Abstract
Aim
This cross-sectional multicenter study was performed aimed at describing the clinical characteristics of women with COPD attended in routine daily practice in Spain.
Methods and results
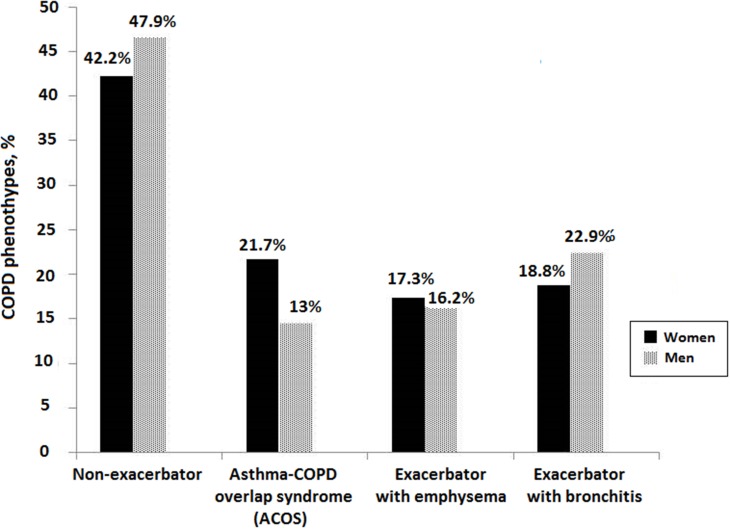
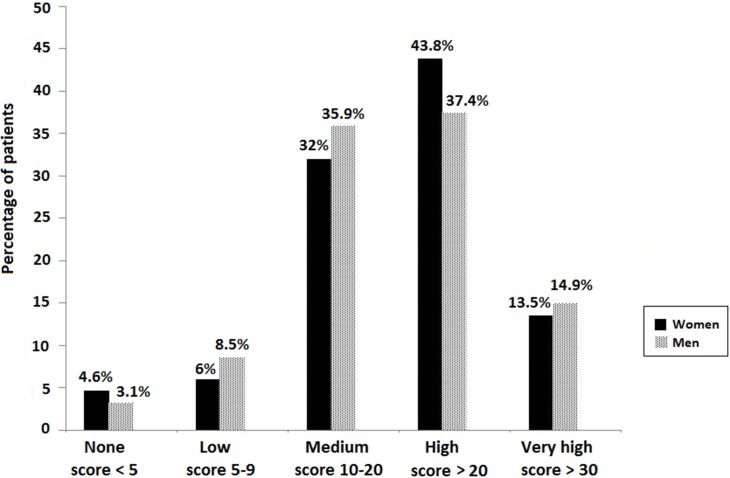
Of a total of 1610 consecutive patients diagnosed with COPD recruited in primary care centers and pneumology services throughout Spain over a 90-day period, 17.9% (n=286) were women, with a median age of 62 years. Differences in COPD phenotypes by sex were statistically significant (P = 0.002). Males as compared with females showed a higher prevalence of non-exacerbator (47.9% vs 42.2%) and exacerbator with chronic bronchitis (22.9% vs 18.8%) phenotypes, whereas the ACOS phenotype was more common among females (21.7% vs 12.9%). The mean (SD) CAT score was similar in men than in women (20.8 [9.0] vs 21.2 [8.7], P = 0.481), as well as the impact of the disease on the quality of life according to CAT scores of <5 (no impact), 5–9 (low), 10–20 (medium), >20 (high), and >30 (very high). Sex-related differences according to smoking status were statistically significant (P < 0.001), with a higher percentage of men as compared with women in the groups of current smokers and ex-smokers; never-smokers were higher in women (9.1%) than in men (0.6%). The mean number of comorbidities was 2.01 (1.43) (95% CI 1.93–2.09) in males and 1.99 (1.42) (95% CI 1.83–2.16) (P = 0.930) in females, but cardiovascular diseases (hypertension, ischemic heart disease, chronic heart failure) were more frequent in men, whereas metabolic disorders (osteoporosis) were more frequent in women.
Conclusion
This study highlights the impact of COPD in women and the importance of continuing sex-based research in tobacco-related respiratory diseases.
Keywords: pulmonary disease, chronic obstructive, chronic bronchitis, phenotype, pulmonary emphysema, quality of life, asthma
Introduction
Chronic obstructive pulmonary disease (COPD) is a major cause of morbidity and mortality throughout the world, with a substantial economic burden and social and quality of life impact on patients.1–3 It is also expected that the worldwide burden of COPD will continue to rise in the forthcoming years, and it is also witnessed a major shift in the sex profile of the disease.4 Although for many years COPD affected men in a higher proportion than women, the prevalence has equalized by now.5 However, there remains an outdated perception of COPD as a male-dominated disease combined with a lack of awareness of symptoms among women. The prevalence and mortality of COPD in women have more than doubled during the past 20 years in industrialized countries while they stabilized in men.6 Different studies have shown a sex effect, with an increase in COPD mortality among women.7,8 In Sweden, COPD mortality in women increased between 1999 and 2009, and life expectancy among COPD patients was 9.4 years lower in women (vs 7.4 years lower in men) compared with the average Swedish population.9 Surveillance data (1971–2000) from the United States showed in 2000, for the first time, that the number of COPD deaths recorded in women surpassed the number of COPD deaths among men.10
A number of factors are likely to have contributed to the increasing prevalence of COPD in women, including increasing tobacco consumption among women during the past several decades, greater exposure to indoor air pollution (biomass smoke from cooking and heating), differential vulnerability and susceptibility to tobacco, anatomic and hormonal differences, as well as behavioral differences in response to available therapeutic modalities.9,10 Moreover, underdiagnosis or misdiagnosis occurs more frequently in women than in men. Among patients with spirometric COPD criteria included in the Epidemiologic Study of COPD in Spain (EPI-SCAN), underdiagnosis was 1.27 times more frequent in women than in men, with an odds ratio of being correctly diagnosed with COPD of 1.9 for men versus women.11 The probability of being diagnosed increases with age, intensity, and duration of smoking, the severity of the disease, and the impairment in health-related quality of life.12 Also, many women are unaware of the key symptoms of COPD, resulting in a failure to report their symptoms to their primary care physician.5 Taken all these findings together, COPD is usually diagnosed late in the course of the disease in females and it is usually associated with impaired quality of life and comorbidities.
