Abstract
Purpose:
There are few reports of refractive surgery on human immunodeficiency virus-positive (HIV+) patients; we sought to assess the frequency of refractive surgery complications in HIV+ individuals and related risk factors.
Settings:
Multiple centers in the United States
Design:
Prospective observational cohort study
Methods:
The U.S. Military HIV Natural History Study is a prospective observational cohort study of HIV+ Servicemembers and beneficiaries. Participants were selected who had CPT codes for LASIK, PRK, and other refractive surgeries. The frequency of complications was determined using ICD-9 codes. Covariates included age, gender, antiretroviral therapy, time since HIV diagnosis, history of AIDS, and CD4 and viral load. Statistical analysis was completed using univariate (Chi-square and Wilcoxon-Mann-Whitney tests) and multivariate analyses.
Results:
Seventy-nine out of 2073 participants had refractive surgery. 53 subjects underwent PRK, 23 LASIK, two radial keratotomy (RK), and one astigmatic correction. Complications occurred in 6/79 (7.6%) of participants, including five subjects who underwent PRK and one following RK, occurring between eight to 217 days after surgery. Five ulcers and one unspecified keratitis were noted. In univariate analysis, type of surgery (p=0.02) and history of AIDS (p=0.02) were risk factors for complications. In logistic regression analysis, no variables were found to be risk factors for complications.
Conclusion:
Complications were infrequent among HIV+ participants following refractive surgery. Point estimates suggest that PRK may have more complications than LASIK and that advanced HIV, reflected by prior AIDS, may be associated with an increased risk of complications. Further study will be needed to confirm these findings.
Keywords: HIV, Refractive Surgery, LASIK, PRK
Introduction
In the 1980s and early 1990s, human immunodeficiency virus (HIV) infection was largely considered a fatal disease. The emergence of improved disease recognition, access to care, and effective treatment with effective combination antiretroviral therapy (ART) have significantly decreased the number of HIV-related deaths, as well as increased the total life expectancy of HIV-positive (HIV+) patients.1,a Given improved survival, HIV+ patients are now more likely to pursue common elective procedures, such as refractive surgery to improve visual acuity. However, the FDA currently states that patients with HIV or other immunodeficiency states are not good candidates for refractive surgery.b A recent published guideline by the American Academy of Ophthalmology (AAO) lists uncontrolled autoimmune or other immune-mediated disease as an absolute contraindication to refractive surgery, while controlled disease is only relatively contraindicated.2
The current body of literature is limited on the outcomes of elective refractive surgery in the HIV+ population.3,4 The objectives of this study were to first evaluate the type of refractive surgery performed and then characterize the subjects by the following: antiretroviral therapy use, time since HIV diagnosis, presence of AIDS, CD4+ T-lymphocyte count, HIV-1 viral load, and select comorbidities (diabetes mellitus type II and smoking). Secondly, we studied both the incidence of and risk factors for postoperative complications of refractive surgery.
Materials and Methods
Started in 1986, the U.S. Military HIV Natural History Study (NHS) is a large, continuous enrollment cohort study of HIV+ active duty U.S. servicemembers, their family members and retirees from the Department of Defense (DoD).5–7 Active duty service members are routinely screened for HIV infection, approximately every two years, and negative test dates are collected in addition to positive dates. Participants have study visits approximately every six months including coordinator and physician interviews, centralized DoD electronic medical record review, and laboratory assays. The study has been approved by the Institutional Review Board of the Uniformed Services University of the Health Sciences (USU) and participating sites; all participants provide written informed consent.
Figure 1 outlines the selection of subjects for this study. Inclusion criteria consisted of 1) HIV-positive status between 1997 and 2016; 2) a history of refractive surgery demonstrated by one of the following current procedural terminology (CPT) codes: 65760/S0800 (laser-assisted in situ keratomileusis; LASIK), 66999/S0810 (photorefractive keratectomy; PRK), 65771 (radial keratotomy; RK), 65772/65775 (astigmatism correction), 65765 (keratophakia), 65767 (epikeratoplasty), S0812 (phototherapeutic keratectomy; PTK), 0402T (collagen cross-linking), 65785 (implantation of intrastromal corneal ring); and 3) a refractive International Classification of Disease (ICD)-9 code (367.0-367.9). Complications were defined by ICD-9 codes: [corneal ulcer (370.00 – 370.07), interstitial keratitis (370.50 – 370.59), unspecified keratitis (370.9), corneal abrasion (918.1), corneal haze (371.89), or diffuse lamellar keratitis [DLK (370.8)] within one year after refractive surgery.
