Abstract
Objective
Physicochemical approach such as strong ion difference provides a novel concept in understanding and managing acid–base disturbance in patients. However, its application in pediatrics is limited. This study aimed to evaluate a correlation between the physicochemical approach and blood gas pH for acid–base determination in critically ill pediatric patients.
Results
A total of 130 pediatric patients were included, corresponding to 1338 paired measures for analyses. Of these, the metabolic subgroup (743 paired measures) was defined. Among physicochemical parameters, the effective strong ion difference showed the best correlation with the blood gas pH in the whole cohort (R = 0.398; p < 0.001) and the metabolic subgroup (R = 0.685; p < 0.001). Other physicochemical parameters (i.e., the simplified and the apparent strong ion difference, the strong ion gap, and the sodium chloride gap) and the traditional measures (standard base excess, lactate, chloride and bicarbonate) also showed varying degrees of correlation. This study revealed the positive correlation between physicochemical parameters and the blood gas pH, serving as a connecting dot for further investigations using physicochemical approach to evaluate acid–base disturbance in pediatric population.
Keywords: Acidosis, Alkalosis, Blood gas, Pediatrics, Strong ion difference
Introduction
Acid–base disturbances, more specifically metabolic acidosis, is one of most concerning issues found in most, if not all, critically ill patients which affect morbidity and mortality. Our understanding of acid–base physiology is continually evolving. From Latin origin of the word ‘acidus’ (sour taste) to Brønsted and Lowry’s definition of acid as substances that can donate a proton (H+) in 1923 and Henderson–Hasselbalch formula of the relationship between serum bicarbonate, pCO2, and pH in 1916. New understanding provides scientists and clinicians insight into the acid–base as tools to understand and treat patient’s acid–base disturbance [1].
The traditional approach of acid–base disturbances by Henderson–Hasselbalch has specific weaknesses that need to be addressed. First, there are non-bicarbonate buffers such as hemoglobin and albumin, which frequently alters in the intensive care setting. Thus, a change in bicarbonate alone might not truly reflect the total amount of non-respiratory acids and bases [2, 3]. Another traditional approach involves a concept of buffer base which takes into account of all plasma buffer anions and non-volatile, weak acid buffers (albumin and phosphate) as well as consideration of hemoglobin as a buffer [4, 5]. By incorporating these buffers, it yields the concept of base excess (BE) which represents the amount of alkali or acid that need to be added to 1 L of oxygenated blood at pCO2 of 40 mmHg to obtain pH of 7.4 [5]. BE might suffer inaccuracy due to pCO2 changes across extracellular fluid space. Thus the term of standard base excess (SBE) was introduced after standardizing the effect of hemoglobin on CO2 titration. Moreover, BE and SBE equation assumes normal non-buffer ions such that of albumin and phosphate. The decrease in these buffers might result in unstable BE and SBE [6].
A more recent physicochemical approach to acid–base status, introduced by Peter Stewart in 1978, challenge clinician’s understanding of acid–base physiology of human body fluid [7]. With the principle of electroneutrality and the conservation of mass, Stewart proposed that the acid–base status of body fluid is determined by three independent variables, pCO2, concentration of total weak acid (ATOT), and strong ion difference (SID), rather than serum bicarbonates, which are dependent variables [7, 8]. Since then, the physicochemical approach had been applied to understanding and treatment of various acid–base disorders. Several studies were conducted in attempt to compare the physicochemical approach with the traditional approaches in term of diagnostic abilities for classification of acid–base disorders and in the determination of prognosis in critically ill patients [2, 9–13]. Few studies were done using both traditional and physicochemical approach in the determination of acid–base disturbances in critically ill pediatric patients [1, 14, 15]. Most of this evidence, nonetheless, were based on data from adult population and the application of the physicochemical approach in pediatric patients is scant.
This study aimed to provide direct evidence of the correlation between several physicochemical approaches with blood pH in order to illustrate its importance in acid–base disorders determination in critically ill pediatric patients. The base excess model and the traditional approach of acid–base determinations were also evaluated.
Main text
Methods
Study design
This retrospective, observational study collected clinical data and laboratory results from Electronic Medical Records of pediatric patients with the age of 1 month to 15 years who were admitted to pediatric intensive care unit (PICU) at Ramathibodi Hospital during 2014–2016. Patient characteristics including age, gender, the cause of PICU admission as well as the laboratory results were reviewed. The laboratory data of a simultaneous collection of blood gas analysis (e.g., pH, pCO2, pO2) and blood chemistry (i.e., [Na+], [K+], [Cl−], [HCO3−], [Ca2+], [Mg2+], [PO4−], arterial lactate, and albumin), so-called the paired specimen, were collected. The Ethic Committee of Ramathibodi Hospital, Mahidol University approved this study, and informed consent was waived due to the retrospective nature of the study (protocol ID 10-57-07).