In addition, women are more likely to be significantly burdened by the symptoms of COPD than men, and this effect appears most pronounced among younger women.13 Interestingly, in a study of sex-specific differences in emphysema across a large population of COPD subjects, women with severe emphysema and severe early-onset COPD, as well as those with Global Initiative for Chronic Obstructive Lung Disease (GOLD) grade IV exhibited similar rates of emphysema to men but were associated with markedly fewer pack-years.14 These findings illustrate aspects of COPD that warrant further study,15 such as the advantages and benefits of phenotyping COPD patients, the perspective of sex regarding the public health phenomenon of COPD, and the need for early diagnosis of COPD in smokers. An early diagnosis of COPD in smokers is not only important to prevent the late consequences of severe COPD but also the early consequences in terms of comorbidities and the early impact on the quality of life.
To further explore sex differences in patients with COPD, a cross-sectional multicenter study was performed aimed at describing the clinical characteristics of women with COPD attended in routine daily practice in Spain.
Materials And Methods
Study Design
The “ESPIRAL-ES Study” was an observational, cross-sectional and multicenter study conducted in primary care centers and services of pneumology throughout Spain. “ESPIRAL-ES” is the Spanish acronym for Study of the Prevalence of COPD phenotypes, assessment of health-related quality, and geographic distribution in Spain (“EStudio de la Prevalencia de los fenotIpos de la EPOC, valoRación de la cALidad de vida relacionada con la salud y su distribución geográfica en España”). Results regarding the prevalence and geographic distribution of COPD phenotypes among the different autonomous communities of the country have been previously reported.16 The primary objective of the present study was to assess whether there were sex-related differences in the prevalence of COPD phenotypes and clinical characteristics of the disease. The secondary objective was to define the clinical profile of women diagnosed with COPD collected from the ESPIRAL-ES study population.
The study protocol was approved by the Clinical Research Ethics Committee of Hospital San Pedro de Alcántara, Cáceres (Spain). The study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients.
Patients
Consecutive COPD patients who met the inclusion criteria visited by family physicians or pulmonologists in routine daily practice were prospectively recruited during a 90-day period between March and May 2015. Physicians who participated in the study worked in the primary health care setting throughout in Spain. Patients who met the inclusion criteria were asked to take part in the study during usual care. Inclusion criteria were men and women aged 35 years or older, in whom a definitive diagnosis of COPD had been established according to the 2014 GOLD criteria,17 which are consistent with 2012 GesCOPD guidelines published by the Spanish Society of Pulmonology and Thoracic Surgery18 at least 6 months before enrollment. Excluded were patients with symptoms with acute COPD exacerbation or with a history of a recent episode of COPD exacerbation, but those patients could be eligible 4 weeks after the exacerbation. Other exclusion criteria were presence of significant chronic respiratory disorders other than COPD and asthma, or cognitive impairment that prevented understanding and completing the study questionnaires.
Study Procedures
For each participant the following data were recorded: age; sex; body mass index; smoking status (categorized as current smoker, ex-smoker, never-smoker) and smoking index (pack-years); duration of COPD; comorbid conditions (hypertension, diabetes mellitus, arrhythmia, coronary artery disease, heart failure, osteoporosis, dyslipidemia, and dementia); pulmonary function tests, degree of dyspnea assessed with the modified Medical Research Council (MRC) scale;19 6-min walking distance test; severe exacerbations requiring admission to the hospital and/or emergency department for more than 24 h in the previous 12 months; severity of COPD using the BODEx index20 (scored 0–2 points for quartile 1, 3–4 points for quartile 2, 5–6 points for quartile 3, and ≥7 points for quartile 4); quality of life using the COPD Assessment Test (CAT)21 (scores range from 0 to 40, with higher scores indicating a more severe impact of COPD on the quality of life); and COPD phenotype using the 2012 GesCOPD algorithm18 classified as non-exacerbator, asthma-COPD overlap syndrome (ACOS), exacerbator with emphysema, and exacerbator with chronic bronchitis phenotypes. The diagnosis of ACOS was made according to recommendations of a consensus document,22 when 2 major criteria or 1 major criterion and 2 minor criteria were met. The three major criteria included very positive bronchodilator test with an increase in FEV1 ≥15% and ≥400 mL over baseline, sputum eosinophilia, and history of asthma (before the age of 40). The three minor criteria were elevated total IgE, history of atopy, and positive bronchodilator test with an increase in FEV1 ≥ 12% and ≥200 mL over baseline on two or more occasions.22
Statistical Analysis
The sample size was calculated according to an expected prevalence of 10.2% in the general Spanish population aged 40–80 years as reported in the EPI-SCAN study.12 With a precision of 3.1% at the national level and 38% in a bilateral contrast, with an alpha risk of 5% assuming maximal variability (p=q=50%) and with 5% of losses, a total sample of 1050 patients would be required. Therefore, for an expected recruitment of 2 to 4 patients per physician, a minimum of 262 and a maximum of 525 participating researchers would be necessary. Participating physicians were selected using a commercially available database (www.medynet.com). Medynet database is the first Internet node exclusively devoted to the health care sector in Spain that currently includes data of approximately 190,000 users. It is a free registration database of physicians and health care providers that includes health care professionals working both in the public National Health Care System and in the private sector. A stratified random sampling method based on the population size of each autonomous community was used.