Figure 1:
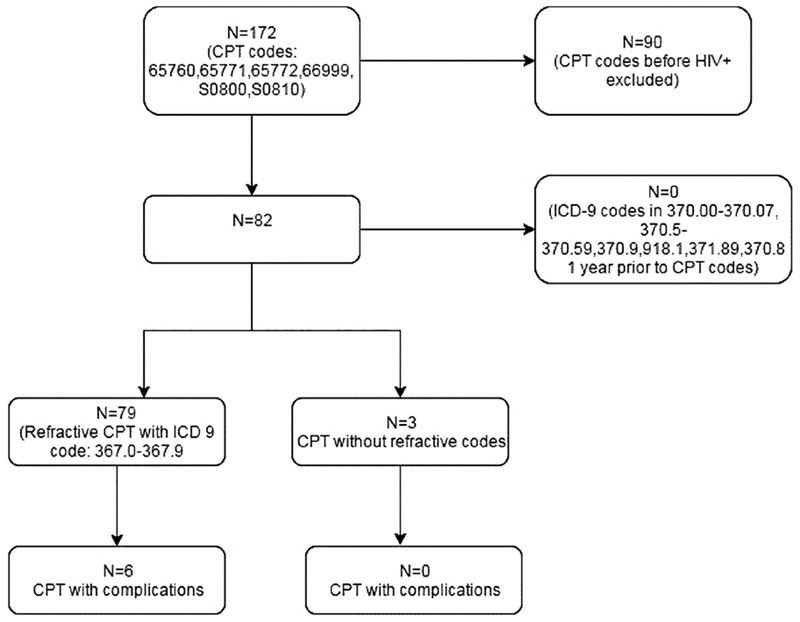
Flow Chart of Subject Selection
Subjects were excluded from this study for any one of the following: 1) a history of refractive surgery prior to the diagnosis of HIV infection; 2) a history of an ICD-9 code of a surgical complication [corneal ulcer (370.00 – 370.07), interstitial keratitis (370.50 – 370.59), unspecified keratitis (370.9), corneal abrasion (918.1), corneal haze (371.89), or diffuse lamellar keratitis [DLK (370.8)] within one year before refractive surgery; or 3) absence of a refractive CPT code. The outcome studied was the proportion of post-refractive surgical complication(s) after refractive surgery.
Demographic and clinical data were extracted from the study database for analysis including age, gender, race, time since HIV diagnosis, history of AIDS (1993 CDC-rev), antiretroviral therapy (ART) by medication class, CD4 count and HIV viral load at time of ophthalmic diagnosis, total number of ophthalmic diagnoses, diabetes mellitus type II (DMII), hypertension (HTN), hyperlipidemia (HLD), and smoking. Baseline was defined as earliest documented HIV positive test date; ART was defined as in previous NHS studies (Supplemental Table 1).9 Most patients take two or more nucleoside reverse transcriptase inhibitors (NRTI) and either a non-nucleoside reverse transcriptase inhibitor (NNRTI), unboosted versus boosted protease inhibitor (PI) or an integrase inhibitor.
Statistical Analysis
All events occurred in HIV+ participants. Events were defined as either time of refractive surgery or in controls as censorship date (death, lost to follow-up, or the last study visit). Statistical analysis was completed using Chi square or Wilcoxon-Mann-Whitney tests. Further multivariate analysis was completed using logistic regression. All tests were two-sided, and a p-value less than 0.05 was considered statistically significant. Statistical analyses were performed using SAS version 9.4 (Cary, North Carolina, USA).
Results
Baseline Characteristics
In the NHS cohort 79 out of 2073 participants met inclusion criteria. Of the participants 53 underwent PRK, 23 LASIK, 2 RK and 1 astigmatic correction. Indications for surgery can be found in Supplemental Table 2. Baseline characteristics are found in Table 1. Compared to the HIV-positive subjects who did not undergo refractive surgery, a greater proportion of refractive surgery patients in the cohort were active duty (n=60, 75.9% versus (vs) n=1008, 50.6%, p=0.0005) and enlisted (n=62, 78.5% vs. n=1441, 72.3%, p<0.0001). A significant difference in Armed Service branch representation existed (n=39, 49.4% Navy; n=25, 31.6% Army; n=8 10.1% Marines; n=7, 8.9% Air Force; p=0.021).