Correlation analysis was performed on the basis of the whole cohort (using all collected samples from the paired specimens) and the subgroup of metabolic acidosis or alkalosis. To exclude data with primary respiratory acid–base disturbance, in which the pH change is directly affected by carbon dioxide but not the organic/inorganic ions, any sample that show the acidic pH (< 7.4) with high HCO3− (> 24 mmol/L) and the basic pH (> 7.4) with low HCO3− (< 24 mmol/L) were excluded. The remaining samples were then analyzed as the metabolic subgroup.
Evaluation of acid–base parameters
The simplified SID and the apparent SID (SIDa) are depended on the difference between the measured strong cations and anions which represent the unmeasured anions and thus directly correlates with [H+] as dictated by the law of electroneutrality. The effective SID (SIDe) observes the relationship among the measured pH, bicarbonate, albumin, and phosphate, as well as the effect of remaining anions, to estimate the unmeasured cations. Increase in the simplified SID, SIDa, and SIDe would correlates with alkalosis and decrease in these parameters would signifies acidosis in patients. These physicochemical parameters were calculated as follows [2, 16, 17];
The strong ion gap (SIG) is the difference between the unmeasured anions and cations which were estimated from SIDa and SIDe, respectively. Increase in SIG suggests the presence of unmeasured anions. SIG was determined by the following equation;
The sodium chloride (Na–Cl) gap can be considered as the SID surrogate and was calculated by the following equation;
Standard base excess (SBE), arterial lactate, serum bicarbonate and serum chloride were included to serve as a traditional approach for evaluation of acid–base disturbances. SBE was calculated from the measured pH and HCO3− as following;
Statistical analysis
Sample size was calculated using G*Power program (http://www.gpower.hhu.de) with alpha = 0.05, power = 0.95, and the effect size of 0.1021 obtained from the preliminary data of the measured pH and the simplified SID (21 patients; 105 samples). As a result, the estimated sample size of 130 would be sufficient to observe the significant correlation between the measured pH and the strong ion difference.
Data were presented as frequency (percentage), mean ± SD, median [IQR] as appropriate. Pearson correlation (R) and the coefficient of determination (R2) between the measured pH and the physicochemical parameters were obtained by SPSS statistics 17.0. p-value < 0.05 was considered statistically significant.
Results
A total of 1338 paired measures were obtained from 130 pediatric patients who admitted to PICU of Ramathibodi Hospital during 2014–2016. After exclusion of acid–base disturbances from respiratory causes, a total of 743 paired measures was subjected to the metabolic subgroup analysis. The demographic data was illustrated in Table 1. Of these patients, the most common causes of PICU admission were severe sepsis or septic shock (17.7%) and postoperative care (29.2%). Approximately 50% of patients had one or more organ failures at the time of PICU admission.
Table 1.
Demographic data of patients whose laboratory results were included in the study
| Patient characteristics | Total n = 130 patients |
|---|---|
| Male gender, n (%) | 61 (47) |
| Age (year), median [IQR] | 5.0 [2, 10] |
| The cause of PICU admission, n (%) | |
| Severe sepsis or septic shock | 23 (17.7) |
| Hypovolemic or hemorrhagic shock | 4 (3.1) |
| Anaphylaxis or distributive shock | 1 (0.8) |
| Heart failure or cardiogenic shock | 8 (6.2) |
| Post-cardiac arrest | 4 (3.1) |
| Respiratory failure | 18 (13.8) |
| Liver failure or hepatic encephalopathy | 3 (2.3) |
| Upper gastrointestinal bleeding | 5 (3.9) |
| Renal failure | 3 (2.3) |
| Diabetes ketoacidosis | 2 (1.5) |
| Organic acidemia | 1 (0.8) |
| Status epilepticus | 8 (6.2) |
| Post-operative | 38 (29.1) |
| Others | 12 (9.2) |
| Numbers of paired specimen per patient, median [IQR] | 6 [2, 14] |
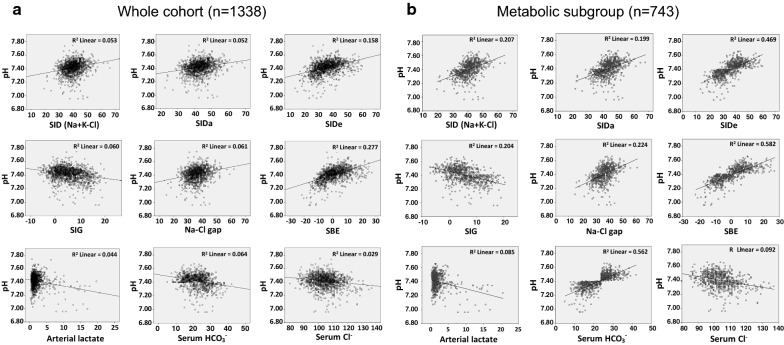