Data were expressed as mean and standard deviation (SD) for continuous variables and absolute and relative frequencies (percentages) for categorical variables, with their 95% confidence intervals (CIs). Categorical variables were compared with the chi-square (χ2) test or the Fisher’s exact test, and continuous variables with the Student’s t-test or the analysis of variance (ANOVA) for values with a normal distribution and the Mann–Whitney U-test or the Kruskal–Wallis test for data whose distribution departed from normality. Statistical significance was set at P < 0.05. Data were analyzed using the Statistical Analysis Systems (SAS) (SAS Institute, Cary, NC, USA) statistical software package, version 9.4 for Windows.
Results
During the study period, a total of 563 physicians, mostly pneumologists (56%) and family/community medicine specialists (37%), recruited a total of 1680 consecutive patients with COPD, but 70 (4.2%) were excluded because of symptoms of exacerbation in the previous 6 weeks in 58 patients, age under 35 years in 1, and lack of registration of the selection criteria in the case report form in 11. The participating physicians worked in primary health care centers from 16 out of the 17 Spanish autonomous communities.
Of the 1610 patients with COPD included in the study, 286 (17.8%) were women, with a mean (SD) age of 63.4 (10.2) years. The main characteristics of the study population are shown in Table 1. Salient features included a mean body mass index (BMI) of 27.4 kg/m2 (35.2% of women with overweight and 29.5% with obesity), and 53.3% of patients who stated they were active smokers, with a smoking index of 60.6 pack-years, and a mean FEV1 of 59.6%. At the time of the study, non-smokers accounted for 46.7% of the cases (ex-smokers 37.5% and never-smokers 9.1%).
Table 1.
Characteristics Of 286 Women With COPD
| Study Variables | Female Patients | Male Patients | P value | ||
|---|---|---|---|---|---|
| Number | Descriptive Data | Number | Descriptive Data | ||
| Age, years, mean (SD) [95% CI] | 279 | 63.4 (10.2) [66.2 to 64.6] | 1298 | 67.4 (9.4) [66.9 to 67.9] | < 0.001 |
| Body mass index, kg/m2, mean (SD) [95% CI] | 281 | 27.4 (5.2) [26.8 to 28.0] | 1296 | 28 (4.6) [27.7 to 28.2] | 0.072 |
| Smoking status | 285 | 1313 | < 0.001 | ||
| Current smoker | 152 (53.3) | 738 (56.2) | |||
| Ex-smoker | 107 (37.5) | 567 (43.2) | |||
| Never-smoker | 26 (9.1) | 8 (0.6) | |||
| Smoking index, pack-years, mean (SD) [95% CI] | 242 | 62.1 (105.8) [48.7 to 75.5] | 1261 | 63.9 (89.5) [58.9 to 68.8] | 0.785 |
| Years from COPD diagnosis, mean (SD) [95% CI] | 267 | 7.7 (7.3) [6.9 to 8.6] | 1235 | 9.2 (8) [8.7 to 9.6] | 0.007 |
| Comorbidities | 286 | 1314 | |||
| Yes | 237 (82.9) | 1105 (84.1) | 0.595 | ||
| Number of comorbidities, mean (SD) [95% CI] | 286 | 2.0 (1.4) [1.8 to 2.2] | 2 (1.4) [1.9 to 2.1] | 0.862 | |
| Spirometry, mean (SD) [95% CI] | |||||
| FVC, mL | 222 | 2360.9 (782.4) [2257.5 to 2464.4] |
1008 | 2533.9 (883.7) [2479.2 to 2588.5] |
0.007 |
| FVC, % | 229 | 77.5 (13.0) [75.8 to 79.2] | 1094 | 72.7 (14.5) [71.8 to 73.5] | < 0.001 |
| FEV1, mL | 223 | 1295.1 (503.2) [1228.7 to 1361.5] |
1009 | 1363.7 (561.5) [1329.1 to 1398.4] |
0.092 |
| FEV1, % | 245 | 59.6 (14.0) [57.8 to 61.3] | 1093 | 53.6 (15.1) [52.7 to 54.4] | < 0.001 |
| FVC/FEV1 | 236 | 57.7 (11.1) [56.3 to 59.1] | 1115 | 54.8 (12.3) [54.1 to 55.6] | < 0.001 |