Table 1.
Baseline characteristics of HIV+ participants who had refractive surgery
| Overall | Refractive surgery | P-value | ||
|---|---|---|---|---|
| N (%) or Median (IQR) | No N (%) or Median (IQR) | Yes N (%) or Median (IQR) | ||
| Participants | 2073 | 1994 | 79 | |
| Demographics | ||||
| Age at surgery or censor | 40.8 (31.9,50.2) | 41.2 (32.1,50.7) | 31.2 (26.6,38.7) | <.0001 |
| Gender | 0.8535 | |||
| Male | 1904 (91.8) | 1831 (91.8) | 73 (92.4) | |
| Female | 169 (8.2) | 163 (8.2) | 6 (7.6) | |
| Race | 0.9406 | |||
| Caucasian | 786 (37.9) | 755 (37.9) | 31 (39.2) | |
| African-American | 932 (45.0) | 898 (45.0) | 34 (43.0) | |
| Hispanic/Other | 355 (17.1) | 341 (17.1) | 14 (17.7) | |
| Marital status | 0.1179 | |||
| Single | 1059 (51.1) | 1022 (51.3) | 37 (46.8) | |
| Married | 866 (41.8) | 826 (41.4) | 40 (50.6) | |
| Missing | 148 (7.1) | 146 (7.3) | 2 (2.5) | |
| Rank | <.0001 | |||
| Officer/Warrant | 188 (9.1) | 173 (8.7) | 15 (19.0) | |
| Enlisted | 1503 (72.5) | 1441 (72.3) | 62 (78.5) | |
| N/A (e.g. Dependent) | 382 (18.4) | 380 (19.1) | 2 (2.5) | |
| Duty Status | 0.0005 | |||
| Active Duty | 1068 (51.5) | 1008 (50.6) | 60 (75.9) | |
| Retired | 887 (42.8) | 869 (43.6) | 18 (22.8) | |
| Dependent | 87 (4.2) | 86 (4.3) | 1 (1.3) | |
| Other (e.g. Civilian, end of service) | 30 (1.4) | 30 (1.5) | 0 (0.0) | |
| Service | 0.0211 | |||
| Air Force | 448 (21.6) | 441 (22.1) | 7 (8.9) | |
| Army | 562 (27.1) | 537 (26.9) | 25 (31.6) | |
| Marines | 147 (7.1) | 139 (7.0) | 8 (10.1) | |
| Navy | 856 (41.3) | 817 (41.0) | 39 (49.4) | |
| Other (e.g. public health service, foreign military) | 60 (2.9) | 60 (3.0) | 0 (0.0) | |
| HIV related | ||||
| Age HIV dx | 28.8 (24.2,35.1) | 29.0 (24.4,35.3) | 25.5 (22.8,31.3) | 0.0004 |
| Year of HIV dx | 0.0040 | |||
| Before 1997 | 749 (36.1) | 734 (36.8) | 15 (19.0) | |
| 1997-2000 | 315 (15.2) | 306 (15.3) | 9 (11.4) | |
| 2001-2005 | 380 (18.3) | 360 (18.1) | 20 (25.3) | |
| 2006-2010 | 422 (20.4) | 400 (20.1) | 22 (27.8) | |
| 2011-2016 | 207 (10.0) | 194 (9.7) | 13 (16.5) | |
| CD4 at HIV dx (cells/ul) | 475(343,628) | 475 (341,630) | 505 (380,615) | 0.5711 |
| VL at HIV dx (log10 copies/ml) | 4.4 (3.8,4.9) | 4.4 (3.8,4.9) | 4.5 (3.9,4.8) | 0.5371 |
| HIV dx to surgery or censor | 9.1 (4.7,16.2) | 9.3 (4.9,16.6) | 4.1 (2.1,7.7) | <.0001 |
| Age ART start | 33.1 (27.4,39.7) | 33.2 (27.6,39.9) | 28.7 (23.9,34.3) | 0.0002 |
| ART Initiation Era | 0.0184 | |||
| 1996-2000 | 804 (38.8) | 786 (39.4) | 18 (22.8) | |
| 2001-2008 | 469 (22.6) | 446 (22.4) | 23 (29.1) | |
| 2009-2017 | 532 (25.7) | 504 (25.3) | 28 (35.4) | |