Among acid–base parameters that based on the physicochemical properties, SIDe showed the greatest correlation with the measured pH in the whole cohort (R2 = 0.158; Fig. 1a) and the metabolic subgroup analyses (R2 = 0.469; Fig. 1b). The simplified SID, SIDa, SIG, and Na–Cl gap also had positive, even though weaker, correlation with the measured pH (Fig. 1a, b). The traditional acid–base parameter that demonstrated the best correlation with the measured pH was SBE with R2 = 0.277 from the whole cohort and R2 = 0.582 from the metabolic subgroup (Fig. 1a, b). Interestingly, serum HCO3− which has been routinely used as a convenient screening of acid–base disturbances, showed a small degree of correlation with the measured pH in the whole cohort analysis (R2 = 0.171), but not the metabolic subgroup (R2 = 0.562). Note that there was absence to low correlation between the measured pH and serum chloride or the arterial lactate in this study (Fig. 1a, b). Pearson correlation (R) and significant assessment of all acid–base parameters were summarized in Table 2, in which the data corresponded with those of Fig. 1a, b.
Fig. 1.
Linear correlation between the measured pH and various acid–base parameters. a the whole cohort analysis (n = 1338 samples). b the metabolic subgroup analysis (n = 743 samples). The coefficient of determination (R2) was shown for each pair
Table 2.
Pearson correlation between the measured pH and various acid–base parameters
| Whole cohort (n = 1338 samples) R (sig 2-tailed) |
Metabolic subgroup (n = 743 samples) R (sig 2-tailed) |
|
|---|---|---|
| SID | 0.230 (< 0.001) | 0.455 (< 0.001) |
| SIDa | 0.227 (< 0.001) | 0.446 (< 0.001) |
| SIDe | 0.398 (< 0.001) | 0.685 (< 0.001) |
| SIG | − 0.245 (< 0.001) | − 0.452 (< 0.001) |
| Na–Cl gap | 0.247 (< 0.001) | 0.473 (< 0.001) |
| SBE | 0.526 (< 0.001) | 0.763 (< 0.001) |
| Arterial lactate | − 0.210 (< 0.001) | − 0.292 (< 0.001) |
| Serum HCO3− | 0.413 (< 0.001) | 0.749 (< 0.001) |
| Serum Cl− | − 0.170 (< 0.001) | − 0.303 (< 0.001) |
Discussion
Since the physicochemical approach to acid–base status was introduced by Peter Stewart in 1981, it had been subjected to several studies, update, and refinement [7, 8, 18, 19]. However, most of the studies and clinical applications using the physicochemical approach were restricted to adult subjects [1, 2, 9–13]. There were studies showing promises of physicochemical approach in pediatric population [14, 15, 20–22]; however, those studies focused only on the association between physicochemical parameters and the clinical endpoints, but not the correlation with the measured pH directly. This study, therefore, investigated the correlation between the measured pH from blood gas analysis and several physicochemical parameters in critically ill pediatric population.
The degree of correlation varied among parameters, with SBE showing the greatest correlation with the measured pH while the single parameters such that of serum chloride and arterial lactate revealed the least association. This might reflect that single parameter alone might not be adequate in term of determination of complex acid and base disturbances in PICU. The SIDe showed the best correlation regarding physicochemical approach; nevertheless, this parameter involved with a complicated equation. In a practical standpoint, the simplified SID and Na–Cl gap which showed moderate correlation with the measured pH, especially in the metabolic subgroup, might be applicable as the convenient screening tools of acid–base derangement.
Our findings supported a possibility that Stewart’s physicochemical approach is applicable as a tool to preliminarily evaluate acid–base status in pediatric patients, mainly where arterial puncture and blood gas analysis are not commonly performed. The correlation between the measured pH and the physicochemical parameters were stronger than that of serum bicarbonate, particularly in the metabolic subgroup. Nonetheless, the SIDe and SIG still need the measured pH in their formula, and the calculation is very complicated. Only the simplified SID, SIDa, and the Na–Cl gap should be considered as the sole physicochemical approach, which is convenient at the bedside applications. Of these, the Na–Cl gap exhibited a higher correlation with the measured pH than the simplified SID and SIDa. The applicability and feasibility of the Na–Cl gap in replacement of serum bicarbonate as the screening tool of acid–base disturbances in pediatric patients should also be evaluated in the future.
