.7) |
| 1st onset after reference age | 53 (25.0) | 56 (24.4) |
| No | 64 (30.2) | 108 (47.0) |
| Genital warts & HPV, n (%) | ||
| Yes | 17 (8.0) | 6 (2.6) |
| No | 195 (92.0) | 223 (97.0) |
| Missing | 0 (0.0) | 1 (0.4) |
| Sleeping medications, n (%) | ||
| Yes | 27 (12.7) | 7 (3.1) |
| No | 185 (87.3) | 222 (96.9) |
| Missing | 0 (0.0) | 1 (0.4) |
| Number of Cigarettes per day, n (%) | ||
| Less than 1 | 123 (58.0) | 156 (67.8) |
| 1 to 5 | 34 (16.0) | 35 (15.2) |
| 6 to 10 | 29 (13.7) | 21 (9.1) |
| More than 10 | 26 (12.3) | 17 (7.4) |
| Missing | 0 (0.0) | 1 (0.4) |
| Age 1st Sexual Intercourse* yrs, mean (SD) | 18.2 (±3.6) | 17.8 (±3.7) |
| Number of Sexual Partners**, mean (SD) | 7.7 (±9.0) | 9.2 (±11.0) |
| History of Abuse, n (%) | ||
| None | 70 (33.0) | 83 (36.1) |
| Moderate | 28 (13.2) | 39 (17.0) |
| Severe | 64 (30.2) | 46 (20.0) |
| Missing | 50 (23.6) | 62 (27.0) |
| Antecedent*** Anxiety, n (%) | ||
| None | 122 (57.6) | 169 (73.5) |
| Yes, not diagnosed | 27 (12.7) | 28 (12.2) |
| Yes, diagnosed | 61 (28.8) | 31 (13.5) |
| Missing | 2 (0.9) | 2 (0.9) |
| Antecedent Depression, n (%) | ||
| None | 134 (63.2) | 152 (66.1) |
| Yes, not diagnosed | 15 (7.1) | 23 (10.0) |
| Yes, diagnosed | 63 (29.7) | 52 (22.6) |
| Missing | 0 (0.0) | 3 (1.3) |
No. of missing for subjects with vulvodynia: 3, without: 6;
No. of missing for subjects with vulvodynia: 5, without: 2
Antecedent is defined as exposures reported before age at first onset of vulvodynia, or the reference age among women with/without vulvodynia
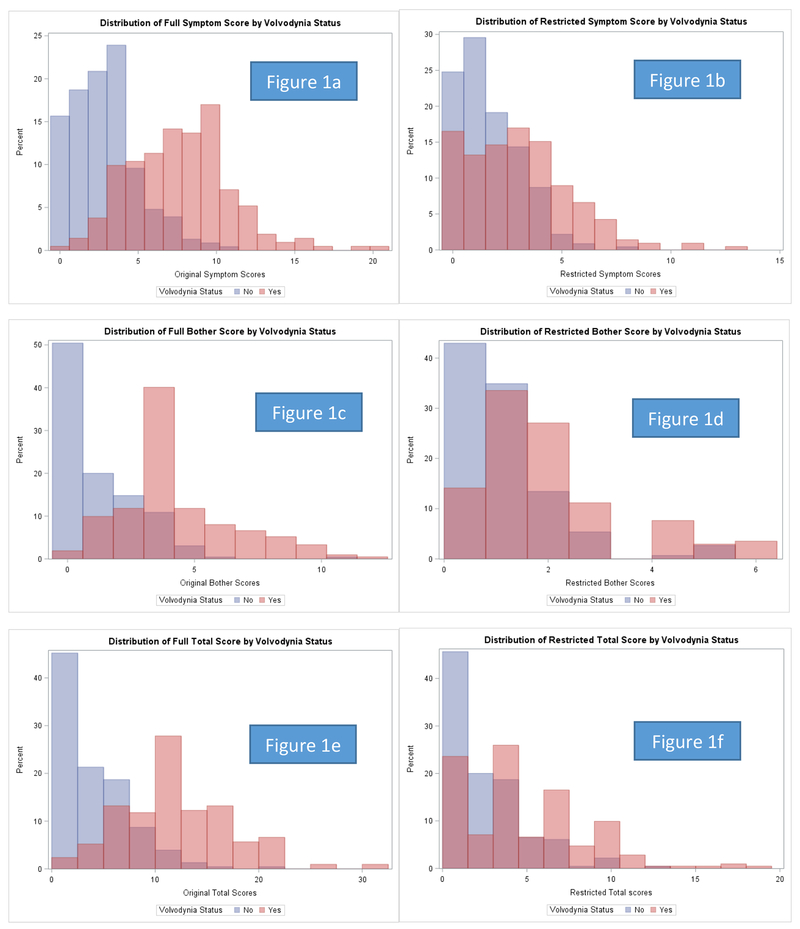
The distributions of full and restricted PUF symptom, bother and total scores by vulvodynia status are presented in Figures 1a-1f. Among women with clinically-confirmed vulvodynia, 49% had PUF symptom scores greater than 8, 58% had PUF bother scores greater than 4, and 40% had total PUF scores greater than 12, compared to 3%, 6% and 2% among controls, respectively (Figures 1a, 1c, 1e). After excluding questions that overlap with the diagnostic criteria for vulvodynia (Q3a, 3b, 4, 4a, and 4b, Table 1) leaving only urinary symptom questions, approximately 15% of women with vulvodynia had symptoms scores greater than 5, 20% had bother scores greater than 2, and 8% had total scores greater than 9, compared to 1%, 6% and 0.4% of controls, respectively (Figures 1b, 1d, 1f).