| No ART Record Start | 268 (12.9) | 258 (12.9) | 10 (12.7) | |
| Time from ART to surgery or censor | 7.1 (3.4,13.4) | 7.3 (3.6,13.9) | 3.2 (0.6,6.0) | <.0001 |
| CD4 at ART (cells/ul) | 355 (251,478) | 352 (249,474) | 421 (301,515) | 0.0085 |
| VL at ART (log10 copies/ml) | 4.5 (3.8,5.0) | 4.5 (3.8,5.0) | 4.5 (3.8,4.9) | 0.7251 |
| History of AIDS | 0.3568 | |||
| No | 1976 (95.3) | 1899 (95.2) | 77 (97.5) | |
| Yes | 97 (4.7) | 95 (4.8) | 2 (2.5) | |
| Year of surgery or censor | 0.0129 | |||
| Before 1997 | 52 (2.5) | 52 (2.6) | 0 (0.0) | |
| 1997-2000 | 163 (7.9) | 156 (7.8) | 7 (8.9) | |
| 2001-2005 | 258 (12.4) | 241 (12.1) | 17 (21.5) | |
| 2006-2010 | 381 (18.4) | 361 (18.1) | 20 (25.3) | |
| 2011-2016 | 1219 (58.8) | 1184 (59.4) | 35 (44.3) | |
| CD4 at surgery or censor (cells/ul) | 627 (450,839) | 627 (450,841) | 624 (446,744) | NR* |
| VL at Surgery or censor | 1.6(1.3,2.6) | 1.5 (1.3,2.6) | 1.7 (1.3,3.4) | NR* |
| ART status at surgery or censor | NR* | |||
| Yes | 1659 (80.0) | 1609 (80.7) | 50 (63.3) | |
| No | 414 (20.0) | 385 (19.3) | 29 (36.7) | |
| ART medication by class at surgery or censor | NR* | |||
| Boosted PI | 282 (17.0) | 279 (17.3) | 3 (6.0) | |
| II | 475 (28.6) | 467 (29.0) | 8 (16.0) | |
| NNRTI | 669 (40.3) | 636 (39.5) | 33 (66.0) | |
| Other | 52 (3.1) | 52 (3.2) | 0 (0.0) | |
| Three or more NRTI | 31 (1.9) | 31 (1.9) | 0 (0.0) | |
| Unboosted PI | 150 (9.0) | 144 (8.9) | 6 (12.0) | |
| Diabetes Mellitus Type II at baseline | 0.1559 | |||
| Yes | 201 (9.7) | 197 (9.9) | 4 (5.1) | |
| No | 1872 (90.3) | 1797 (90.1) | 75 (94.9) | |
| Hypertension at baseline | 0.3862 | |||
| Yes | 670 (32.3) | 648 (32.5) | 22 (27.8) | |
| No | 1403 (67.7) | 1346 (67.5) | 57 (72.2) | |
| Hyperlipidemia at baseline | 0.1962 | |||
| Yes | 1040 (50.2) | 1006 (50.5) | 34 (43.0) | |
| No | 1033 (49.8) | 988 (49.5) | 45 (57.0) | |
| Tobacco Smoking at baseline | 0.2028 | |||
| Yes | 1209 (78.6) | 1159 (78.9) | 50 (72.5) | |
| No | 329 (21.4) | 310 (21.1) | 19 (27.5) | |
NR - not reported due to differing follow-up between groups
Reflecting the overall trend toward more elective refractive surgery within this population and the general population, an increasing number of refractive surgeries were noted in successive calendar intervals within the cohort (Figure 2, p=0.014 for increasing trend). Nearly two-thirds of subjects undergoing refractive surgery (50/79) were on treatment with ART at the time of surgery and 49 subjects had VL<400 copies/mL; the median CD4 was 624 cells/uL and only one subject had <200 cells/uL.