| Dyspnea | 283 | 1301 | 0.132 | ||
| Grade 0 | 16 (5.6) | 81 (6.2) | |||
| Grade 1 | 114 (40.3) | 455 (35) | |||
| Grade 2 | 105 (37.1) | 456 (35.1) | |||
| Grade 3 | 42 (14.8) | 274 (21.1) | |||
| Grade 4 | 6 (2.1) | 35 (2.7) | |||
| 6-min walking test, m | 286 | 822 | 0.537 | ||
| ≥ 350 | 67 (23.4) | 338 (41.1) | |||
| 250–349 | 64 (22.4) | 251 (30.5) | |||
| 150–249 | 40 (14.0) | 160 (19.5) | |||
| < 149 | 15 (5.2) | 73 (8.9) | |||
| Severe exacerbations previous year, mean (SD) [95% CI] | 278 | 0.9 (1.3) [0.8 to 1.1] | 1279 | 1 (1.3) [0.9 to 1] | 0.747 |
| Two or more moderate-severe exacerbations | 286 | 113 (39.5) | 1307 | 553 (42.3) | 0.390 |
| CAT score, mean (SD) [95% CI] | 281 | 21.2 (8.7) [20.2 to 22.2] | 1301 | 20.8 (9) [20.3 to 21.3] | 0.546 |
| COPD impact according to CAT | 281 | 1301 | 0.137 | ||
| None, score < 5 | 13 (4.6) | 41 (3.2) | |||
| Low, score 5–9 | 17 (6.0) | 111 (8.5) | |||
| Medium, score 10–20 | 90 (32.0) | 467 (35.9) | |||
| High, score > 20 | 123 (43.8) | 487 (37.4) | |||
| Very high, score > 30 | 38 (13.5) | 195 (15) | |||
| BODEx index, mean (SD) [95% CI] | 252 | 2.3 (1.7) [2.1 to 2.5] | 1167 | 2.9 (2) 2.7 to 3] | < 0.001 |
| 0–2 points | 145 (57.5) | 545 (46.7) | < 0.001 | ||
| 3–4 points | 80 (31.7) | 368 (31.5) | |||
| 5–6 points | 25 (9.9) | 210 (18) | |||
| ≥ 7 points | 2 (0.8) | 44 (3.8) | |||
Note: Data expressed as frequencies and percentages in parenthesis unless otherwise stated.
Abbreviations: CI, confidence interval; FVC, forced vital capacity; FEV1, forced expiratory volume in 1 s; BODEx, body mass index, airflow obstruction, dyspnea, and exacerbations; CAT, COPD Assessment Test.
The mean (SD) years from COPD diagnosis was 7.7 (7.3) years. Also, comorbidities were present in 82.9% of patients, with dyslipidemia (56.6%), hypertension (54.2%), osteoporosis (45.8%), and diabetes (26.6%) as the most frequent. Dyspnea grade ≥2 was recorded in 54.1% of patients. In the 6 min walking test, 41.6% of patients walked less than 350 m. The mean CAT score was 21.2. In 43.8% of patients, the impact of COPD on quality of life was high and in 13.5% the impact was very high. The mean BODEx index was 2.3. Regarding components of the BODEx index, the BMI was <21 kg/m2 in 11% of patients, FEV1 <50% in 22%, and at least three severe exacerbations in the previous 12 months were recorded in 6.8% of the patients.
In relation to COPD phenotypes, the non-exacerbator phenotype (42.2%, 95% CI 36.5–48.0) and the ACOS phenotype (21.7%, 95% CI 16.9%-26.4%) were the most frequent, followed by the exacerbator with chronic bronchitis phenotype (18.8%, 95% CI 14.2–23.3) and the exacerbator with emphysema phenotype (17.3%, 95% CI 12.9–21.7). The distribution of COPD phenotypes in relation to the study variables is summarized in Table 2. There were statistically significant differences in the distribution of phenotypes by sex, physician specialty, comorbidities, CAT score, impact on the quality of life, and COPD severity. The non-exacerbator phenotype was more frequently diagnosed by pneumologists versus primary care physicians, the mean number of comorbidities was higher in the exacerbator with chronic bronchitis phenotype, the mean CAT score was higher in the exacerbator with emphysema phenotype, and the lowest COPD severity was found in the non-exacerbator phenotype.
Table 2.