Figures 1a-1f –
Distribution of symptom, bother, and total scores in women with (N=212) and without (N=230) clinically-confirmed vulvodynia using all PUF questions (figs a,c,e), and then after exclusion of vulvar pain questions 3a,3b,4,4a,4b and leaving only urinary symptom questions (figs b,d,f)
We further assessed the association between urinary symptoms and vulvodynia using selected items from the PUF scale (Table 3). Women with vulvodynia, compared to women without, reported greater frequency of daytime and nighttime voiding after adjustment for current age, use of sleeping medication, smoking history, antecedent anxiety and history of UTIs. A stronger association was observed with respect to bother during voiding. Women with vulvodynia were 2.4 times more likely than women without vulvodynia to report being usually or always bothered by night time voiding (95% CI 1.2–4.8). When restricted only to women who reported night time voiding, women with vulvodynia, compared to those without, were 3.4 times more likely to report being usually or always bothered by nighttime voiding after the same multivariate adjustments (95% CI 1.7–7.1).
Table 3.
Association of vulvodynia and urinary symptoms, n=442
| Vulvodynia Status | |||||
|---|---|---|---|---|---|
| Yes (N=212) | No (N=230) | ||||
| N (%) | N (%) | Crude OR | Adjusted ORa | 95% CI | |
| Frequency of daytime voiding | |||||
| 3-6 times per day | 98 (46.2) | 131 (57.0) | 1.0 | 1.0 | Referent |
| 7-10 times | 85 (40.1) | 75 (32.6) | 1.5 | 1.7 | (1.1, 2.6) |
| 10 times or more | 29 (13.7) | 24 (10.4) | 1.6 | 1.4 | (0.77, 2.9) |
| Frequency & bother due to night time voiding | |||||
| Never void at night | 68 (32.1) | 89 (38.7) | 1.0 | 1.0 | Referent |
| 1 time | 107 (50.5) | 118 (51.3) | 1.2 | 1.2 | (0.79, 1.9) |
| 2 times or more | 37 (17.5) | 23 (10.0) | 2.1 | 1.7 | (0.89, 3.4) |
| Never bothers | 36 (17.0) | 67 (29.1) | 0.7 | 0.7 | (0.43, 1.3) |
| Occasionally | 64 (30.2) | 56 (24.4) | 1.5 | 1.6 | (0.97, 2.8) |
| Usually/always | 44 (20.8) | 18 (7.8) | 3.2 | 2.4 | (1.2, 4.8) |
| Get up, never bothers | 36 (25.0) | 67 (47.5) | 1.0 | 1.0 | Referent |
| Get up, occasionally | 64 (44.4) | 56 (39.7) | 2.1 | 2.1 | (1.2, 3.8) |
| Get up, usually/always | 44 (30.6) | 18 (12.8) | 4.6 | 3.4 | (1.7, 7.1) |
| Urgency, severity & bother after going to the bathroom | |||||
| Never | 93 (43.9) | 188 (81.7) | 1.0 | 1.0 | Referent |
| Mild urgency | 80 (37.7) | 38 (16.5) | 4.3 | 3.7 | (2.3, 6.1) |
| Moderate/severe urgency | 39 (18.4) | 4 (1.7) | 19.7 | 19.1 | (5.6, 65.4) |
| Never bothers/occasionally | 92 (43.4) | 34 (14.8) | 5.5 | 5.0 | (3.1, 8.2) |
| Usually/always bothers | 27 (12.7) | 8 (3.5) | 6.8 | 4.4 | (1.7, 11.4) |
| Urgency, mild | 80 (67.2) | 38 (90.5) | 1.0 | 1.0 | Referent |
| Urgency, moderate/severe | 39 (32.8) | 4 (9.5) | 4.6 | 5.0 | (1.4, 17.9) |
| Urgency, never bothers/occasionally | 92 (77.3) | 34 (81.0) | 1.0 | 1.0 | Referent |
| Urgency, usually/always | 27 (22.7) | 8 (19.1) | 1.3 | 0.8 | (0.27, 2.4) |
All models adjusted for current age, use of sleeping medication, smoking history, antecedent anxiety and UTI before the reference age;
All models excluded subjects with interstitial cystitis (n=7)
CI, confidence interval; OR, odds ratio
In our assessment of self-reported urgency, severity, and bother after going to the bathroom, women with vulvodynia, compared to those without, were 19.1 times more likely to report moderate to severe urgency after urination (95% CI 5.6– 65.4), after adjustment for the same set of potential confounders listed above. Women with vulvodynia were also 5.0 times more likely to be occasionally bothered by urgency after urination, and 4.4 times more likely to be usually or always bothered after urination, in comparison to women who never had urgency after going to the bathroom. When restricted to women who experienced any urgency after urination, women with vulvodynia, compared to those without, were nearly 5.0 times more likely to report moderate or severe urgency (95% CI 1.4–17.9).