Figure 2:
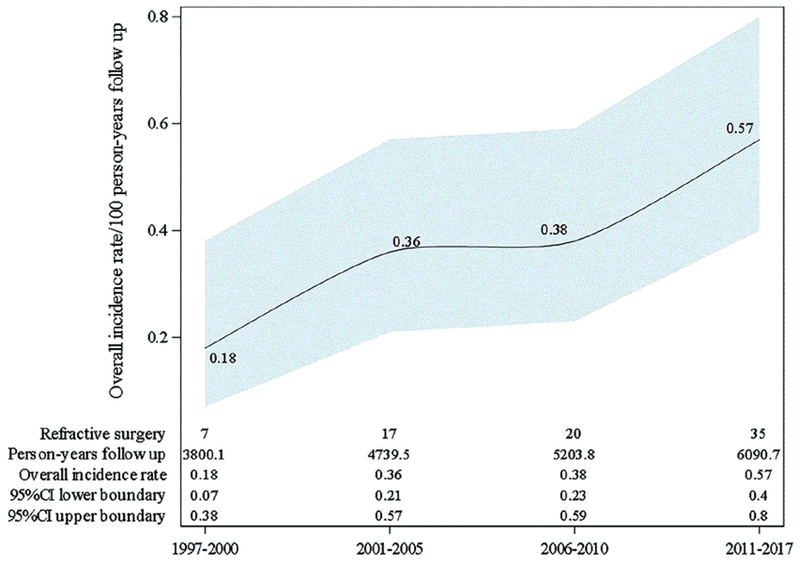
Incidence of Refractive Surgery
Complications and Risk Factors
Six out 79 participants (7.6%) undergoing refractive surgery experienced postoperative complications. No complications were observed in patients undergoing LASIK. Complications within 1 year of surgery occurred in only one RK patient (44 days). However, five patients (9.6%) who underwent PRK had complications within one year (8, 13, 127, 134, and 217 days). Of the six complications, three were an unspecified corneal ulcer, one marginal corneal ulcer,one perforated corneal ulcer, and one unspecified keratitis. In univariate analysis, type of surgery performed (p=0.0206) and a prior history of AIDS at time of procedure (p=0.0219) were risk factors for complications (Supplemental Table 3). In the patients that had complications, three of six subjects were on ART at time of surgery and four had a detectable viral load >400 copies/mL (1,735; 2,547; 12,600; 36,269). But none had a CD4 counts less than 200 cells/uL at time of surgery (median 658.0 cell/ul; range 349.0-691.0). Of those that were on ART, in addition to two NRTI, one was on an unboosted PI, one a boosted PI and another a NNRTI. Using logistic regression analysis, no covariates were found to be risk factors for complications; however, the sample size was small (Supplemental Table 4).
Discussion
This study represents the first published cohort of HIV-positive patients that underwent refractive surgery, to the authors’ knowledge. Hovanesian et al., reported in 1999 a case of bilateral bacterial keratitis following a LASIK procedure in an HIV-positive patient.3 Unquantified anecdotal reports of postoperative keratitis, delayed wound healing, and dry-eye after refractive surgery in HIV-positive patients have also been reported.4 The lack of published data on postsurgical outcomes in this population has led to inconsistency between published recommendations and actual practice patterns. The United States Food and Drug Administration (FDA) established a list of contraindications to PRK in the 1990s, and later published a similar list of contraindications to LASIK. The FDA currently states that patients with HIV or other immunodeficiency states are not good candidates for refractive surgery.b Cobo-Soriano et al., suggested that controlled systemic disease need not be an absolute contraindication to LASIK.8 A recent published guideline by the American Academy of Ophthalmology (AAO) lists uncontrolled autoimmune or other immune-mediated disease as an absolute contraindication to refractive surgery, while controlled disease is only relatively contraindicated.2 In actual practice, there is no universal approach to refractive surgery in the HIV population. A 2010 web-based survey of 285 refractive surgeons revealed that 50.2% of respondents consider persons with HIV acceptable candidates for elective refractive surgery, but 88% felt that patients with current AIDS were not appropriate candidates.4
In our study of HIV+ active duty, retirees, and dependents, we found an overall proportion of post-refractive surgical complications of 7.6%. The proportion of complications was 9.4% in those who underwent PRK, whereas no complications were observed in the LASIK patients; PRK was more than twice as common as LASIK in this population, reflecting military practice. Corneal ulcer accounted for five out of the six total complications. Although it was originally thought that PRK predisposes patients to an increased risk of infectious keratitis, large studies have demonstrated similar rates between LASIK and PRK. Wroblewski et al., reported five cases of post-procedural infectious keratitis out of 25,337 PRK procedures (0.019%) performed at six institutions within the Army and Navy database between 1995-2004.9 Llovet et al., reported 72 cases of post-procedural infectious keratitis out of 204,586 LASIK procedures (0.035% rate) at a single institution in Spain between 2002-2008.10 Despite the similar complication rates, it has been suggested that PRK poses an increased risk for post-procedural infectious keratitis due to the breakdown of the barrier function of the corneal epithelium.11 On the other hand, a break in the epithelial barrier during LASIK has been reported to predispose patients to keratitis.10 It appears from the data collected in our study that PRK in HIV+ patients may be a risk factor for ulcers, although whether they were specifically infectious is difficult to discern due to use of ICD-9 codes. In addition, it is critical to recognize that three of the five PRK complications occurred late after the surgery (127, 134, and 217 days). It is possible that these are unrelated to the refractive surgery, or that the disruption of the epithelial barrier at the time of surgery may predispose these patients to later complications. A previous study12 found that atypical organisms like mycobacteria and fungus have a later mean onset of presentation; however, unfortunately the specific culture data was not available in our complications. Finally, the small sample size limits the precision of the point estimates, so should be interpreted cautiously.