Distribution Of Clinical Characteristics In 286 Women With COPD According To COPD Phenotypes
| Variables | COPD Phenotypes | P value | |||
|---|---|---|---|---|---|
| Non-Exacerbator | ACOS | Exacerbator With Emphysema | Exacerbator With Chronic Bronchitis | ||
| Sex | |||||
| Male | 618 (47.9) | 167 (12.9) | 209 (16.2) | 296 (22.9) | 0.002 |
| Female | 117 (42.2) | 60 (21.7) | 48 (17.3) | 52 (18.8) | |
| Age, years | |||||
| 35–60 | 45 (44.5) | 22 (21.8) | 15 (14.8) | 19 (18.8) | 0.104 |
| 61–65 | 27 (44.3) | 14 (22.9) | 15 (24.6) | 5 (8.2) | |
| 66–75 | 29 (40.3) | 11 (15.3) | 11 (15.3) | 21 (29.2) | |
| > 75 | 13 (36.1) | 12 (33.3) | 5 (13.9) | 6 (16.7) | |
| Physician specialty | |||||
| Primary care | 35 (32.1) | 27 (24.8) | 19 (17.4) | 28 (25.7) | 0.0004 |
| Pneumology | 63 (57.3) | 17 (15.4) | 19 (17.3) | 11 (10.0) | |
| Smoking status | |||||
| Current smoker | 64 (43.5) | 25 (17.0) | 28 (19.0) | 30 (20.4) | 0.438 |
| Ex-smoker | 42 (40.4) | 27 (26.0) | 18 (17.3) | 17 (16.3) | |
| Never-smoker | 11 (44.0) | 8 (32.0) | 2 (8.0) | 4 (16.0) | |
| Comorbidities, mean (SD) | 1.77 (1.28) | 2.17 (1.51) | 1.92 (1.29) | 2.50 (1.57) | 0.03 |
| One | 31 (26.5) | 6 (10.0) | 12 (25.0) | 9 (17.1) | 0.281 |
| Two | 34 (29.1) | 18 (30.0) | 14 (29.2) | 16 (30.8) | |
| Three | 18 (15.4) | 13 (21.7) | 9 (18.7) | 13 (25.0) | |
| More than three | 13 (11.1) | 11 (18.3) | 6 (12.5) | 10 (19.2) | |
| CAT score, mean (SD) | 17.8 (8.2) | 23.6 (6.9) | 24.5 (9.0) | 22.4 (9.4) | < 0.001 |
| COPD impact according to CAT | |||||
| None, score < 5 | 8 (6.9) | 0 | 2 (4.3) | 3 (5.9) | < 0.001 |
| Low, score 5–9 | 13 (11.2) | 2 (3.3) | 1 (2.2) | 1 (2.0) | |
| Medium, score 10–20 | 49 (42.2) | 17 (28.3) | 8 (17.4) | 14 (27.4) | |
| High, score > 20 | 39 (33.6) | 32 (53.3) | 22 (47.8) | 24 (47.1) | |
| Very high, score > 30 | 7 (6.0) | 9 (15.0) | 13 (28.3) | 9 (17.6) | |
| BODEx index | |||||
| 0–2 points | 81 (57.4) | 30 (21.3) | 10 (7.1) | 20 (14.2) | < 0.001 |
| 3–4 points | 19 (24.7) | 15 (19.5) | 24 (31.2) | 19 (24.7) | |
| 5–6 points | 5 (20.0) | 5 (20.0) | 9 (36.0) | 6 (24.0) | |
| ≥ 7 points | 0 | 1 (50.0) | 0 | 1 (50.0) | |
Note: Data expressed as frequencies and percentages in parenthesis unless otherwise stated.
Abbreviations: ACOS, asthma-COPD overlap syndrome; CAT, COPD Assessment Test; BODEx, body mass index, airflow obstruction, dyspnea, and exacerbations.
As shown in Figure 1, differences in COPD phenotypes by sex were statistically significant (P = 0.002) with higher prevalence of non-exacerbator and exacerbator with chronic bronchitis phenotypes in men as compared with women; by contrast, the ACOS phenotype was more common in women than in men. On the other hand, the mean (SD) CAT score was similar in men than in women (20.8 [9.0] vs 21.2 [8.7], P = 0.481), as well as the impact of the disease on the quality of life (Figure 2). Sex-related differences according to smoking status were statistically significant (P < 0.001), with a higher percentage of men as compared with women in the groups of current smokers (56.2% and 53.3%, respectively) and ex-smokers (43.2% and 37.5%, respectively). Never-smokers were higher in women (9.1%) than in men (0.6%). The analysis of the number of comorbidities showed similar results in men (mean 2.01 [1.43], 95% CI 1.93–2.09) than in women (mean 1.99 [1.42], 95% CI 1.83–2.16) (P = 0.930). However, some comorbid diseases were more frequent in men as compared to women, including hypertension (64.8% vs 54.2%, P = 0.001), chronic ischemic heart disease (15.6% vs 7.9%, P = 0.001), and chronic heart failure (16.7% vs 10.2%, P = 0.01). Osteoporosis was significantly more frequent in women than in men (45.8% vs 11.7%, P < 0.001).
Figure 1.
Differences in the overall prevalence of COPD phenotypes between women and men.
Figure 2.
Impact of COPD in the patient’s quality of life according to the CAT score.
Discussion
This study carried out in a sample of 1610 patients with stable COPD attended in routine daily practice by pneumologists and primary care physicians in Spain shows a higher proportion of COPD males than females. Previous studies have shown that proportions of the population with diagnosed COPD are higher among males than females.23 This has been explained by the higher prevalence of smoking in males, which is the principal risk factor associated with COPD. In the past decade, however, a steady increase in COPD prevalence and age-adjusted death rates among women has been reported.7,24,25
Also, underdiagnosis of COPD has been consistently found, which is especially striking in patients with important risk factors for COPD attended in primary care.26,27 Underdiagnosis and misdiagnosis of COPD in both sexes have been related to different factors, including underuse of objective measures of lung function. Underdiagnosis in females is usually greater than in men. In a survey random sample of 192 primary-care physicians, a hypothetic case of cough and dyspnea in a smoker was presented in six versions differing only in the patent’s age and sex.28 COPD was given as the most probable diagnosis significantly more often for men than women (58% vs 42%, P < 0.05). The initial differences between sexes decreased as objective information was provided. After spirometry, COPD diagnosis rates for men and women were 74% vs 66% (P = NS), but interestingly, only 22% of physicians would have requested spirometry at initial presentation.28
We found that ACOS phenotype was the most frequent in women, which is in agreement with data reported in the literature.29–31 In a retrospective observational study of 499 patients with a diagnosis of COPD due to biomass or tobacco smoke, the ACOS phenotype was more common in the biomass group, although this difference disappeared when corrected for sex.32 Moreover, the percentage of never-smokers among women was higher than in men. Never-smokers comprise a substantial proportion of individuals with COPD. In an analysis of data from 14 countries that participated in the international, population-based Burden of Obstructive Lung Disease (BOLD) study, more than two-thirds of never-smokers with moderate to severe airway obstruction were women.33 In the IBERPOC cross-sectional study of a noninstitutionalized general population of 40–69 years of age from seven areas of different sizes and urban characteristics in Spain, non-smokers with COPD were more frequently women.34 It has been suggested that women are more susceptible to the effects of tobacco smoke, and there is evidence that exposure to environmental tobacco smoke is associated with COPD and affects women more often than men.35,36