Discussion
Our findings suggest that after excluding the PUF questions pertaining to bladder or vulvovaginal pain which overlap with the diagnostic criteria for vulvodynia, women with vulvodynia, compared to those without, were substantially more likely to be bothered by night time voiding, and reported the experience of moderate to severe urgency after urination, even after adjustment for urinary tract infections. Previous studies have shown that women who suffer from vulvodynia are more likely than others to experience co-morbid IC and a history of UTIs [6–8, 13]. However, no studies to our knowledge have assessed whether women with vulvodynia suffer from other urinary symptoms in the absence of IC and UTI history.
Kahn et al. [14] suggests that vulvar pain could be referred from the bladder as a consequence of bladder epithelial dysfunction. They support this by showing in a case series of women with vulvodynia that 80% reported a positive intravesical potassium sensitivity test (PST), a well-established predictor of interstitial cystitis. However, these authors also go on to state that most studies of women with vulvodynia have not quantified urinary symptoms and that women with vulvar pain consider urinary urgency or frequency less significant and in many cases choose not to report those symptoms.
Salonia and colleagues [15] studied a consecutive series of 60 women being seen for uncomplicated UTIs and stratified them by those with and without co-morbid provoked vestibulodynia. Based on the American Urological Association Symptom Index (AUI-SI), no differences were observed for voiding dysfunction. This suggests that in the presence of UTI infections, voiding dysfunction does not appear to vary by those with and without vulvodynia. However, our study suggests that in the absence of UTIs, or after adjustment for their history, voiding dysfunction appears to be strongly associated with vulvodynia.
The same investigators assembled a consecutive series of 227 women being seen for urinary incontinence or recurrent or persistent LUTS [16]. Female sexual dysfunction was observed in 46% of participants. When they compared these women to women being seen for a routine gynecological visit, those with LUTS reported less sexual desire, lubrication, and satisfaction, and significantly greater sexual pain, compared to controls. These findings indirectly corroborate our findings within a population of women with and without LUTS.
We recognize certain limitations within our study. First, the outcome of lower urinary tract symptoms were measured through self-reported questionnaires and not confirmed through real time diary assessments. There is the risk that women with vulvodynia may exaggerate their urological symptoms as a consequence of their vulvar pain. There is also the possibility that women without vulvodynia may under report abnormal urological symptoms either due to stigma or their belief that voiding and urgency issues are normal. Although we cannot rule out this bias, our findings are very strong and even if part of our observed associations are due to misclassification bias, it is unlikely to account for all of the associations observed. Lastly, the PUF questionnaire only assessed current LUTS and we could not evaluate the timing of first onset or duration of LUTS.
Secondly, the temporal sequence of LUTS and vulvodynia cannot be disentangled. LUTS were recorded at the time of study enrollment but the questionnaire did not inquire as to the presence of these urological symptoms before the onset of vulvar pain or reference age among controls. A third consideration is that although we analyzed a restricted version of the PUF to eliminate questions that overlapped with the diagnostic criteria for vulvodynia, we cannot rule out that some women with unreported bladder related pain were retained and more likely to be among the women with vulvodynia. However, we did exclude 23 women with vulvodynia who reported co-morbid IC at the outset of the study.
Conclusions
Our findings suggest that women with vulvodynia are substantially more likely to report voiding dysfunction and symptoms of urgency than women with no history of vulvar pain. These findings may be independent of comorbid interstitial cystitis or history of urinary tract infections. In the discussion of these findings with our urological colleagues, we have heard that many believe that LUTS occur more commonly in women with vulvodynia. It was therefore surprising to find few if any studies in the scientific literature that directly assessed this association. Clearly, further research is needed to better understand the temporal association between vulvar pain and benign urological symptoms and whether LUTS phenotypes align more so with certain vulvodynia phenotypes than others. These findings also suggest that women with vulvodynia should be routinely managed by clinicians with experience in both gynecology and urology.