We found that a history of AIDS was a potential risk factor for complication after refractive surgery. To our knowledge, there are no prior studies that address post-refractive surgical complications in the HIV population, nor are there published guidelines that suggest an ideal preoperative CD4 count. In cataract surgery, there are very few studies discussing surgical complications in this patient populace and no published guidelines.13,14 A report of abdominal and plastic surgeries among HIV+ also found that lower CD4 (<200 cells/ uL) and viral load>10,000 copies/ml were associated with increased risk of complications and some surgical guidelines have reinforced this.15,16 In orthopedic trauma, a CD4 count <300 cells/uL was associated with development of postoperative infection.17 However, in patients with HIV, the surgical risk assessment should be individualized and discussed with the patient.18,c It seems prudent that surgeons who are considering operating on patients with HIV should review CD4 counts and viral load to help inform the approach to follow-up. The surgeon could consider that if the CD4 count is <200 cell/ul and viral load >10,000 copies/ml to defer surgery and recommend that the patient start ART therapy; but further studies and guidelines are needed in ophthalmic surgery. In addition, poor ART compliance may signal poor post-operative compliance with topical medications. This is also a potential area of future study in HIV+ patients.
One of the lingering concerns of refractive surgeons operating on patients with HIV infection has been risk of viral transmission during the procedure. However, despite concerns in the pre-ART era, HIV transmission from patients to operating surgeons is extremely rare. Hagen et al., concluded that, based on experimentation with the similarly structured pseudorabies virus, excimer laser ablation of the cornea of an HIV-infected patient is unlikely to transmit the virus to the surgeon.19 In another study by Taravella et al., only DNA fragments of an attenuated varicella-zoster virus were found to have survived excimer laser ablation.20 Both of these studies reinforce the low risk, however, a web-based survey of refractive surgeons operating on HIV patients revealed that 51% were concerned about virus transmission to the surgeon or operating room staff and 40% were concerned about virus transmission to other patients.4 Standard precautions to prevent occupational exposure to HIV and other infectious pathogens in the healthcare setting and during surgery have proven highly effective with only one confirmed healthcare worker HIV transmission event from 2000-2013.21 These data reinforce the need for ongoing and further education of providers and staff regarding the utility of standard precautions and low risk of HIV transmission. And while additional studies to fully characterize HIV transmission risks in various surgical settings such as ophthalmology are also needed, the increasing trend of refractive surgeries in our study suggests that attitudes may be shifting in a positive way.
The key limitations of this study are related to the patient population and number of procedures performed. The NHS subjects are mostly male, young and previously healthy, and active duty with open access to healthcare and medications. These limitations may impact the generalizability. The overall number of subjects was small, so findings should be interpreted cautiously. In addition, specific microorganism culture data was unavailable.
In conclusion, complications occurred infrequently in HIV+ patients with virologic suppression on ART following refractive surgery. Many patients living with HIV infection may be appropriate candidates for refractive surgery. PRK may predispose to more complications than LASIK in this population, although larger studies will be required to fully evaluate this. Advanced HIV infection, reflected by a prior diagnosis of AIDS, as well as active viremia and the absence of ART, may be associated with an increased risk of complications. Further study using larger cohorts or meta-analysis will be needed to better understand the risk factors of complications of refractive surgery in HIV+ patients.
Supplementary Material
What Was Known
There is limited literature on refractive surgery in HIV+ patients. This study evaluated a cohort of HIV+ patients that underwent refractive surgery in order to assess the rate of complications and related risk factors.
What This Paper Adds
No HIV+ patients that underwent LASIK had a complication. Further analysis is needed in larger cohorts to better understand if the type of refractive surgical procedure is a risk factor for complications.