The mean number of comorbid conditions was similar in men than in women, but concomitant cardiovascular disorders were significantly more frequent in male patients. Metabolic comorbidities, i.e. osteoporosis, were significantly more common in women. Comorbidities complicate the management of COPD and contribute to increased hospitalization and health care costs.37 Cardiovascular comorbidities, particularly coronary heart disease, heart failure, and COPD, are diseases with very similar risk factors especially through the role of smoking. Coexistence of COPD and either coronary heart disease and heart failure worsens the prognosis of each disease.37 Also, patients with COPD are at increased risk of osteoporosis. In a systematic review of 13 studies with a total of 775 COPD patients, the overall mean prevalence of osteoporosis was 35.1%, with a higher proportion of women.38
We also identified a clinical profile of women with COPD who were current smokers, with overweight and obesity but at low risk regarding pulmonary function and clinical symptoms (40% with dyspnea grade 1 mMRC scale), but with a notable percentage (39%) with two or more moderate-severe exacerbations in the previous year. Despite these characteristics, the severity of COPD was mild/moderate in 87.4% of women according to the BODEx index. However, following the risk profiles of COPD outlined in the 2017 Spanish COPD guidelines (GesEPOC),39 this majority of patients would move to high-risk level because of exacerbations or GOLD groups B and D due to exacerbations and/or CAT scores.40
The impact of COPD in women is understudied but the evidence that does exist reveals potentially substantial sex differences in susceptibility, severity, and clinical profile of the disease.41 The greater prevalence of COPD and related mortality reported for men in earlier epidemiological studies may be due to underdiagnosis of women. In addition, factors such as prevalence of symptoms, triggering stimuli, susceptibility to smoking, frequency of exacerbations, impairment in quality of life, and presence of comorbidities (e.g. malnutrition, depression, osteoporosis) are more frequently seen in women with COPD.42,43 Results of the BODEx index and 6-min walking test were as expected in a population of symptomatic COPD. Despite these differences, the current guidelines for the diagnosis and treatment of men or women with COPD are the same. Therefore, health care professionals should be particularly aware to recognize the sex differences in patients with COPD to optimize assessment, monitoring and treatment of this disease. In an excellent review of the management of COPD in women, Jenkins et al.44 present key suggestions to address the sex bias that exist among COPD patients, especially the need of further research to identify the factors influencing attitudes and coping strategies for women with COPD to enable improvements in care, the assessment of sex-specific effects of various interventions and sex-specific differences in response to treatment, and the promotion of better awareness within the health care community of the increasing burden of COPD in women to improve disease diagnosis and treatment.
The present results should be interpreted taking into account some limitations of the study, such as the cross-sectional design, the relative small number of women in the study population, and the fact that women and men were not matched by age and COPD severity. Another limitation is the lack of a control group, which could mislead results by showing differences that are not related to COPD presentation. In relation to the recruitment process, although the number of practices was not recorded, the participating physicians worked in primary health care centers distributed in 16 out of the total 17 autonomous communities of the country, so that a recruitment bias associated with geographical location seems unlikely. The reason for consultation was not registered, but it seems very likely that patients had been recruited during a follow-up visit in the context of the usual care in patients with COPD. Also, the influence of recent changes of COPD guidelines regarding definitions of severity, classification of risk groups, or phenotypes in the study population was unknown. The small number of cases when variables are divided into different subgroups is a limitation of the statistical analysis. Patients were on treatment at the time of enrollment for which it is unknown whether any phenotype could have been changed at the time of assessment. However, data recorded were obtained in a non-trial setting, which enhances the external validity of the study.
Conclusion
This study provides evidence of the clinical characteristics of women with COPD attended in the primary and specialized care in routine daily practice in Spain and is important for primary care clinicians in order to improve COPD awareness in women in which underdiagnosis is very common. Differences in the prevalence rates of COPD phenotypes between men and women have been documented, with ACOS particularly frequent in female patients. Lung function impairment, COPD severity, and impact of COPD on the patient’s quality of life were apparently similar in men and women. The number of concurrent comorbidities was also similar, but individual disorders affected differently according to sex, with cardiovascular diseases more frequently present in men and osteoporosis in women. In the pattern of smoking habit, the percentage of never-smokers was significantly higher in women. This study highlights the impact of COPD in women and the importance of continuing sex-based research in tobacco-related respiratory diseases.
Acknowledgments
The authors thank Marta Pulido, MD, PhD, for editing the manuscript and editorial assistance. This study was founded by Grupo Ferrer, Barcelona, Spain.
Disclosure
Dr Alcázar-Navarrete reports personal fees from GSK; grants, personal fees, and non-financial support from Novartis AG; personal fees and non-financial support from Boehringer Ingelheim and Chiesi; grants, personal fees, and non-financial support from Laboratorios Menarini; grants, personal fees, non-financial support from Laboratorios Ferrer; personal fees, non-financial support from Laboratorios Rovi; and personal fees from Gebro and Astra-Zeneca, outside the submitted work. In addition, Dr Alcázar-Navarrete has a patent P201730724 licensed. Ms Anna Campuzano and Joselín Pérez are full-time employees at Grupo Ferrer Internacional, Spain. The remaining authors report no conflicts of interest to be disclosed in this work.