In conclusion, this study provided direct evidence of the positive correlation between physicochemical parameter and blood pH in pediatric subjects. We hope this finding will encourage more study utilizing the physicochemical approach of acid–base status in pediatric patients.
Limitations
No clinical correlation (i.e., the length of PICU and hospital stay, morbidity or mortality) with the acid–base determination using physicochemical approach was observed in this study.
Supplementary information
Additional file 1: Table S1. Raw data of the measured pH from blood gas analysis and physicochemical parameters in the whole cohort (n = 1338 samples).
Additional file 2: Table S2. Raw data of the measured pH from blood gas analysis and physicochemical parameters in the metabolic subgroup (n = 743 samples).
Acknowledgements
The authors thank Professor Duangrudee Wattanasirichaigoon, Department of Pediatrics, Faculty of Medicine Ramathibodi Hospital for her strong support and Dr. Arpa Chutipongtanate, Department of Anesthesiology, Faculty of Medicine Ramathibodi Hospital for a critical discussion. PM was a pediatric resident during the research activity. This study was supported by Department of Pediatrics, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Thailand. SC was financially supported by the Faculty Staff Development Program of Faculty of Medicine Ramathibodi Hospital, Mahidol University, for his research activities.
Abbreviations
- PICU
pediatric intensive care unit
- SID
strong ion difference
- SIDa
apparent strong ion difference
- SIDe
effective strong ion difference
- SBE
standard base excess
Authors’ contributions
SC initiated the conception. RL and SC developed the design. PM collected the data. CC and PM analyzed the data, prepared the figures and tables. CC wrote the first draft of the manuscript. PM, RL, SC revised the manuscript. RL and SC finalized the manuscript. All authors read and approved the final manuscript.
Funding
No funding was received.
Availability of data and materials
The datasets containing the blood gas pH and physicochemical parameters from the whole cohort (n = 1338) and the metabolic subgroup (n = 743) that support the findings of this study are made available as Additional files 1, 2.
Ethics approval and consent to participate
This study was approved by the Ethic Committee of Ramathibodi Hospital, Mahidol University (protocol ID 10-57-07). Informed consent was waived due to the retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Rojjanee Lertbunrian, Email: lrojjanee@hotmail.com.
Somchai Chutipongtanate, Email: schuti.rama@gmail.com, Email: somchai.chu@mahidol.edu.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13104-019-4770-6.
References
- 1.Rastegar A. Clinical utility of Stewart’s method in diagnosis and management of acid-base disorders. Clin J Am Soc Nephrol. 2009;4(7):1267–1274. doi: 10.2215/CJN.01820309. [DOI] [PubMed] [Google Scholar]
- 2.Kimura S, Shabsigh M, Morimatsu H. Traditional approach versus Stewart approach for acid-base disorders: inconsistent evidence. SAGE Open Med. 2018;6:1–9. doi: 10.1177/2050312118801255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hughes R, Brain MJ. A simplified bedside approach to acid-base: fluid physiology utilizing classical and physicochemical approaches. Anaesth Intens Care Med. 2013;14(10):445–452. doi: 10.1016/j.mpaic.2013.07.013. [DOI] [Google Scholar]
- 4.Singer RB, Hastings AB. An improved clinical method for the estimation of disturbances of the acid-base balance of human blood. Medicine (Baltimore). 1948;27(2):223–242. doi: 10.1097/00005792-194805000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Siggard-Andersen O. The van Slyke equation. Scand J Clin Lab Invest Suppl. 1977;146:15–20. doi: 10.3109/00365517709098927. [DOI] [PubMed] [Google Scholar]
- 6.Stewart PA. How to understand acid-base: a quantitative acid-base primer for biology and medicine. New York: Elsevier North Holland Inc; 1981. [Google Scholar]
- 7.Stewart PA. Independent and dependent variables of acid-base control. Respir Physiol. 1978;33(1):9–26. doi: 10.1016/0034-5687(78)90079-8. [DOI] [PubMed] [Google Scholar]