A history of AIDS is a risk factor for complications in univariate analysis. It is critical that ophthalmologists evaluate anti-retroviral therapy status, CD4 and viral load, and history of AIDS prior to operating on an HIV+ patient.
Synopsis:
This study analyzed the outcomes of HIV-positive patients undergoing refractive surgery. There were no complications in patients that underwent LASIK. A history of AIDS was a significant risk factor.
Acknowledgements
We would like to express appreciation to Camille Estupigan for editorial assistance during preparation of this manuscript.
Members of the Infectious Disease Clinical Research Program HIV Working Group include the following:
Brooke Army Medical Center, Fort Sam Houston, TX: S. De Leon; S. Merritt; T. Merritt; Lt Col J. Okulicz; T. Sjoberg
Madigan Army Medical Center, Joint Base Lewis McChord, WA: C. Baker; S. Chambers; R. Colombo; COL T. Ferguson; LTC A. Kunz; C. Schofield; M. Stein
National Institute of Allergy and Infectious Diseases, Bethesda, MD: J. Powers; COL (Ret.) E. Tramont
Naval Medical Center Portsmouth, Portsmouth, VA: S. Banks; CAPT K. Kronmann; T. Lalani; R. Tant; T. Warkentien
Naval Medical Center San Diego, San Diego, CA: S. Cammarata; N. Kirkland; CAPT R. Maves; CAPT (Ret.) G. Utz
Tripler Army Medical Center, Honolulu, HI: COL M. Price
Uniformed Services University of the Health Sciences, Bethesda, MD: B. Agan; X. Chu; W. Horton; H. Hsieh; A. Noiman; E. Parmelee; D. Tribble; X. Wang; S. Won
Walter Reed Army Institute of Research, Silver Spring, MD: S. Peel
Walter Reed National Military Medical Center, Bethesda, MD: I. Barahona; LTC J. Blaylock; C. Decker; A. Ganesan; COL R. Ressner; D. Wallace
Financial Support: This study was conducted by the Infectious Disease Clinical Research Program (IDCRP), a Department of Defense (DoD) program executed by the Uniformed Services University of the Health Sciences (USUHS) through a cooperative agreement with The Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc. (HJF). This project has been funded in whole, or in part, with federal funds from the National Institute of Allergy and Infectious Diseases, National Institutes of Health (NIH), under Inter-Agency Agreement Y1-AI-5072.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: No conflicting relationship exists for any author
Meeting Presentation: Presented at the ASCRS-ASOA Society of Military Ophthalmology Symposium, May 3-7, 2019, San Diego, CA
Disclaimer: The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, Naval Medical Center San Diego, Madigan Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Air Force, the Department of the Army, the Department of the Navy, Department of Defense, the Uniformed Services University of the Health Sciences, the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc. or any other agency of the U.S. Government. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government. The investigators have adhered to the policies for protection of human subjects as prescribed in 45CRF46.
References
- 1.Marcus J, Chao C, Leyden WA, et al. Narrowing the Gap in Life Expectancy for HIV+ Compared with HIV− Individuals. CROI; Boston Massachusetts: 2016. Abstract #54. [Google Scholar]
- 2.“Refractive Errors & Refractive Surgery Preferred Practice Pattern.” American Academy of Ophthalmology. 9 September 2017. [Google Scholar]
- 3.Hovanesian JA, Faktorovich EG, Hoffbauer JD, et al. Bilateral bacterial keratitis after laser in situ keratomileusis in a patient with human immunodeficiency virus infection. Arch Ophthalmol. 1999; 117:968–70. [PubMed] [Google Scholar]
- 4.Aref AA, Scott IU, Zerfoss EL, Kunselman AR. Refractive surgical practices in persons with human immunodeficiency virus positivity or acquired immune deficiency syndrome. J Cataract Refract Surg. 2010; 36:153–60. [DOI] [PubMed] [Google Scholar]