References
- 1.Viegi G, Pistelli F, Sherrill DL, Maio S, Baldacci S, Carrozzi L. Definition, epidemiology and natural history of COPD. Eur Respir J. 2007;30(5):993–1013. doi: 10.1183/09031936.00082507 [DOI] [PubMed] [Google Scholar]
- 2.Guarascio AJ, Ray SM, Finch CK, Self TH. The clinical and economic burden of chronic obstructive pulmonary disease in the USA. Clincoecon Outcomes Res. 2013;5:235–245. doi: 10.2147/CEOR.S34321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miravitlles M, Ribera A. Understanding the impact of symptoms on the burden of COPD. Respir Res. 2017;18:67. doi: 10.1186/s12931-017-0548-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.GBD. 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5(9):691–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsiligianni I, Román Rodríguez M, Lisspers K, LeeTan T, Infantino A. Call to action: improving care for women with COPD. Prim Care Respir Med. 2017;27:11. doi: 10.1038/s41533-017-0013-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mannino DM, Gagnon RC, Petty TL, Lydick E. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2000;160(11):1683–1689. [DOI] [PubMed] [Google Scholar]
- 7.Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance–United States, 1971–2000. MMWR Surveill Summ. 2002;51(6):1–16. [PubMed] [Google Scholar]
- 8.Laviolette L, Lacasse Y, Doucet M, et al. Chronic obstructive pulmonary disease in women. Can Respir J. 2007;14(2):93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ställberg B, Janson C, Johansson G, et al. Management, morbidity and mortality of COPD during an 11-year period: an observational retrospective epidemiological register study in Sweden (PATHOS). Prim Care Respir J. 2014;23(1):38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ntritsos G, Franek J, Belbasis L, et al. Sex-specific estimates of COPD prevalence: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2018;13:1507–1514. doi: 10.2147/COPD.S146390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ancochea J, Miravitlles M, García-Río F, et al. Underdiagnosis of chronic obstructive pulmonary disease in women: quantification of the problem, determinants and proposed actions. Arch Bronconeumol. 2013;49(6):223–229. doi: 10.1016/j.arbres.2012.11.010 [DOI] [PubMed] [Google Scholar]
- 12.Miravitlles M, Soriano JB, García-Río F, et al. Prevalence of COPD in Spain: impact of undiagnosed COPD on quality of life and daily life activities. Thorax. 2009;64(10):863–868. doi: 10.1136/thx.2009.115725 [DOI] [PubMed] [Google Scholar]
- 13.DeMeo DL, Ramagopalan S, Kavati A, et al. Women manifest more severe COPD symptoms across the life course. Int J Chron Obstruct Pulmon Dis. 2018;13:3021–3029. doi: 10.2147/COPD.S160270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hardin M, Foreman M, Dransfield MT, et al. Sex-specific features of emphysema among current and former smokers with COPD. Eur Respir J. 2016;47(1):104–112. doi: 10.1183/13993003.00996-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sansores RH, Ramírez-Venegas A. COPD in women: susceptibility or vulnerability? Eur Respir J. 2016;47(1):19–22. doi: 10.1183/13993003.01781-2015 [DOI] [PubMed] [Google Scholar]
- 16.Alcázar-Navarrete B, Trigueros JA, Riesco JA, Campuzano A, Pérez J. Geographic variations of the prevalence and distribution of COPD phenotypes in Spain: “the ESPIRAL-ES study”. Int J Chron Obstruct Pulmon Dis. 2018;13:1115–1124. doi: 10.2147/COPD.S158031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Global strategy for the diagnosis, management and prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2014. Available from: http://www.goldcopd.org Accessed September15, 2016.
- 18.Miravitlles M, Soler-Cataluña JJ, Calle M, et al. Spanish COPD guidelines (GesEPOC): pharmacological treatment of stable COPD. Spanish Society of Pulmonology and Thoracic Surgery. Arch Bronconeumol. 2012;48(7):247–257. doi: 10.1016/j.arbres.2012.04.001 [DOI] [PubMed] [Google Scholar]
- 19.Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest. 1988;93(3):580–586. doi: 10.1378/chest.93.3.580 [DOI] [PubMed] [Google Scholar]
- 20.Soler-Cataluña JJ, Martínez-García MA, Sánchez Sánchez L, Perpiñá Tordera M, Román Sánchez P. Severe exacerbations and BODE index: two independent Risk factors for death in male COPD patients. Respir Med. 2009;103(5):692–699. doi: 10.1016/j.rmed.2008.12.005 [DOI] [PubMed] [Google Scholar]
- 21.Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD assessment test. Eur Respir J. 2009;34(3):648–654. doi: 10.1183/09031936.00102509 [DOI] [PubMed] [Google Scholar]
- 22.Soler-Cataluña JJ, Cosío B, Izquierdo JL, et al. Consensus document on the overlap phenotype COPD-asthma in COPD. Arch Bronconeumol. 2012;48(9):331–337. doi: 10.1016/j.arbres.2011.12.009 [DOI] [PubMed] [Google Scholar]
- 23.British Lung Foundation. Chronic obstructive pulmonary disease statistics. Available from: https://statistics.blf.org.uk/copd Accessed January24, 2019.