Acknowledgements
The authors wish to thank Dr. Elizabeth Lukacz from the University of California San Diego and Dr. Tamara Bavendam from the National Institute of Diabetes and Digestive and Kidney Diseases their peer review and advice on this article. No fee for this service was incurred. This research was supported by NIH-NICHD-R01 HD058608
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Financial Disclaimers: Both authors report no conflicts of interest.
References
- 1.Moyal-Barracco M, Lynch PJ. (2003) ISSVD terminology and classification of vulvodynia: a historical perspective. The Journal of reproductive medicine. 49:772. [PubMed] [Google Scholar]
- 2.Bornstein J, Goldstein AT, Stockdale CK, Bergeron S, Pukall C, Zolnoun D, Coady D, Goldstein A, Bachmann GA, Bissonnette I, Starke NB (2015) ISSVD, ISSWSH, and IPPS consensus terminology and classification of persistent vulvar pain and vulvodynia. The Journal of sexual medicine. 13:607–12. [DOI] [PubMed] [Google Scholar]
- 3.Harlow BL, Kunitz CG, Nguyen RH, Rydell SA, Turner RM, MacLehose RF. Prevalence of symptoms consistent with a diagnosis of vulvodynia: population-based estimates from 2 geographic regions (2014) American journal of obstetrics and gynecology. 210:40-e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harlow BL, Stewart EG (2003) A population-based assessment of chronic unexplained vulvar pain: have we underestimated the prevalence of vulvodynia? Journal of the American Medical Women′s Association 58:82–8. [PubMed] [Google Scholar]
- 5.Gardella B, Porru D, Nappi RE, Daccò MD, Chiesa A, Spinillo A (2011) Interstitial cystitis is associated with vulvodynia and sexual dysfunction—a case-control study. Journal Sexual Med, 8:1726–34. [DOI] [PubMed] [Google Scholar]
- 6.Arnold LD, Bachmann GA, Rosen R, Rhoads GG (2007) Assessment of vulvodynia symptoms in a sample of US women: a prevalence survey with a nested case control study. American journal of obstetrics and gynecology. 196:128-e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen RH, Swanson D, Harlow BL (2009) Urogenital infections in relation to the occurrence of vulvodynia. J Reprod Med. 54:385–92. [PubMed] [Google Scholar]
- 8.Harlow BL, Caron RE, Parker SE, Chatterjea D, Fox MP, Nguyen RH (2017) Recurrent yeast infections and vulvodynia: can we believe associations based on self-Reported data? Journal of Women’s Health 26:1069–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oakes JM, MacLehose RF, McDonald K, Harlow BL (2015) Using administrative health care system records to recruit a community-based sample for population research. Ann Epidemiol 25:526–531. [DOI] [PubMed] [Google Scholar]
- 10.Parsons CL, Dell J, Stanford EJ, Bullen M, Kahn BS, Waxell T, Koziol JA (2002) Increased prevalence of interstitial cystitis: previously unrecognized urologic and gynecologic cases identified using a new symptom questionnaire and intravesical potassium sensitivity. Urology 60:573–8. [DOI] [PubMed] [Google Scholar]
- 11.National Heart, Lung, and Blood Institute (1998). Clinical guidelines on identification, evaluation, and treatment of overweight and obesity in adults. Bethesda, MD: National Institutes of Health, National. Heart, Lung, and Blood Institute. [Google Scholar]
- 12.Khandker M, Brady SS, Stewart EG, Harlow BL (2014) Is chronic stress during childhood associated with adult-onset vulvodynia? Journal of women’s health. 23:649–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arnold LD, Bachmann GA, Kelly S, Rosen R, Rhoads GG (2006) Vulvodynia: characteristics and associations with co-morbidities and quality of life. Obstetrics and gynecology. 210:40-e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kahn BS, Tatro C, Parsons CL, Willems JJ (2010) Prevalence of interstitial cystitis in vulvodynia patients detected by bladder potassium sensitivity. J Sexual Med 7:996–1002. [DOI] [PubMed] [Google Scholar]
- 15.Salonia A, Clementi MC, Graziottin A, Nappi RE, Castiglione F, Ferrari M, Capitanio U, Damiano R, Montorsi F (2013) Secondary provoked vestibulodynia in sexually active women with uncomplicated recurrent urinary tract infections. J Sexual Med 10:2265–73. [DOI] [PubMed] [Google Scholar]
- 16.Salonia A, Zanni G, Nappi RE, Briganti A, Dehò F, Fabbri F, Colombo R, Guazzoni G, Di Girolamo V, Rigatti P, Montorsi F (2004) Sexual dysfunction is common in women with lower urinary tract symptoms and urinary incontinence: results of a cross-sectional study. European urology. 45:642–8. [DOI] [PubMed] [Google Scholar]