- 5.Ganesan A, Landrum ML, Chun H, et al. Outcomes of highly active antiretroviral therapy in the context of universal access to healthcare: the U.S. Military HIV Natural History Study. AIDS Research and Therapy 2010; 7(1): 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guest JL, Weintrob AC, Rimland D, et al. A Comparison of HAART Outcomes between the US Military HIV Natural History Study (NHS) and HIV Atlanta Veterans Affairs Cohort Study (HAVACS). PLoS ONE. 2013; 8(5): e62273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marconi VC, Grandits GA, Weintrob AC, et al. Outcomes of highly active antiretroviral therapy in the context of universal access to healthcare: the U.S. Military HIV Natural History Study. AIDS Res Ther. 2010; 7: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cobo-Soriano R, Beltran J, Baviera J. LASIK Outcomes in Patients with Underlying Systemic Contraindications. Ophthalmology. 2006; 113(7): 1118e1–e8. [DOI] [PubMed] [Google Scholar]
- 9.Wroblewski KJ, Pasternak JF, Bower KS, et al. Infectious Keratitis after Photorefractive Keratectomy in the United States Army and Navy. Ophthalmology. 2006; 113(4): 520–525. [DOI] [PubMed] [Google Scholar]
- 10.Llovet F, de Rojas V, Interlandi E, et al. Infectious Keratitis in 204 586 LASIK Procedures. Ophthalmology 2010; 117(2): 232–238. [DOI] [PubMed] [Google Scholar]
- 11.Donnenfeld ED, O’Brien TP, Solomon R, et al. Infectious Keratitis after Photorefractive Keratectomy. Ophthalmology 2003; 110:743–747. [DOI] [PubMed] [Google Scholar]
- 12.Karp CL, Tuli SS, Yoo SH, et al. Infectious keratitis after Lasik. Ophthalmology. 2003. March;110(3):503–10. [DOI] [PubMed] [Google Scholar]
- 13.Accorinti M, Cecere M, Scala A, Pirraglia MP. Cataract Surgery in HIV Seropositive Patients: Long-Term Follow-Up. OculImmunolInflamm. 2018. January 15:1–12. [DOI] [PubMed] [Google Scholar]
- 14.Chew GWM, Teoh SCB, Agrawal R. Analysis and Outcomes of Cataract Surgery in Patients with Acquired Immunodeficiency Syndrome. Ocul Immunol Inflamm. 2017. August;25(4):535–539. [DOI] [PubMed] [Google Scholar]
- 15.Deneve JL, Shantha JG, Page AJ, Wyrzykowski AD, Rozycki GS, Feliciano DV. CD4 count is predictive of outcome in HIV-positive patients undergoing abdominal operations. Am J Surg. 2010. December;200(6):694–9. [DOI] [PubMed] [Google Scholar]
- 16.Davison SP, Reisman NR, Pellegrino ED, Larson EE, Dermody M, Hutchison PJ. Perioperative guidelines for elective surgery in the human immunodeficiency virus positive patient. Plast Reconstr Surg. 2008. May;121(5):1831–40. [DOI] [PubMed] [Google Scholar]
- 17.Guild GN, Moore TJ, Barnes W, Hermann C. CD4 count is associated with postoperative infection in patients with orthopaedic trauma who are HIV positive. Clin Orthop Relat Res. 2012. May;470(5):1507–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madiba TE, Muckart DJ, Thomson SR. Human immunodeficiency disease: how should it affect surgical decision making? World J Surg. 2009. May;33(5):899–909. [DOI] [PubMed] [Google Scholar]
- 19.Hagen KB, Kettering JD, Aprecio RM, Beltran F, Maloney RK. Lack of Virus Transmission by the Excimer Laser Plume. Am J Ophthalmol. 1997; 124:206–11. [DOI] [PubMed] [Google Scholar]
- 20.Taravella MJ, Weinberg A, Blackburn P, May M. Do Intact Viral Particles Survive Excimer Laser Ablation? Arch Ophthalmol. 1997;115:1028–1030. [DOI] [PubMed] [Google Scholar]
- 21.Joyce MP, Kuhar D, Brooks JT. Notes from the field: occupationally acquired HIV infection among health care workers - United States, 1985-2013. MMWR Morb Mortal Wkly Rep. 2015: 9;63(53):1245–6. [PMC free article] [PubMed] [Google Scholar]
Other Cited Material
- a.“HIV/AIDS.” World Health Organization, 19 July 2018, www.who.int/en/news-room/fact-sheets/detail/hiv-aids. [Google Scholar]
- b.“When is LASIK not for me?” U.S. Food & Drug Administration, 11 July 2018, https://www.fda.gov/medicaldevices/productsandmedicalprocedures/surgeryandlifesupport/lasik/ucm061366.htm. [Google Scholar]
- c.“Perioperative Management” New York State Department of Health AIDS Institute, January 2012, https://www.hivguidelines.org/hiv-care/perioperative-management/. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