- 24.Ford ES, Croft JB, Mannino DM, Wheaton AG, Zhang X, Giles WH. COPD surveillance–United States, 1999–2011. Chest. 2013;144(1):284–305. doi: 10.1378/chest.13-0809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chronic obstructive pulmonary disease. Data and statistics. Available from: https://www.cdc.gov/copd/data.html Accessed January24, 2019.
- 26.Buist AS, McBurnie MA, Vollmer WM, et al. International variation in the prevalence of COPD (the BOLD study): a population-based prevalence study. Lancet. 2007;370(9589):741–750. doi: 10.1016/S0140-6736(07)61377-4 [DOI] [PubMed] [Google Scholar]
- 27.Hill K, Goldstein RS, Guyatt GH, et al. Prevalence and underdiagnosis of chronic obstructive pulmonary disease among patients at risk in primary care. CMAJ. 2010;182(7):673–678. doi: 10.1503/cmaj.091784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chapman KR, Tashkin DP, Pye DJ. Sex bias in the diagnosis of COPD. Chest. 2001;119(6):1691–1695. doi: 10.1378/chest.119.6.1691 [DOI] [PubMed] [Google Scholar]
- 29.Wheaton AG, Pleasants RA, Croft JB, et al. Sex and asthma-chronic obstructive pulmonary disease overlap syndrome. J Asthma. 2016;53(7):720–731. doi: 10.3109/02770903.2016.1154072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koblizek V, Milenkovic B, Barczyk A, et al. Phenotypes of COPD patients with a smoking history in Central and Eastern Europe: the POPE Study. Eur Respir J. 2017;49(5):1601446. doi: 10.1183/13993003.01446-2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mindus S, Malinovschi A, Ekerljung L, et al. Asthma and COPD overlap (ACO) is related to a high burden of sleep disturbance and respiratory symptoms: results from the RHINE and Swedish GA2LEN surveys. PLoS One. 2018;13(4):e0195055. doi: 10.1371/journal.pone.0195055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Golpe R, Sanjuán López P, Cano Jiménez E, Castro Añón O, Pérez de Llano LA. Distribution of clinical phenotypes in patients with chronic obstructive pulmonary disease caused by biomass and tobacco smoke. Arch Bronconeumol. 2014;50(8):318–324. doi: 10.1016/j.arbres.2013.12.013 [DOI] [PubMed] [Google Scholar]
- 33.Lamprecht B, McBurnie MA, Vollmer WM, et al. COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest. 2011;139(4):752–763. doi: 10.1378/chest.10-1253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miravitlles M, Ferrer M, Pont A, et al. Characteristics of a population of COPD patients identified from a population-based study. Focus on previous diagnosis and never smokers. Respir Med. 2005;99(8):985–995. doi: 10.1016/j.rmed.2005.01.012 [DOI] [PubMed] [Google Scholar]
- 35.Iribarren C, Friedman GD, Klatsky AL, Eisner MD. Exposure to environmental tobacco smoke: association with personal characteristics and self reported health conditions. J Epidemiol Community Health. 2001;55(10):721–728. doi: 10.1136/jech.55.10.721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Larsson ML, Loit HM, Meren M, et al. Passive smoking and respiratory symptoms in the FinEsS study. Eur Respir J. 2003;21(4):672–676. doi: 10.1183/09031936.03.00033702 [DOI] [PubMed] [Google Scholar]
- 37.Cavaillès A, Brinchault-Rabin G, Dixmier A, et al. Comorbidities of COPD. Eur Respir Rev. 2013;22(130):454–475. doi: 10.1183/09059180.00008612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Graat-Verboom L, Wouters EF, Smeenk FW, van Den Borne BE, Lunde R, Spruit MA. Current status of research on osteoporosis in COPD: a systematic review. Eur Respir J. 2009;34(1):209–218. [DOI] [PubMed] [Google Scholar]
- 39.Miravitlles M, Soler-Cataluña JJ, Calle M, et al. Spanish guidelines for management of chronic obstructive pulmonary disease (GesEPOC) 2017. Pharmacological treatment of stable phase. Arch Bronconeumol. 2017;53(6):324–335. [DOI] [PubMed] [Google Scholar]
- 40.Global Initiative for chronic obstructive lung disease. Pocket guide to COPD diagnosis, management, and prevention. A guide for health care professionals. 2018 Report. Available from: https://goldcopd.org/wp-content/uploads/2018/02/WMS-GOLD-2018-Feb-Final-to-print-v2.pdf Accessed January4, 2019.
- 41.Varkey AB. Chronic obstructive pulmonary disease in women: exploring sex differences. Curr Opin Pulm Med. 2004;10(2):98–103. [DOI] [PubMed] [Google Scholar]
- 42.Cote CG, Chapman KR. Diagnosis and treatment considerations for women with COPD. Int J Clin Pract. 2009;63(3):486–493. [DOI] [PubMed] [Google Scholar]
- 43.Rodríguez-González Moro JM, Izquierdo JL, Antón E, de Lucas P, Martín A. Health-related quality of life in outpatient women with COPD in daily practice: the MUVICE Spanish study. Respir Med. 2009;103(9):1303–1312. [DOI] [PubMed] [Google Scholar]
- 44.Jenkins CR, Chapman KR, Donohue JF, Roche N, Tsiligianni I, Han MK. Improving the management of COPD in women. Chest. 2017;151(3):686–696. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Global strategy for the diagnosis, management and prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2014. Available from: http://www.goldcopd.org Accessed September15, 2016.