- 8.Kellum JA, Elbers PWG, Stewart PA. Stewart’s textbook of acid-base. London: Lulu Enterprises; 2009. [Google Scholar]
- 9.Zheng CM, Liu WC, Zheng JQ, Liao MT, Ma WY, Hung KC, et al. Metabolic acidosis and strong ion gap in critically ill patients with acute kidney injury. Biomed Res Int. 2014;2014:819528. doi: 10.1155/2014/819528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dubin A, Menises MM, Masevicius FD, Moseinco MC, Kurtscherauer DO, Ventrice E, et al. Comparison three different methods of evaluation of metabolic acid-base disorders. Crit Care Med. 2007;35(5):1264–1270. doi: 10.1097/01.CCM.0000259536.11943.90. [DOI] [PubMed] [Google Scholar]
- 11.Fencl V, Jabor A, Kazda A, Figge J. Diagnosis of metabolic acid-base disturbances in critically ill patients. Am J Respir Crit Care Med. 2000;162(6):2246–2251. doi: 10.1164/ajrccm.162.6.9904099. [DOI] [PubMed] [Google Scholar]
- 12.Cusack RJ, Rhodes A, Lochhead P, Jordan B, Perry S, Ball JA, et al. The strong ion gap does not have prognostic value in critically ill patients in a mixed medical/surgical adult ICU. Intensive Care Med. 2002;28(7):864–869. doi: 10.1007/s00134-002-1318-2. [DOI] [PubMed] [Google Scholar]
- 13.Ratanarat R, Sodapak C, Poomphichet A, Toomthong P. Use of different approaches of acid-base derangement to predict mortality in critically ill patients. J Med Assoc Thai. 2013;96(Suppl 2):S216–S223. [PubMed] [Google Scholar]
- 14.Balasubramanyan N, Havens PL, Hoffman GM. Unmeasured anions identified by the Fencl-Stewart method predict mortality better than base excess, anion gap, and lactate in patients in the pediatric intensive care unit. Crit Care Med. 1999;27(8):1577–1581. doi: 10.1097/00003246-199908000-00030. [DOI] [PubMed] [Google Scholar]
- 15.Durward A, Tibby SM, Skelett S, Austin C, Anderson D, Murdoch IA. The strong ion gap predicts mortality in children following cardiopulmonary bypass. Pediatr Crit Care Med. 2005;6(3):281–285. doi: 10.1097/01.PCC.0000163979.33774.89. [DOI] [PubMed] [Google Scholar]
- 16.Van Regenmortel N, Verbrugghe W, Van de Wyngaert T, Jorens PG. Impact of chloride and strong ion difference on ICU and hospital mortality in a mixed intensive care population. Ann Intensive Care. 2016;6(1):91. doi: 10.1186/s13613-016-0193-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ronco C, Kellum JA, Bellomo R, Ricci Z. Critical care nephrology. 3. Philadelphia: Elsevier, Inc.; 2019. [Google Scholar]
- 18.Story DA. Stewart acid-base: a simplified bedside approach. Anesth Analg. 2016;123(2):511–515. doi: 10.1213/ANE.0000000000001261. [DOI] [PubMed] [Google Scholar]
- 19.Kishen R, Honore PM, Jacobs R, Joannes-Boyau O, De Waele E, De Regt J, et al. Facing acid-base disorders in the third millennium—the Stewart approach revisited. Int J Nephrol Renovasc Dis. 2014;7:209–217. doi: 10.2147/IJNRD.S62126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kurt A, Ecevit A, Ozkiraz S, Ince DA, Akcan AB, Tarcan A. The use of chloride-sodium ratio in the evaluation of metabolic acidosis in critically ill neonates. Eur J Pediatr. 2012;171(6):963–969. doi: 10.1007/s00431-011-1666-4. [DOI] [PubMed] [Google Scholar]
- 21.Sen S, Wiktor A, Berndtson A, Greenhalgh D, Palmieri T. Strong ion gap is associated with mortality in pediatric burn injuries. J Burn Care Res. 2014;35(4):337–341. doi: 10.1097/BCR.0000000000000043. [DOI] [PubMed] [Google Scholar]
- 22.Hatherill M, Waggie Z, Purves L, Reynolds L, Argent A. Mortality and the nature of metabolic acidosis in children with shock. Intensive Care Med. 2003;29(2):286–291. doi: 10.1007/s00134-002-1585-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Raw data of the measured pH from blood gas analysis and physicochemical parameters in the whole cohort (n = 1338 samples).
Additional file 2: Table S2. Raw data of the measured pH from blood gas analysis and physicochemical parameters in the metabolic subgroup (n = 743 samples).
Data Availability Statement
The datasets containing the blood gas pH and physicochemical parameters from the whole cohort (n = 1338) and the metabolic subgroup (n = 743) that support the findings of this study are made available as Additional files 1, 2.